The Association of Cooking Fuel Use, Dietary Intake, and Blood Pressure among Rural Women in China
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Data Collection
2.3. Statistical Analysis
2.4. Sensitivity Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Wang, H.; Abajobir, A.A.; Abate, K.H.; Abbafati, C.; Abbas, K.M.; Abd-Allah, F.; Abera, S.F.; Abraha, H.N.; Abu-Raddad, L.J.; Abu-Rmeileh, N.M.E.; et al. Global, regional, and national under-5 mortality, adult mortality, age-specific mortality, and life expectancy, 1970–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1084–1150. [Google Scholar] [CrossRef]
- Forouzanfar, M.H.; Afshin, A.; Alexander, L.T.; Anderson, H.R.; Bhutta, Z.A.; Biryukov, S.; Brauer, M.; Burnett, R.; Cercy, K.; Charlson, F.J.; et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1659–1724. [Google Scholar] [CrossRef]
- Lim, S.S.; Vos, T.; Flaxman, A.D.; Danaei, G.; Shibuya, K.; Adair-Rohani, H.; AlMazroa, M.A.; Amann, M.; Anderson, H.R.; Andrews, K.G.; et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2224–2260. [Google Scholar] [CrossRef]
- Duan, X.; Jiang, Y.; Wang, B.; Zhao, X.; Shen, G.; Cao, S.; Huang, N.; Qian, Y.; Chen, Y.; Wang, L. Household fuel use for cooking and heating in China: Results from the first Chinese Environmental Exposure-Related Human Activity Patterns Survey (CEERHAPS). Appl. Energy 2014, 136, 692–703. [Google Scholar] [CrossRef]
- Yu, K.; Qiu, G.; Chan, K.-H.; Lam, K.-B.H.; Kurmi, O.P.; Bennett, D.A.; Yu, C.; Pan, A.; Lv, J.; Guo, Y.; et al. Association of Solid Fuel Use With Risk of Cardiovascular and All-Cause Mortality in Rural China. JAMA 2018, 319, 1351. [Google Scholar] [CrossRef] [PubMed]
- Brook, R.D.; Rajagopalan, S.; Pope, C.A.; Brook, J.R.; Bhatnagar, A.; Diez-Roux, A.V.; Holguin, F.; Hong, Y.; Luepker, R.V.; Mittleman, M.A.; et al. Particulate Matter Air Pollution and Cardiovascular Disease: An Update to the Scientific Statement From the American Heart Association. Circulation 2010, 121, 2331–2378. [Google Scholar] [CrossRef] [PubMed]
- Nie, P.; Sousa-Poza, A.; Xue, J. Fuel for Life: Domestic Cooking Fuels and Women’s Health in Rural China. Int. J. Environ. Res. Public Health 2016, 13, 810. [Google Scholar] [CrossRef]
- Baumgartner, J.; Zhang, Y.; Schauer, J.J.; Huang, W.; Wang, Y.; Ezzati, M. Highway proximity and black carbon from cookstoves as a risk factor for higher blood pressure in rural China. Proc. Natl. Acad. Sci. USA 2014, 111, 13229–13234. [Google Scholar] [CrossRef]
