Abstract
Many prehospital factors that are known to influence survival rates after out-of-hospital cardiac arrest (OHCA) have been rarely studied as to how their influence varies depending on the age. In this study, we tried to find out what prehospital factors affect the survival rate after OHCA by age groups and how large the effect size of those factors is in each age group. We used the South Korean OHCA registry, which includes information on various prehospital factors relating OHCA and final survival status. The association between prehospital factors and survival was explored through logistic regression analyses for each age group. The effects of prehospital factors vary depending on the patient’s age. Being witnessed was relatively more influential in younger patients and the presence of first responders became more important as patients became older. While bystander cardiopulmonary resuscitation (CPR) did not appear to significantly affect survival in younger people, use of an automated external defibrillator (AED) showed the largest effect size on the survival in all age groups. Since the pathophysiology and etiologies of OHCA vary according to age, more detailed information on life support by age is needed for the development and application of more specialized protocols for each age.
1. Introduction
Out-of-hospital cardiac arrest (OHCA) is a global health problem that affects 55 people per 100,000 people worldwide, but the survival rate varies significantly from community to community [1,2]. Many studies have attempted to identify factors affecting the survival rate after OHCA. Basically, predictors of survival after OHCA can be broadly classified into patient factors, event factors, system factors, and treatment factors [3,4,5,6]. Specifically, a series of actions are needed, including the immediate recognition of the cardiac arrest and the activation of an emergency response system, early cardiopulmonary resuscitation (CPR), rapid defibrillation, effective advanced life support, and integrated treatment after cardiac arrest [7,8]. Past medical literature had focused more on hospitals and advanced life-sustaining treatments than problems related to community care and basic life-sustaining. However, in recent years, awareness of the importance of basic life support (BLS), the role of the community, and the key functions of emergency medical dispatch in coordinating bystander CPR and early defibrillation has increased [9,10].
However, several factors that have been recognized to influence survival rates after OHCA have been rarely studied as to how their influence varies depending on the demographic variables of OHCA patients, especially age. Since the pathophysiology and etiologies of OHCA are different for each age group [11,12,13], it can be expected that factors affecting survival or their influence will differ according to age. The aims of this study were to find out what prehospital factors affect the survival rate after OHCA and how large the effect size of those factors is by age groups based on the data source conducted by the Korea Centers for Disease Control and Prevention (KCDC) for all OHCAs that have occurred in South Korea for two years.
2. Materials and Methods
2.1. Data Source and Study Population
Since 2006, the South Korean OHCA registry (KOHCAR) of cardiac arrest patients transported through the Emergency Medical Service (EMS) has been built by the KCDC in cooperation with the Central Fire Service (CFS). The EMS run sheet, EMS CPR registration, and dispatch CPR registration were merged into one database by CFS’s EMS quality committee and sent to KCDC. The KCDC cleaned up the hospital information database and reviewed hospital records for inpatient treatment and outcomes [14]. The data used in this study included only those who were confirmed to be OHCA by EMS personnel and were finally identified as OHCA based on the medical records of each patient after being transferred to the hospital. Data obtained from KOHCAR include the date of the OHCA, the patient’s demographic information, the location of the OHCA, the witness of the event, the bystander CPR, application of prehospital automated external defibrillators (AEDs), the etiology of the OHCA, the initial electrocardiographic rhythm, and the experience of return of spontaneous circulation (ROSC), survival to discharge, and cerebral performance categories (CPC) at discharge.
The study population of this study initially included all OHCAs that occurred from 1 January 2015 to 31 December 2016. As shown in Figure 1, we first excluded cases where the etiology of OHCA was unclear or not cardiogenic. In addition, we excluded cases in which survival status was unclear, and finally 43,688 cases were selected for the study. The KOHCAR we used was approved by the National Statistical Office as a national statistic (approval number 117088), and is released to the general public through the National Statistical Office (http://kosis.kr). The raw data does not disclose any information that can estimate a specific individual based on the “Personal Information Protection Act” and “Statistics Act”. The institutional review board of the Konyang University Hospital and the KCDC approved the study protocol (KYU-2018-056-01).
