The Age-Related Risk of Severe Outcomes Due to COVID-19 Infection: A Rapid Review, Meta-Analysis, and Meta-Regression
Abstract
1. Introduction
2. Methods
2.1. Search, Selection, and Data Extraction
2.2. Risk of Bias Assessment
2.2.1. Recruitment Procedure and Follow-Up
2.2.2. Exposure Definition and Measurement
2.2.3. Outcome Source and Validation
2.2.4. Age-Dependent Risk Factors
2.2.5. Analysis Methods Including Chronology
2.2.6. Funding
2.2.7. Conflict of Interest
2.2.8. Overall Assessment of Risk of Bias
2.3. Statistical Analysis
3. Results
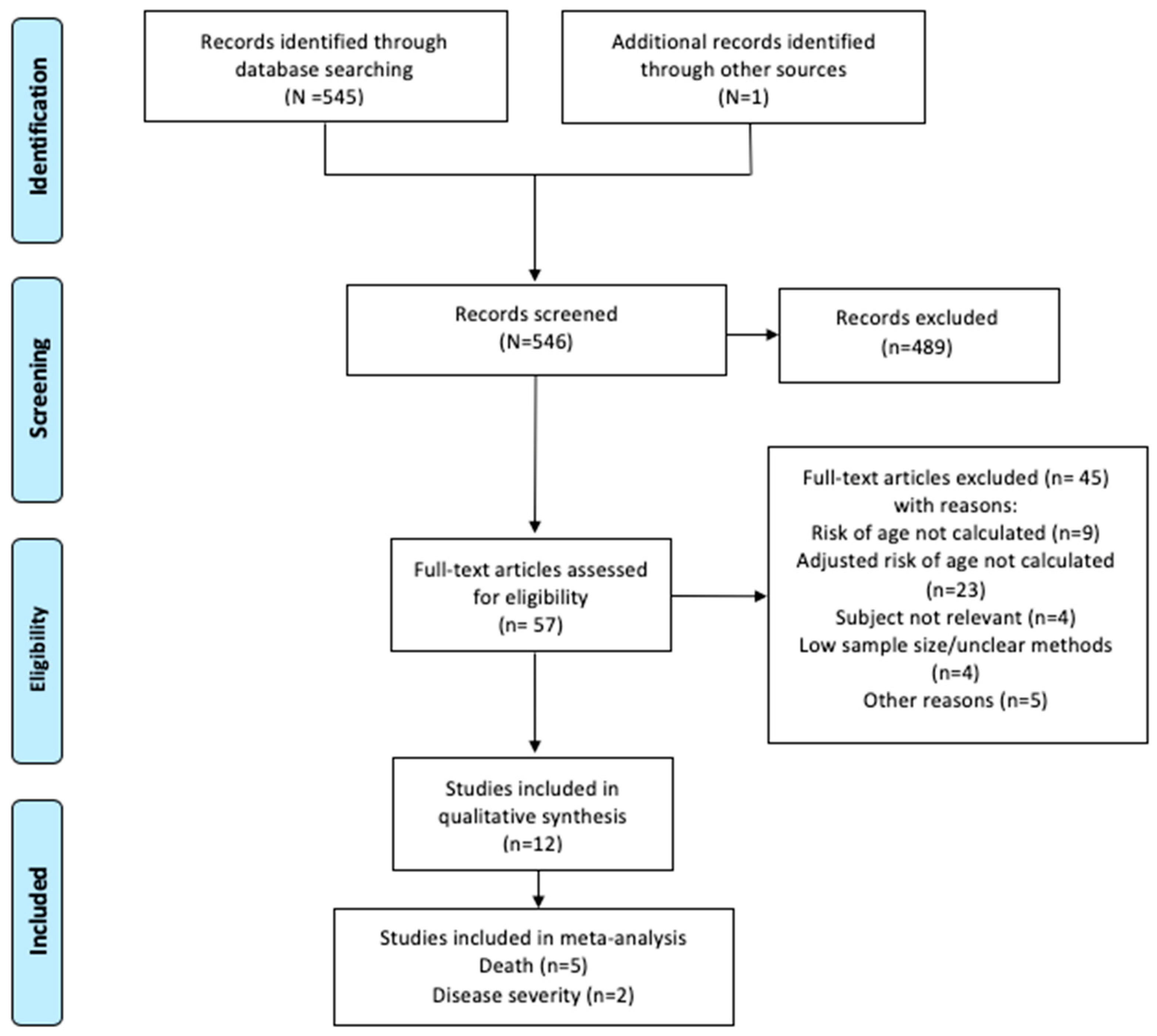
3.1. Search Results
3.2. Disease Severity by a Composite Index
3.2.1. Description of Studies
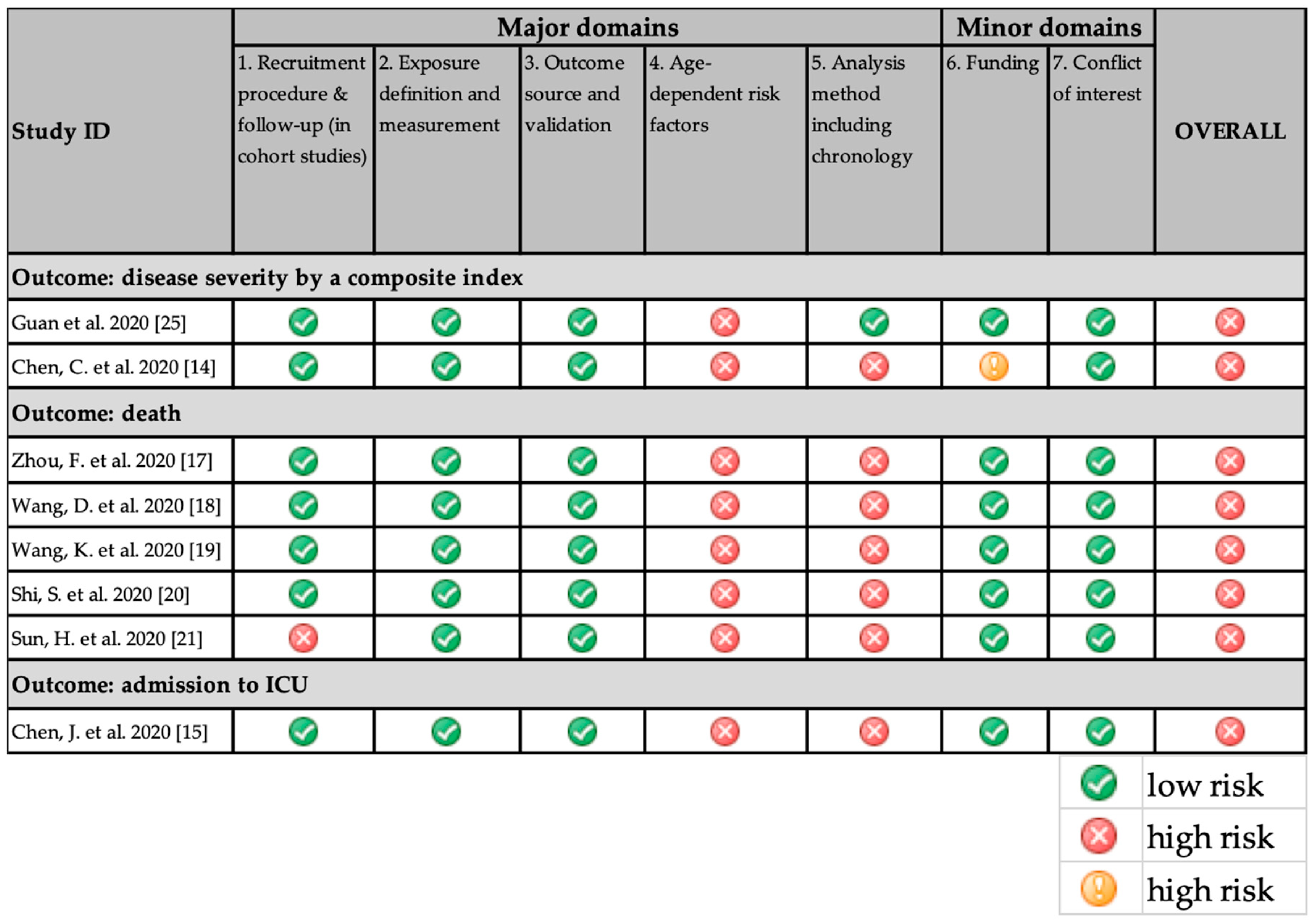
3.2.2. Risk of Bias
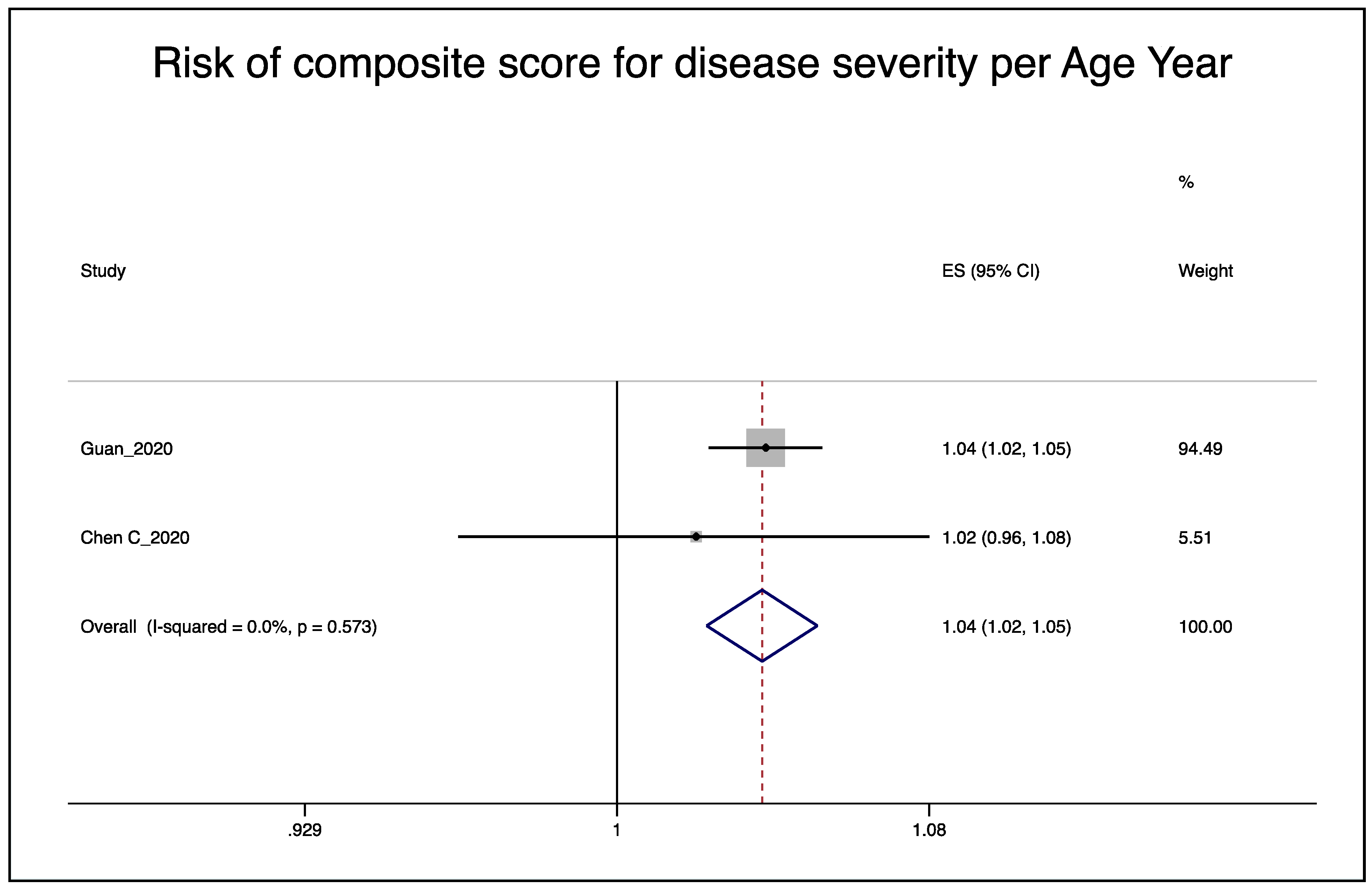
3.2.3. Meta-Analysis and Meta-Regression
3.3. Death
3.3.1. Description of Studies
3.3.2. Risk of Bias
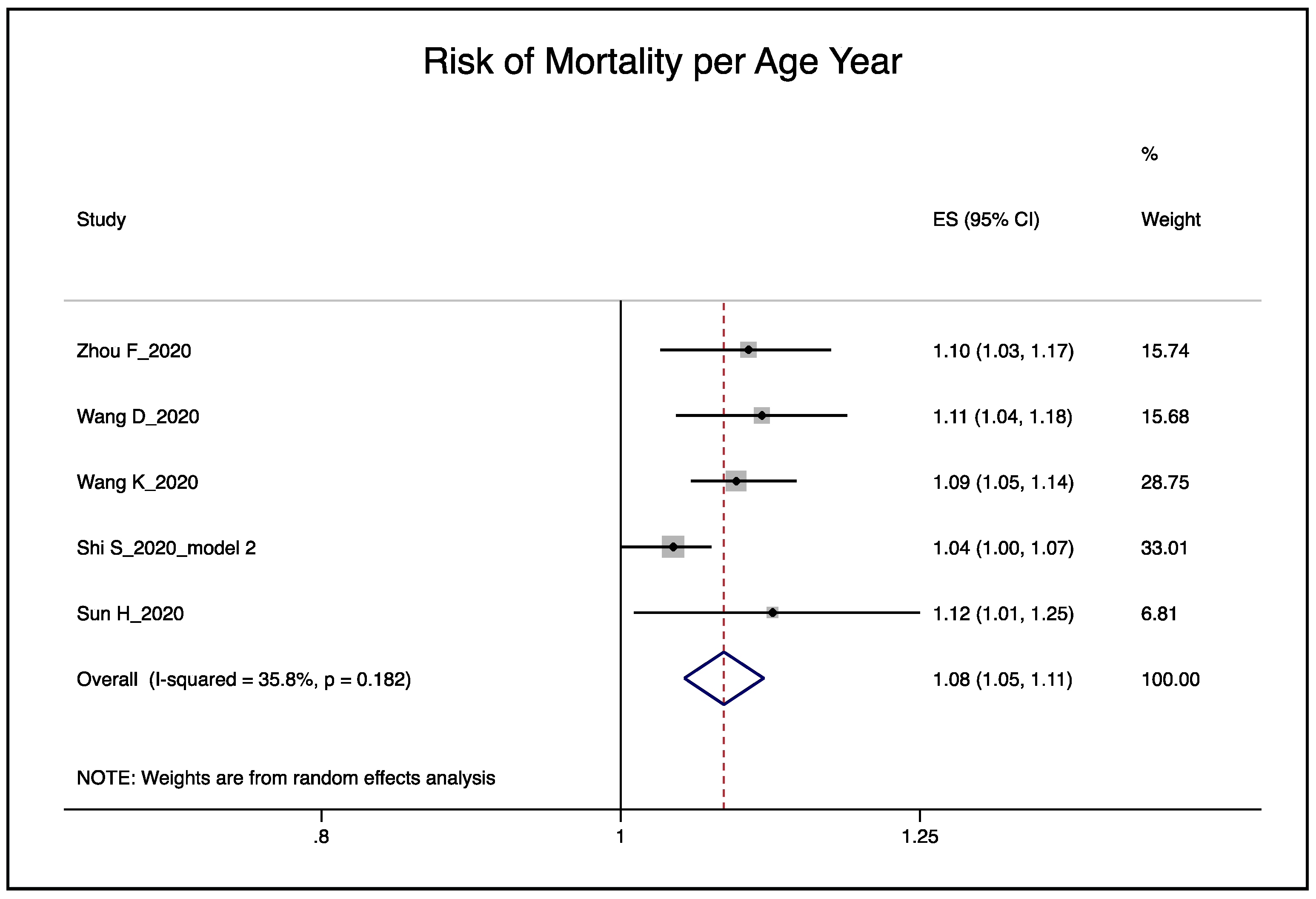
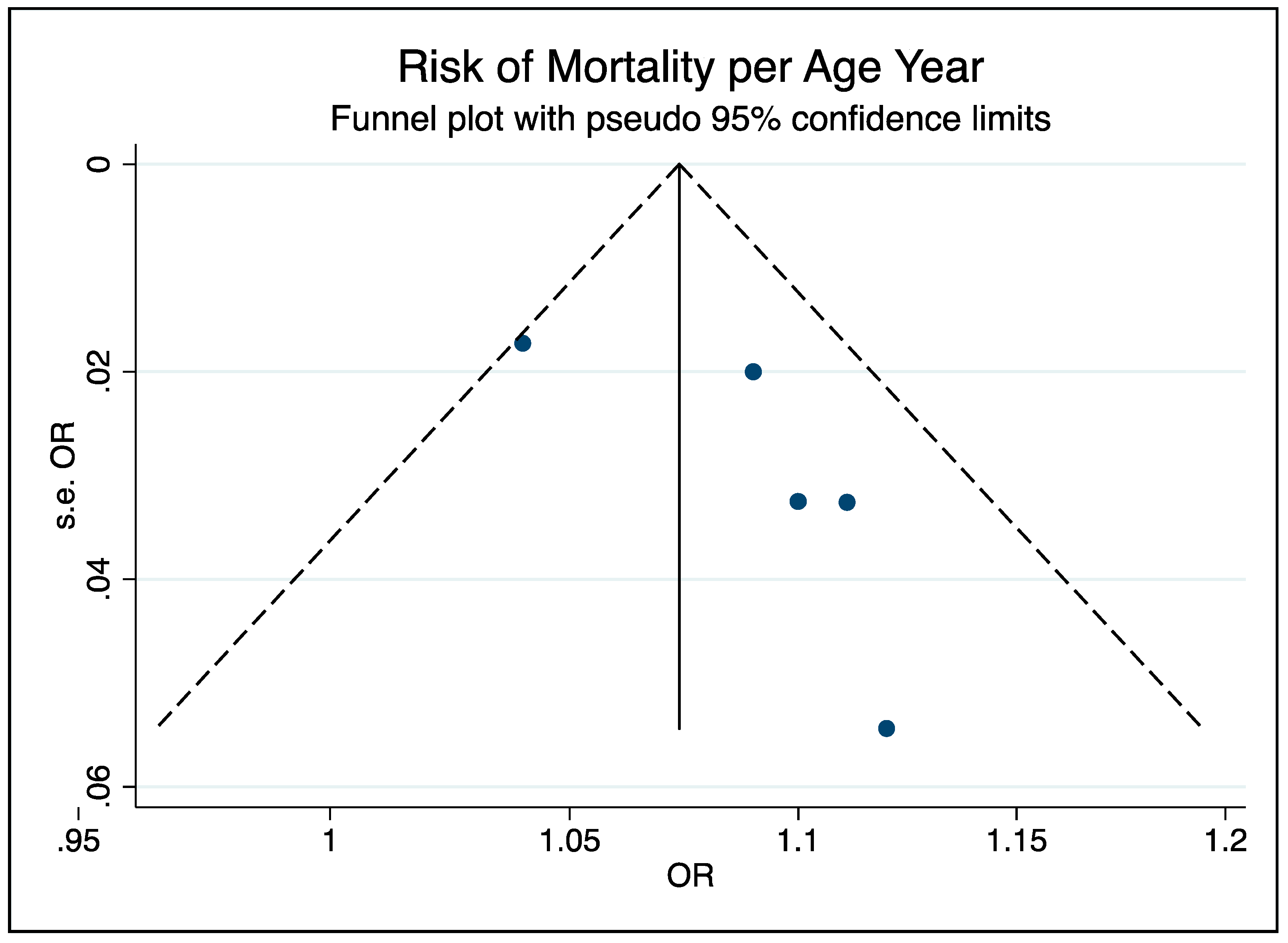
3.3.3. Meta-Analysis and Meta-Regression
3.4. Admission to ICU
Description of Studies
