Poor Sleep Quality, Depression and Social Support Are Determinants of Serum Phosphate Level among Hemodialysis Patients in Malaysia
Abstract
1. Introduction
2. Materials and Methods
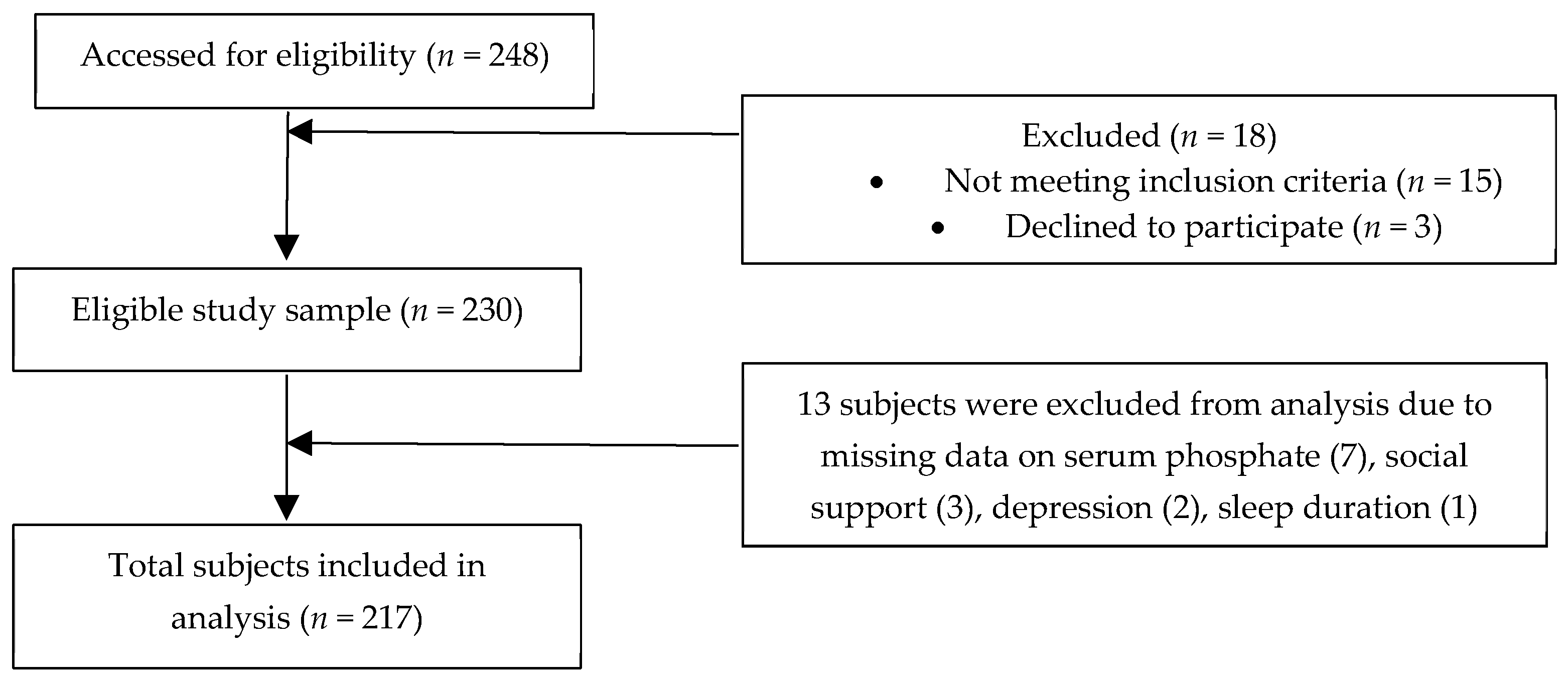
2.1. Subjects
2.2. Instrumentation
2.3. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Eknoyan, G.; Lameire, N.; Barsoum, R.; Eckardt, K.U.; Levin, A.; Levin, N.; Locatelli, F.; MacLeod, A.; Vanholder, R.; Walker, R.; et al. The burden of kidney disease: Improving global outcomes. Kidney Int. 2004, 66, 1310–1314. [Google Scholar] [CrossRef] [PubMed]
- National Kidney Foundation. Global Facts: About Kidney Disease—The National Kidney Foundation. Available online: https://www.kidney.org/kidneydisease/global-facts-about-kidney-disease (accessed on 7 April 2020).
