Nutrition Labeling Usage Influences Blood Markers in Body-Size Self-Conscious Individuals: The Korean National Health and Nutrition Examination Survey (KNHANES) 2013–2018
Abstract
1. Introduction
2. Materials and Methods
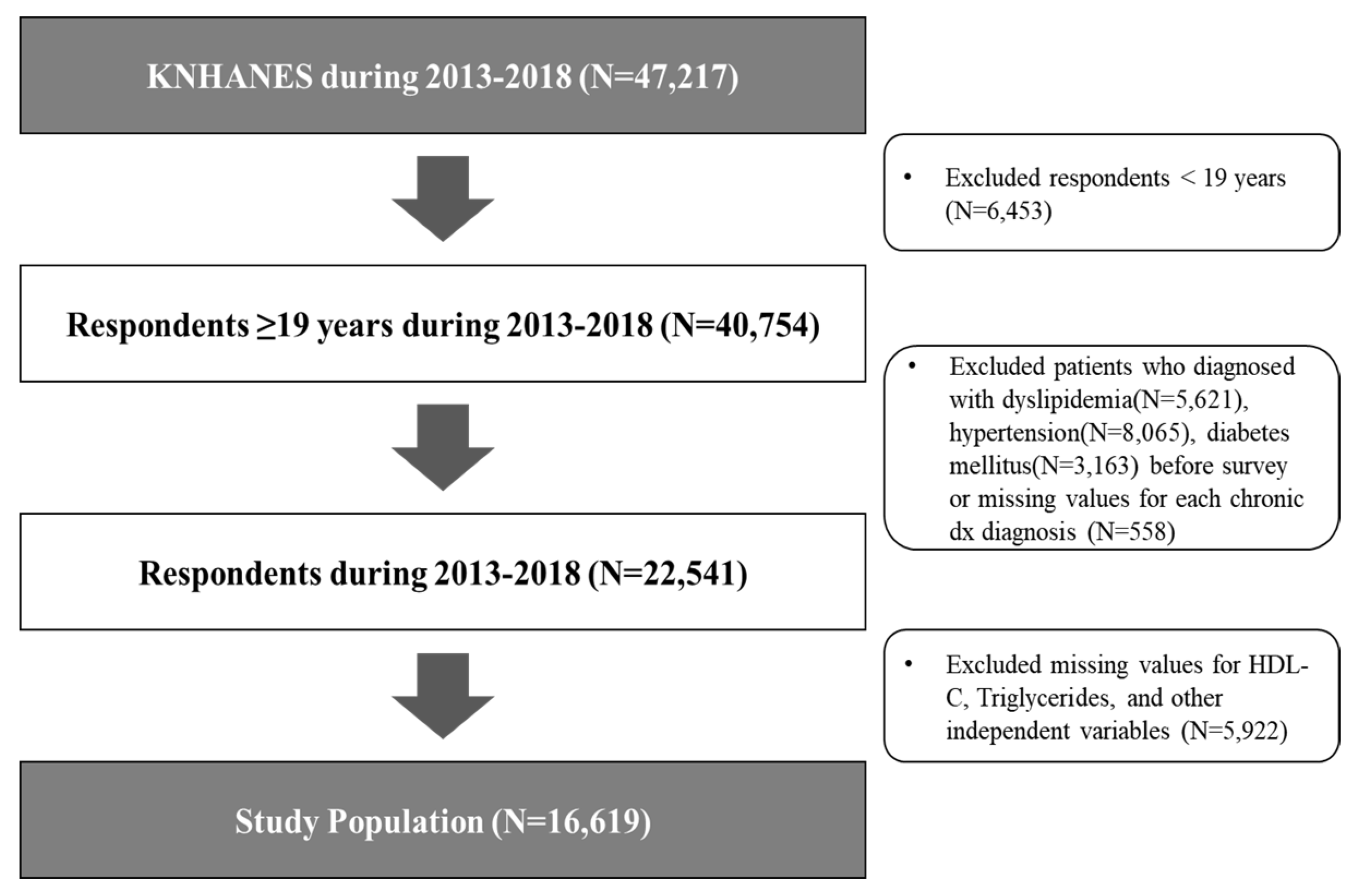
2.1. Participants
2.2. Measurements
2.2.1. Outcome Variables
Levels of HDL-C and TG
2.2.2. Independent Variables
2.2.3. Body-Size Perception
2.3. Statistical Analysis
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Johnson, J.D.; Case, D.O. Health Information Seeking; Peter Lang Publishing: New York, NY, USA, 2012. [Google Scholar]
- Shim, M.; Kelly, B.; Hornik, R. Cancer information scanning and seeking behavior is associated with knowledge, lifestyle choices, and screening. J. Health Commun. 2006, 11 (Suppl. 001), 157–172. [Google Scholar] [CrossRef] [PubMed]
- Marlow, L.A.; Waller, J.; Wardle, J. The Impact of human papillomavirus information on perceived risk of cervical cancer. Cancer Epidemiol. Biomark. 2009, 18, 373–376. [Google Scholar] [CrossRef] [PubMed]
- Egan, B.M.; Lackland, D.T.; Cutler, N.E. Awareness, knowledge, and attitudes of older Americans about high blood pressure: Implications for health care policy, education, and research. Arch. Intern. Med. 2003, 163, 681–687. [Google Scholar] [CrossRef] [PubMed]
- Yap, A.F.; Thirumoorthy, T.; Kwan, Y.H. Systematic review of the barriers affecting medication adherence in older adults. Geriatr. Gerontol. Int. 2015, 16, 1093–1101. [Google Scholar] [CrossRef]
- Kye, S.Y.; Kwon, J.H.; Kim, Y.C.; Shim, M.; Kim, J.H.; Cho, H.; Jung, K.W.; Park, K. Cancer risk factors in Korean news media: A content analysis. Asian Pac. J. Cancer Prev. 2015, 16, 731–736. [Google Scholar] [CrossRef]
- Campos, S.; Doxey, J.; Hammond, D. Nutrition labels on pre-packaged foods: A systematic review. Public Health Nutr. 2011, 14, 1496–1506. [Google Scholar] [CrossRef]
- Liu, R.; Hoefkens, C.; Verbeke, W. Chinese consumers’ understanding and use of a food nutrition label and their determinants. Food Qual. Prefer. 2015, 41, 103–111. [Google Scholar] [CrossRef]
- Han, K.T.; Kim, S.J.; Kim, D.J.; Kim, S.J. Does the active use of nutrition labeling reduce the risk of diabetes mellitus? Results of insulin resistance using Korean National Health and Nutrition Examination Survey. Prim. Care Diabetes 2018, 12, 445–452. [Google Scholar] [CrossRef]
- Hoefkens, C.; Veettil, P.C.; Huylenbroeck, G.V.; Camp, J.V.; Verbeke, W. What nutrition label to use in a catering environment? A discrete choice experiment. Food Policy 2012, 37, 741–750. [Google Scholar] [CrossRef]