3.5. Effect of Age-Dependent Risk Factors Adjustment on Age-Related Risk Estimates
4. Discussion
4.1. Strengths and Limitations
4.2. Methodological Quality of the Included Studies
4.3. Implications for Public Policy
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Chen, T.; Dai, Z.; Mo, P.; Li, X.; Ma, Z.; Song, S.; Chen, X.; Luo, M.; Liang, K.; Gao, S.; et al. Clinical characteristics and outcomes of older patients with coronavirus disease 2019 (COVID-19) in Wuhan, China (2019): A single-centered, retrospective study. J. Gerontol. Ser. A 2020. [Google Scholar] [CrossRef]
- Chen, T.; Wu, D.; Chen, H.; Yan, W.; Yang, D.; Chen, G.; Ma, K.; Xu, D.; Yu, H.; Wang, H.; et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: Retrospective study. BMJ 2020, 368, m1091. [Google Scholar] [CrossRef] [PubMed]
- Dudley, J.P.; Lee, N.T. Disparities in Age-specific Morbidity and Mortality From SARS-CoV-2 in China and the Republic of Korea. Clin. Infect. Dis. 2020, 71, 863–865. [Google Scholar] [CrossRef] [PubMed]
- Verity, R.; Okell, L.C.; Dorigatti, I.; Winskill, P.; Whittaker, C.; Imai, N.; Cuomo-Dannenburg, G.; Thompson, H.; Walker, P.G.T.; Fu, H.; et al. Estimates of the severity of coronavirus disease 2019: A model-based analysis. Lancet Infect. Dis. 2020, 20, 669–677. [Google Scholar] [CrossRef]
- Robert Koch Institut (RKI). Informationen und Hilfestellungen für Personen mit Einem Höheren Risiko für einen Schweren COVID-19-Krankheitsverlauf. Available online: https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Risikogruppen.html (accessed on 1 June 2020).
- Niedersächsischer Kultusminister. Schule in Corona-Zeiten. Leitfaden für Schulleitungen Lehrkräfte und Pädagogische Fachkräfte an Schulen. Available online: http://www.mk.niedersachsen.de/download/154309/Leitfaden_fuer_Schulleitungen_Lehrkraefte_und_paedagogische_Fachkraefte_an_Schulen.pdf (accessed on 28 May 2020).
- Surveillances, V. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19)—China, 2020. China CDC Wkly. 2020, 2, 113–122. [Google Scholar]
