Psychodynamic Based Equine—Assisted Psychotherapy in Adults with Intertwined Personality Problems and Traumatization: A Systematic Review
Abstract
1. Introduction
1.1. Psychodynamic Psychotherapy
1.2. Animal-Assisted Psychotherapy
1.3. Equine-Assisted Psychotherapy
2. Method
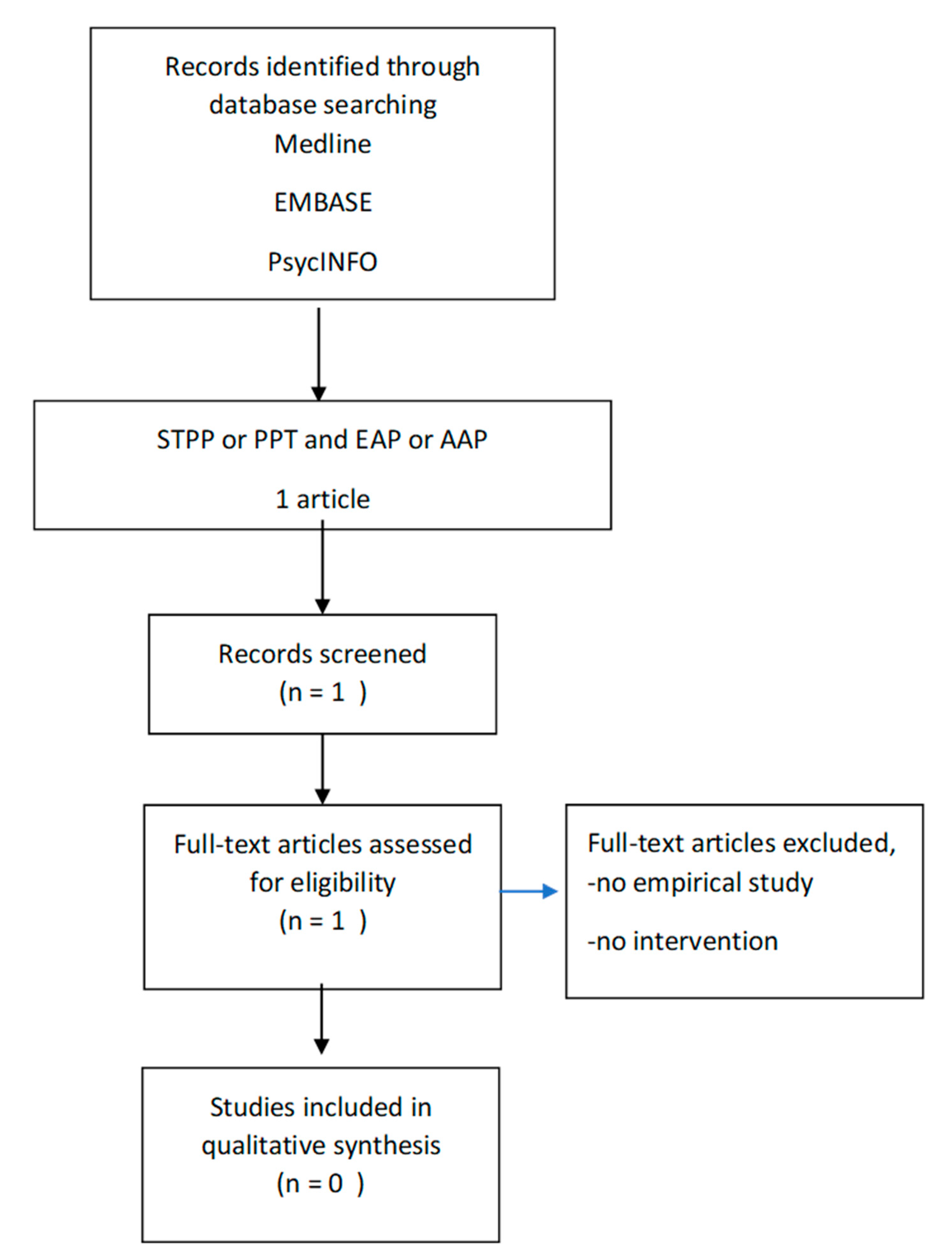
2.1. Existing Clinical Studies on Psychodynamic Based Equine-Assisted Psychotherapy
2.1.1. Study 1: Method
2.1.2. Inclusion Criteria
- 1)
- Were animal-assisted psychotherapeutic interventions with an emphasis on equine-assisted therapy with a psychodynamic characteristic for adults 18 years and over and currently experiencing symptoms or meeting criteria for a mental health condition.