- Kim, J.Y.; Kweon, K.H.; Kim, M.J.; Park, E.-C.; Jang, S.-Y.; Kim, W.; Han, K.-T. Is nutritional labeling associated with individual health? The effects of labeling-based awareness on dyslipidemia risk in a South Korean population. Nutr. J. 2015, 15. [Google Scholar] [CrossRef]
- Satia, J.A.; Galanko, J.A.; Neuhouser, M.L. Food nutrition label use is associated with demographic, behavioral, and psychosocial factors and dietary intake among African Americans in North Carolina. J. Am. Diet. Assoc. 2005, 105, 392–403. [Google Scholar] [CrossRef] [PubMed]
- Yoo, J.S.; Han, K.T.; Chung, S.H.; Park, E.C. Association between awareness of nutrition labeling and high-density lipoprotein cholesterol concentration in cancer survivors and the general population: The Korean National Health and Nutrition Examination Survey (KNHANES) 2010-2016. BMC Cancer 2019, 19, 16. [Google Scholar] [CrossRef] [PubMed]
- Glanz, K.; Rimer, B.K.; Viswanath, K. Health Behavior and Health Education: Theory, Research, and Practice; Jossey Bass: San Francisco, CA, USA, 2008. [Google Scholar]
- Hawkins, R.P.; Kreuter, M.; Resnicow, K.; Fishbein, M.; Dijkstra, A. Understanding tailoring in communicating about health. Health Educ. Res. 2008, 23, 454–466. [Google Scholar] [CrossRef] [PubMed]
- Op den Akker, H.; Cabrita, M.; Op den Akker, R.; Jones, V.M.; Hermens, H.J. Tailored motivational message generation: A model and practical framework for real-time physical activity coaching. J. Biomed. Inform. 2015, 55, 104–115. [Google Scholar] [CrossRef] [PubMed]
- Grogan, S. Body image and health: Contemporary perspectives. J. Health Psychol. 2006, 11, 523–530. [Google Scholar] [CrossRef]
- Joh, H.K.; Oh, J.; Lee, H.J.; Kawachi, I. Gender and socioeconomic status in relation to weight perception and weight control behavior in Korean adults. Obes. Facts 2013, 6, 17–27. [Google Scholar] [CrossRef]
- Grogan, S. Body Image: Understanding Body Dissatisfaction in Men, Women and Children; Routledge: London, UK, 2016. [Google Scholar] [CrossRef]
- Seo, J.; Ma, H.; Kim, S.; Kim, J.; Shin, M.; Yang, Y.J. Effects of the difference between actual body condition and body image perception on nutrient intake, weight control and mental health in Korean adults: Based on the 5th Korea National Health and Nutrition Examination Survey. J. Nutr. Health 2016, 49, 153. [Google Scholar] [CrossRef]
- Rawana, J.S.; Morgan, A.S. Trajectories of depressive symptoms from adolescence to young adulthood: The role of self-esteem and body-related predictors. J. Youth Adolesc. 2014, 43, 597–611. [Google Scholar] [CrossRef]