- Wang, H.; Naghavi, M.; Allen, C.; Barber, R.M.; Bhutta, Z.A.; Carter, A.; Casey, D.C.; Charlson, F.J.; Chen, A.Z.; Coates, M.M.; et al. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1459–1544. [Google Scholar] [CrossRef]
- Friedman, E.L.I.A. Consequences and management of hyperphosphatemia in patients with renal insufficiency. Kidney Int. 2005, 67, S1–S7. [Google Scholar] [CrossRef]
- Chiroli, S.; Mattin, C.; Belozeroff, V.; Perrault, L.; Mitchell, D.; Gioni, I. Impact of mineral and bone disorder on healthcare resource use and associated costs in the European Fresenius medical care dialysis population: A retrospective cohort study. BMC Nephrol. 2012, 13, 140. [Google Scholar] [CrossRef]
- Kutner, N.G. Improving compliance in dialysis patients: Does anything work? Semin. Dial. 2001, 14, 324–327. [Google Scholar] [CrossRef] [PubMed]
- D’Alessandro, C.; Piccoli, G.B.; Cupisti, A. The “Phosphorous Pyramid”: A Visual Tool for Dietary Phosphate Management in Dialysis and CKD Patients. BMC Nephrol. 2015, 16, 9. [Google Scholar] [CrossRef]
- Port, F.K.; Pisoni, R.L.; Bommer, J.; Locatelli, F.; Jadoul, M.; Eknoyan, G.; Kurokawa, K.; Canaud, B.J.; Finley, M.P.; Young, E.W. Improving outcomes for dialysis patients in the international dialysis outcomes and practice patterns study. Clin. J. Am. Soc. Nephrol. 2006, 1, 246–255. [Google Scholar] [CrossRef]
- Ibrahim, S.; Hossam, M.; Belal, D. Study of Non-Compliance among Chronic Hemodialysis Patients and its Impact on Patients’ Outcomes. Saudi J. Kidney Dis. Transpl. 2015, 26, 243–249. [Google Scholar] [CrossRef]
- Correa, D.; Kruger, T.S.; Sczip, A.C.; Vieira, M.A.; Morais, J.G. Perceptions of hemodialysis patients about dietary and fluid restrictions. J. Bras. Nefrol. 2017, 39, 154–161. [Google Scholar]
- Chan, Y.M.; Zalilah, M.S.; Hii, S.Z. Determinants of Compliance Behaviours among Patients Undergoing Hemodialysis in Malaysia. PLoS ONE 2012, 7, e41362. [Google Scholar] [CrossRef] [PubMed]
- Victoria, A.; Evangelos, F.; Sofia, Z. Family support, social and demographic correlations of non-adherence among haemodialysis patients. Am. J. Nurs. Sci. 2015, 4, 60–65. [Google Scholar] [CrossRef][Green Version]
- Martin, L.R.; Williams, S.L.; Haskard, K.B.; Dimatteo, M.R. The challenge of patient adherence. Ther. Clin. Risk Manag. 2005, 1, 189–199. [Google Scholar] [PubMed]
- Rosenthal Asher, D.; Ver Halen, N.; Cukor, D. Depression and nonadherence predict mortality in hemodialysis treated end-stage renal disease patients. Hemodial. Int. 2012, 6, 387–393. [Google Scholar]
- Cohen, S.D.; Sharma, T.; Acquaviva, K.; Peterson, R.A.; Patel, S.S.; Kimmel, P.L. Social Support and Chronic Kidney Disease: An Update. Adv. Chronic Kidney Dis. 2007, 14, 335–344. [Google Scholar] [CrossRef]
- Untas, A.; Thumma, J.; Rascle, N.; Rayner, H.; Mapes, D.; Lopes, A.A.; Fukuhara, S.; Akizawa, T.; Morgenstern, H.; Robinson, B.M.; et al. The associations of social support and other psychosocial factors with mortality and quality of life in the dialysis outcomes and practice patterns study. Clin. J. Am. Soc. Nephrol. 2011, 6, 142–152. [Google Scholar] [CrossRef]
- Waheed, A.A.; Pedraza, F.; Lenz, O.; Isakova, T. Phosphate control in end-stage renal disease: Barriers and opportunities. Nephrol. Dial. Transplant. 2013, 28, 2961–2968. [Google Scholar] [CrossRef]
- Van Camp, Y.P.M.; Vrijens, B.; Abraham, I.; Van Rompaey, B.; Elseviers, M.M. Adherence to phosphate binders in hemodialysis patients: Prevalence and determinants. J. Nephrol. 2014, 27, 673–679. [Google Scholar] [CrossRef]
- Pollock, J.B.; Jaffery, J.B. Knowledge of Phosphorus Compared with Other Nutrients in Maintenance Dialysis Patients. J. Ren. Nutr. 2007, 17, 323–328. [Google Scholar] [CrossRef]
- Elder, S.J.; Pisoni, R.L.; Akizawa, T.; Fissell, R.; Andreucci, V.E.; Fukuhara, S.; Kurokawa, K.; Rayner, H.C.; Furniss, A.L.; Port, F.K.; et al. Sleep quality predicts quality of life and mortality risk in haemodialysis patients: Results from the Dialysis Outcomes and Practice Patterns Study (DOPPS). Nephrol. Dial. Transplant. 2008, 23, 998–1004. [Google Scholar] [CrossRef]