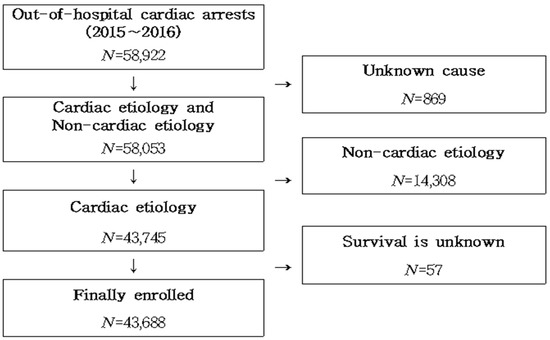
Figure 1.
Process for selecting the study population.
2.2. Independent and Dependent Variables
This study basically focused on prehospital factors. The initial electrocardiographic rhythm, ROSC, the response time, and the time of witnessing are important prehospital factors, but many of these items were often missing and recorded as ‘unknown’, so they were not included in the final analysis. We included six prehospital variables with complete data fidelity in the final analytical model. The independent variables were classified into the subject’s personal factors, situation factors, and CPR/AED factors. Gender was used as the personal factor, and whether or not witness, witness type, and place of event were used as the situational factors. CPR/AED factors included whether CPR was performed and whether or not AED was used (Figure 2).
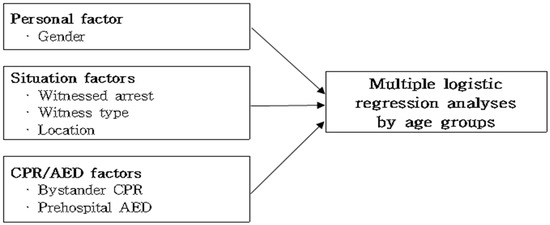
Figure 2.
Study framework. CPR, cardiopulmonary resuscitation; AED, automated external defibrillator.
The gender was divided into ‘male’ and ‘female’, and whether or not witnessed were classified as ‘unwitnessed’ and ‘witnessed’. Witness types were divided into ‘first responders’ and the ‘laypeople’. The first responders were those who have essentially completed training on rescue and first aid, including CPR, according to Article 14 (Education on Rescue and First Aid) of the Korean Emergency Medical Care Act, and other witnesses were designated as the layperson. The place where the cardiac arrest occurred was classified as ‘public place’ and ‘non-public place’. Public places include roads/highways, public buildings, leisure-related facilities, industrial facilities, commercial facilities, and transportation terminals. Among the CPR/AED factors, whether CPR was performed by the layperson was classified as ‘yes’ or ‘no’. Likewise, according to whether AED was used before arrival at the hospital, it was also classified as ‘yes’ or ‘no’.
The dependent variable was the survival status. If the patient was transferred to another hospital after the spontaneous circulation was recovered, or if the patient was discharged after the spontaneous circulation was recovered, it was designated as ‘survival’. Those who died or were discharged without hope were classified as ‘death’.
2.3. Statistical Analyses
The age groups of the study subjects were divided into six groups as follows: 0–6 years old, 7–18 years old, 19–39 years old, 40–59 years old, 60–79 years old, and 80 years old or older. To understand the general characteristics of the subjects, the frequency and percentage of categorical variables and the mean and standard deviation were used for continuous variables. To compare the survival results according to each factor, a chi-square test was performed on categorical variables and an independent sample t-test was performed on continuous variables. We performed multivariate logistic regression analysis for each of the six age groups to understand the relationship with factors affecting survival outcomes (Figure 2). Each analysis was performed with a single model consisting of survival variables and six independent variables. In each Hosmer and Lemeshow goodness-of-fit test of the six analyses, all models were found to be suitable because the p-value was greater than 0.05. All tests were treated as statistically significant when the probability of significance was 0.05 or less. SPSS Statistics 20.0 (IBM, Armonk, NY, USA) was used for data analysis.
3. Results
Table 1 shows the distribution of variables by study subjects by survival and death after OCHA. Male patients survived 13.7% higher than female patients. By age, the survival proportion for patients aged 7–18 was the highest at 30.7%, and declined with age. Survival proportions were higher in cases where OHCA was witnessed, was seen by a first responder, or occurred in public places, and CPR or AED was performed.

Table 1.