- Wilson, R.E.; Marshall, R.D.; Murakami, J.M.; Latner, J.D. Brief non-dieting intervention increases intuitive eating and reduces dieting intention, body image dissatisfaction, and anti-fat attitudes: A randomized controlled trial. Appetite 2020, 148, 104556. [Google Scholar] [CrossRef]
- Cernelic-Bizjak, M. Changes in body image during a 6-month lifestyle behaviour intervention in a sample of overweight and obese individuals. J. Bodyw. Mov. Ther. 2019, 23, 515–520. [Google Scholar] [CrossRef]
- Genest, J.; McPherson, R.; Frohlich, J.; Anderson, T.; Campbell, N.; Carpentier, A.; Couture, P.; Dufour, R.; Fodor, G.; Francis, G.A.; et al. 2009 Canadian Cardiovascular Society/Canadian guidelines for the diagnosis and treatment of dyslipidemia and prevention of cardiovascular disease in the adult–2009 recommendations. Can. J. Cardiol. 2009, 25, 567–579. [Google Scholar] [CrossRef]
- Rashid, S.; Genest, J. Effect of obesity on high-density lipoprotein metabolism. Obesity 2007, 15, 2875–2888. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health and Welfare. The Korean National Health and Nutrition Examination Survey (KNHANES) 2013–2018, Versions 6 and 7. Available online: http://knhanes.cdc.go.kr (accessed on 15 June 2020).
- Kweon, S.; Kim, Y.; Jang, M.J.; Kim, Y.; Kim, K.; Choi, S.; Chun, C.; Khang, Y.-H.; Oh, K. Data resource profile: The Korea National Health and Nutrition Examination Survey (KNHANES). Int. J. Epidemiol. 2014, 43, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Santo, L.R.E.; Faria, T.O.; Silva, C.S.O.; Xavier, L.A.; Reis, V.C.; Mota, G.A.; Silveira, M.F.; Mill, J.G.; Baldo, M.P. Socioeconomic status and education level are associated with dyslipidemia in adults not taking lipid-lowering medication: A population-based study. Int. Health 2019. [Google Scholar] [CrossRef]
- Shin, J.; Cho, K.H.; Choi, Y.; Lee, S.G.; Park, E.C.; Jang, S.I. Combined effect of individual and neighborhood socioeconomic status on mortality in patients with newly diagnosed dyslipidemia: A nationwide Korean cohort study from 2002 to 2013. Nutr. Metab. Cardiovasc. Dis. 2016, 26, 207–215. [Google Scholar] [CrossRef]
- Choi, M.K.; Lee, Y.K.; Bae, Y.J. Association of eating out frequency with the risks of obesity, diabetes, and dyslipidemia among Korean adults. Curr. Dev. Nutr. 2019. [Google Scholar] [CrossRef]
- Jung, C.H.; Park, J.S.; Lee, W.Y.; Kim, S.W. Effects of smoking, alcohol, exercise, level of education, and family history on the metabolic syndrome in Korean adults. Korean J. Med. 2002, 63, 649–659. Available online: https://www.koreamed.org/SearchBasic.php?RID=1007KJM/2002.63.6.649&DT=1 (accessed on 7 August 2020).