- Lighter, J.; Phillips, M.; Hochman, S.; Sterling, S.; Johnson, D.; Francois, F.; Stachel, A. Obesity in patients younger than 60 years is a risk factor for Covid-19 hospital admission. Clin. Infect. Dis. 2020, 71, 896–897. [Google Scholar] [CrossRef]
- Ryan, D.H.; Ravussin, E.; Heymsfield, S. COVID 19 and the Patient with Obesity—The Editors Speak Out. Obesity 2020, 28, 847. [Google Scholar] [CrossRef]
- Vardavas, C.I.; Nikitara, K. COVID-19 and smoking: A systematic review of the evidence. Tob. Induc. Dis. 2020, 18, 20. [Google Scholar] [CrossRef]
- Ijaz, S.; Verbeek, J.; Seidler, A.; Lindbohm, M.-L.; Ojajärvi, A.; Orsini, N.; Costa, G.; Neuvonen, K. Night-shift work and breast cancer—A systematic review and meta-analysis. Scand. J. Work. Environ. Health 2013, 39, 431–447. [Google Scholar] [CrossRef]
- Scottish Intercollegiate Guidelines Network (SIGN). Methodology Checklist 3: Cohort Studies. Available online: http://www.sign.ac.uk (accessed on 28 May 2020).
- Critical Appraisal Skills Programme. CASP Cohort Study Checklist. Available online: https://casp-uk.net/casp-tools-checklists/ (accessed on 28 May 2020).