General characteristics of the study population by survival status.
Table 2 shows the results of the multiple logistic regression analysis conducted to identify factors affecting the survival of OHCA by age groups while controlling the effects of other variables. Gender did not appear to be associated with the survival at all ages. However, when witnessed during OHCA, survivable odds were 2.6–8.4 higher than those not witnessed. In particular, in early childhood and adolescence, being witnessed had greater effects on the probability of survival than other age groups. When the witness was the first responder, the relative impact of this on survival increased as the patient’s age increased. Survival odds after OHCA in a public place were higher in all age groups than in a non-public place, especially in early childhood. Whether bystander CPR was performed at the place where OHCA occurred had little effect on survival in younger people, whereas AED application showed significantly high odds ratios at all ages.

Table 2.
Prehospital factors related to survival of out-of-hospital cardiac arrest (OHCA) patients by age groups. Odds ratios (95% confidence interval).
4. Discussion
4.1. Main Findings
In this study, we found that the prehospital factors affecting the survival of OHCA were not just identified, but that the factors related to survival and the size of effects varied according to the age group. Being witnessed was relatively more influential in childhood and younger ages, and being witnessed by first responders became more important as patients became older. The survival rate is high in OHCAs occurring in public places, especially in children and the elderly. On the other hand, bystander CPR did not appear to significantly affect survival in younger people. The factor showing the largest effect size was the use of AED, which showed very large strength of associations in all age groups. In other words, this study showed that the effects of prehospital factors known to be important in surviving of OHCA could vary depending on the patient’s age.
4.2. Implications in South Korean Context
In South Korea, nearly 300,000 OHCA occurred every year, and the probability of survival or a good neurological outcome is relatively low compared to other developed countries [15,16,17]. Under the perception of this problem, South Korea has recently taught laypeople to learn how to provide bystander CPR, including the use of AEDs, and has introduced prehospital advanced life support (ALS) by Emergency Medical Services [18]. South Korea has collected OHCA data for the past 14 years, reporting the risk factors of death to the public [19,20]. Risk factors for OHCA deaths include elderly and female patients [21], non-public locations [22], and no witnesses [19,20]. On the other hand, factors that can reduce death include bystander CPR [17,22,23], shockable rhythm [17,23], and prehospital AED use [24,25].
Our findings enrich the knowledge of survival-related factors on OHCA identified in previous studies. Since the pathophysiology and causes of OHCA vary according to age, it is important to know that factors that are expected to increase survival in general may appear ineffective, depending on the patient’s age [26,27,28,29]. Currently, BLS protocols are applied differently to the two groups, children and adults, based on previously identified evidence. More detailed medical and public health information on BLS by age is needed for the development and application of more specialized BLS protocols for each age. For example, the higher the age group, the greater the survival rate if found in public places, by first respondents, or bystander CPR, so the following intervention needs to be considered. In places where people of middle-aged and older gather more, more primary respondents need to be deployed, and more CPR training programs for families supporting the elderly should be implemented. In order to reduce the probability of OHCA occurring when the elderly are alone in a private space such as a home, it may be necessary to further increase the public facilities for the elderly.
The prehospital factors we studied later affect various hospital factors and are also related to the recently recommended extracorporeal cardiopulmonary resuscitation (ECPR). South Korea added new information on ECPR in the field of ALS in the 2015 revised Korean CPR guidelines. When an extracorporeal circulation device is connected, oxygenated blood circulates without chest compressions and artificial respiration. Many indications for ECPR are related to prehospital factors, such as those under 80 years of age, or a refractory OHCA, or bystander CPR [30]. The results of our study show the impact on the survival of prehospital factors by age and can be considered when applying ECPR with age.
In South Korea, there are a total of 429 emergency medical institutions with three hierarchical orders depending on the size of the region. However, the distribution of these institutions is regionally skewed, and there are only a few emergency medical institutions located in rural areas, so regional disparities exist. In particular, the regional variation in establishing a medical infrastructure for specialized emergency diseases such as cardiovascular, mental, and pediatric diseases is more serious. This biased deployment of emergency medical resources increases the regional variation in mortality rates for critically ill patients. As a result, South Korea still has lower numbers of emergency arrivals in a reasonable time and reliability of emergency medical service other developed countries. It is highly likely that emergency patients will survive after receiving the final emergency treatment within the golden hour. In 2018, the rate of trauma patients arriving within 3 h after the onset was only 35.01%. The incidence of traffic accidents is still high, and as the rate of suicide among young people and the elderly ranks first among Organization for Economic Cooperation and Development (OECD) countries, the demand for emergency medical treatment by trauma continues to increase [31].