- Baumgartner, J.; Schauer, J.J.; Ezzati, M.; Lu, L.; Cheng, C.; Patz, J.A.; Bautista, L.E. Indoor Air Pollution and Blood Pressure in Adult Women Living in Rural China. Environ. Health Perspect. 2011, 119, 1390–1395. [Google Scholar] [CrossRef]
- Lee, M.-S.; Hang, J.; Zhang, F.; Dai, H.; Su, L.; Christiani, D.C. In-home solid fuel use and cardiovascular disease: A cross-sectional analysis of the Shanghai Putuo study. Environ. Health 2012, 11. [Google Scholar] [CrossRef]
- Baumgartner, J.; Carter, E.; Schauer, J.J.; Ezzati, M.; Daskalopoulou, S.S.; Valois, M.-F.; Shan, M.; Yang, X. Household air pollution and measures of blood pressure, arterial stiffness and central haemodynamics. Heart 2018, 104, 1515–1521. [Google Scholar] [CrossRef] [PubMed]
- Popkin, B.M. Synthesis and implications: China’s nutrition transition in the context of changes across other low-and middle-income countries. Obes. Rev. 2014, 15, 60–67. [Google Scholar] [CrossRef] [PubMed]
- Du, H.; Li, L.; Bennett, D.; Guo, Y.; Key, T.J.; Bian, Z.; Sherliker, P.; Gao, H.; Chen, Y.; Yang, L.; et al. Fresh Fruit Consumption and Major Cardiovascular Disease in China. N. Engl. J. Med. 2016, 374, 1332–1343. [Google Scholar] [CrossRef] [PubMed]
- Adair, L.S.; Gordon-Larsen, P.; Du, S.F.; Zhang, B.; Popkin, B.M. The emergence of cardiometabolic disease risk in Chinese children and adults: Consequences of changes in diet, physical activity and obesity. Obes. Rev. 2014, 15, 49–59. [Google Scholar] [CrossRef] [PubMed]
- McCracken, J.P.; Smith, K.R.; Díaz, A.; Mittleman, M.A.; Schwartz, J. Chimney Stove Intervention to Reduce Long-term Wood Smoke Exposure Lowers Blood Pressure among Guatemalan Women. Environ. Health Perspect. 2007, 115, 996–1001. [Google Scholar] [CrossRef] [PubMed]
- Schulz, A.J.; Mentz, G.B.; Sampson, N.R.; Dvonch, J.T.; Reyes, A.G.; Izumi, B. Effects of Particulate Matter and Antioxidant Dietary Intake on Blood Pressure. Am. J. Public Health 2015, 105, 1254–1261. [Google Scholar] [CrossRef] [PubMed]
- Cross, C.E.; Valacchi, G.; Schock, B.; Wilson, M.; Weber, S.; Eiserich, J.; van der Vliet, A. Environmental Oxidant Pollutant Effects on Biologic Systems: A Focus on Micronutrient Antioxidant–Oxidant Interactions. Am. J. Respir. Crit. Care Med. 2002, 166, S44–S50. [Google Scholar] [CrossRef]