- Seo, M.H.; Lee, W.Y.; Kim, S.S.; Kang, J.H.; Kang, J.H.; Kim, K.K.; Kim, B.-Y.; Kim, Y.-H.; Kim, W.-J.; Kim, E.M.; et al. 2018 Korean Society for the Study of Obesity Guideline for the Management of Obesity in Korea. J. Obes. Metab. Syndr. 2019, 28, 40–45. [Google Scholar] [CrossRef]
- Chung, S.J.; Kim, J.H.; Lee, J.S.; Lee, D.H.; Kim, S.H.; Yu, C.H. A suggestion to develop a nutrition policy on food and nutrition labeling and education systems for fast food and carbonated soft drinks in Korea. Korean J. Nutr. 2004, 37, 394–405. [Google Scholar]
- Chisuwa, N.; O’Dea, J.A. Body image and eating disorders amongst Japanese adolescents. A review of the literature. Appetite 2010, 54, 5–15. [Google Scholar] [CrossRef]
- Wal, J.S.V.; Thomas, N. Predictors of body image dissatisfaction and disturbed eating attitudes and behaviors in African American and Hispanic girls. Eat. Behav. 2004, 5, 291–301. [Google Scholar] [CrossRef]
- Parekh, S.; Vandelanotte, C.; King, D.; Boyle, F.M. Improving diet, physical activity and other lifestyle behaviours using computer-tailored advice in general practice: A randomised controlled trial. Int. J. Behav. Nutr. Phys. 2012, 9, 108. [Google Scholar] [CrossRef] [PubMed]
- Krebs, P.; Prochaska, J.O.; Rossi, J.S. A meta-analysis of computer-tailored interventions for health behavior change. Prev. Med. 2010, 51, 214–221. [Google Scholar] [CrossRef] [PubMed]
- Elbert, S.P.; Dijkstra, A.; Oenema, A. A mobile phone app intervention targeting fruit and vegetable consumption: The efficacy of textual and auditory tailored health information tested in a randomized controlled trial. J. Med. Internet Res 2016, 18, e147. [Google Scholar] [CrossRef] [PubMed]
| Variables | Study Population | Male | Female | |||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| Active use of nutrition labeling | ||||||
| Check and make dependent purchase decisions | 4308 | 26.04 | 1052 | 16.81 | 3256 | 35.06 |
| Not actively using | 12,311 | 73.96 | 6075 | 83.19 | 6236 | 64.94 |
| Sex | ||||||
| Male | 7127 | 49.45 | 7127 | 100.00 | ||
| Female | 9492 | 50.55 | 9492 | 100.00 | ||
| Age (years) | ||||||
| <20 | 264 | 1.94 | 140 | 2.13 | 124 | 1.76 |
| <30 | 2735 | 22.67 | 1211 | 24.13 | 1524 | 21.24 |
| <40 | 4058 | 25.42 | 1591 | 24.45 | 2467 | 26.36 |
| <50 | 4024 | 24.02 | 1505 | 21.85 | 2519 | 26.15 |
| <60 | 2942 | 16.34 | 1233 | 16.40 | 1709 | 16.29 |
| <70 | 1669 | 6.52 | 874 | 7.28 | 795 | 5.77 |
| 70+ | 927 | 3.09 | 573 | 3.77 | 354 | 2.42 |
| Educational level | ||||||
| High school or below | 7294 | 39.25 | 2958 | 35.67 | 4336 | 42.75 |
| Bachelor’s degree | 8325 | 54.58 | 3668 | 57.21 | 4657 | 52.01 |
| Master’s degree and above | 1000 | 6.17 | 501 | 7.12 | 499 | 5.24 |
| Economic status | ||||||
| Employed | 5556 | 31.87 | 1587 | 21.38 | 3969 | 42.12 |
| Unemployed | 11,063 | 68.13 | 5540 | 78.62 | 5523 | 57.88 |
| Household income | ||||||
| Low | 3844 | 24.05 | 1638 | 23.76 | 2206 | 24.33 |