4.3. Reasons for Different Effects for Age
Child subjects in this study were limited to cardiogenic OHCA. Children usually have an unshockable rhythm, asystole, or bradycardia, unlike adults when cardiac arrest occurs [32,33,34]. Therefore, in the case of OHCA in children, ALS is relatively more important than BLS. This seems to be the reason why the effects of the first responder, bystander CPR, and AED application on survival were unclear in our study. While the effect of the bystander CPR or first responder is not clear in school age patients (aged 7–18), the use of AED directly or indirectly through witnesses when an event occurs has been shown to dramatically improve survival. This is probably because many major etiologies of OHCA in the school age are congenital and/or genetic like in children [35,36]. Young adults generally have more OHCA due to coronary artery disease (CAD) than younger groups, and more OHCA due to genetic factors than older groups. Young adults generally have more OHCA due to CAD than younger groups, and more OHCA due to genetic factors than older groups [37,38,39]. Therefore, the patterns of impact of the first responder, bystander CPR, and AED use are located between the younger and the older. OHCA in the elderly, where CAD is the most common cause, shows in our study that the survival rate is lower than that of other age groups, and that several prehospital factors need to operate simultaneously. Taken together, our research shows that the relative importance of BLS to ALS for survival is different because the cause of OHCA is age-dependent, and the survival rate in OHCA due to CAD can only rise if all elements of BLS are performed together.
4.4. Limitations
The most serious limitation of this study is that this study reflects a lot of Korean context, so it takes a lot of attention to generalize. Korea has a very limited distribution of primary respondents compared to other developed countries, and their performance is low. In addition, the probability and quality of bystander CPR is relatively low. Therefore, the size of the effect of these factors, which was confirmed to have a great influence on the survival rate in the previous studies, came to be low across all ages in our analysis. Care must be taken to interpret the small effect size of these factors in our analysis.
Direct comparison of odds ratios, especially applied to different groups, requires careful interpretation. Each of the odds ratios presented in our analysis is for only one variable in one age group. However, if this characteristic is sufficiently considered, the relative importance of the variable can be grasped by comparing the odds ratios. For example, the odds ratio of AED use at 19–39 years was 7.82, which was greater than the odds ratio of 5.41 at 40–59 years, indicating that the relative impact of the AED use at the age of 19–39 is greater than that of 40–59 years.
The study did not take into account hospital factors and other Utstein factors [40]. The KOHCAR we used was initially designed to reflect the Utstein Style’s recommendations, but did not include all Utstein factors due to the unfavorable survey conditions in South Korea. Additionally, as mentioned in the methods section, some of the items included in the survey were often missing or marked as unknown, so the failure to use these variables in this study is another major limitation. Therefore, our logistic analysis model cannot be considered as an extensive evaluation of factors affecting the survival rate after OHCA. Most studies of OHCA survival so far, including ours, have focused on finding out what factors influence survival. However, few studies have recently been conducted to quantify the relative impacts of these factors to develop a predictive model of OHCA survival [41,42]. This predictive model can be used for stratifying each patient according to risk. The results of this study, suggesting that factors affecting OHCA survival may differ with age, also need to be included in the survival prediction model.
5. Conclusions
This study tried to find out what prehospital factors affect the survival rate after OHCA and how large the effect size of those factors is by age groups using a national OHCA registry. This study showed that the effects of prehospital factors known to be important in surviving of OHCA through the previous studies could vary depending on the patient’s age. Being witnessed was relatively more influential in younger patients and the presence of first responders became more important as patients became older. While bystander CPR did not appear to significantly affect survival in younger people, use of AED showed the largest effect size on the survival in all age groups. Since the pathophysiology and etiologies of OHCA vary according to age, more detailed information on BLS by age is needed for the development and application of more specialized BLS protocols for each age.