- 2)
- Had been published (as journal articles) between 2015 and 2020.
- 3)
- Employed an experimental study design with a control or comparison condition, including randomized trials, matched group designs, and designs in which the sample served as their own control.
- 4)
- Included data on clinical effectiveness (e.g., changes in: interpersonal conflict and relationships, adaptive functioning, global functioning score, quality of life score, social skills, in stress response, ability to perform activities of daily living, ability to attend work/school/volunteering, changes in symptoms like PTSS symptoms, depression, mood, affect, illness perception).
2.1.3. Exclusion Criteria
3. Results
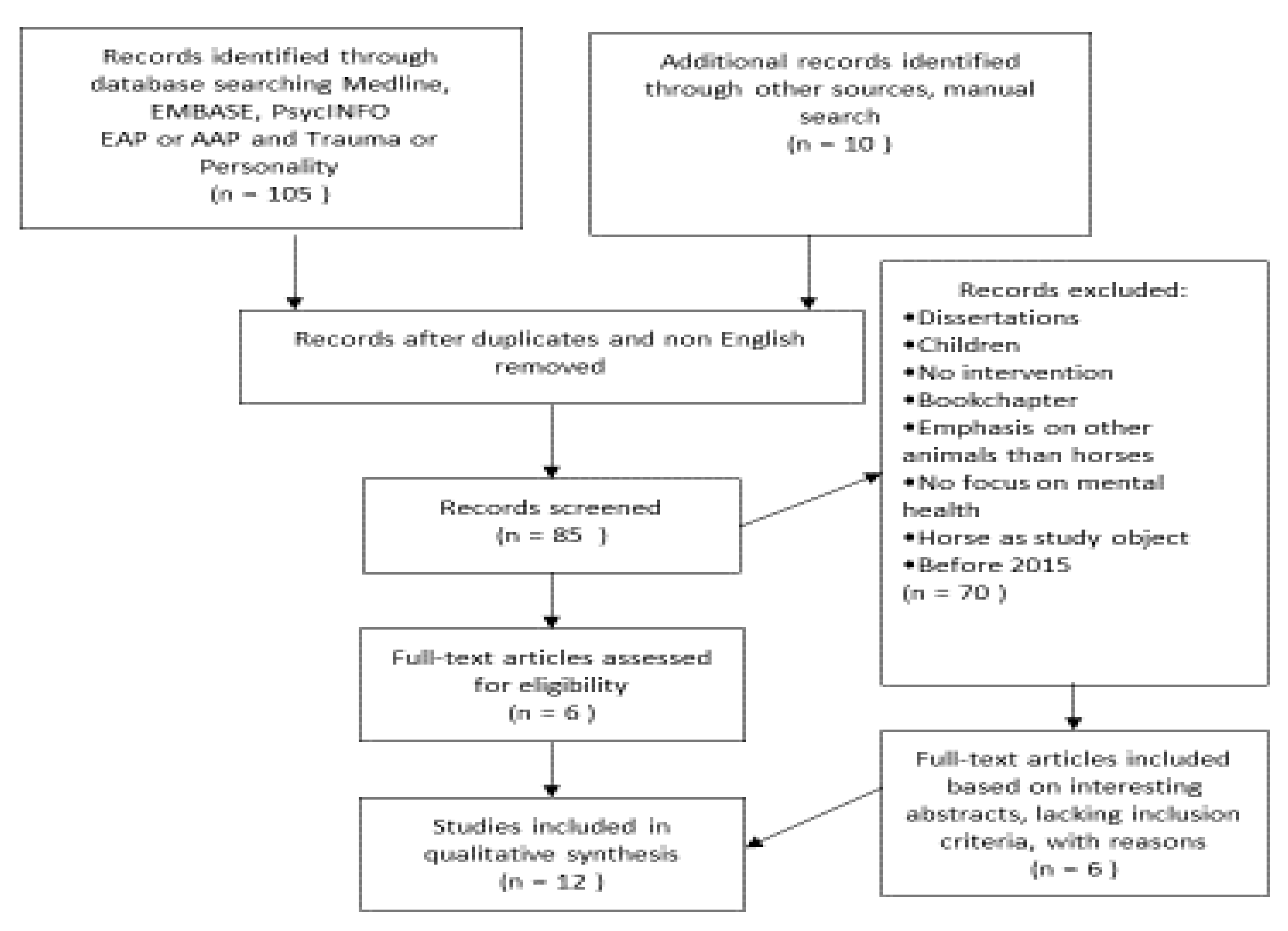
3.1. Existing Clinical Studies on Trauma and Personality in Relation to Equine-Assisted Psychotherapy
3.1.1. Study 2: Target Population
3.1.2. Psychodynamic Based EAP with Intertwined Trauma and Personality Problems
3.2. Method
4. Results
4.1. Population
4.2. Design
4.3. Intervention
4.4. Outcome
4.5. Limitations
4.6. Clinical Relevance/Therapeutic Asset
5. Discussion of Studies 1 and 2 in Unison
5.1. Study 1
5.2. Study 2
5.3. Limitations and Strengths
6. Conclusions and Recommendations
Future Directions
Author Contributions
Funding
Conflicts of Interest
References
- Luyten, P.; Lowyck, B.; Blatt, S.J. Mechanisms of Change through the Lens of Two-Polarities Models of Personality Development: State of the Art and New Directions. Psychoanal. Inq. 2017, 37, 179–190. [Google Scholar] [CrossRef]
- Fonagy, P. The effectiveness of psychodynamic psychotherapies: An update. World Psychiatry 2015, 14, 137–150. [Google Scholar] [CrossRef] [PubMed]
- Abbass, A.; Town, J.; Driessen, E. The efficacy of short-term psychodynamic psychotherapy for depressive disorders with comorbid personality disorder. Psychiatry 2011, 74, 58–71. [Google Scholar] [CrossRef] [PubMed]
- Hadjipavlou, G.; Ogrodniczuk, J.S. Promising psychotherapies for personality disorders. Can. J. Psychiatry 2010, 55, 202–210. [Google Scholar] [CrossRef]
- Gabbard, G.O.; Westen, D. Rethinking therapeutic action. Int. J. Psychoanal. 2003, 84, 823–841. [Google Scholar] [CrossRef]
- Bamelis, L.L.M.; Evers, S.M.A.A.; Spinhoven, P.; Arntz, A. Results of a multicenter randomized controlled trial of the clinical effectiveness of schema therapy for personality disorders. Am. J. Psychiatry 2014, 171, 305–322. [Google Scholar] [CrossRef]
- Steinert, C.; Munder, T.; Rabung, S.; Hoyer, J.; Leichsenring, F. Psychodynamic therapy: As efficacious as other empirically supported treatments? A meta-analysis testing equivalence of outcomes. Am. J. Psychiatry 2017, 174, 943–953. [Google Scholar] [CrossRef]
- Town, J.M.; Abbass, A.; Hardy, G. Short-term Psychodynamic Psychotherapy for Personality disorders: A critical review of randomized controlled trials. J. Pers. Disord. 2011, 25, 723–740. [Google Scholar] [CrossRef]
- Parish Plass, N. 7. The Therapy Zoo as a Mirror to the Psyche; Purdue University Press: West Lafayette, IN, USA, 2013; ISBN 978-1-61249-273-5. [Google Scholar]
- Verheggen, T.; Enders-Slegers, M.-J.; Eshuis, J. Enactive Anthrozoology: Toward an integrative theoretical model for understanding the therapeutic relationships between humans and animals. Hum.-Anim. Interact. Bull. 2017, 5, 13–35. [Google Scholar]