| Mid-low | 4200 | 25.43 | 1819 | 25.95 | 2381 | 24.91 |
| Mid-high | 4282 | 25.48 | 1848 | 25.42 | 2434 | 25.54 |
| High | 4293 | 25.04 | 1822 | 24.87 | 2471 | 25.21 |
| Marital status | ||||||
| Single | 3776 | 29.69 | 1941 | 35.32 | 1835 | 24.19 |
| Separated/divorced/bereavement | 1261 | 5.93 | 346 | 3.86 | 915 | 7.95 |
| Married | 11,582 | 64.38 | 4840 | 60.83 | 6742 | 67.86 |
| Residence Area | ||||||
| Metropolitan | 9960 | 60.29 | 4178 | 59.11 | 5782 | 61.45 |
| Others | 6659 | 39.71 | 2949 | 40.89 | 3710 | 38.55 |
| Perceived health status | ||||||
| Good | 14,484 | 87.43 | 6341 | 89.09 | 8143 | 85.80 |
| Bad | 2135 | 12.58 | 786 | 10.91 | 1349 | 14.20 |
| Stress awareness | ||||||
| High | 4524 | 28.36 | 1762 | 26.24 | 2762 | 30.43 |
| Low | 12,095 | 71.64 | 5365 | 73.76 | 6730 | 69.57 |
| Alcohol intake | ||||||
| Less than 1 time per month | 6176 | 34.18 | 1739 | 23.41 | 4437 | 44.72 |
| 1–3 times per week | 9402 | 59.6 | 4605 | 66.83 | 4797 | 52.53 |
| More than 4 times per week | 1041 | 6.21 | 783 | 9.76 | 258 | 2.75 |
| Smoking status | ||||||
| Smoker | 3305 | 23.16 | 2743 | 40.03 | 562 | 6.64 |
| Ex-smoker | 3256 | 19.77 | 2607 | 32.76 | 649 | 7.06 |
| Non-smoker | 10,058 | 57.08 | 1777 | 27.21 | 8281 | 86.30 |
| Aerobic exercise habits | ||||||
| Yes | 7539 | 48.34 | 3432 | 48.56 | 4107 | 45.31 |
| No | 9080 | 51.66 | 3695 | 51.44 | 5385 | 54.69 |
| Walking for more than 10 min | ||||||
| Few | 2515 | 14.27 | 1157 | 15.24 | 1358 | 13.32 |
| 1–4 days per week | 5133 | 30.18 | 2109 | 28.97 | 3024 | 31.36 |
| 5–7 days per week | 8971 | 55.55 | 3861 | 55.80 | 5110 | 55.31 |
| Frequency of eat out | ||||||
| More than 4 times per week | 9762 | 63.83 | 5111 | 76.38 | 4841 | 48.45 |
| Less than 3 times per week | 6857 | 36.17 | 2016 | 23.62 | 4651 | 51.55 |
| Family history of hyperlipidemia | ||||||
| Yes | 1158 | 7.01 | 368 | 5.63 | 790 | 8.36 |
| No | 15,461 | 92.99 | 6759 | 94.37 | 8702 | 91.64 |
| Year | ||||||
| 2013 | 2715 | 15.94 | 1173 | 16.18 | 1542 | 15.69 |
| 2014 | 2491 | 15.57 | 1034 | 15.53 | 1457 | 15.60 |
| 2015 | 2564 | 16.52 | 1126 | 16.54 | 1438 | 16.49 |
| 2016 | 2854 | 16.55 | 1177 | 16.17 | 1677 | 16.94 |
| 2017 | 2917 | 17.17 | 1263 | 16.94 | 1654 | 17.39 |
| 2018 | 3078 | 18.25 | 1354 | 18.64 | 1724 | 17.88 |
| Body-size perception | ||||||
| Misperception (over) | 3051 | 18.53 | 1822 | 24.30 | 824 | 8.07 |
| Misperception (under) | 2646 | 15.11 | 613 | 9.11 | 2438 | 26.53 |
| Healthy perception | 10,922 | 66.36 | 4692 | 66.60 | 6230 | 65.40 |
| Total | 16,619 | 100.00 | 7127 | 100.00 | 9492 | 100.00 |
| Variables | Study Population | Male | Female | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| BMI (kg/m2) | 23.45 | 0.03 | 24.28 | 0.05 | 22.64 | 0.05 |
| Total energy intake (kcal) | 2145.85 | 9.88 | 2508.22 | 15.48 | 1791.34 | 8.76 |
| Cholesterol (mg) | 191.20 | 0.33 | 192.14 | 0.47 | 190.29 | 0.41 |
| Variables | N | HDL-C (mg/dL) | TG (mg/dL) | ||||