Author Contributions
Conceptualization, B.Y.R., B.K. and Y.H.L.; methodology, B.Y.R., B.K. and Y.H.L.; software, B.Y.R., B.K. and Y.H.L.; validation, B.Y.R., B.K. and Y.H.L.; formal analysis, B.Y.R., B.K. and Y.H.L.; data curation, B.Y.R., B.K. and Y.H.L.; writing—original draft preparation, B.Y.R., B.K. and Y.H.L.; writing—review and editing, B.Y.R., B.K. and Y.H.L.; visualization, B.Y.R., B.K. and Y.H.L.; supervision, B.Y.R., B.K. and Y.H.L. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Berdowski, J.; Berg, R.A.; Tijssen, J.G.; Koster, R.W. Global incidences of out-of-hospital cardiac arrest and survival rates: Systematic review of 67 prospective studies. Resuscitation 2010, 81, 1479–1487. [Google Scholar] [CrossRef] [PubMed]
- Nichol, G.; Thomas, E.; Callaway, C.W.; Hedges, J.; Powell, J.L.; Aufderheide, T.P.; Davis, D. Regional variation in out-of-hospital cardiac arrest incidence and outcome. JAMA 2008, 300, 1423–1431. [Google Scholar] [CrossRef] [PubMed]
- Benditt, D.G.; Goldstein, M.; Sutton, R.; Yannopoulos, D. Dispatcher-directed bystander initiated cardiopulmonary resuscitation: A safe step, but only a first step, in an integrated approach to improving sudden cardiac arrest survival. Circulation 2010, 121, 10–13. [Google Scholar] [CrossRef] [PubMed]
- Cummins, R.O.; Ornato, J.P.; Thies, W.H.; Pepe, P.E. Improving survival from sudden cardiac arrest: The “chain of survival” concept. A statement for health professionals from the Advanced Cardiac Life Support Subcommittee and the Emergency Cardiac Care Committee, American Heart Association. Circulation 1991, 83, 1832–1847. [Google Scholar] [CrossRef] [PubMed]
- Marenco, J.P.; Wang, P.J.; Link, M.S.; Homoud, M.K.; Estes, N.A. Improving survival from sudden cardiac arrest: The role of the automated external defibrillator. JAMA 2001, 285, 1193–1200. [Google Scholar] [CrossRef] [PubMed]
- SoRelle, R. Automated external defibrillators improving survival after sudden cardiac arrest. Circulation 2001, 103, E9024–E9025. [Google Scholar] [CrossRef]
- Iwami, T.; Nichol, G.; Hiraide, A.; Hayashi, Y.; Nishiuchi, T.; Kajino, K.; Morita, H.; Yukioka, H.; Ikeuchi, H.; Sugimoto, H.; et al. Continuous improvements in “chain of survival” increased survival after out-of-hospital cardiac arrests: A large-scale population-based study. Circulation 2009, 119, 728–734. [Google Scholar] [CrossRef]
- Lund-Kordahl, I.; Olasveengen, T.M.; Lorem, T.; Samdal, M.; Wik, L.; Sunde, K. Improving outcome after out-of-hospital cardiac arrest by strengthening weak links of the local Chain of Survival; quality of advanced life support and post-resuscitation care. Resuscitation 2010, 81, 422–426. [Google Scholar] [CrossRef]
- Rea, T.D.; Cook, A.J.; Stiell, I.G.; Powell, J.; Bigham, B.; Callaway, C.W.; Chugh, S.; Aufderheide, T.P.; Morrison, L.; Terndrup, T.E.; et al. Predicting survival after out-of-hospital cardiac arrest: Role of the Utstein data elements. Ann. Emerg. Med. 2010, 55, 249–257. [Google Scholar] [CrossRef]
- Shinozaki, K.; Nonogi, H.; Nagao, K.; Becker, L.B. Strategies to improve cardiac arrest survival: A time to act. Acute Med. Surg. 2016, 3, 61–64. [Google Scholar] [CrossRef]