- Ezzat, H.; Mohab, A. Prevalence of sleep disorders among ESRD patients. Ren. Fail. 2015, 37, 1013–1019. [Google Scholar] [CrossRef]
- Durose, C.L.; Holdsworth, M.; Watson, V.; Przygrodzka, F. Knowledge of Dietary Restrictions and the Medical Consequences of Noncompliance by Patients on Hemodialysis Are Not Predictive of Dietary Compliance. J. Am. Diet. Assoc. 2004, 104, 35–41. [Google Scholar] [CrossRef] [PubMed]
- Thong, M.S.Y.; Kaptein, A.A.; Krediet, R.T.; Boeschoten, E.W.; Dekker, F.W. Social support predicts survival in dialysis patients. Nephrol. Dial. Transplant. 2007, 22, 845–850. [Google Scholar] [CrossRef]
- Unruh, M.L.; Hartunian, M.G.; Chapman, M.M.; Jaber, B.L. Sleep quality and clinical correlates in patients on maintenance dialysis. Clin. Nephrol. 2003, 59, 280–288. [Google Scholar] [CrossRef] [PubMed]
- Chan, Y.M.; Zalilah, M.S.; Lim, C.T.S.; Goh, B.L. Factors associated with poor nutritional status Among hemodialysis patients in Malaysia. Mal. J. Med. Health Sci. 2019, 15, 77–83. [Google Scholar]
- Nor Baizura, M.Y.; Chan, Y.M.; Zalilah, M.S.; Choo, B.H. Factors associated with quality of life among hemodialysis patients in Malaysia. PLoS ONE 2013, 8, e84152. [Google Scholar] [CrossRef]
- Umeukeje, E.M.; Mixon, A.S.; Cavanaugh, K.L. Phosphate-control adherence in hemodialysis patients: Current perspectives. Patient Prefer. Adherence 2018, 4, 1175–1191. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.T.; Steer, R.A.; Garbin, M.G. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clin. Psychol. Rev. 1988, 8, 77–100. [Google Scholar] [CrossRef]
- Watnick, S.; Wang, P.L.; Demadura, T.; Ganzini, L. Validation of 2 depression screening tools in dialysis patients. Am. J. Kidney Dis. 2005, 46, 919–924. [Google Scholar] [CrossRef]
- Zimet, G.D.; Dahlem, N.W.; Zimet, S.G.; Farley, F.G. The Multidimensional Scale of Perceived Social Support. J. Pers. Assess. 1988, 52, 30–41. [Google Scholar] [CrossRef]
- Knobel, H.; Alonso, J.; Casado, J.L.; Collazos, J.; González, J.; Ruiz, I.; Kindelan, J.M.; Carmona, A.; Juega, J.; Ocampo, A.; et al. Validation of a simplified medication adherence questionnaire in a large cohort of HIV-infected patients: The GEEMA Study. AIDS 2002, 16, 605–613. [Google Scholar] [CrossRef]
- Karavetian, M.; Abboud, S.; Elzein, H.; Haydar, S.; de Vries, N. Nutritional education for management of osteodystrophy (NEMO) trial: Design and patient characteristics, Lebanon. Nutr. Res. Pract. 2014, 8, 103–111. [Google Scholar] [CrossRef] [PubMed]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Ministry of Health Malaysia. Clinical Practice Guidelines: Renal Replacement Therapy, 4th ed.; Post Graduate Renal Society of Malaysia: Kuala Lumpur, Malaysia, 2017. [Google Scholar]
- IBM Corp. IBM SPSS Statistics for Windows, Version 24.0; IBM Corp: Armonk, NY, USA, 2016. [Google Scholar]
- Hosmer, D.W.; Lemeshow, S. Applied Logistic Regression, 2nd ed.; John Wiley & Sons Inc.: New York, NY, USA, 2000. [Google Scholar]
- Morton, R.L.; Da Silva-Gane, M.; Cass, A.; Patterson, K.; Yip, A.C.W.; Handke, W.A.; Webster, A.C. Interventions to aid employment for people on dialysis and their families. Cochrane Database Syst. Rev. 2017, 2017, CD012702. [Google Scholar] [CrossRef]
- Jones, D.J.W.; Harvey, K.; Harris, J.P.; Butler, L.T.; Vaux, E.C. Understanding the impact of haemodialysis on UK National Health Service patients’ well-being: A qualitative investigation. J. Clin. Nurs. 2018, 27, 193–204. [Google Scholar] [CrossRef] [PubMed]
- Tang, C.H.; Chen, H.H.; Wu, M.J.; Hsu, B.G.; Tsai, J.C.; Kuo, C.C.; Lin, S.P.; Chen, T.H.; Sue, Y.M. Out-of-pocket costs and productivity losses in haemodialysis and peritoneal dialysis from a patient interview survey in Taiwan. BMJ Open 2019, 9, e023062. [Google Scholar] [CrossRef] [PubMed]