- Pope, C.A.; Dockery, D.W. Health Effects of Fine Particulate Air Pollution: Lines that Connect. J. Air Waste Manag. Assoc. 2006, 56, 709–742. [Google Scholar] [CrossRef]
- Tong, H.; Rappold, A.G.; Diaz-Sanchez, D.; Steck, S.E.; Berntsen, J.; Cascio, W.E.; Devlin, R.B.; Samet, J.M. Omega-3 Fatty Acid Supplementation Appears to Attenuate Particulate Air Pollution–Induced Cardiac Effects and Lipid Changes in Healthy Middle-Aged Adults. Environ. Health Perspect. 2012, 120, 952–957. [Google Scholar] [CrossRef]
- Popkin, B.M.; Du, S.; Zhai, F.; Zhang, B. Cohort Profile: The China Health and Nutrition Survey--monitoring and understanding socio-economic and health change in China, 1989–2011. Int. J. Epidemiol. 2010, 39, 1435–1440. [Google Scholar] [CrossRef]
- Li, S.; Meng, L.; Chiolero, A.; Ma, C.; Xi, B. Trends in smoking prevalence and attributable mortality in China, 1991–2011. Prev. Med. 2016, 93, 82–87. [Google Scholar] [CrossRef] [PubMed]
- Zimmer, Z.; Kaneda, T.; Spess, L. An Examination of Urban Versus Rural Mortality in China Using Community and Individual Data. J. Gerontol. Ser. B 2007, 62, S349–S357. [Google Scholar] [CrossRef] [PubMed]
- Popkin, B.M.; Lu, B.; Zhai, F. Understanding the nutrition transition: Measuring rapid dietary changes in transitional countries. Public Health Nutr. 2002, 5, 947–953. [Google Scholar] [CrossRef] [PubMed]
- Pickering, T.G.; Hall, J.E.; Appel, L.J.; Falkner, B.E.; Graves, J.; Hill, M.N.; Jones, D.W.; Kurtz, T.; Sheps, S.G.; Roccella, E.J. Recommendations for Blood Pressure Measurement in Humans and Experimental Animals: Part 1: Blood Pressure Measurement in Humans: A Statement for Professionals From the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation 2005, 111, 697–716. [Google Scholar] [CrossRef] [PubMed]
- Jones-Smith, J.C.; Popkin, B.M. Understanding community context and adult health changes in China: Development of an urbanicity scale. Soc. Sci. Med. 2010, 71, 1436–1446. [Google Scholar] [CrossRef] [PubMed]
- Gordon, S.B.; Bruce, N.G.; Grigg, J.; Hibberd, P.L.; Kurmi, O.P.; Lam, K.H.; Mortimer, K.; Asante, K.P.; Balakrishnan, K.; Balmes, J.; et al. Respiratory risks from household air pollution in low and middle income countries. Lancet Respir. Med. 2014, 2, 823–860. [Google Scholar] [CrossRef]