|---|---|---|---|---|---|---|---|
| Mean | SD | p-Value | Mean | SD | p-Value | ||
| Active use of nutrition labelling | |||||||
| Check and make dependent purchase decisions | 4308 | 54.42 | 0.23 | 0.2282 | 110.61 | 1.46 | 0.0653 |
| Not actively using | 12,311 | 51.69 | 0.14 | 131.78 | 1.24 | ||
| Sex | |||||||
| Male | 7127 | 48.10 | 0.15 | <0.0001 | 153.40 | 1.75 | <0.0001 |
| Female | 9492 | 56.61 | 0.16 | 99.72 | 0.81 | ||
| Age (years) | |||||||
| <20 | 264 | 54.61 | 0.77 | 0.0008 | 91.28 | 3.78 | <0.0001 |
| <30 | 2735 | 54.01 | 0.27 | 103.38 | 1.64 | ||
| <40 | 4058 | 52.85 | 0.21 | 127.28 | 2.05 | ||
| <50 | 4024 | 52.10 | 0.23 | 137.11 | 2.40 | ||
| <60 | 2942 | 51.42 | 0.27 | 141.76 | 2.27 | ||
| <70 | 1669 | 49.81 | 0.34 | 134.75 | 2.56 | ||
| 70+ | 927 | 48.59 | 0.45 | 123.65 | 2.92 | ||
| Educational level | |||||||
| High school or below | 7294 | 51.68 | 0.17 | 0.1423 | 135.84 | 1.60 | 0.0002 |
| Bachelor’s degree | 8325 | 52.99 | 0.17 | 119.16 | 1.32 | ||
| Master’s degree and above | 1000 | 51.84 | 0.47 | 128.23 | 3.88 | ||
| Economic status | |||||||
| Employed | 5556 | 53.73 | 0.21 | 0.9016 | 114.36 | 1.38 | 0.0586 |
| Unemployed | 11,063 | 51.78 | 0.14 | 131.84 | 1.32 | ||
| Household income | |||||||
| Low | 3844 | 51.92 | 0.23 | 0.0319 | 130.64 | 2.10 | 0.0847 |
| Mid-low | 4200 | 52.04 | 0.23 | 129.12 | 2.05 | ||
| Mid-high | 4282 | 52.42 | 0.22 | 125.16 | 1.81 | ||
| High | 4293 | 53.21 | 0.24 | 120.30 | 1.83 | ||
| Marital status | |||||||
| Single | 3776 | 53.54 | 0.24 | <0.0001 | 113.39 | 1.87 | 0.0087 |
| Separated/divorced/bereavement | 1261 | 51.87 | 0.41 | 140.73 | 4.18 | ||
| Married | 11,582 | 51.93 | 0.13 | 130.87 | 1.15 | ||
| Residence Area | |||||||
| Metropolitan | 9960 | 52.64 | 0.15 | 0.5638 | 123.02 | 1.24 | 0.1663 |
| Others | 6659 | 52.05 | 0.20 | 131.20 | 1.69 | ||
| Perceived health status | |||||||
| Good | 14,484 | 52.55 | 0.13 | 0.0004 | 125.39 | 1.05 | 0.146 |
| Bad | 2135 | 51.42 | 0.30 | 132.35 | 2.88 | ||
| Stress awareness | |||||||
| High | 4524 | 52.32 | 0.22 | 0.0138 | 129.51 | 2.01 | 0.0133 |
| Low | 12,095 | 52.44 | 0.14 | 124.98 | 1.12 | ||
| Alcohol intake | |||||||
| Less than 1 time per month | 6176 | 51.52 | 0.18 | <0.0001 | 113.95 | 1.22 | <0.0001 |
| 1–3 times per week | 9402 | 52.68 | 0.16 | 127.61 | 1.32 | ||
| More than 4 times per week | 1041 | 54.60 | 0.51 | 181.14 | 6.20 | ||
| Smoking status | |||||||
| Smoker | 3305 | 48.52 | 0.25 | <0.0001 | 169.75 | 2.94 | <0.0001 |
| Ex-smoker | 3256 | 50.46 | 0.24 | 138.83 | 2.21 | ||
| Non-smoker | 10,058 | 54.65 | 0.15 | 104.27 | 0.88 | ||
| Aerobic exercise habits | |||||||
| Yes | 7539 | 52.91 | 0.17 | 0.0007 | 122.68 | 1.53 | 0.0003 |
| No | 9080 | 51.93 | 0.16 | 129.62 | 1.33 | ||
| Walking for more than 10 min | |||||||
| Few | 2515 | 50.99 | 0.26 | <0.0001 | 131.95 | 2.48 | 0.0125 |
| 1–4 days per week | 5133 | 51.89 | 0.21 | 131.75 | 1.89 | ||