- Kovács, G. Experiential equine-assisted focal psychodynamic psychotherapy: Addressing personality and attachment in clients with chronic childhood trauma. In Equine-Assisted Mental Health for Healing Trauma; Routledge: London, UK, 2018; ISBN 9780429850738. [Google Scholar]
- Siporin, S. Talking horses: Equine psychotherapy and intersubjectivity. Psychodyn. Pract. 2012, 18, 457–464. [Google Scholar] [CrossRef]
- Lundgren, K.F. What science says about equine-human interaction in equine-assisted therapy: An outline to a theoretical framework. In Equine-Assisted Mental Health Interventions: Harnessing Solutions to Common Problems; Routledge: London, UK, 2018; ISBN 9781351673266. [Google Scholar]
- Porges, S.W. The polyvagal theory: Phylogenetic substrates of a social nervous system. Int. J. Psychophysiol. 2001, 42, 123–146. [Google Scholar] [CrossRef]
- van der Kolk, B.A. The Body Keep Score Bessel van der Kolk. The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma; Penguin Books: London, UK, 2014. [Google Scholar]
- Perry, B. Applying Principles of Neurodevelopment to Clinical Work with Maltreated and Traumatized Children: The Neurosequential Model of Therapeutics. In Working with Traumatized Youth in Child Welfare; Webb, N.B., Ed.; The Guilford Press: New York, NY, USA, 2006; ISBN 159385224X. [Google Scholar]
- Young, C.; Horton, J. Canine and Equine Therapy for Mental Health: A Review of Clinical Effectiveness. Rapid Response Serv. 2019. [Google Scholar]
- Hoagwood, K.E.; Acri, M.; Morrissey, M.; Peth-Pierce, R. Animal-assisted therapies for youth with or at risk for mental health problems: A systematic review. Appl. Dev. Sci. 2017, 21, 1–13. [Google Scholar] [CrossRef] [PubMed]
- O’Haire, M.E. Animal-assisted intervention for autism spectrum disorder: A systematic literature review. J. Autism Dev. Disord. 2013. [Google Scholar] [CrossRef]
- Kamioka, H.; Okada, S.; Tsutani, K.; Park, H.; Okuizumi, H.; Handa, S.; Oshio, T.; Park, S.J.; Kitayuguchi, J.; Abe, T.; et al. Effectiveness of animal-assisted therapy: A systematic review of randomized controlled trials. Complement. Ther. Med. 2014, 22, 371–390. [Google Scholar] [CrossRef]
- Anestis, M.D.; Anestis, J.C.; Zawilinski, L.L.; Hopkins, T.A.; Lilienfeld, S.O. Equine-related treatments for mental disorders lack empirical support: A systematic review of empirical investigations. J. Clin. Psychol. 2014, 70, 1115–1132. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef]
- Bartak, A.; Soeteman, D.I.; Verheul, R.; Busschbach, J.J.V. Strengthening the status of psychotherapy for personality disorders: An integrated perspective on effects and costs. Can. J. Psychiatry 2007, 52, 803–810. [Google Scholar] [CrossRef]
- Liotti, G. Attachment Disorganization and the Controlling Strategies: An Illustration of the Contributions of Attachment Theory to Developmental Psychopathology and to Psychotherapy Integration. J. Psychother. Integr. 2011, 21, 232–252. [Google Scholar] [CrossRef]
- Courtois, C.A.; Ford, J.D. Treating Complex Traumatic Stress Disorders: Scientific Foundations and Therapeutic Models; An Evidence-Based Guide; The Guilford Press: New York, NY, USA, 2009. [Google Scholar]
- Putnam, K.T.; Harris, W.W.; Putnam, F.W. Synergistic childhood adversities and complex adult psychopathology. J. Trauma. Stress 2013, 26, 435–442. [Google Scholar] [CrossRef]
- van Dijke, A.; Ford, J.D. Adult attachment and emotion dysregulation in borderline personality and somatoform disorders. Bord. Personal. Disord. Emot. Dysregul. 2015, 2, 6. [Google Scholar] [CrossRef] [PubMed]
