Asthma Mortality and Hospitalizations in Mexico from 2010 to 2018: Retrospective Epidemiologic Profile
Abstract
1. Introduction
2. Materials y Methods
2.1. Study Design and Data Sources
2.2. Sociodemographic Variables
2.3. Clinical Variables
3. Statistical Analysis
4. Results
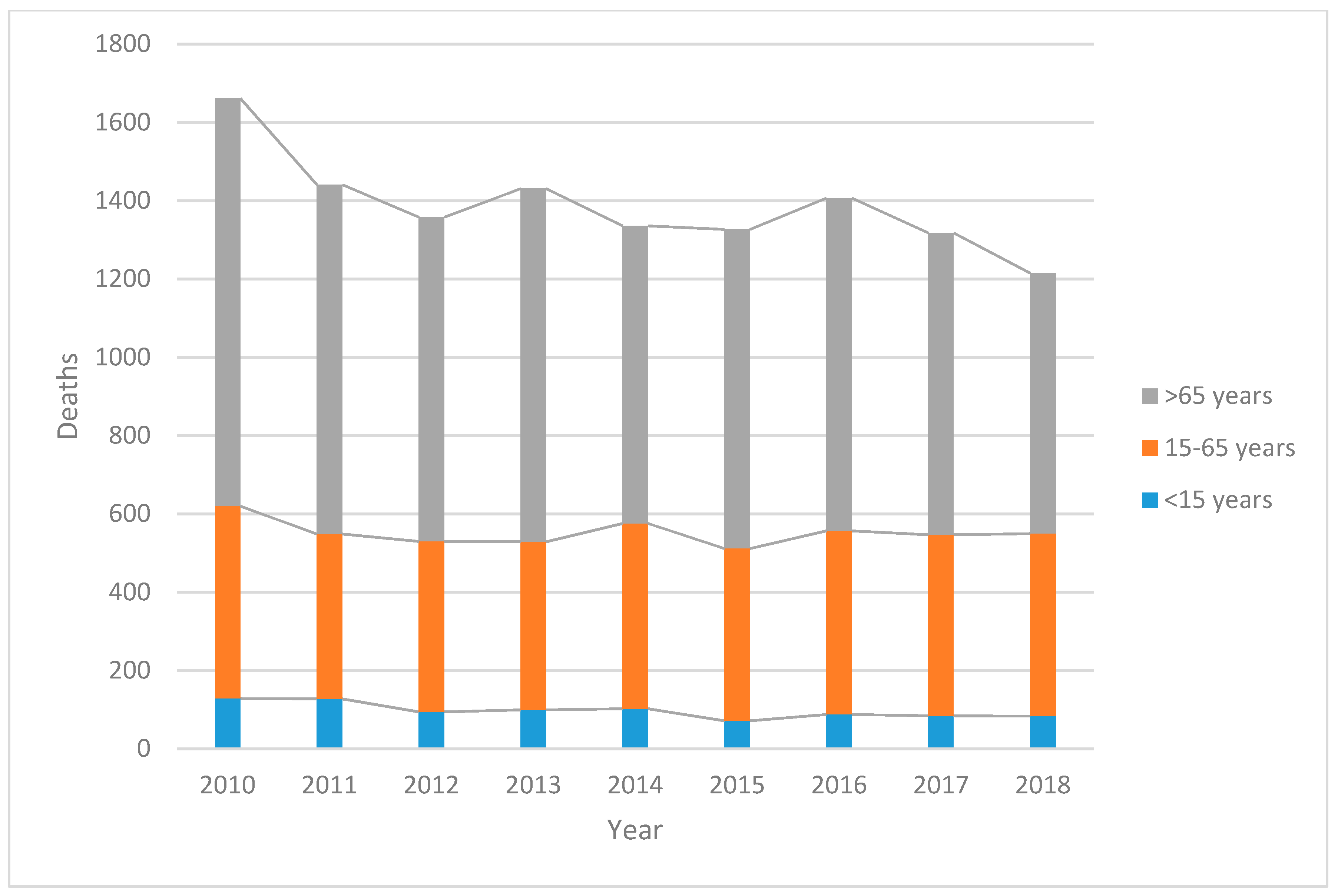