| 5–7 days per week | 8971 | 53.05 | 0.16 | 121.83 | 1.31 | ||
| Frequency of eating out | |||||||
| More than 4 times per week | 9762 | 52.07 | 0.15 | 0.1223 | 128.56 | 1.29 | 0.1362 |
| Less than 3 times per week | 6857 | 53.00 | 0.19 | 122.22 | 1.45 | ||
| Family history for hyperlipidemia | |||||||
| Yes | 1158 | 54.05 | 0.48 | 0.1396 | 128.26 | 4.01 | 0.0141 |
| No | 15,461 | 52.28 | 0.12 | 126.12 | 1.03 | ||
| Total | 16,619 | 52.40 | 0.12 | 126.27 | 1.01 | ||
| Variables | HDL-C (mg/dL) | TG (mg/dL) | ||||
|---|---|---|---|---|---|---|
| β | SE | p-Value | β | SE | p-Value | |
| Active use of nutrition labelling | ||||||
| Check and make dependent purchase decisions | 0.012 | 0.004 | 0.0079 | −0.032 | 0.011 | 0.0029 |
| Not actively using | Ref | - | - | Ref | - | - |
| Sex | ||||||
| Male | −0.150 | 0.005 | <0.0001 | 0.236 | 0.012 | <0.0001 |
| Female | Ref | - | - | Ref | - | - |
| Age (years) | ||||||
| <20 | 0.105 | 0.017 | <0.0001 | −0.097 | 0.044 | 0.0287 |
| <30 | 0.094 | 0.012 | <0.0001 | −0.090 | 0.030 | 0.0031 |
| <40 | 0.074 | 0.011 | <0.0001 | −0.016 | 0.026 | 0.5315 |
| <50 | 0.048 | 0.010 | <0.0001 | 0.040 | 0.024 | 0.1006 |
| <60 | 0.032 | 0.010 | 0.0021 | 0.046 | 0.024 | 0.0564 |
| <70 | 0.017 | 0.011 | 0.1121 | 0.021 | 0.026 | 0.4191 |
| 70+ | Ref | - | - | Ref | - | - |
| Educational level | ||||||
| High school or below | 0.013 | 0.008 | 0.1082 | −0.001 | 0.020 | 0.9793 |
| Bachelor’s degree | 0.009 | 0.008 | 0.2213 | −0.010 | 0.019 | 0.5880 |
| Master’s degree and above | Ref | - | - | Ref | - | - |
| Economic status | ||||||
| Employed | −0.001 | 0.004 | 0.7727 | 0.028 | 0.010 | 0.0033 |
| Unemployed | Ref | - | - | Ref | - | - |
| Household income | ||||||
| Low | −0.009 | 0.006 | 0.1226 | 0.031 | 0.014 | 0.0243 |
| Mid-low | −0.009 | 0.005 | 0.1165 | 0.024 | 0.013 | 0.0699 |
| Mid-high | −0.005 | 0.005 | 0.3555 | 0.023 | 0.013 | 0.0638 |
| High | Ref | - | - | Ref | - | - |
| Marital status | ||||||
| Single | 0.026 | 0.007 | <0.0001 | −0.002 | 0.017 | 0.9177 |
| Separated/divorced/bereavement | −0.005 | 0.008 | 0.5187 | 0.048 | 0.019 | 0.0122 |
| Married | Ref | - | - | Ref | - | - |
| Residence Area | ||||||
| Metropolitan | −0.001 | 0.004 | 0.8193 | −0.004 | 0.011 | 0.7401 |
| Others | Ref | - | - | Ref | - | - |
| Perceived health status | ||||||
| Good | 0.009 | 0.005 | 0.1091 | −0.013 | 0.014 | 0.3533 |
| Bad | Ref | - | - | Ref | - | - |
| Stress awareness | ||||||
| High | −0.010 | 0.004 | 0.0153 | 0.020 | 0.010 | 0.0499 |
| Low | Ref | - | - | Ref | - | - |
| Alcohol intake | ||||||
| Less than 1 time per month | −0.142 | 0.009 | <0.0001 | −0.142 | 0.024 | <0.0001 |
| 1–3 times per week | −0.089 | 0.008 | <0.0001 | −0.129 | 0.023 | <0.0001 |
| More than 4 times per week | Ref | - | - | Ref | - | - |
| Smoking status | ||||||
| Smoker | −0.040 | 0.006 | <0.0001 | 0.190 | 0.014 | <0.0001 |
| Ex-smoker | 0.013 | 0.006 | 0.0162 | 0.034 | 0.013 | 0.0095 |
| Non-smoker | Ref | - | - | Ref | - | - |