- van Dijke, A.; Hopman, J.A.B.; Ford, J.D. Affect dysregulation, psychoform dissociation, and adult relational fears mediate the relationship between childhood trauma and complex posttraumatic stress disorder independent of the symptoms of borderline personality disorder. Eur. J. Psychotraumatol 2018, 9, 1400878. [Google Scholar] [CrossRef] [PubMed]
- Comer, R.J. Fundamentals of Abnormal Psychology; Worth Publishers: New York, NY, USA, 1985; ISBN 9787040247916. [Google Scholar]
- Levine, P.A. Polyvagal Theory and Trauma. In Clinical Applications of the Polyvagal Theory: The Emergence of Polyvagal-Informed Therapies; Porges, S.W., Dana, D., Eds.; W. W. Norton & Company: New York, NY, USA, 2018; ISBN 9781324000501. [Google Scholar]
- Schlote, S. Integrating Somatic Experiencing® and Attachment into Equine-Assisted Trauma Recovery. In Equine-Assisted Mental Health for Healing Trauma; Routledge: London, UK, 2018. [Google Scholar]
- Shultz-Jobe, B.; Naylor, K.; Jobe, T. Natural lifemanship’s trauma- focused EAP for reactive attachment disorder. In Equine-Assisted Mental Health for Healing Trauma; Routledge: London, UK, 2018; ISBN 9780429850738. [Google Scholar]
- Johnson, R.A.; Albright, D.L.; Marzolf, J.R.; Bibbo, J.L.; Yaglom, H.D.; Crowder, S.M.; Carlisle, G.K.; Willard, A.; Russell, C.L.; Grindler, K.; et al. Effects of therapeutic horseback riding on post-traumatic stress disorder in military veterans. Mil. Med. Res. 2018, 5, 3. [Google Scholar] [CrossRef] [PubMed]
- Bolden, L.; Bentley, D.; Adkins, S.; Jagielski, C.; Schwebel, D. The Effects of Animal Assisted Therapy on Perceived Pain in Patients with Spinal Cord Injury. Arch. Phys. Med. Rehabilit. 2017, 98, e117. [Google Scholar] [CrossRef]
- Alfonso, S.v.; Alfonso, L.A.; Llabre, M.M.; Isabel Fernandez, M. Project Stride: An Equine-Assisted Intervention to Reduce Symptoms of Social Anxiety in Young Women. Explor. J. Sci. Heal. 2015, 11, 461–467. [Google Scholar] [CrossRef]
- Kern-Godal, A.; Arnevik, E.A.; Walderhaug, E.; Ravndal, E. Substance use disorder treatment retention and completion: A prospective study of horse-assisted therapy (HAT) for young adults. Addict. Sci. Clin. Pract. 2015, 10, 21. [Google Scholar] [CrossRef]
- Romaniuk, M.; Evans, J.; Kidd, C. Evaluation of an equine-assisted therapy program for veterans who identify as “wounded, injured or ill” and their partners. PLoS ONE 2018, 13, e0203943. [Google Scholar] [CrossRef]
- Burton, L.E.; Qeadan, F.; Burge, M.R. Efficacy of equine-assisted psychotherapy in veterans with posttraumatic stress disorder. J. Integr. Med. 2019, 17, 14–19. [Google Scholar] [CrossRef]
- Shelef, A.; Brafman, D.; Rosing, T.; Weizman, A.; Stryjer, R.; Barak, Y. Equine Assisted Therapy for Patients with Post Traumatic Stress Disorder: A Case Series Study. Mil. Med. 2019, 184, 394–399. [Google Scholar] [CrossRef]
- Malinowski, K.; Yee, C.; Tevlin, J.M.; Birks, E.K.; Durando, M.M.; Pournajafi-Nazarloo, H.; Cavaiola, A.A.; McKeever, K.H. The Effects of Equine-Assisted Activities Therapy on Plasma Cortisol and Oxytocin Concentrations and Heart Rate Variability in Horses and Measures of Symptoms of Posttraumatic Stress Disorder in Veterans. J. Equine Vet. Sci. 2018, 64, 17–26. [Google Scholar] [CrossRef]