4.1. General Mortality
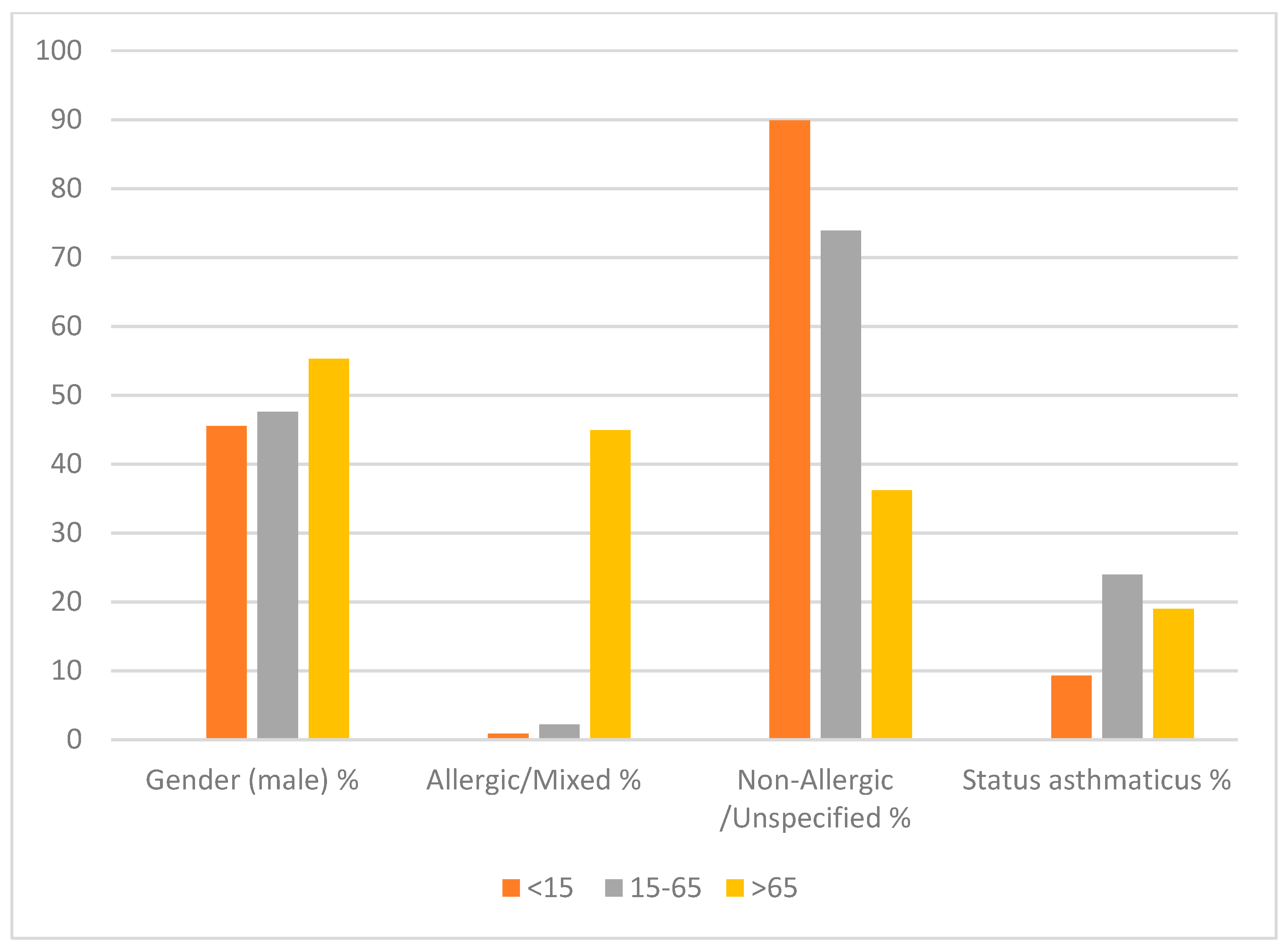
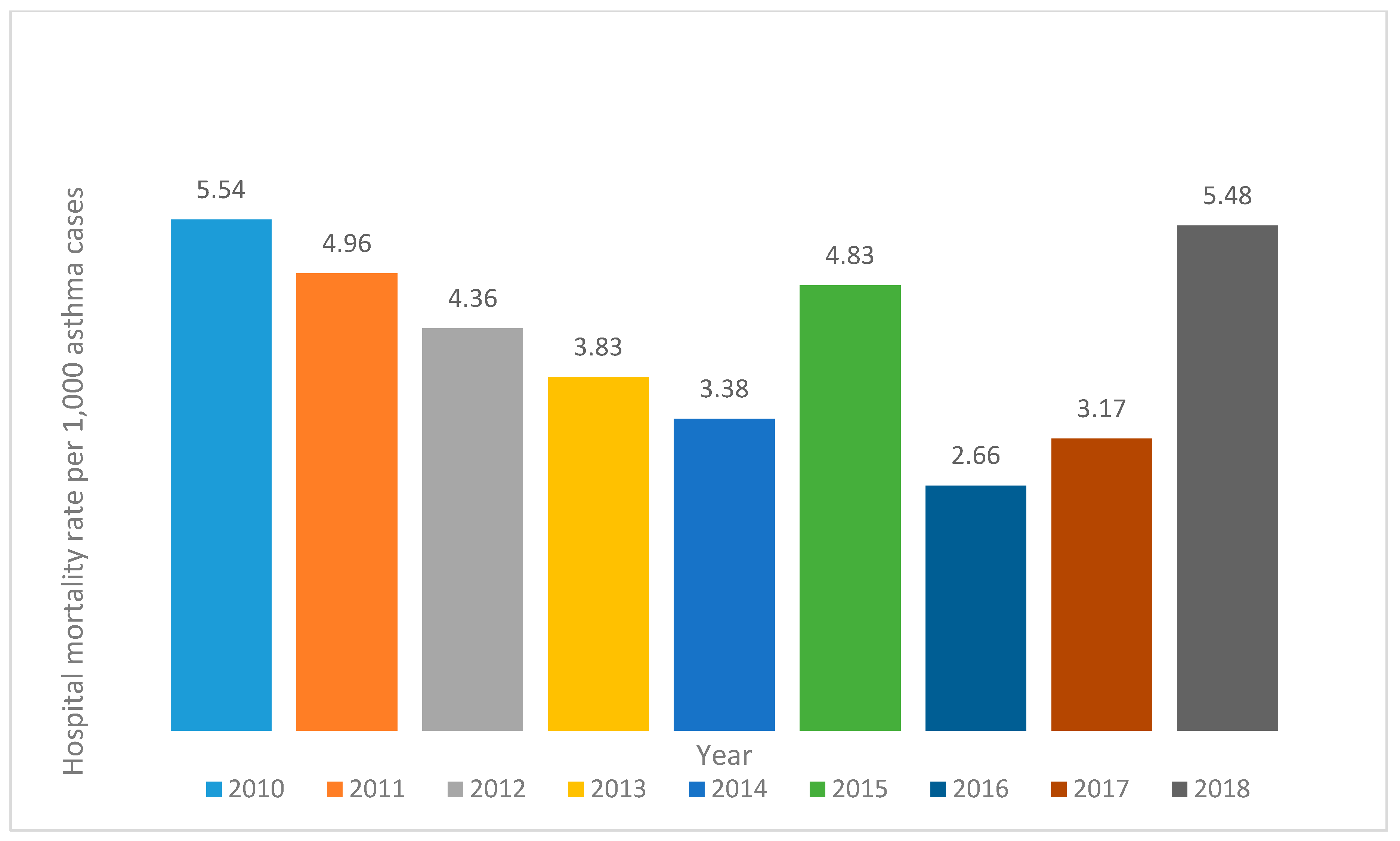
4.2. Hospitalizations with Asthma as Primary Diagnosis
5. Discussion
5.1. Limitations
5.2. Public Health and Policy Implications
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- National Asthma Education and Prevention Program.: Expert panel Report III: Guidelines for the Diagnosis and Management of Asthma; NIH publication no. 08-4051; National Heart, Lung, and Blood Institute: Bethesda, MD, USA, 2007. Available online: www.nhlbi.nih.gov/guidelines/asthma/asthgdln.htm (accessed on 22 March 2020).
- Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention. 2020. Available online: www.ginasthma.org (accessed on 22 March 2020).
- Holgate, S.T.; Wenzel, S.; Postma, D.S.; Weiss, S.T.; Renz, H.; Sly, P.D. Asthma. Nat. Rev. Dis. Primers 2015, 1, 15025. [Google Scholar] [CrossRef]
- Loftus, P.A.; Wise, S.K. Epidemiology of asthma. Curr. Opin. Otolaryngol. Head Neck Surg. 2016, 24, 245–249. [Google Scholar] [CrossRef]
- Vargas, B.M.H. Epidemiología del asma. Neumol. Cir. Torax. 2009, 68, 91–97. [Google Scholar]
- Ellwood, P.; Asher, M.I.; Beasley, R.; Clayton, T.O.; Stewart, A.W.; ISAAC Steering Committee. The international study of asthma and allergies in childhood (ISAAC): Phase three rationale and methods. Int. J. Tuberc. Lung Dis. 2005, 9, 10–16. [Google Scholar] [PubMed]
- Croisant, S. Epidemiology of asthma: Prevalence and burden of disease. Adv. Exp. Med. Biol. 2014, 795, 17–29. [Google Scholar] [CrossRef] [PubMed]
- García-Sancho, C.; Fernández-Plata, R.; Martínez-Briseño, D.; Franco-Marina, F.; Pérez-Padilla, J.R. Prevalencia y riesgos asociados con pacientes adultos con asma de 40 años o más de la Ciudad de México: Estudio de base poblacional. Salud Publica Mex. 2012, 54, 425–432. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Morales-Romero, J.; Bedolla-Barajas, M.; López-Cota, G.A.; Bedolla-Pulido, T.I.; Bedolla-Pulido, T.R.; Navarro-Lozano, E.; Robles-Figueroa, M.; Lerma-Partida, S.; Fregoso-Fregoso, M. Trends in asthma prevalence and its symptoms in Mexican late adolescents over a 7-year period. Rev. Alerg Mex. 2018, 65, 331–340. [Google Scholar] [CrossRef] [PubMed]
- Del-Rio-Navarro, B.; Del Rio-Chivardi, J.M.; Berber, A.; Sienra-Monge, J.J.; Rosas-Vargas, M.A.; Baeza-Bacab, M. Asthma prevalence in children living in north Mexico City and a comparison with other Latin American cities and world regions. Allergy Asthma Proc. 2006, 27, 334–340. [Google Scholar] [CrossRef]
- Herrera, A.M.; Fitzgerald, D.A. Question 1: Why do children still die from asthma? Paediatr Respir. Rev. 2018, 27, 40–43. [Google Scholar] [CrossRef]
- Gullach, A.J.; Risgaard, B.; Lynge, T.H.; Jabbari, R.; Glinge, C.; Haunsø, S.; Backer, V.; Winkel, B.G.; Tfelt-Hansen, J. Sudden death in young persons with uncontrolled asthma--a nationwide cohort study in Denmark. BMC Pulm Med. 2015, 15, 35. [Google Scholar] [CrossRef] [PubMed]
- Levy, M.L.; Winter, R. Asthma deaths: What now? Thorax 2015, 70, 209–210. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Pelkonen, M.K.; Notkola, I.K.; Laatikainen, T.K.; Jousilahti, P. 30-year trends in asthma and the trends in relation to hospitalization and mortality. Respir Med. 2018, 142, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Levy, M.L. The national review of asthma deaths: What did we learn and what needs to change? Breathe 2015, 11, 14–24. [Google Scholar] [CrossRef] [PubMed]
- Salas Ramírez, M.; Segura Méndez, N.H.; Martínez-Cairo Cueto, S. Asthma mortality trends in Mexico. Bol. Oficina Sanit Panam. 1994, 116, 298–306. [Google Scholar]
- Secretaría de Salud. Anuarios de Morbilidad 1984–2018. Available online: https://www.gob.mx/salud/acciones-y-programas/anuarios-de-morbilidad-1984-2019 (accessed on 30 March 2020).