- Zhang, J.; Smith, K.R. Household Air Pollution from Coal and Biomass Fuels in China: Measurements, Health Impacts, and Interventions. Environ. Health Perspect. 2007, 115, 848–855. [Google Scholar] [CrossRef]
- Fitzmaurice, G.M.; Laird, N.M.; Ware, J.H. Applied Longitudinal Analysis, 2nd ed.; Wiley series in probability and statistics; John Wiley & Sons: Hoboken, NJ, USA, 2011; ISBN 978-0-470-38027-7. [Google Scholar]
- Miglioretti, D.L.; Heagerty, P.J. Marginal Modeling of Nonnested Multilevel Data using Standard Software. Am. J. Epidemiol. 2006, 165, 453–463. [Google Scholar] [CrossRef]
- Miglioretti, D.L. Marginal modeling of multilevel binary data with time-varying covariates. Biostatistics 2004, 5, 381–398. [Google Scholar] [CrossRef][Green Version]
- Govindarajulu, U.S.; Spiegelman, D.; Thurston, S.W.; Ganguli, B.; Eisen, E.A. Comparing smoothing techniques in Cox models for exposure–response relationships. Stat. Med. 2007, 26, 3735–3752. [Google Scholar] [CrossRef]
- Govindarajulu, U.S.; Malloy, E.J.; Ganguli, B.; Spiegelman, D.; Eisen, E.A. The Comparison of Alternative Smoothing Methods for Fitting Non-Linear Exposure-Response Relationships with Cox Models in a Simulation Study. Int. J. Biostat. 2009, 5. [Google Scholar] [CrossRef] [PubMed]
- Nevo, D.; Liao, X.; Spiegelman, D. Estimation and Inference for the Mediation Proportion. Int. J. Biostat. 2017, 13. [Google Scholar] [CrossRef] [PubMed]
- Arku, R.E.; Ezzati, M.; Baumgartner, J.; Fink, G.; Zhou, B.; Hystad, P.; Brauer, M. Elevated blood pressure and household solid fuel use in premenopausal women: Analysis of 12 Demographic and Health Surveys (DHS) from 10 countries. Environ. Res. 2018, 160, 499–505. [Google Scholar] [CrossRef] [PubMed]
- Quinn, A.K.; Ae-Ngibise, K.A.; Kinney, P.L.; Kaali, S.; Wylie, B.J.; Boamah, E.; Shimbo, D.; Agyei, O.; Chillrud, S.N.; Mujtaba, M.; et al. Ambulatory monitoring demonstrates an acute association between cookstove-related carbon monoxide and blood pressure in a Ghanaian cohort. Environ. Health 2017, 16. [Google Scholar] [CrossRef] [PubMed]
- Clark, M.L.; Bachand, A.M.; Heiderscheidt, J.M.; Yoder, S.A.; Luna, B.; Volckens, J.; Koehler, K.A.; Conway, S.; Reynolds, S.J.; Peel, J.L. Impact of a cleaner-burning cookstove intervention on blood pressure in Nicaraguan women. Indoor Air 2013, 23, 105–114. [Google Scholar] [CrossRef] [PubMed]