- Yang, F.; Lau, T.; Luo, N. Cost-effectiveness of haemodialysis and peritoneal dialysis for patients with end-stage renal disease in Singapore. Nephrology 2016, 21, 669–677. [Google Scholar] [CrossRef]
- Cukor, D.; Coplan, J.; Brown, C.; Friedman, S.; Cromwell-Smith, A.; Peterson, R.A.; Kimmel, P.L. Depression and anxiety in urban hemodialysis patients. Clin. J. Am. Soc. Nephrol. 2007, 2, 484–490. [Google Scholar] [CrossRef]
- Bujang, M.A.; Musa, R.; Liu, W.J.; Chew, T.F.; Lim, C.T.S.; Morad, Z. Depression, anxiety and stress among patients with dialysis and the association with quality of life. Asian J. Psychiatr 2015, 18, 49–52. [Google Scholar] [CrossRef]
- Khalil, A.A.; Darawad, M.; Al Gamal, E.; Hamdan-Mansour, A.M.; Abed, M.A. Predictors of dietary and fluid non-adherence in Jordanian patients with end-stage renal disease receiving haemodialysis: A cross-sectional study. J. Clin. Nurs. 2013, 22, 127–136. [Google Scholar] [CrossRef]
- Al Dukhayel, A. Prevalence of Depressive Symptoms among Hemodialysis and Peritoneal Dialysis Patients. Int. J. Health Sci. (Qassim) 2015, 9, 9–16. [Google Scholar] [CrossRef]
- Nelson, V.; Gopalakrishnan, S.; Rakesh, P.S.; Simon, S.; Babu, V.; Vikraman, V.; Abraham, S.; Mohammaed, Y. Depression Among Dialysis Patients. J. Nephrol. Soc. Work. 2008, 40, 34–37. [Google Scholar]
- Čengić, B.; Resić, H. Depression in Hemodialysis Patients. Bosn. J. Basic Med. Sci. 2017, 10, S73–S78. [Google Scholar] [CrossRef] [PubMed]
- Kimmel, P.L.P. Psychosocial factors in adult end-stage renal disease patients treated with hemodialysis: Correlates and outcomes. Am. J. Kidney Dis. 2000, 35, 132–140. [Google Scholar] [CrossRef]
- Cukor, D.; Peterson, R.A.; Cohen, S.D.; Kimmel, P.L. Depression in end-stage renal disease hemodialysis patients. Nat. Clin. Pract. Nephrol. 2006, 2, 678–687. [Google Scholar] [CrossRef]
- Shirazian, S.; Grant, C.D.; Aina, O.; Mattana, J.; Khorassani, F.; Ricardo, A.C. Depression in Chronic Kidney Disease and End-Stage Renal Disease: Similarities and Differences in Diagnosis, Epidemiology, and Management. Kidney Int. Rep. 2017, 2, 94–107. [Google Scholar] [CrossRef] [PubMed]
- Rambod, M.; Rafii, F. Perceived Social Support in Hemodialysis Patients. Iran. J. Nurs. 2009, 22, 99–110. [Google Scholar]
- Theodoritsi, A.; Aravantinou, M.E.; Gravani, V.; Bourtsi, E.; Vasilopoulou, C.; Theofilou, P.; Polikandrioti, M. Factors Associated with the Social Support of Hemodialysis Patients. Iran. J. Public Health 2016, 45, 1261–1269. [Google Scholar] [PubMed]
- Bayat, A.; Kazemi, R.; Toghiani, A.; Mohebi, B.; Tabatabaee, M.N.; Adibi, N. Psychological evaluation in hemodialysis patients. J. Pak. Med. Assoc. 2012, 62, S1–S5. [Google Scholar]
- Lilympaki, I.; Makri, A.; Vlantousi, K.; Koutelekos, I.; Babatsikou, F.; Polikandrioti, M. Effect of perceived social support on the levels of anxiety and depression of hemodialysis patients. Mater. Sociomed. 2016, 28, 361–365. [Google Scholar] [CrossRef]
- Isakova, T.; Nickolas, T.L.; Denburg, M.; Yarlagadda, S.; Weiner, D.E. KDOQI Commentary KDOQI US Commentary on the 2017 KDIGO Clinical Practice Guideline Update for the Diagnosis, Evaluation, Prevention, and Treatment of Chronic Kidney Disease—Mineral and Bone Disorder (CKD-MBD). Am. J. Kidney Dis. 2017, 70, 737–751. [Google Scholar] [CrossRef]
- Karamanidou, C.; Clatworthy, J.; Weinman, J.; Horne, R. A systematic review of the prevalence and determinants of end-stage renal disease. BMC Nephrol. 2008, 10, 1–10. [Google Scholar]
- Ossareh, S.; Tabrizian, S.; Zebarjadi, M. Prevalence of Depression in Maintenance Hemodialysis Patients and Its Correlation with Adherence to Medications. Iran. J. Kidney Dis. 2014, 8, 467–475. [Google Scholar] [PubMed]
- Covic, A.; Rastogi, A. Hyperphosphatemia in patients with ESRD: Assessing the current evidence linking outcomes with treatment adherence. BMC Nephrol. 2013, 14, 153. [Google Scholar] [CrossRef] [PubMed]