- Busse, W.W.; Lemanske, R.F., Jr.; Gern, J.E. Role of viral respiratory infections in asthma and asthma exacerbations. Version 2. The Lancet 2010, 376, 826–834. [Google Scholar] [CrossRef]
- Soto-Estradaa, G.; Moreno-Altamiranoa, L.; Pahua, D.D. Panorama epidemiológico de México, principales causas de morbilidad y mortalidad. Rev. Fac. Med. UNAM 2016, 59, 8–22. [Google Scholar]
- León-Cortés, J.L.; Leal Fernández, G.; Sánchez-Pérez, H.J. Health reform in Mexico: Governance and potential outcomes. Int. J. Equity Health 2019, 18, 30. [Google Scholar] [CrossRef]
- Instituto Nacional de Estadística y Geografía. Derechohabiencia. Available online: https://www.inegi.org.mx/temas/derechohabiencia/ (accessed on 15 March 2020).
- Urquieta-Salomón, J.E.; Villarreal, H.J. Evolution of health coverage in Mexico: Evidence of progress and challenges in the Mexican health system. Health Policy Plan. 2016, 31, 28–36. [Google Scholar] [CrossRef]
- Dirección General de Información en Salud. Normas. Available online: http://www.dgis.salud.gob.mx/contenidos/normatividad/normas_gobmx.html (accessed on 12 May 2020).
- Dirección General de Información en Salud. Egresos Hospitalarios. Available online: http://www.dgis.salud.gob.mx/contenidos/basesdedatos/da_egresoshosp_gobmx.html (accessed on 12 May 2020).
- National Center for Technological Excellence in Health (CENETEC). Master Catalogo f Clinical Practice Guidelines. Available online: http://www.cenetec.gob.mx/spry/gpc/catalogoMaestroGPC_no_js.html (accessed on 13 May 2020).
- Silva, G.E.; Sherrill, D.L.; Guerra, S.; Barbee, R.A. Asthma as a risk factor for COPD in a longitudinal study. Chest 2004, 126, 59–65. [Google Scholar] [CrossRef]
- Mahdavinia, M.; Foster, K.J.; Jauregui, E.; Moore, D.; Adnan, D.; Andy-Nweye, A.B.; Khan, S.; Bishehsari, F. Asthma prolongs intubation in COVID-19. J. Allergy Clin. Immunol. Pract. 2020. [Google Scholar] [CrossRef]
- Akinbami, L.J.; Moorman, J.E.; Bailey, C.; Zahran, H.S.; King, M.; Johnson, C.A.; Liu, X. Trends in asthma prevalence, health care use, and mortality in the United States, 2001–2010. In NCHS Data Brief; Akinbami, O.J., Ed.; U.S. Department of Health and Human Services: Hyattsville, MD, USA, 2012; pp. 1–8. [Google Scholar]
- Ziyab, A.H.; Abul, A.T. Trends in asthma hospital admissions and mortality in Kuwait, 2000-2014: A national retrospective observational study. BMJ Open 2018, 8, e021244. [Google Scholar] [CrossRef]
- Fuhrman, C.; Jougla, E.; Uhry, Z.; Delmas, M.C. Deaths with asthma in France, 2000-2005: A multiple-cause analysis. J. Asthma 2009, 46, 402–406. [Google Scholar] [CrossRef] [PubMed]