- Snider, G.; Carter, E.; Clark, S.; Tseng, J.; Tzu, W.; Yang, X.; Ezzati, M.; Schauer, J.J.; Wiedinmyer, C.; Baumgartner, J. Impacts of stove use patterns and outdoor air quality on household air pollution and cardiovascular mortality in southwestern China. Environ. Int. 2018, 117, 116–124. [Google Scholar] [CrossRef] [PubMed]
- Zhao, B.; Zheng, H.; Wang, S.; Smith, K.R.; Lu, X.; Aunan, K.; Gu, Y.; Wang, Y.; Ding, D.; Xing, J.; et al. Change in household fuels dominates the decrease in PM2.5 exposure and premature mortality in China in 2005–2015. Proc. Natl. Acad. Sci. USA 2018, 115, 12401–12406. [Google Scholar] [CrossRef]
- Ou, C.-Q.; Wong, C.-M.; Ho, S.-Y.; Schooling, M.; Yang, L.; Hedley, A.J.; Lam, T.-H. Dietary habits and the short-term effects of air pollution on mortality in the Chinese population in Hong Kong. J. Epidemiol. Community Health 2012, 66, 254–258. [Google Scholar] [CrossRef]
- Chinese Nutrition Society. Chinese Dietary Guidelines: Summary; People’s Medical Publishing House: Beijing, China, 2016. [Google Scholar]
- Ruiz-Mercado, I.; Masera, O.; Zamora, H.; Smith, K.R. Adoption and sustained use of improved cookstoves. Energy Policy 2011, 39, 7557–7566. [Google Scholar] [CrossRef]
- Balakrishnan, K.; Sambandam, S.; Ghosh, S.; Mukhopadhyay, K.; Vaswani, M.; Arora, N.K.; Jack, D.; Pillariseti, A.; Bates, M.N.; Smith, K.R. Household Air Pollution Exposures of Pregnant Women Receiving Advanced Combustion Cookstoves in India: Implications for Intervention. Ann. Glob. Health 2015, 81, 375. [Google Scholar] [CrossRef]
- Sambandam, S.; Balakrishnan, K.; Ghosh, S.; Sadasivam, A.; Madhav, S.; Ramasamy, R.; Samanta, M.; Mukhopadhyay, K.; Rehman, H.; Ramanathan, V. Can Currently Available Advanced Combustion Biomass Cook-Stoves Provide Health Relevant Exposure Reductions? Results from Initial Assessment of Select Commercial Models in India. EcoHealth 2015, 12, 25–41. [Google Scholar] [CrossRef] [PubMed]
- Smith, K.R.; Dutta, K.; Chengappa, C.; Gusain, P.P.S.; Masera, O.; Berrueta, V.; Edwards, R.; Bailis, R.; Shields, K.N. Monitoring and evaluation of improved biomass cookstove programs for indoor air quality and stove performance: Conclusions from the Household Energy and Health Project. Energy Sustain. Dev. 2007, 11, 5–18. [Google Scholar] [CrossRef]
- Tooze, J.A.; Midthune, D.; Dodd, K.W.; Freedman, L.S.; Krebs-Smith, S.M.; Subar, A.F.; Guenther, P.M.; Carroll, R.J.; Kipnis, V. A New Statistical Method for Estimating the Usual Intake of Episodically Consumed Foods with Application to Their Distribution. J. Am. Diet. Assoc. 2006, 106, 1575–1587. [Google Scholar] [CrossRef] [PubMed]