- Burton, L.E.; Burge, M.R. Equine assisted therapy reduces symptoms in veterans with post-traumatic stress disorder. J. Investig. Med. 2015, 63, 165. [Google Scholar]
- Earles, J.L.; Vernon, L.L.; Yetz, J.P. Equine-Assisted Therapy for Anxiety and Posttraumatic Stress Symptoms. J. Trauma. Stress 2015, 28, 149–152. [Google Scholar] [CrossRef]
- Lanning, B.A.; Wilson, A.L.; Krenek, N.; Beaujean, A.A. Using Therapeutic Riding as an Intervention for Combat Veterans: An International Classification of Functioning, Disability, and Health (ICF) Approach. Occup. Ther. Ment. Health 2017, 33, 259–278. [Google Scholar] [CrossRef]
- Balluerka, N.; Muela, A.; Amiano, N.; Caldentey, M.A. Promoting psychosocial adaptation of youths in residential care through animal-assisted psychotherapy. Child Abus. Negl. 2015, 50, 193–205. [Google Scholar] [CrossRef] [PubMed]
- Luborsky, L.; Rosenthal, R.; Diguer, L.; Andrusyna, T.P.; Berman, J.S.; Levitt, J.T.; Seligman, D.A.; Krause, E.D. The Dodo bird verdict is alive and well—Mostly. Clin. Psychol. Sci. Pract. 2002, 9, 2–12. [Google Scholar] [CrossRef]
- Truijens, F.; Zühlke-van Hulzen, L.; Vanheule, S. To manualize, or not to manualize: Is that still the question? A systematic review of empirical evidence for manual superiority in psychological treatment. J. Clin. Psychol. 2019, 75, 329–343. [Google Scholar] [CrossRef]
- Zilcha-Mano, S.; Barber, J.P. Learning from well-trained and experienced dynamic psychotherapists: Research on the efficacy of dynamic psychotherapy and its mechanisms of change. Contemp. Psychoanal. 2014, 50, 58–88. [Google Scholar] [CrossRef]
- Vanheule, S. Psychotherapy and research: A relation that needs to be reinvented. Br. J. Psychother. 2009, 25, 91–109. [Google Scholar] [CrossRef]
- Greeson, J.K.P.; Briggs, E.C.; Layne, C.M.; Belcher, H.M.E.; Ostrowski, S.A.; Kim, S.; Lee, R.C.; Vivrette, R.L.; Pynoos, R.S.; Fairbank, J.A. Traumatic Childhood Experiences in the 21st Century: Broadening and Building on the ACE Studies With Data From the National Child Traumatic Stress Network. J. Interpers. Violence 2014, 29, 536–556. [Google Scholar] [CrossRef]
- Taylor, P.; Rietzschel, J.; Danquah, A.; Berry, K. Changes in attachment representations during psychological therapy. Psychother. Res. 2015, 25. [Google Scholar] [CrossRef]
- Barlow, D.H. Negative Effects from Psychological Treatments: A Perspective. Am. Psychol. 2010, 65, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Fonagy, P. Attachment Theory and Psychoanalysis; Routledge: London, UK, 2001; ISBN 9780429896835. [Google Scholar]
- Leichsenring, F.; Abbass, A.; Hilsenroth, M.J.; Luyten, P.; Munder, T.; Rabung, S.; Steinert, C. “Gold standards,” plurality and monocultures: The need for diversity in psychotherapy. Front. Psychiatry 2018. [Google Scholar] [CrossRef] [PubMed]
- Solms, M. The Feeling Brain: Selected Papers on Neuropsychoanalysis; Routledge: London, UK, 2015; ISBN 978-1-78220-272-1. [Google Scholar]
- Kazdin, A.E.; Blase, S.L. Rebooting psychotherapy research and practice to reduce the burden of mental illness. Perspect. Psychol. Sci. 2011, 6, 21–37. [Google Scholar] [CrossRef] [PubMed]
| Journal | Population | Design | Intervention | Outcome and Limitation | Clinical Relevance/ Therapeutic Asset | |
|---|---|---|---|---|---|---|