- Ghimire, S.; Castelino, R.L.; Lioufas, N.M.; Peterson, G.M. Nonadherence to Medication Therapy in Haemodialysis Patients: A Systematic Review. PLoS ONE 2015, 10, e0144119. [Google Scholar] [CrossRef]
- Chan, S.; Au, K.; Francis, R.S.; Mudge, D.W.; Johnson, D.W.; Pillans, P.I. Phosphate binders in patients with chronic kidney disease. Aust. Prescr. 2017, 40, 10–14. [Google Scholar] [CrossRef]
- Arenas, M.D.; Malek, T.; Gil, M.T.; Moledous, A.; Alvarez-Ude, F.; Reig-Ferrer, A. Challenge of phosphorus control in hemodialysis patients: A problem of adherence? J. Nephrol. 2010, 23, 525–534. [Google Scholar]
- Alshamrani, M.; Almalki, A.; Qureshi, M.; Yusuf, O.; Ismail, S. Polypharmacy and Medication-Related Problems in Hemodialysis Patients: A Call for Deprescribing. Pharmacy 2018, 6, 76. [Google Scholar] [CrossRef]
- Schmidt, I.M.; Hübner, S.; Nadal, J.; Titze, S.; Schmid, M.; Bärthlein, B.; Schlieper, G.; Dienemann, T.; Schultheiss, U.T.; Meiselbach, H.; et al. Patterns of medication use and the burden of polypharmacy in patients with chronic kidney disease: The German Chronic Kidney Disease study. Clin. Kidney J. 2019, 12, 663–672. [Google Scholar] [CrossRef]
- Schoenthaler, M.A.; Lancaster, K.J.; Chaplin, W.; Butler, M.; Forsyth, J.; Ogedegbe, G. Cluster Randomized Clinical Trial of FAITH (Faith-Based Approaches in the Treatment of Hypertension) in Blacks. Circ. Cardiovasc. Qual. Outcomes 2018, 11, e004691. [Google Scholar] [CrossRef]
- Churillo, T.O. Medication Reminder Systems: An Adjunct Technique in Improving Phosphate Binder. J. Ren. Nutr. 2012, 22, e3–e9. [Google Scholar] [CrossRef]
- Pafili, Z.; Maridaki, M.; Giannaki, C.; Karatzaferi, C.; Liakopoulos, V.; Eleftheriadis, T.; Stefanidis, I.; Sakkas, G.K. Phosphorus nutritional knowledge among dialysis health care providers and patients: A multicenter observational study. Clin. Nutr. ESPEN 2019, 31, 33–37. [Google Scholar] [CrossRef]
- Collinson, A.; McMullan, M.; Tse, W.Y.; Sadler, H. Managing serum phosphate in haemodialysis patients: Time for an innovative approach? Eur. J. Clin. Nutr. 2014, 68, 392–396. [Google Scholar] [CrossRef]
- Cupisti, A.; Ferretti, V.; D’Alessandro, C.; Petrone, I.; Di Giorgio, A.; Meola, M.; Panichi, V.; Conti, P.; Lippi, A.; Caprioli, R.; et al. Nutritional Knowledge in Hemodialysis Patients and Nurses: Focus on Phosphorus. J. Ren. Nutr. 2012, 22, 541–546. [Google Scholar] [CrossRef]
- Ford, J.C.; Pope, J.F.; Hunt, A.E.; Gerald, B. The effect of diet education on the laboratory values and knowledge of hemodialysis patients with hyperphosphatemia. J. Ren. Nutr. 2004, 14, 36–44. [Google Scholar] [CrossRef]
- Reddy, V.; Symes, F.; Sethi, N.; Scally, A.J.; Scott, J.; Mumtaz, R.; Stove, R. Dietitian-Led Education Program to Improve Phosphate Control in a Single-Center Hemodialysis Population. J. Ren. Nutr. 2009, 19, 314–320. [Google Scholar] [CrossRef]
- Shaw-Stuart, N.J.; Stuart, A. The effect of an educational patient compliance program on serum phosphate levels in patients receiving hemodialysis. J. Ren. Nutr. 2000, 10, 80–84. [Google Scholar] [CrossRef]
- Lim, E.; Hyun, S.; Lee, J.M.; Kim, S.; Lee, M.J.; Lee, S.M.; Lim, E.; Hyun, S.; Lee, J.M.; Kim, S.; et al. Effects of education on low-phosphate diet and phosphate binder intake to control serum phosphate among maintenance hemodialysis patients: A randomized controlled trial. Kidney Res. Clin. Pract. 2018, 37, 69–76. [Google Scholar] [CrossRef]
- Karavetian, M.; Rizk, R. Patient education for hyperphosphatemia management: Improving outcomes while decreasing costs? Kidney Res. Clin. Pract. 2018, 37, 4–7. [Google Scholar] [CrossRef] [PubMed]
- Matteson, M.L.; Russell, C. Interventions to improve hemodialysis adherence: A systematic review of randomized-controlled trials. Hemodial. Int. 2010, 14, 370–382. [Google Scholar] [CrossRef] [PubMed]
- Russell, C.L.; Cronk, N.J.; Herron, M.; Knowles, N.; Matteson, M.L.; Peace, L.; Ponferrada, L. Motivational Interviewing in Dialysis Adherence Study (MIDAS). Nephrol. Nurs. J. 2011, 38, 229–236. [Google Scholar] [PubMed]