- StataCorp. Stata Statistical Software: Release 15; StataCorp LLC: College Station, TX, USA, 2015. [Google Scholar]
- Chen, C.; Chen, C.; Yan, J.T.; Zhou, N.; Zhao, J.P.; Wang, D.W. Analysis of myocardial injury in patients with COVID-19 and association between concomitant cardiovascular diseases and severity of COVID-19. Zhonghua Xin Xue Guan Bing Za Zhi 2020, 48, E008. [Google Scholar] [CrossRef]
- Chen, J.; Qi, T.; Liu, L.; Ling, Y.; Qian, Z.; Li, T.; Li, F.; Xu, Q.; Zhang, Y.; Xu, S.; et al. Clinical progression of patients with COVID-19 in Shanghai, China. J. Infect. 2020, 80, e1–e6. [Google Scholar] [CrossRef] [PubMed]
- Liang, W.; Liang, H.; Ou, L.; Chen, B.; Chen, A.; Li, C.; Li, Y.; Guan, W.; Sang, L.; Lu, J.; et al. Development and Validation of a Clinical Risk Score to Predict the Occurrence of Critical Illness in Hospitalized Patients With COVID-19. JAMA Intern. Med. 2020, 180, 1081. [Google Scholar] [CrossRef] [PubMed]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Wang, D.; Yin, Y.; Hu, C.; Liu, X.; Zhang, X.; Zhou, S.; Jian, M.; Xu, H.; Prowle, J.; Hu, B.; et al. Clinical course and outcome of 107 patients infected with the novel coronavirus, SARS-CoV-2, discharged from two hospitals in Wuhan, China. Crit. Care 2020, 24, 188. [Google Scholar] [CrossRef]
- Wang, K.; Zuo, P.; Liu, Y.; Zhang, M.; Zhao, X.; Xie, S.; Zhang, H.; Chen, X.; Liu, C. Clinical and laboratory predictors of in-hospital mortality in patients with COVID-19: A cohort study in Wuhan, China. Clin. Infect. Dis. 2020. [Google Scholar] [CrossRef]
- Shi, S.; Qin, M.; Cai, Y.; Liu, T.; Shen, B.; Yang, F.; Cao, S.; Liu, X.; Xiang, Y.; Zhao, Q.; et al. Characteristics and clinical significance of myocardial injury in patients with severe coronavirus disease 2019. Eur. Heart J. 2020, 41, 2070–2079. [Google Scholar] [CrossRef]
- Sun, H.; Ning, R.; Tao, Y.; Yu, C.; Deng, X.; Zhao, C.; Meng, S.; Tang, F.; Xu, D. Risk Factors for Mortality in 244 Older Adults With COVID-19 in Wuhan, China: A Retrospective Study. J. Am. Geriatr. Soc. 2020, 68, E19–E23. [Google Scholar] [CrossRef]
- Chen, R.; Liang, W.; Jiang, M.; Guan, W.; Zhan, C.; Wang, T.; Tang, C.; Sang, L.; Liu, J.; Ni, Z.; et al. Risk Factors of Fatal Outcome in Hospitalized Subjects With Coronavirus Disease 2019 From a Nationwide Analysis in China. Chest 2020, 158, 97–105. [Google Scholar] [CrossRef]
- Du, R.-H.; Liang, L.-R.; Yang, C.-Q.; Wang, W.; Cao, T.-Z.; Li, M.; Guo, G.-Y.; Du, J.; Zheng, C.-L.; Zhu, Q.; et al. Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: A prospective cohort study. Eur. Respir. J. 2020, 55, 2000524. [Google Scholar] [CrossRef]
- Meng, Y.; Wu, P.; Lu, W.; Liu, K.; Ma, K.; Huang, L.; Cai, J.; Zhang, H.; Qin, Y.; Sun, H.; et al. Sex-specific clinical characteristics and prognosis of coronavirus disease-19 infection in Wuhan, China: A retrospective study of 168 severe patients. PLoS Pathog. 2020, 16, e1008520. [Google Scholar] [CrossRef]
- Guan, W.-J.; Liang, W.-H.; Zhao, Y.; Liang, H.-R.; Chen, Z.-S.; Li, Y.-M.; Liu, X.-Q.; Chen, R.-C.; Tang, C.-L.; Wang, T.; et al. Comorbidity and its impact on 1590 patients with Covid-19 in China: A Nationwide Analysis. Eur. Respir. J. 2020, 55, 2000547. [Google Scholar] [CrossRef] [PubMed]
- Barnett, K.; Mercer, S.W.; Norbury, M.; Watt, G.; Wyke, S.; Guthrie, B. Epidemiology of multimorbidity and implications for health care, research, and medical education: A cross-sectional study. Lancet 2012, 380, 37–43. [Google Scholar] [CrossRef]
- Jimenez-Sotomayor, M.R.; Gomez-Moreno, C.; Soto-Perez-de-Celis, E. Coronavirus, Ageism, and Twitter: An Evaluation of Tweets about Older Adults and COVID-19. J. Am. Geriatr. Soc. 2020. [Google Scholar] [CrossRef] [PubMed]
- Morrow-Howell, N.; Galucia, N.; Swinford, E. Recovering from the COVID-19 Pandemic: A Focus on Older Adults. J. Aging Soc. Policy 2020, 32, 526–535. [Google Scholar] [CrossRef] [PubMed]
- Ayalon, L.; Chasteen, A.; Diehl, M.; Levy, B.; Neupert, S.D.; Rothermund, K.; Tesch-Römer, C.; Wahl, H.-W. Aging in Times of the COVID-19 Pandemic: Avoiding Ageism and Fostering Intergenerational Solidarity. J. Gerontol. Ser. B 2020. [Google Scholar] [CrossRef] [PubMed]
- Council of the European Union. Council Declaration on the European Year for Active Ageing and Solidarity between Generations (2012): The Way Forward; Council of the European Union: Brussels, Belgium, 2012; Available online: http://register.consilium.europa.eu/doc/srv?l=EN&f=ST%2017468%202012%20INIT (accessed on 30 June 2020).