- Batis, C.; Aburto, T.C.; Sánchez-Pimienta, T.G.; Pedraza, L.S.; Rivera, J.A. Adherence to Dietary Recommendations for Food Group Intakes Is Low in the Mexican Population. J. Nutr. 2016, 146, 1897S–1906S. [Google Scholar] [CrossRef] [PubMed]
- Carroll, R.J.; Midthune, D.; Subar, A.F.; Shumakovich, M.; Freedman, L.S.; Thompson, F.E.; Kipnis, V. Taking Advantage of the Strengths of 2 Different Dietary Assessment Instruments to Improve Intake Estimates for Nutritional Epidemiology. Am. J. Epidemiol. 2012, 175, 340–347. [Google Scholar] [CrossRef]
- Gong, W.; Liu, A.; Yao, Y.; Ma, Y.; Ding, C.; Song, C.; Yuan, F.; Zhang, Y.; Feng, G.; Chen, Z.; et al. Nutrient Supplement Use among the Chinese Population: A Cross-Sectional Study of the 2010–2012 China Nutrition and Health Surveillance. Nutrients 2018, 10, 1733. [Google Scholar] [CrossRef]
- Wang, S.; Petzold, M.; Cao, J.; Zhang, Y.; Wang, W. Direct Medical Costs of Hospitalizations for Cardiovascular Diseases in Shanghai, China: Trends and Projections. Medicine (Baltimore) 2015, 94, e837. [Google Scholar] [CrossRef]

| Demographic and Socio-Economic Characteristics, and Lifestyle Risk Factors | Clean Cooking Fuel (n = 7114) | Coal Cooking Fuel (n = 6811) | Wood Cooking Fuel(n = 8193) |
|---|---|---|---|
| Age (years) | 44.84 ± 13.86 | 44.21 ± 14.87 | 44.27 ± 14.53 |
| Annual total household income (yuan inflated to 2011) | 35,678.59 ± 41,832.66 | 19,103.19 ± 25,645.52 | 17,580.39 ± 2122.14 |
| Community urbanicity index | 61.97 ± 16.70 | 47.30 ± 14.14 | 41.57 ± 11.65 |
| Educational attainment | |||
| No education | 1057 (14.86) | 2147 (31.52) | 2527 (30.84) |
| Some primary school | 1463 (20.57) | 1718 (25.22) | 2165 (26.42) |
| Completed primary school | 863 (12.13) | 735 (10.79) | 1197 (14.61) |
| Some high school | 2463 (34.62) | 1717 (25.21) | 1873 (22.86) |
| Completed high school or higher | 1268 (17.82) | 494 (7.25) | 431 (5.26) |
| Average time spent cooking per week (hours) | 7.86 ± 6.70 | 10.05 ± 8.16 | 10.09 ± 7.78 |
| Ever smoked | 293 (4.12) | 189 (2.77) | 477 (5.82) |
| Alcohol intake | |||
| Not a consumer | 6450 (90.67) | 6166 (90.53) | 7480 (91.30) |
| Consumer | 664 (9.33) | 645 (9.47) | 713 (8.70) |
| Body mass index (kg/m2) | 23.17 ± 3.54 | 22.47 ± 3.19 | 22.13 ± 3.09 |