| 1. Alfonso, L., Llabre, M., Fernandez, I. 2015 [35] | The Journal of Science and Healing, 11/2015, V. 11, 6 | Social anxiety in young women, N = 12 | Randomly assigned to experimental or a no-treatment condition. Pre-post and follow up. | combining equine-assisted activities and cognitive-behavioral strategies to reduce symptoms of social anxiety | Experimental condition significantly greater reductions in social anxiety scores from baseline to immediate-post and from baseline to follow-up. | -success experiences -teambuilding -bonding with horse -trust in others -safe haven to explore emotions |
| 2. Balluerka, N., Nekane, M., Muela, C., 2015 [44] | Child Abuse & Neglect, 2015, V.50 2015, pp. 193-205. | adolescents in residential care suffered traumatic childhood experiences with mental health problems. N = 63 | Sequential two-armed design, N = 39(19 female and 20 male; mean age = 15.03) EAP+ TAU and a control group of 5 female and 19 male; mean age = 15.67 TAU | EAP involves an ongoing treatment with clearly established goals, 12 weeks of 2 days consecutive. Attachment-based psychotherapy combined to EAP. Six thematic blocks: (1) establishing a secure base, (2) identification, understanding and verbalization of emotions, (3) emotional regulation, (4) Interpersonal relationships, (5) self-esteem and self-competence, and (6) close. | EAP compared TAU: sign.reduction hyperactivity, large ES; adaptive skills sign improved, large ES; Sign.improved social adaption, moderate ES. Pre-post EAP condition: sign reduction symptoms and depression, resp. moderate and large ES; improved social skills, large ES; Interpersonal and self-esteem, moderate ES -no randomization, sequential assignment -relatively small N | -secure attachment, relations -coping skills - touching and being touched: reciprocity and synchrony - The horse as a mirror of emotions and behaviors - Response to success and failure, resilience -six clear blocks (structure) - internal working models and defense mechanisms. - the natural environment generated a sense of security -presence of other animals (i.e., dogs) |
| 3. Bolden L.; Bentley D.; Adkins S.; Jagielski C.; Schwebel D, 2017 [34] | Archives of Physical Medicine and Rehabilitation. 94th Annual Conference of the American Congress of Rehabilitation Medicine, ACRM 2017. USA. 98 (10) (pp e117), 2017. | Perceived pain of patients with spinal cord injury (SCI). N = 25 | A randomized control trial. Experimental condition n = 11 | No information on the intervention | the average pre to post NRS score decreased for participants in the intervention group, but increased for participants in the control group | No information on the intervention |
| 4.Burton L., Burge, M., 2015 [41] | Journal of Investigative Medicine. Conference: American Federation for Medical Research Western Regional Meeting, AFMR 2015. Carmel, CA USA, 63 (1) (pp 165), 2015 | War veterans, N = 10 with PTSD | Pre-post, 6 weeks design; PTSD and resilience | 6 weeks EAGALA sessions, no riding | Reduced PTSD-related symptoms and increased adaptive coping skill of Resilience. -no control -small N | -brief intervention reduces symptoms -no information on long term effects |
| 5. Burton, L., Qeadan, F., Burge M., 2019 [38] | Journal of Integrated Medicine 2019;17(1):1419 | War veterans, N = 20; experimental condition n = 10, control n = 10 | a sequentially assigned, two-arm parallel group trial comparing 6 weeks of EAP with standard, previously established, ongoing PTSD therapy | Eagala; group; ground-work focusing on metaphors an awareness of emotions | Significant decrease PTSD, increase resilience both groups. No significant difference in PTSD, resilience and salivary cortisol compared to control. Low N, no information on control condition, short program | -decrease PTSD symptoms -increase resilience -experiencing stress relieve and improved self esteem -use of metaphors -use of a group |