- Röhr, S.; Müller, F.; Jung, F.; Apfelbacher, C.; Seidler, A.; Riedel-Heller, S.G. Psychosoziale Folgen von Quarantänemaßnahmen bei schwerwiegenden Coronavirus-Ausbrüchen: Ein Rapid Review. Psychiatr. Prax. 2020, 47, 179–189. [Google Scholar]

| Inclusion Criteria | Exclusion Criteria | |
|---|---|---|
| Population | General population infected with COVID-19 (both sexes, all ages) | All others |
| Intervention(s), exposure(s) | Age, in years | All other exposures which do not include age |
| Comparator/control | Persons from the same study population as the cases differing in age | Other populations which are not comparable to the cases in age |
| Outcomes | Disease severity due to infection with COVID-19: risk of hospitalization, admission to intensive care unit (ICU), intubation, death, other markers of severe disease due to COVID-19 Risks measured as adjusted hazard ratios, risk ratios, odds ratios | Other outcomes |
| Study design | cross-sectional, case-control, and cohort studies | Randomized controlled trials (RCTs), qualitative studies, ecological studies, case reports, experiments, comments, letters, editorials, congress abstracts, posters |
| Author, Year Country [Ref] | Study Design | Population Sampling | Age/Sex | Time Period of Study | Age Categories Used | Outcome Measurement |
|---|---|---|---|---|---|---|
| Guan, W. * 2020 China [26] | Retrospective cohort | COVID-19 laboratory-confirmed hospitalized patients (13.5% of cases as of 1/31/2020) from 575 hospitals (32% of all certified hospitals for COVID-19) and 31 areas across mainland China Complete random sampling could not be done n = 1590 | Mean age: 48.9 yrs. Male: 904 (57.3%) Female: 674 (42.7%) | 12/11/2019–01/31/2020 | Per year and <65 yrs. vs. ≥65 yrs. | Composite measure of admission to intensive care unit (ICU), invasive ventilation, or death |
| Chen, R. * 2020 China [23] | Retrospective cohort | Same population as above (n = 1590) | Same as above | Unknown–01/31/2020 | 65–74 yrs. vs. <65 yrs. and ≥75 yrs. vs. <65 yrs. | Death |
| Liang, W. * 2020 China [17] | Retrospective cohort | Same population as above (n = 1590) | Same as above | 11/21/2019–01/31/2020 | Per year | Composite measure of admission to intensive care unit (ICU), invasive ventilation, or death |
| Du, R.-H. * 2020 China [24] | Prospective cohort | Patients hospitalized at Wuhan Pulmonary Hospital, Wuhan City (most likely a sub-set of Guan et al. 2020′s population) All patients included n = 179 | Mean age: 57.6 yrs. SD: 13.7 yrs. Male: 97 (54.2%) Female: 82 (45.8%) | 12/25/2019–02/07/2020 | ≥65 yrs. vs. <65 yrs. | Death |
| Zhou, F. * 2020 China [18] | Retrospective cohort | Two cohorts of adult patients (≥18 yrs.) from Jinyintan Hospital and Wuhan Pulmonary Hospital (Wihan, China). n = 191 Jinyintan Hospital: n = 135 Wuhan Pulmonary Hospital: n = 56 | Median age: 56.0 yrs. IQR: 46.0–67.0 yrs. Male: 119 (62%) Female: 72 (38%) | 12/29/2019–01/31/2020 | Per year | Death |
| Wang, D. 2020 China [19] | Retrospective cohort | Patients hospitalized at Zhongnan Hospital of Wuhan University and Xishui Hospital, Hubei Province n = 107 patients | Median age: 51 yrs. Range: 19–92 yrs. Male: 57 (53.3%) Female: 50 (46.7%) | unknown–02/10/2020 | Per year | Death |
| Wang, K. 2020 China [20] | Retrospective cohort | Participants diagnosed with COVID-19 and hospitalized in First People’s Hospital of Jiangxia District in Wuhan n = 305 | Mean age: 47.8 yrs. SD: 15.1 yrs. Male: 142 (46.6%) Female: 163 (53.4%) | 01/07/2020–02/11/2020 | Per year | Death |
| Chen, J. 2020 China [16] | Retrospective cohort | Patients at Shanghai Public Health Clinical Center (SPHCC). n = 249 | Median age: 51 yrs. IQR: 36–64 yrs. Male: 126 (50.6%) Female: 123 (49.4%) | 01/20/2020–02/25/2020 | per year | Admission to ICU |
| Chen, C. ** 2020 China [15] | Retrospective cohort | Patients admitted to fever ward in Tongji Hospital, Tongji Medical College in Huazhong University of Science and Technology n = 150 | Median age: Non-critical group: 57.1 ± 15.6 yrs. Critical group: 68.5 ± 13.6 yrs. Male: 84 (56%) Female: 66 (44%) | January to February 2020 | per year | Composite measure of critical and severe coronavirus pneumonia (with one of the following conditions): respiratory failure and mechanical ventilation; shock; combined with failure of other organs should be treated in the ICU |
| Meng, Y. ** 2020 China [25] | Retrospective cohort | Patients hospitalized at Tongji Hospital in Wuhan, China n = 168 | Mean age: 56.7 yrs. SD: 15.1 yrs. Male: 86 (51.2%) Female: 82 (48.8%) | Hospitalized 01/16/2020–02/04/2020 and monitored up to 03/24/202 | 0–59 yrs. 60–79 yrs. ≥80 yrs. | Critically ill cases defined as patients who met any of the following criteria: developed respiratory failure requiring intubation; presented with shock; developed other organ failure or were admitted to ICU |
| Shi S. 2020 China [21] | Retrospective cohort | All consecutive patients admitted to Renmin Hospital of Wuhan University with lab-confirmed COVID-19 n = 671 | Median age: 63 yrs. IQR: 50–72 yrs. Male: 322 (48.0%) Female: 349 (52.0%) | 01/01/2020–02/23/2020 | Per year | Death |