- Bagnall, R.D.; Weintraub, R.G.; Ingles, J.; Duflou, J.; Yeates, L.; Lam, L.; Davis, A.M.; Thompson, T.; Connell, V.; Wallace, J.; et al. A Prospective Study of Sudden Cardiac Death among Children and Young Adults. N. Engl. J. Med. 2016, 374, 2441–2452. [Google Scholar] [CrossRef]
- Terman, S.W.; Shields, T.A.; Hume, B.; Silbergleit, R. The influence of age and chronic medical conditions on neurological outcomes in out of hospital cardiac arrest. Resuscitation 2015, 89, 169–176. [Google Scholar] [CrossRef] [PubMed]
- Beesems, S.G.; Blom, M.T.; van der Pas, M.H.; Hulleman, M.; van de Glind, E.M.; van Munster, B.C.; Tijssen, J.G.; Tan, H.L.; van Delden, J.J.; Koster, R.W. Comorbidity and favorable neurologic outcome after out-of-hospital cardiac arrest in patients of 70 years and older. Resuscitation 2015, 94, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.T.; Shin, S.D.; Hong, S.O.; Ahn, K.O.; Ro, Y.S.; Song, K.J.; Hong, K.J. Effect of national implementation of utstein recommendation from the global resuscitation alliance on ten steps to improve outcomes from Out-of-Hospital cardiac arrest: A ten-year observational study in Korea. BMJ Open 2017, 7, e016925. [Google Scholar] [CrossRef] [PubMed]
- Buick, J.E.; Drennan, I.R.; Scales, D.C.; Brooks, S.C.; Byers, A.; Cheskes, S.; Dainty, K.N.; Feldman, M.; Verbeek, P.R.; Zhan, C.; et al. Improving Temporal Trends in Survival and Neurological Outcomes after Out-of-Hospital Cardiac Arrest. Circ. Cardiovasc. Qual. Outcomes 2018, 11, e003561. [Google Scholar] [CrossRef]
- Kashiura, M.; Hamabe, Y.; Akashi, A.; Sakurai, A.; Tahara, Y.; Yonemoto, N.; Nagao, K.; Yaguchi, A.; Morimura, N. Association between cardiopulmonary resuscitation duration and one-month neurological outcomes for out-of-hospital cardiac arrest: A prospective cohort study. BMC Anesthesiol. 2017, 17, 59. [Google Scholar] [CrossRef]
- McNally, B.; Robb, R.; Mehta, M.; Vellano, K.; Valderrama, A.L.; Yoon, P.W.; Sasson, C.; Crouch, A.; Perez, A.B.; Merritt, R.; et al. Out-of-hospital cardiac arrest surveillance–Cardiac Arrest Registry to Enhance Survival (CARES), United States, 1 October 2005–31 December 2010. MMWR Surveill. Summ. 2011, 60, 1–19. [Google Scholar]
- Song, K.J.; Shin, S.D.; Park, C.B.; Kim, J.Y.; Kim, D.K.; Kim, C.H.; Ha, S.Y.; Eng Hock Ong, M.; Bobrow, B.J.; McNally, B. Dispatcher-assisted bystander cardiopulmonary resuscitation in a metropolitan city: A before-after population-based study. Resuscitation 2014, 85, 34–41. [Google Scholar] [CrossRef]
- Ro, Y.S.; Shin, S.D.; Song, K.J.; Lee, E.J.; Kim, J.Y.; Ahn, K.O.; Chung, S.P.; Kim, Y.T.; Hong, S.O.; Choi, J.A.; et al. A trend in epidemiology and outcomes of out-of-hospital cardiac arrest by urbanization level: A nationwide observational study from 2006 to 2010 in South Korea. Resuscitation 2013, 84, 547–557. [Google Scholar] [CrossRef]
- Ro, Y.S.; Shin, S.D.; Lee, Y.J.; Lee, S.C.; Song, K.J.; Ryoo, H.W.; Ong, M.E.H.; McNally, B.; Bobrow, B.; Tanaka, H.; et al. Effect of Dispatcher-Assisted Cardiopulmonary Resuscitation Program and Location of Out-of-Hospital Cardiac Arrest on Survival and Neurologic Outcome. Ann. Emerg. Med. 2017, 69, 52–61.e51. [Google Scholar] [CrossRef]