- Soto-Martínez, M.; Avila, L.; Soto, N.; Chaves, A.; Celedón, J.C.; Soto-Quiros, M.E. Trends in hospitalizations and mortality from asthma in Costa Rica over a 12- to 15-year period. J. Allergy Clin. Immunol. Pract. 2014, 2, 85–90. [Google Scholar] [CrossRef] [PubMed]
- Pitchon, R.R.; Alvim, C.G.; Andrade, C.R.; Lasmar, L.M.L.B.F.; Cruz, Á.A.; Reis, A.P.D. Asthma mortality in children and adolescents of Brazil over a 20-year period. J. Pediatr. (Rio J.) 2019. [Google Scholar] [CrossRef] [PubMed]
- Vargas, M.H.; Díaz-Mejía, G.S.; Furuya, M.E.; Salas, J.; Lugo, A. Trends of asthma in Mexico: An 11-year analysis in a nationwide institution. Chest 2004, 125, 1993–1997. [Google Scholar] [CrossRef]
- Gonzalez-Barcala, F.J.; Aboal, J.; Carreira, J.M.; Rodriguez-Alvarez, M.X.; Puga, A.; Sanjose, E.; Pintos, M.; Valdes, L. Trends of asthma mortality in Galicia from 1993 to 2007. J. Asthma 2012, 49, 1016–1020. [Google Scholar] [CrossRef]
- Santos, N.; Bugalho de Almeida, A.; Covas, A.; Prates, L.; Morais-Almeida, M. Trends of asthma hospitalization and hospital mortality in mainland Portugal. Eur. Ann. Allergy Clin. Immunol. 2016, 48, 237–241. [Google Scholar]
- Watson, L.; Turk, F.; James, P.; Holgate, S.T. Factors associated with mortality after an asthma admission: A national United Kingdom database analysis. Respir. Med. 2007, 101, 1659–1664. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.L.; Ko, H.K.; Lu, M.S.; Chou, C.L.; Su, K.C.; Hsu, C.C.; Chou, K.-T.; Chen, T.-J.; Perng, D.-W.; Chou, Y.-C. Independent risk factors for death in patients admitted for asthma exacerbation in Taiwan. NPJ Prim. Care Respir. Med. 2020, 30, 7. [Google Scholar] [CrossRef]
- Chua, K.L.; Soh, S.E.; Ma, S.; Lee, B.W.; Pacific Association of Pediatric Allergy, Respirology & Immunology (APAPARI). Pediatric asthma mortality and hospitalization trends across Asia pacific: Relationship with asthma drug utilization patterns. World Allergy Organ. J. 2009, 2, 77–82. [Google Scholar] [CrossRef]
- Gupta, R.P.; Mukherjee, M.; Sheikh, A.; Strachan, D.P. Persistent variations in national asthma mortality, hospital admissions and prevalence by socioeconomic status and region in England. Thorax 2018, 73, 706–712. [Google Scholar] [CrossRef] [PubMed]
- Carrillo, G.; Spence-Almaguer, E.; Lucio, R.L.; Chong-Menard, B.; Smith, K. Improving asthma in Hispanic families through a home-based educational intervention. Pediatr. Allergy Immunol. Pulmonol. 2015, 28, 165–171. [Google Scholar] [CrossRef]