- Ekramzadeh, M.; Mazloom, Z.; Jafari, P.; Ayatollahi, M.; Sagheb, M.M. Major Barriers Responsible for Malnutrition in Hemodialysis Patients: Challenges to Optimal Nutrition. Nephrourol. Mon. 2014, 6, e23158. [Google Scholar] [CrossRef] [PubMed]
- Montazeri, R.S.; Sharifi, N. Evaluation of Nutritional Knowledge in Terms of Dietary Sources of Protein, Phosphorous, Potassium and Fluids Restriction in Hemodialysis Patients. Jentashapir J. Heal. Res. 2014, 5. [Google Scholar] [CrossRef]
- Kalantar-Zadeh, K.; Gutekunst, L.; Mehrotra, R.; Kovesdy, C.P.; Bross, R.; Shinaberger, C.S.; Noori, N.; Hirschberg, R.; Benner, D.; Nissenson, A.R.; et al. Understanding sources of dietary phosphorus in the treatment of patients with chronic kidney disease. Clin. J. Am. Soc. Nephrol. 2010, 5, 519–530. [Google Scholar] [CrossRef] [PubMed]
- Kalantar-Zadeh, K. Patient education for phosphorus management in chronic kidney disease. Patient Prefer. Adherence 2013, 7, 379–390. [Google Scholar] [CrossRef]
- Kugler, C.; Vlaminck, H.; Haverich, A.; Maes, B. Nonadherence with Diet and Fluid Restrictions Receiving Hemodialysis. J. Nurs. Scholarsh. 2005, 37, 25–29. [Google Scholar] [CrossRef]
- Baraz, S.; Parvardeh, S.; Mohammadi, E.; Broumand, B. Dietary and fluid compliance: An educational intervention for patients having haemodialysis. J. Adv. Nurs. 2010, 66, 60–68. [Google Scholar] [CrossRef]
- Youngmee, K.; Evangelista, L.S. Relationship between Illness Perceptions, Treatment Adherence, and Clinical Outcomes in Patients on Maintenance Hemodialysis. Nephrol. Nurs. J. 2010, 37, 271–281. [Google Scholar]
- Ahrari, S.; Moshki, M.; Bahrami, M. The Relationship Between Social Support and Adherence of Dietary and Fluids Restrictions among Hemodialysis Patients in Iran. J. Caring Sci. 2014, 3, 11–19. [Google Scholar]
- Park, K.A.; Choi-Kwon, S.; Sim, Y.M.; Kim, S.B. Comparison of Dietary Compliance and Dietary Knowledge Between Older and Younger Korean Hemodialysis Patients. J. Ren. Nutr. 2008, 18, 415–423. [Google Scholar] [CrossRef]
- Clark-Cutaia, M.N.; Dianxu, R. Adherence to Hemodialysis Dietary Sodium Recommendations: Influence of Patien Characteristics, Self-Efficacy and Perceived Barriers. J. Ren. Nutr. 2012, 76, 211–220. [Google Scholar] [CrossRef]
- Laurain, E.; Thilly, N.; Boini, S.; Kessler, M.; Briancon, S.; Frimat, L. Hyperphosphatemia in chronic kidney disease: Patient characteristics and dialysis mortality during the first year of dialysis. J. Nephrol. Ther. 2012, S3, 009. [Google Scholar] [CrossRef]
- Block, G.A.; Klassen, P.S.; Lazarus, J.M.; Ofsthun, N.; Lowrie, E.G.; Chertow, G.M. Mineral metabolism, mortality, and morbidity in maintenance hemodialysis. J. Am. Soc. Nephrol. 2004, 15, 2208–2218. [Google Scholar] [CrossRef] [PubMed]
- Lam, L.W.; Twinn, S.F.; Chan, S.W. Self-reported adherence to therapeutic regimen among patients undergoing continuous ambulatory peritoneal dialysis. J. Adv. Nurs. 2010, 66, 763–773. [Google Scholar] [CrossRef] [PubMed]
- Ix, J.H.; De Boer, I.H.; Peralta, C.A.; Adeney, K.L.; Duprez, D.A.; Jenny, N.S.; Siscovick, D.S.; Kestenbaum, B.R. Serum phosphorus concentrations and arterial stiffness among individuals with normal kidney function to moderate kidney disease in MESA. CJASN 2009, 4, 609–615. [Google Scholar] [CrossRef]
- Van Kuijk, J.P.; Flu, W.J.; Chonchol, M.; Valentijn, T.M.; Verhagen, H.J.; Bax, J.J.; Poldermans, D. Elevated preoperative phosphorus levels are an independent risk factor for cardiovascular mortality. Am. J. Nephrol. 2010, 32, 163–168. [Google Scholar] [CrossRef]
- Naves-Díaz, M.; Passlick-Deetjen, J.; Guinsburg, A.; Marelli, C.; Fernández-Martín, J.L.; Rodríguez-Puyol, D.; Cannata-Andía, J.B. Calcium, phosphorus, PTH and death rates in a large sample of dialysis patients from Latin America. The CORES Study. Nephrol. Dial. Transplant. 2011, 26, 1938–1947. [Google Scholar] [CrossRef]