| Sun, H. 2020 China [22] | Retrospective cohort | Participants identified from inpatients of the Sino-French New City Branch of Tongji hospitals with 1085 beds for treating Covid-19 designated by the government Participants 60 yrs. and older with definitive outcomes by March 5, 2020 were enrolled n = 244 | Discharged: Median age: 67 yrs. Range: 64–72 yrs. Died: Median age: 72 yrs. Range: 66–78 yrs. Male: 133 (54.5%) Female: 111 (45.5%) | 01/29/2020–03/05/2020 | Per year | Death |
| Author, Year [Ref] | Confounders/ Age-Dependent Risk Factors Used in the Model In RoB/Meta-Analysis (Yes/No) Number of Age-Dependent Risk Factors for Meta-Regression | Type of Analysis Number of Cases/Number of Non-Cases | Results |
|---|---|---|---|
| Guan, W.* 2020 [26] | Malignancy, COPD, diabetes, hypertension, smoking Comorbidity, defined as: hypertension, other cardiovascular disease, cerebrovascular diseases, diabetes, hepatitis B infections, COPD, malignancy, immune deficiency In meta-analysis: yes Number of age-dependent risk factors for meta-regression: 4 (malignancy, COPD, diabetes, hypertension) | Cox proportional hazards regression cases = 131 (8.3%): died: n = 50 ICU: n = 99 Invasive ventilation: n = 50 Non-cases: 1459 (91.7%) | Association of age (per yr.) and severe outcome: Unadjusted OR: 1.051 95% CI (1.039−1.064) OR adjusted for malignancy: 1.050, 95% CI (1.037−1.062) OR adj. for malignancy, COPD: 1.045, 95% CI (1.032−2.058) OR adj. for malignancy, COPD, diabetes: 1.041, 95% CI (1.027−1.055) OR adj. for malignancy, COPD, diabetes, hypertension: 1.036, 95% CI (1.022−1.051) OR adj. for malignancy, COPD, diabetes, hypertension, smoking: 1.036, 95% CI (1.022−1.050 Number of comorbidities and severe outcome by age: 1 comorbidity: <65 yrs.: HR 2.210, 95% CI (1.234−3.960) ≥65 yrs.: HR 1.801, 95% CI (0.912−3.554) ≥2 comorbidities: 65 yrs.: HR 3.332, 95% CI (1.557−7.132) ≥65 yrs.: HR 2.724, 95% CI (1.409−5.265) Smoking (yes vs. no) 65 yrs.: HR 1.495, 95% CI (0.641−3.488) ≥65 yrs.: HR 1.534, 95% CI (0.813−2.892) |
| Liang, W.* 2020 [17] | X-ray abnormality, hemoptysis, dyspnea unconsciousness, number of comorbidities, cancer history, neutrophil to lymphocyte ratio, lactate dehydrogenase, direct bilirubin In meta-analysis: no (same population as Guan et al. 2020 [26]) | Logistic regression cases = 131 (8.3%) Non-cases = 1459 (91.7%) | Association of age (per yr.) and severe outcome: Adj. OR: 1.03, 95% CI (1.01−1.05) |
| Chen, C.** 2020 [15] | Sex, increased NT-proBNP, increased cTnI, increased hs_CRP, increased blood creatinine, hypertension, diabetes, history of previous coronary heart disease In meta-analysis: yes Number of age-dependent risk factors for meta-regression: 4 (NT-proBNP increased, hypertension, diabetes, history of previous coronary heart disease) | Logistic regression cases = 24 Non-cases = 126 | Association of age (per yr.) and severe coronavirus pneumonia: Unadj. OR: 1.056, 95% CI (1.020−1.092) Adj. OR: 1.019, 95% CI (0.963−1.077) |
| Meng, Y.** 2020 [25] | Comorbidities: hypertension, diabetes, cardiovascular disease, chronic kidney disease, cerebrovascular disease, COPD, malignancy In meta-analysis: no (same or sub-population as Chen et al. 2020 [15]) | Logistic regression Cases = Died: 17 (8.9%) Critically ill: 48 (28.6%) Non-cases = 136 (81%) | Association of age and severe outcome: Women and men Age 0−59 yrs.: Ref. Age 60−79 yrs.: Unadj. OR: 5 (2−10) † Adj. OR: 3 (0.9−8) † ≥80 yrs.: Unadj. OR: 10.968 (3.005−40.037) Adj. OR: 10 (2−40) † Men: Age 0−59 yrs.: Ref ≥80 yrs.: Unadj. OR: 10 (1−50) † Adj. OR: 9.333 (1.618−53.845) Women: Age 0−59 yrs.: Ref ≥80 yrs.: Unadj. OR: 20 (2−200) † Adj. OR: 10.161 (0.911−113.346) |
| Author, Year [Ref] | Confounders/ Age-Dependent Risk Factors Used in Model In RoB/Meta-Analysis (Yes/No) Number of Age-Dependent Risk Factors for Meta-Regression | Type of Analysis Number of Cases/Number of Non-Cases | Results |
|---|---|---|---|
| Zhou, F. * 2020 [18] | Coronary heart disease, Sequential Organ Failure Assessment (SOFA) score, lymphocite count, D-dimer In meta-analysis: yes Number of age-dependent risk factors for meta-regression: 1 (coronary heart disease) | Logistic regression Only significant factors from univariate taken in multivariate model Cases = 54 (28.3%) Non-cases = 137 (71.7%) | Association between age (per yr.) and in-hospital mortality: Unadj. OR: 1.14, 95% CI (1.09−1.18) Adj. OR: 1.10, 95% CI (1.03−1.17)) |
| Du, R.H. * 2020 [24] | Cardiovascular or cerebrovascular diseases, CD3 + CD8+ T cells ≤ 75 cell/ug, Cardiac troponin I ≥ 0.05 ng/mL In meta-analysis: no (same or sub-population as Zhou et al. 2020 [18] and larger age categories used in analysis) | Logistic regression Cases = 21 Non-cases = 158 | Association between age and mortality: Unadj. OR 0−49 yrs.: Ref. 50−64 yrs.: 2.673, 95% CI (0.859−8.318) ≥65 yrs.: 9.740, 95% CI (3.113−30.476) Adj. OR < 65 yrs.: Ref ≥65 yrs.: 3.765 (1.146–17.394) |