| Aerobic exercise habits | ||||||
| Yes | Ref | - | - | Ref | - | - |
| No | −0.017 | 0.004 | <0.0001 | 0.050 | 0.010 | <0.0001 |
| Walking for more than 10 min | ||||||
| Few | −0.014 | 0.006 | 0.0124 | −0.009 | 0.014 | 0.5196 |
| 1–4 days per week | −0.015 | 0.004 | 0.0005 | 0.021 | 0.011 | 0.0542 |
| 5–7 days per week | Ref | - | - | Ref | - | - |
| Frequency of eating out | ||||||
| More than 4 times per Week | −0.003 | 0.004 | 0.5391 | 0.011 | 0.010 | 0.2717 |
| Less than 3 times per week | Ref | - | - | Ref | - | - |
| Family history for hyperlipidemia | ||||||
| Yes | −0.006 | 0.008 | 0.4780 | 0.030 | 0.018 | 0.0932 |
| No | Ref | - | - | Ref | - | - |
| BMI (kg/m2) | −0.022 | 0.001 | <0.0001 | 0.042 | 0.001 | <0.0001 |
| Cholesterol (mg/dL) | 0.002 | 0.000 | <0.0001 | 0.005 | 0.000 | <0.0001 |
| Total energy intake (kcal) | 0.010 | 0.002 | <0.0001 | 0.001 | 0.005 | 0.8851 |
| Year | −0.002 | 0.001 | 0.1116 | −0.004 | 0.003 | 0.1404 |
| Body-Size Perception | Active Use of Nutrition Labelling | HDL-C (mg/dL) | TG (mg/dL) | ||||
|---|---|---|---|---|---|---|---|
| β | SE | p-Value | β | SE | p-Value | ||
| Misperception (Over) | Check and make dependent purchase decisions | 0.010 | 0.014 | 0.4438 | −0.036 | 0.031 | 0.2457 |
| Misperception (Under) | Check and make dependent purchase decisions | 0.010 | 0.009 | 0.3019 | −0.031 | 0.021 | 0.1430 |
| Healthy Perception | Check and make dependent purchase decisions | 0.013 | 0.005 | 0.0100 | −0.033 | 0.013 | 0.0105 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kye, S.Y.; Han, K.-T.; Jeong, S.H.; Choi, J.Y. Nutrition Labeling Usage Influences Blood Markers in Body-Size Self-Conscious Individuals: The Korean National Health and Nutrition Examination Survey (KNHANES) 2013–2018. Int. J. Environ. Res. Public Health 2020, 17, 5769. https://doi.org/10.3390/ijerph17165769
Kye SY, Han K-T, Jeong SH, Choi JY. Nutrition Labeling Usage Influences Blood Markers in Body-Size Self-Conscious Individuals: The Korean National Health and Nutrition Examination Survey (KNHANES) 2013–2018. International Journal of Environmental Research and Public Health. 2020; 17(16):5769. https://doi.org/10.3390/ijerph17165769
Chicago/Turabian StyleKye, Su Yeon, Kyu-Tae Han, Sung Hoon Jeong, and Jin Young Choi. 2020. "Nutrition Labeling Usage Influences Blood Markers in Body-Size Self-Conscious Individuals: The Korean National Health and Nutrition Examination Survey (KNHANES) 2013–2018" International Journal of Environmental Research and Public Health 17, no. 16: 5769. https://doi.org/10.3390/ijerph17165769
APA StyleKye, S. Y., Han, K.-T., Jeong, S. H., & Choi, J. Y. (2020). Nutrition Labeling Usage Influences Blood Markers in Body-Size Self-Conscious Individuals: The Korean National Health and Nutrition Examination Survey (KNHANES) 2013–2018. International Journal of Environmental Research and Public Health, 17(16), 5769. https://doi.org/10.3390/ijerph17165769