- Imtiaz, R.; Hawken, S.; McCormick, B.B.; Leung, S.; Hiremath, S.; Zimmerman, D.L. Diabetes Mellitus and Younger Age Are Risk Factors for Hyperphosphatemia in Peritoneal Dialysis Patients. Nutrients 2017, 9. [Google Scholar] [CrossRef]
- Han, B.; Zhu, F.X.; Shi, C.; Wu, H.L.; Gu, X.H. Association between Serum Vitamin D Levels and Sleep Disturbance in Hemodialysis Patients. Nutrients 2017, 9, 139. [Google Scholar] [CrossRef] [PubMed]
- Mehrabi, S.; Sarikhani, S.; Roozbeh, J. Sleep Quality in Patients Undergoing Long-term Hemodialysis Using the Pittsburgh Sleep Quality Index. Nephrourol. Mon. 2017, 9, e13137. [Google Scholar] [CrossRef]
- Acar, D.; Güneş, Z. Factors affecting therapeutic compliance in patients with chronic renal failure: Anxiety, Depression, İllness Perception. Health Prim. Care 2018, 2. [Google Scholar] [CrossRef]
- Bezerra, C.I.L.; Silva, B.C.; Elias, R.M. Decision-making process in the pre-dialysis CKD patients: Do anxiety, stress and depression matter? BMC Nephrol. 2018, 19, 98. [Google Scholar] [CrossRef] [PubMed]
- Teles, F.; de Azevedo, V.; Miranda, C.; Miranda, M.; Teixeira, M.; Elias, R. Depression in hemodialysis patients: The role of dialysis shift. Clinics 2014, 69, 198–202. [Google Scholar] [CrossRef]
- Collister, D.; Rodrigues, J.C.; Mazzetti, A.; Salisbury, K.; Morosin, L.; Rabbat, C.; Brimble, K.S.; Walsh, M. Single Questions for the Screening of Anxiety and Depression in Hemodialysis. CJKHD 2019. [Google Scholar] [CrossRef]
- Alexopoulou, M.; Giannakopoulou, N.; Komna, E.; Alikari, V.; Toulia, G.; Polikandrioti, M. The Effect of Perceived Social Support on Hemodialysis Patients’ Quality of Life. Mater. Sociomed. 2016, 28, 338–342. [Google Scholar] [CrossRef] [PubMed]
- Plantinga, L.C.; Fink, N.E.; Harrington-Levey, R.; Finkelstein, F.O.; Hebah, N.; Powe, N.; Jaar, B.G. Association of social support with outcomes in incident dialysis patients. CJASN 2010, 5, 1480–1488. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | n (%) | Mean ± SD | Range | |
|---|---|---|---|---|
| Age | <60 years old | 121 (55.8) | 57 ± 13 | 24–80 |
| ≥60 years old | 96 (44.2) | |||
| Sex | Female | 110 (50.2) | ||
| Male | 108 (49.8) | |||
| Marital status | Single | 18 (8.3) | ||
| Married | 170 (78.3) | |||
| Divorced | 3 (1.4) | |||
| Widow/widower | 26 (12.0) | |||
| Educational level | No formal education | 4 (1.8) | ||
| Primary | 37 (17.1) | |||
| Secondary | 104 (47.9) | |||
| Tertiary | 72 (33.2) | |||
| Employment status | Employed | 51 (23.5) | ||
| Unemployed | 64 (29.5) | |||
| Retired | 102 (47.0) | |||
| Monthly Household income (RM) * | B40 (<3860) | 151 (69.6) | ||
| M40 (3860–8319) | 46 (21.2) | |||
| T20 (≥8320) | 20 (9.2) | |||
| Duration of dialysis (months) | 55.4 ± 48.7 | 3–360 | ||
| Presence of Comorbidities † | Hypertension | 176 (81.1) | ||
| Diabetes mellitus | 121 (55.8) | |||
| Total BDI Score | 5.76 ± 5.66 | 0.00–27.00 | ||
| Level of Depression | None or minimal | 165 (76.0) | ||
| Mild to moderate | 44 (20.3) | |||
| Moderate to severe | 8 (3.7) | |||
| Level of Social Support ‡ | Family | 190 (87.6) | ||
| Friends | 127 (58.5) | |||
| Significant others | 175 (80.6) | |||
| PSQI score | 6.15 ± 3.54 | |||
| Classification of Sleep Quality | Good sleepers | 104 (46.6) | ||
| Poor sleepers | 119 (53.4) | |||
| Duration of Sleep (hour/day) | <5 hour/day | 74 (34.1) | 5.6 ± 1.8 | |
| 5–6 hour/day | 45 (20.7) | |||
| 6–7 hour/day | 46 (21.2) | |||
| >7 hour /day | 52 (23.9) | |||
| Creatinine (µmol/L) | 950.6 ± 212.5 | 452.7–1021.5 | ||
| Serum alkaline phosphatase (units/L) | 385.0 ± 160.0 | 140–1120 | ||
| Corrected serum calcium (mmol/L) | Low (<2.10) | 36 (16.6) | 2.23 ± 0.24 | 1.65–2.77 |
| Normal (2.10–2.37) | 121 (55.8) | |||
| Elevated (>2.37) | 60 (27.6) | |||
| Intact parathyroid hormone (pg/mL) | <150 | 126 (58.1) | 248.5 ± 163.2 | 118–452 |
| 150–300 | 36 (16.6) | |||
| >300 | 55 (25.3) | |||
| Dialysis Adequacy (Kt/V) | <1.2 | 25 (11.5) | 1.42 ± 0.43 | 1.28–1.51 |
| >1.2 | 192 (88.5) | |||
| Serum phosphate (mmol/L) | Normal (<1.6) | 49 (22.6) | 1.83 ± 0.50 | 0.78–3.37 |