| Chen, R. * 2020 [23] | Coronary heart disease (CHD), cardiovascular disease (CVD), dyspnea, PCT > 0.5 ng/mL, AST > 40U/L, TBIL, Cr In meta-analysis: no (same or sub-population as Zhou et al. 2020 [18] and large age categories used in analysis) | Cox regression Cases = 50 | Association between age and mortality: Age ≥ 75 yrs. vs. <65 yrs.: Adj. HR: 7.86 (95% CI: 2.44–25.35) Age 65–74 yrs. vs. <65 yrs. Adj. HR: 3.43 (95% CI: 1.24–9.5) |
| Wang, D. 2020 [19] | Sex, hypertension, cardiovascular disease, creatinine concentration In meta-analysis: yes Number of age-dependent risk factors for meta-regression: 2 (hypertension, cardiovascular disease) | Logistic regression Cases = 19 Non-cases = 88 | Association between age (per yr.) and mortality: Unadj. OR: 1.102, 95% CI (1.054−1.152) Adj. OR: 1.111, 95% CI (1.042−1.184) |
| Wang, K. 2020 [20] | Hypertension, fever In meta-analysis: yes Number of age-dependent risk factors for meta-regression: 1 (hypertension) | Logistic regression Cases = 22 (7.2%) Non-cases = 283 (92.8%) | Association between age (per yr.) and mortality: Adj. OR: 1.09, 95% CI (1.054−1.14) |
| Shi S. 2020 [21] | Model 1: Sex, hypertension, diabetes, coronary heart disease, chronic renal disease, cerebrovascular disease, and following biomarkers as categorical variables: procalcitomin, c-reactive protein, CK-MB, MYO, cTnI, NT-proBNP Model 1: Sex, hypertension, diabetes, coronary heart disease, chronic renal disease, cerebrovascular disease, and following biomarkers as continuous variables: procalcitomin, c-reactive protein, CK-MB, MYO, cTnI, NT-proBNP In meta-analysis: yes Number of age-dependent risk factors for meta-regression: 5 (hypertension, diabetes, coronary heart disease/cerebrovascular disease, chronic renal disease, NT-proBNP) | Cox regression Cases = 62 Non-cases = 609 | Association between age (per yr.) and in-hospital mortality: Model 1 Adj. OR: 1.01, 95% CI (0.98−1.05) Model 2 Adj. OR: 1.04, 95% CI (1.00−1.07) |
| Sun, H. 2020 [22] | Sex, SpO2, heart rate, respiratory rate, consciousness disorders, hypertension, previous respiratory diseases, WBC count, LYM count, NT-prBNP, PCT, hs-TnI, D-dimer, ALT, AST, creatinine, eGFR, hs-CRP In meta-analysis: yes Number of age-dependent risk factors for meta-regression: 3 (hypertension, NT-proBNP, hs-Tnl) | Logistic regression Cases = 122 Non-cases = 123 | Association between age (per yr.) and mortality: Adj. OR: 1.12, 95% CI (1.01−1.25) |
| Author, Year [Ref] | Confounders/ Age-Dependent Risk Factors Used in the Model In RoB/Meta-Analysis (Yes/No) Number of Age-Dependent Risk Factors for Meta-Regression | Type of Analysis Number of Cases/Number of Non-Cases | Results |
|---|---|---|---|
| Chen, J. 2020 [16] | Sex, comorbidity (cardiovascular and cerebrovascular diseases, endocrine system diseases, digestive system diseases, respiratory system diseases, chronic hepatitis B, malignant tumor), white blood cells, lymphocytes, C-reactive protein, albumin, lactate dehydrogenase, estimated glomerular filtration rate, CD4 T cell counts In meta-analysis: no (insufficient studies) | Logistic regression Cases = 22 Non-cases = 227 | Association between age (per yr.) and risk of admission to ICU: Unadj. OR: 1.08, 95% CI (1.04−1.13) Adj. OR: 1.06, 95% CI (1.00−1.12) |
| Number of Age-Related Risk Factors | RRage Disease Severity † | RRage Death ‡ |
|---|---|---|
| 0 | 1.052 | 1.134 |
| 1 | 1.047 | 1.109 |
| 2 | 1.043 | 1.084 |
| 3 | 1.039 | 1.060 |
| 4 | 1.035 | 1.037 |
| 5 | 1.031 * | 1.014 |
| 6 | 1.027 * | 0.992 * |
| Component | Model Estimate (95% CI) |
|---|---|
| Intercept | 1.139 (1.125, 1.153) |
| β (risk factor) | 0.981 (0.966, 0.998) |
| β (presence of over-adjustment) | 0.979 (0.923, 1.039) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Romero Starke, K.; Petereit-Haack, G.; Schubert, M.; Kämpf, D.; Schliebner, A.; Hegewald, J.; Seidler, A. The Age-Related Risk of Severe Outcomes Due to COVID-19 Infection: A Rapid Review, Meta-Analysis, and Meta-Regression. Int. J. Environ. Res. Public Health 2020, 17, 5974. https://doi.org/10.3390/ijerph17165974
Romero Starke K, Petereit-Haack G, Schubert M, Kämpf D, Schliebner A, Hegewald J, Seidler A. The Age-Related Risk of Severe Outcomes Due to COVID-19 Infection: A Rapid Review, Meta-Analysis, and Meta-Regression. International Journal of Environmental Research and Public Health. 2020; 17(16):5974. https://doi.org/10.3390/ijerph17165974
Chicago/Turabian StyleRomero Starke, Karla, Gabriela Petereit-Haack, Melanie Schubert, Daniel Kämpf, Alexandra Schliebner, Janice Hegewald, and Andreas Seidler. 2020. "The Age-Related Risk of Severe Outcomes Due to COVID-19 Infection: A Rapid Review, Meta-Analysis, and Meta-Regression" International Journal of Environmental Research and Public Health 17, no. 16: 5974. https://doi.org/10.3390/ijerph17165974
APA StyleRomero Starke, K., Petereit-Haack, G., Schubert, M., Kämpf, D., Schliebner, A., Hegewald, J., & Seidler, A. (2020). The Age-Related Risk of Severe Outcomes Due to COVID-19 Infection: A Rapid Review, Meta-Analysis, and Meta-Regression. International Journal of Environmental Research and Public Health, 17(16), 5974. https://doi.org/10.3390/ijerph17165974