- Ng, Y.Y.; Wah, W.; Liu, N.; Zhou, S.A.; Ho, A.F.; Pek, P.P.; Shin, S.D.; Tanaka, H.; Khunkhlai, N.; Lin, C.H.; et al. Associations between gender and cardiac arrest outcomes in Pan-Asian out-of-hospital cardiac arrest patients. Resuscitation 2016, 102, 116–121. [Google Scholar] [CrossRef] [PubMed]
- Ong, M.E.; Shin, S.D.; De Souza, N.N.; Tanaka, H.; Nishiuchi, T.; Song, K.J.; Ko, P.C.; Leong, B.S.; Khunkhlai, N.; Naroo, G.Y.; et al. Outcomes for out-of-hospital cardiac arrests across 7 countries in Asia: The Pan Asian Resuscitation Outcomes Study (PAROS). Resuscitation 2015, 96, 100–108. [Google Scholar] [CrossRef] [PubMed]
- Fosbol, E.L.; Dupre, M.E.; Strauss, B.; Swanson, D.R.; Myers, B.; McNally, B.F.; Anderson, M.L.; Bagai, A.; Monk, L.; Garvey, J.L.; et al. Association of neighborhood characteristics with incidence of out-of-hospital cardiac arrest and rates of bystander-initiated CPR: Implications for community-based education intervention. Resuscitation 2014, 85, 1512–1517. [Google Scholar] [CrossRef] [PubMed]
- Freire-Tellado, M.; Navarro-Paton, R.; Mateos-Lorenzo, J.; Vazquez-Corveiras, C.J. Should Public Access Automated external defibrillators be used in all unresponsive patients to avoid an undetected Out-of-hospital cardiac arrest (OHCA)? Am. J. Emerg. Med. 2018, 36, 723–724. [Google Scholar] [CrossRef] [PubMed]
- Lwanga, A.; Garcia-Sayan, E.; Lwanga, S.; Karreman, E.; Mohamed, A. Automated External Defibrillators and Survival After Nonresidential Out of Hospital Cardiac Arrest in a Small North American City. Am. J. Cardiol. 2017, 119, 1979–1982. [Google Scholar] [CrossRef] [PubMed]
- Alten, J.A.; Klugman, D.; Raymond, T.T.; Cooper, D.S.; Donohue, J.E.; Zhang, W.; Pasquali, S.K.; Gaies, M.G. Epidemiology and Outcomes of Cardiac Arrest in Pediatric Cardiac ICUs. Pediatr. Crit. Care Med. 2017, 18, 935–943. [Google Scholar] [CrossRef] [PubMed]
- Irfan, F.B.; Bhutta, Z.A.; Castren, M.; Straney, L.; Djarv, T.; Tariq, T.; Thomas, S.H.; Alinier, G.; Al Shaikh, L.; Owen, R.C.; et al. Epidemiology and outcomes of out-of-hospital cardiac arrest in Qatar: A nationwide observational study. Int. J. Cardiol. 2016, 223, 1007–1013. [Google Scholar] [CrossRef]
- Luc, G.; Baert, V.; Escutnaire, J.; Genin, M.; Vilhelm, C.; Di Pompeo, C.; Khoury, C.E.; Segal, N.; Wiel, E.; Adnet, F.; et al. Epidemiology of out-of-hospital cardiac arrest: A French national incidence and mid-term survival rate study. Anaesth. Crit. Care Pain Med. 2019, 38, 131–135. [Google Scholar] [CrossRef]
- Refaat, M.M.; Kozhaya, K.; Abou-Zeid, F.; Abdulhai, F.; Faour, K.; Mourani, S.C.; Abi-Gerges, C.; Bachir, R.; Musharrafieh, U.; El Sayed, M. Epidemiology, etiology, and outcomes of out-of-hospital cardiac arrest in young patients in lebanon. Pacing Clin. Electrophysiol. 2019, 42, 1390–1395. [Google Scholar] [CrossRef]
- Lee, M.J.; Rho, T.H.; Kim, H.; Kang, G.H.; Kim, J.S.; Rho, S.G.; Park, H.K.; Oh, D.J.; Oh, S.; Wi, J.; et al. Part 3. Advanced cardiac life support: 2015 Korean Guidelines for Cardiopulmonary Resuscitation. Clin. Exp. Emerg. Med. 2016, 3, S17–S26. [Google Scholar] [CrossRef]