| Elevated (≥1.6) | 168 (77.4) | |||
| Missing of phosphate binders | Yes | 155 (71.4) | ||
| No | 62 (28.6) | |||
| Reasons of missing phosphate binders † | Careless | 138 (63.6) | ||
| Forgetful | 112 (51.6) | |||
| High tablet burden | 92 (42.4) | |||
| Gastrointestinal discomfort/Unpleasant taste | 87 (40.1) | |||
| Nutrition knowledge on phosphorus | <60% | 204 (94.0) | ||
| ≥60% | 13 (6.0) | |||
| Factors affecting optimal phosphate control † (patients’ perception) | Dialysis process alone | 183 (84.3) | ||
| Low phosphorus diet alone | 158 (72.8) | |||
| Phosphate binders alone | 116 (53.5) | |||
| All the above | 59 (27.2) |
| Variables | Simple Linear Regression | Multiple Linear Regression | ||
|---|---|---|---|---|
| Standardized Coefficients (β) | p | Standardized Coefficients (β) | p | |
| Dialysis adequacy (Kt/V) | −0.455 | 0.007 | −0.413 | 0.011 |
| Adherence on Phosphate binders | −0.442 | 0.012 | −0.368 | 0.021 |
| Age | −0.334 | 0.015 | −0.305 | 0.026 |
| Sleep Duration | −0.378 | 0.032 | −0.288 | 0.037 |
| Presence of diabetes mellitus | 0.326 | 0.035 | 0.272 | 0.038 |
| Presence of depression | −0.358 | 0.033 | −0.265 | 0.041 |
| Social Support | −0.152 | 0.154 | −0.141 | 0.044 |
| Employment status | −0.271 | 0.037 | - | - |
| Household income | 0.259 | 0.041 | - | - |
| Presence of hypertension | 0.189 | 0.056 | - | - |
| Duration of dialysis | 0.176 | 0.124 | - | |
| PSQI score | 0.130 | 0.274 | - | - |
| Nutritional knowledge on Phosphorus | −0.115 | 0.360 | - | - |
| Variables | n (%) | Serum Phosphate (mmol/L) Mean ± SD | t or F Value † |
|---|---|---|---|
| Dialysis adequacy (Kt/V) | |||
| <1.2 | 25 (11.5) | 2.18 ± 0.33 | 2.64 * |
| >1.2 | 192 (88.5) | 1.78 ± 0.24 | |
| Age (years) | |||
| <60 | 121 (55.8) | 1.93 ± 0.38 | 2.35 * |
| ≥60 | 96 (44.2) | 1.70 ± 0.61 | |
| Presence of Diabetes | |||
| Yes | 121 (55.8) | 1.89 ± 0.51 | 2.01 * |
| No | 96 (44.2) | 1.75 ± 0.54 | |
| Level of Depression ‡ | |||
| None or minimal | 165 (76.0) | 1.90 ± 0.59 a | 5.02 * |
| Mild to moderate | 44 (20.3) | 1.59 ± 0.60 b | |
| Moderate to severe | 8 (3.7) | 1.62 ± 0.45 b | |
| Level of Social Support ‡ | |||
| Low or Moderate# | 59 (27.2) | 1.99 ± 0.61 a | 2.12 * |
| High | 158 (72.8) | 1.77 ± 0.64 b | |
| Duration of Sleep (hour/day) ‡ | |||
| <5 | 74 (34.1) | 2.04 ± 0.53 a | 5.68 * |
| 5–6 | 45 (20.7) | 1.86 ± 0.48 b | |
| 6–7 | 46 (21.2) | 1.67 ± 0.48 c | |
| >7 | 52 (23.9) | 1.65 ± 0.51 c | |
| Adhered to phosphate binders | |||
| Yes | 62 (28.6) | 1.63 ± 0.46 | 2.48 * |
| No | 155 (71.4) | 1.91 ± 0.51 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ng, E.S.Y.; Wong, P.Y.; Kamaruddin, A.T.H.; Lim, C.T.S.; Chan, Y.M. Poor Sleep Quality, Depression and Social Support Are Determinants of Serum Phosphate Level among Hemodialysis Patients in Malaysia. Int. J. Environ. Res. Public Health 2020, 17, 5144. https://doi.org/10.3390/ijerph17145144
Ng ESY, Wong PY, Kamaruddin ATH, Lim CTS, Chan YM. Poor Sleep Quality, Depression and Social Support Are Determinants of Serum Phosphate Level among Hemodialysis Patients in Malaysia. International Journal of Environmental Research and Public Health. 2020; 17(14):5144. https://doi.org/10.3390/ijerph17145144
Chicago/Turabian StyleNg, Eileen Suk Ying, Poh Yoong Wong, Ahmad Teguh Hakiki Kamaruddin, Christopher Thiam Seong Lim, and Yoke Mun Chan. 2020. "Poor Sleep Quality, Depression and Social Support Are Determinants of Serum Phosphate Level among Hemodialysis Patients in Malaysia" International Journal of Environmental Research and Public Health 17, no. 14: 5144. https://doi.org/10.3390/ijerph17145144
APA StyleNg, E. S. Y., Wong, P. Y., Kamaruddin, A. T. H., Lim, C. T. S., & Chan, Y. M. (2020). Poor Sleep Quality, Depression and Social Support Are Determinants of Serum Phosphate Level among Hemodialysis Patients in Malaysia. International Journal of Environmental Research and Public Health, 17(14), 5144. https://doi.org/10.3390/ijerph17145144