| Systolic Blood Pressure (mm Hg) | 117.27 ± 16.68 | 115.15 ± 17.61 | 115.79 ± 17.23 |
| Diastolic Blood Pressure (mm Hg) | 76.24 ± 10.29 | 74.72 ± 10.70 | 74.92 ± 10.60 |
| Salt (g/1000 kcal/day) | 4.98 ± 4.09 | 5.45 ± 4.27 | 5.56 ± 4.50 |
| Vegetables (g/1000 kcal/day) | 136.38 ± 76.55 | 142.68 ± 83.92 | 137.20 ± 79.61 |
| Seafood (g/1000 kcal/day) | 16.76 ± 26.38 | 7.86 ± 19.61 | 9.00 ± 19.50 |
| Fruit (g/1000 kcal/day) | 25.74 ± 60.04 | 7.83 ± 34.05 | 9.60 ± 43.87 |
| Meat (g/1000 kcal/day) | 36.61 ± 31.12 | 22.93 ± 27.26 | 16.81 ± 22.57 |
| Oil (g/1000 kcal/day) | 15.31 ± 11.64 | 9.08 ± 10.52 | 12.97 ± 10.50 |
| Rice (g/1000 kcal/day) | 309.97 ± 180.63 | 325.23 ± 230.44 | 366.14 ± 232.73 |
| Outcome | Coal | Wood | ||||
|---|---|---|---|---|---|---|
| Without Diet | With Diet | % Mediation | Without Diet | With Diet | % Mediation | |
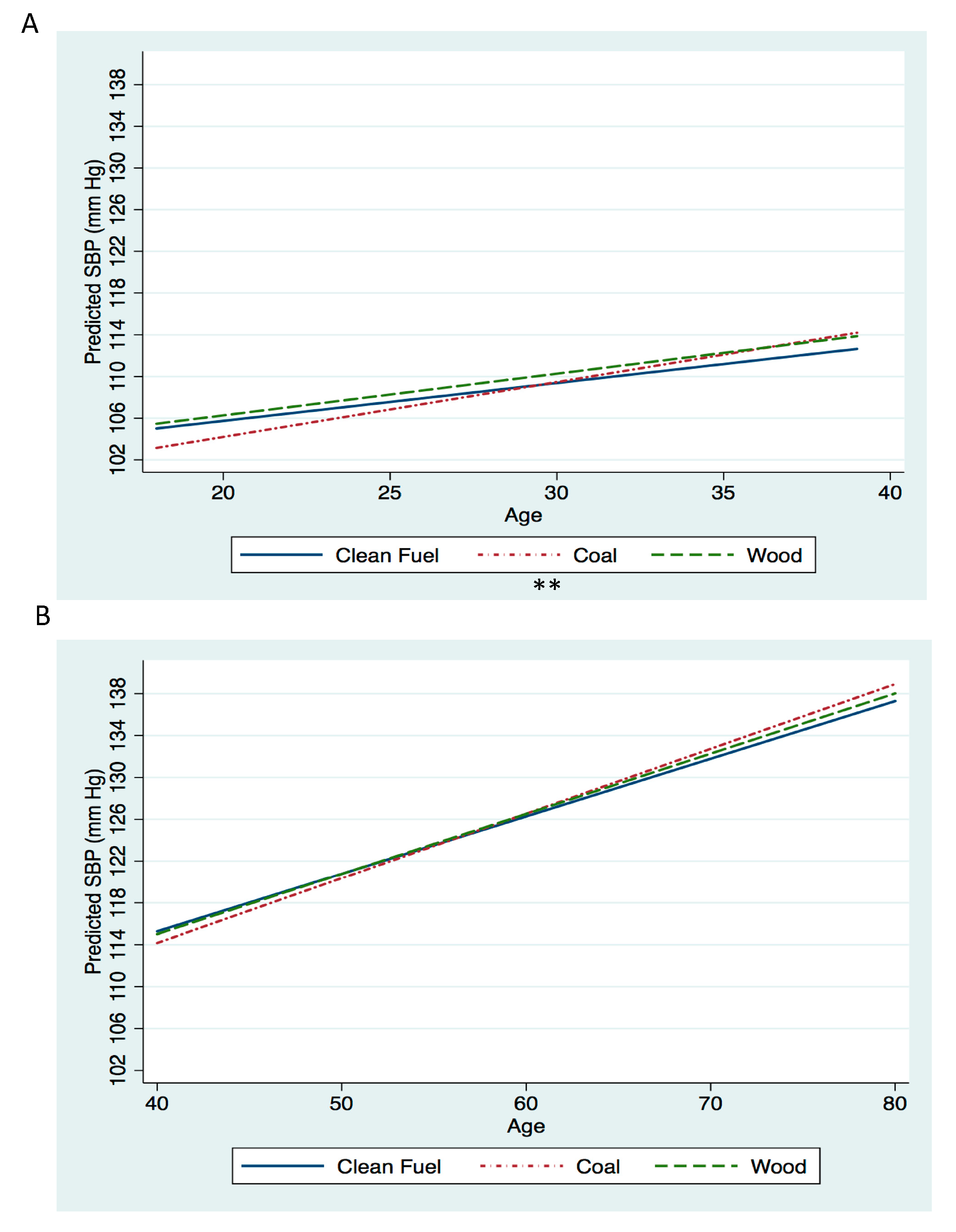
| Change in SBP (mm Hg) by year of age | 0.16 (0.05, 0.28) | 0.16 (0.05, 0.28) | 0.11% | 0.04 (−0.09, 0.16) | 0.03 (−0.09, 0.16) | 0.67% |
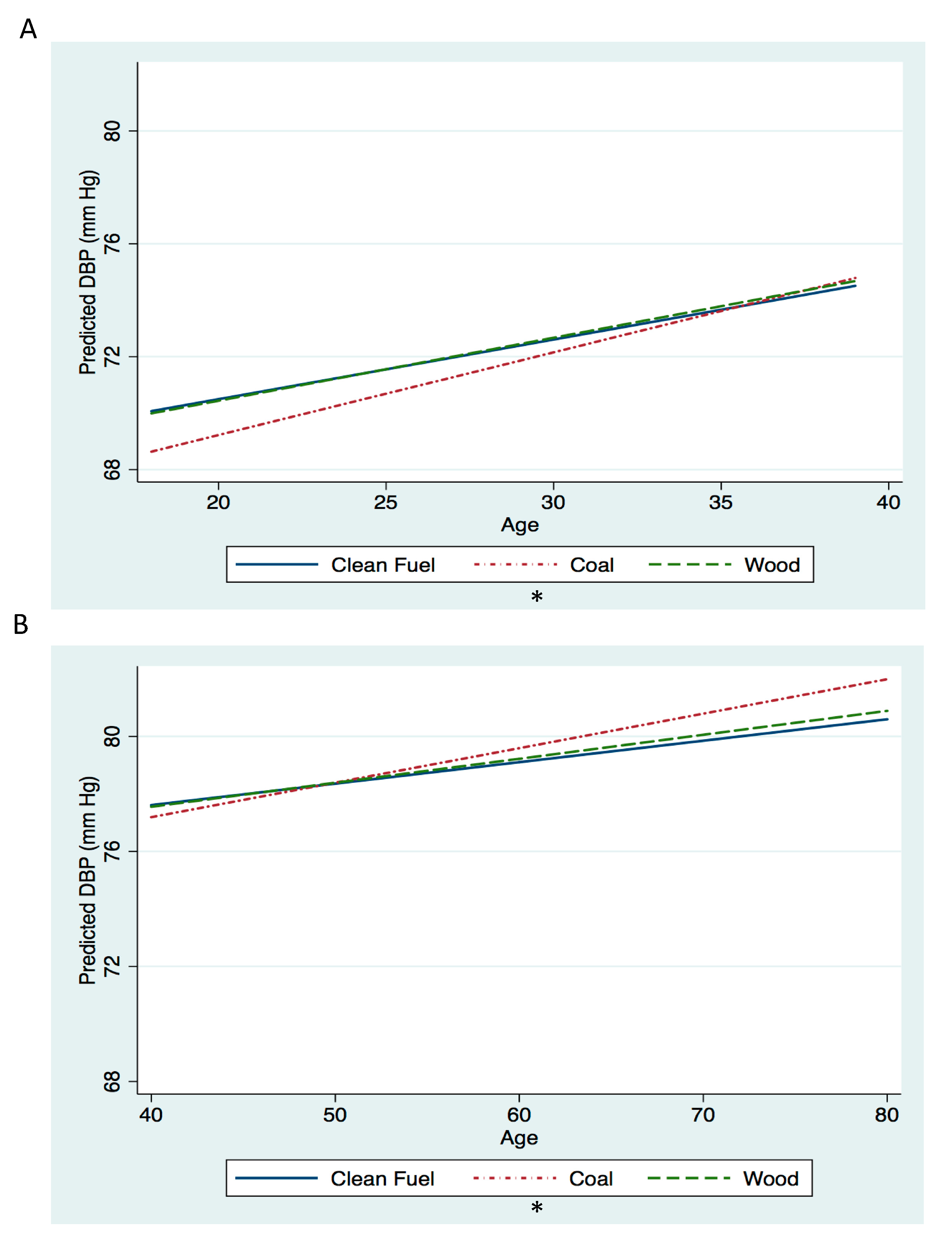
| Change in DBP (mm Hg) by year of age | 0.08 (0.00, 0.17) | 0.08 (−0.01, 0.17) | 0.22% | 0.01 (−0.08, 0.11) | 0.01 (−0.08, 0.11) | 0.85% |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bellows, A.L.; Spiegelman, D.; Du, S.; Jaacks, L.M. The Association of Cooking Fuel Use, Dietary Intake, and Blood Pressure among Rural Women in China. Int. J. Environ. Res. Public Health 2020, 17, 5516. https://doi.org/10.3390/ijerph17155516
Bellows AL, Spiegelman D, Du S, Jaacks LM. The Association of Cooking Fuel Use, Dietary Intake, and Blood Pressure among Rural Women in China. International Journal of Environmental Research and Public Health. 2020; 17(15):5516. https://doi.org/10.3390/ijerph17155516
Chicago/Turabian StyleBellows, Alexandra L., Donna Spiegelman, Shufa Du, and Lindsay M. Jaacks. 2020. "The Association of Cooking Fuel Use, Dietary Intake, and Blood Pressure among Rural Women in China" International Journal of Environmental Research and Public Health 17, no. 15: 5516. https://doi.org/10.3390/ijerph17155516
APA StyleBellows, A. L., Spiegelman, D., Du, S., & Jaacks, L. M. (2020). The Association of Cooking Fuel Use, Dietary Intake, and Blood Pressure among Rural Women in China. International Journal of Environmental Research and Public Health, 17(15), 5516. https://doi.org/10.3390/ijerph17155516