| 6. Earles, J., Vernon, L., Yetz, J., 2015 [42] | Journal of Traumatic Stress. Vol.28(2), 2015, pp. 149-152 | PTSD symptoms following accident, physical or sexual assault, life-threatening illness or injury and sudden, violent death. N = 16 | Pre-post design; 6 weekly 2-h sessions measuring: Posttraumatic stress; Trauma emotion; Generalized anxiety; Depression; Alcohol use; Physical health; Mindfulness; Proactive coping; Self-efficacy; Social support; Life satisfaction; Optimism | Eagala, no riding; individual therapy in group | PTSD symptoms, emotional distress, anxiety symptoms, depression symptoms, and alcohol use decreased significantly, increase in mindfulness. No significant changes in physical health, proactive coping, general perceived self-efficacy, social support, life satisfaction, or optimism. -no control -no follow up | -less intensive outpatient program potential to be effective in reducing symptoms of anxiety and depression. -passive group might have effects -non verbal, mindfulness elements, creating safe place, setting boundaries and non critical self-awareness might be important ingredients |
| 7. Johnson et al., 2018 [33] | Military Medical Research. 5(1):3, 2018 | veterans diagnosed with (PTSD) and/or traumatic brain injury (TBI), N = 29 | randomized waiting-list (resp. n = 15, n = 14) controlled design with repeated measures | a 6-week therapeutic horseback riding (THR) program for decreasing PTSD symptoms and increasing coping self-efficacy, emotion regulation, social and emotional loneliness | significant decrease in PTSD scores and loneliness. Coping, self-efficacy, emotion regulation trended to improve. Outcome effects caused by longer program. -low N -short intervention, no follow up-not clear to be considered as psychotherapy | -less PTSS -bodily interaction with horse -self efficacy likely to improve |
| 8. Kern-Godal, A., Arnevik, E., Walderhaug, E., Ravndal, E., 2015 [36] | Addiction science & clinical practice, 10/2015, V. 10, 1 | young hospitalized substance users N = 107 | An intention-to-treat design, to compare treatment as usual (n = 43) with treatment as usual plus HAT (n = 65). | EAT as complementary to TAU. Activity and mounted work, herd observation and body-oriented | EAT supports motivation to stay longer in treatment | -therapeutic alliance -different environment -physical activity -individual attention -comorbidity |
| 9. Lanning, B., Wilson, A., Krenek, N., Alexander Beaujean, A., 2017 [43] | Occupational Therapy in Mental Health, 2017, V. 33, 3 | War veterans with PTSD, N = 51 | Pre-post design N = 51; 8-week therapeutic riding program | therapeutic riding program | significant decrease in PTSD symptoms with large ES, improved social functioning, vitality, less interference of emotions on daily activities, and increased participation with large ES. -no control -no follow up | -interaction with horse -participation in activities |