- Seo, E.C. The Poblems and Their Solutions of Emgercy Medical Service in South Korea; National Assembly Research Service: Seoul, South Korea, 2020. [Google Scholar]
- Medar, S.; Cassel-Choudhury, G.; Weingarten-Arams, J.; Ushay, H.M. Preventing Cardiac Arrest in a Pediatric Cardiac ICU-Situational Awareness and Early Intervention Work Together! Crit. Care Med. 2020, 48, 1093–1095. [Google Scholar] [CrossRef] [PubMed]
- Pruitt, C.M. Pediatric out-of-hospital cardiac arrest: More common than we thought? Resuscitation 2020, 153, 32485188. [Google Scholar] [CrossRef]
- Silka, M.J.; Hill, A.C. Pediatric unexplained cardiac arrest: When no answer is also an answer. Heart Rhythm 2020, 17, 982–983. [Google Scholar] [CrossRef]
- Fuller, S.; Rajagopalan, R.; Jarvik, G.P.; Gerdes, M.; Bernbaum, J.; Wernovsky, G.; Clancy, R.R.; Solot, C.; Nicolson, S.C.; Spray, T.L.; et al. J. Maxwell Chamberlain Memorial Paper for congenital heart surgery. Deep hypothermic circulatory arrest does not impair neurodevelopmental outcome in school-age children after infant cardiac surgery. Ann. Thorac. Surg. 2010, 90, 1985–1994. [Google Scholar] [CrossRef] [PubMed]
- Mitani, Y.; Ohta, K.; Yodoya, N.; Otsuki, S.; Ohashi, H.; Sawada, H.; Nagashima, M.; Sumitomo, N.; Komada, Y. Public access defibrillation improved the outcome after out-of-hospital cardiac arrest in school-age children: A nationwide, population-based, Utstein registry study in Japan. Europace 2013, 15, 1259–1266. [Google Scholar] [CrossRef] [PubMed]
- Cortes, M.; Roldan, C.A.; Clegg, S. Unusual congenital coronary artery anomaly in a young adult presenting as sudden cardiac arrest. BMJ Case Rep. 2018. [Google Scholar] [CrossRef]
- Topaz, O.; Perin, E.; Cox, M.; Mallon, S.M.; Castellanos, A.; Myerburg, R.J. Young adult survivors of sudden cardiac arrest: Analysis of invasive evaluation of 22 subjects. Am. Heart J. 1989, 118, 281–287. [Google Scholar] [CrossRef]
- Zhu, K.F.; Tang, L.J.; Wu, S.Z.; Tang, Y.M. Out-of-hospital cardiac arrest in a young adult survivor with sequelae of childhood Kawasaki disease: A case report. World J. Clin. Cases 2019, 7, 3583–3589. [Google Scholar] [CrossRef]
- Dyson, K.; Brown, S.P.; May, S.; Smith, K.; Koster, R.W.; Beesems, S.G.; Kuisma, M.; Salo, A.; Finn, J.; Sterz, F.; et al. International variation in survival after out-of-hospital cardiac arrest: A validation study of the Utstein template. Resuscitation 2019, 138, 168–181. [Google Scholar] [CrossRef]
- Balan, P.; Hsi, B.; Thangam, M.; Zhao, Y.; Monlezun, D.; Arain, S.; Charitakis, K.; Dhoble, A.; Johnson, N.; Anderson, H.V.; et al. The cardiac arrest survival score: A predictive algorithm for in-hospital mortality after out-of-hospital cardiac arrest. Resuscitation 2019, 144, 46–53. [Google Scholar] [CrossRef]
- Ji, C.; Brown, T.P.; Booth, S.J.; Hawkes, C.; Nolan, J.P.; Mapstone, J.; Fothergill, R.T.; Spaight, R.; Black, S.; Perkins, G.D.; et al. Risk Prediction Models for Out-of-Hospital Cardiac Arrest Outcomes in England. Eur. Heart J. Qual Care Clin. Outcomes 2020. [Google Scholar] [CrossRef] [PubMed]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).