| 10. Malinowski, K. et al. 2018 [40] | Journal of Equine Veterinary Science. 64:17-26, 2018 | PTSD in Veterans. N = 7 | Pre-post design | 5 days EAA, involves equine activities | BSI inventory significantly reduced except for interpersonal sensitivity and phobic anxiety. Significant reductions Hyperarousal Symptoms of PTSD. HR was significantly reduced on day 2 involving grooming and petting in contrast to more physical activity other days. No effect on respiration rate and systolic or diastolic blood pressure. | -no information about the intervention. -short program -activities is not therapy -grooming reduced heart rate |
| 11. Romaniuk, Evans, Kidd, 2018 [37] | PLOS ONE, 09/2018, V.13, 9 | Defense Force veterans and their partners; domains of depression, anxiety, stress, PTSD, happiness, quality of life. N = 47 | A non-controlled, within-subjects longitudinal design (pre- post-interven-tion and 3 months follow-up). Individual and Couples programs between subjects comparison | equine-assisted therapy (non riding) in residential program of 5 days Relational Gestalt Therapy: exploration of issues, challenges, and behaviours and awareness of responses e.g., fear, anxiety, danger. | equine-assisted therapy useful in the reduction of depression, anxiety, stress, PTSD symptoms and the improvement of happiness and quality of life. Gains short-term unless partners are integrated into the intervention. -no explanation about the effects -no control -small N -short program | -reduction of symptoms short term -partners’ secure attachment conveys a form of resilience in adversity. -intervention without explanation/processing developmental issues might influence sustainability of effects. |
| 12. Shelef, A., Brafman, D., Rosing, T., Weizman, A., Stryjer, R., Barak Y., 2019 [39] | Military Medicine, 2019, 06 | Patients with PTSD (veterans) N = 13; measuring PTSD on daily functioning and work | open case series pre-post design, 6 months | Riding and groundwork group therapy, weekly 3 months. | significant improvement in daily functioning and work after 6 months. -no control -low N | -improvement in performing daily tasks and work/study. -locus of control and trust through structured exercises in relation to the horse. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kovács, G.; van Dijke, A.; Enders-Slegers, M.-J. Psychodynamic Based Equine—Assisted Psychotherapy in Adults with Intertwined Personality Problems and Traumatization: A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 5661. https://doi.org/10.3390/ijerph17165661
Kovács G, van Dijke A, Enders-Slegers M-J. Psychodynamic Based Equine—Assisted Psychotherapy in Adults with Intertwined Personality Problems and Traumatization: A Systematic Review. International Journal of Environmental Research and Public Health. 2020; 17(16):5661. https://doi.org/10.3390/ijerph17165661
Chicago/Turabian StyleKovács, Géza, Annemiek van Dijke, and Marie-Jose Enders-Slegers. 2020. "Psychodynamic Based Equine—Assisted Psychotherapy in Adults with Intertwined Personality Problems and Traumatization: A Systematic Review" International Journal of Environmental Research and Public Health 17, no. 16: 5661. https://doi.org/10.3390/ijerph17165661
APA StyleKovács, G., van Dijke, A., & Enders-Slegers, M.-J. (2020). Psychodynamic Based Equine—Assisted Psychotherapy in Adults with Intertwined Personality Problems and Traumatization: A Systematic Review. International Journal of Environmental Research and Public Health, 17(16), 5661. https://doi.org/10.3390/ijerph17165661