- Sockrider, M.M.; Abramson, S.; Brooks, E.; Caviness, A.C.; Pilney, S.; Koerner, C.; Macias, C.G. Delivering tailored asthma family education in a pediatric emergency department setting: A pilot study. Pediatrics 2006, 117 Pt 2, S135–S144. [Google Scholar] [CrossRef]
- Vernon, M.K.; Bell, J.A.; Wiklund, I.; Dale, P.; Chapman, K.R. Asthma control and asthma triggers: The patient perspective. J. Asthma Allergy Educ. 2013, 4, 155–164. [Google Scholar] [CrossRef]
| Year | Relative Risk Ratio | Standard | z | p | Confidence Intervals 95% | |
|---|---|---|---|---|---|---|
| Error | Lower | Upper | ||||
| 2010 | Base outcome RRR = 1.00 | |||||
| 2011 | 0.99 | 0.08 | −0.18 | 0.856 | 0.84 | 1.16 |
| 2012 | 1.19 | 0.10 | 1.99 | 0.046 | 1.000 | 1.41 |
| 2013 | 1.23 | 0.11 | 2.4 | 0.017 | 1.04 | 1.45 |
| 2014 | 1.12 | 0.10 | 1.31 | 0.189 | 0.95 | 1.33 |
| 2015 | 1.01 | 0.09 | 0.16 | 0.874 | 0.86 | 1.2 |
| 2016 | 1.21 | 0.10 | 2.24 | 0.025 | 1.02 | 1.44 |
| 2017 | 1.28 | 0.11 | 2.79 | 0.005 | 1.08 | 1.52 |
| 2018 | 1.36 | 0.13 | 3.39 | 0.001 | 1.14 | 1.63 |
| Characteristic | Odds Ratio | Standard | z | p | Confidence Intervals 95% | |
|---|---|---|---|---|---|---|
| Error | Lower | Upper | ||||
| Gender (male) | 0.70 | 0.04 | −7.06 | 0.000 | 0.63 | 0.77 |
| Age <15 | 1.46 | 0.11 | 4.82 | 0.000 | 1.25 | 1.70 |
| Age 15–65 | 2.91 | 0.13 | 24.16 | 0.000 | 2.67 | 3.18 |
| Age >65 | 0.39 | 0.02 | −17.84 | 0.000 | 0.35 | 0.43 |
| Employment | 0.94 | 0.05 | −1.15 | 0.250 | 0.85 | 1.04 |
| ≥Elementary school | 1.18 | 0.08 | 2.66 | 0.008 | 1.05 | 1.34 |
| Married | 1.59 | 0.08 | 9.00 | 0.000 | 1.44 | 1.76 |
| Medical Insurance | 2.57 | 0.14 | 16.68 | 0.000 | 2.30 | 2.87 |
| Urban residence | 3.43 | 0.18 | 23.77 | 0.000 | 3.09 | 3.79 |
| Type of Asthma | Age (Years) | Length of Stay (Days) | Male | Medical Insurance | From Emergency Room | From Ambulatory Consultation | Accurate Initial Diagnosis | First Time Hospitalized | In-Hospital Infection | Mortality Per 1000 Patients | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | SD | n | SD | n | SD | n | SD | n | SD | n | SD | n | SD | n | SD | n | SD | n | SD | |
| Allergic | 5.40 | 0.12 | 2.69 | 0.04 | 57.23 | 0.57 | 72.75 | 0.52 | 96.37 | 0.22 | 1.75 | 0.15 | 94.52 | 0.26 | 93.89 | 0.28 | 0.19 | 0.05 | 1.85 | 0.30 |
| Non-Allergic | 16.84 | 0.10 | 3.08 | 0.02 | 47.56 | 0.24 | 68.07 | 0.22 | 93.56 | 0.12 | 4.30 | 0.10 | 95.27 | 0.10 | 90.41 | 0.14 | 0.33 | 0.03 | 4.52 | 0.27 |
| Mixed | 18.09 | 1.11 | 2.86 | 0.12 | 47.37 | 2.45 | 72.49 | 2.19 | 90.67 | 1.42 | 5.26 | 1.09 | 96.17 | 0.94 | 88.76 | 1.55 | 0.72 | 0.41 | 9.30 | 0.63 |
| Status asthmaticus | 15.01 | 0.10 | 3.13 | 0.02 | 48.80 | 0.26 | 66.99 | 0.25 | 94.27 | 0.12 | 4.20 | 0.11 | 96.64 | 0.09 | 82.54 | 0.20 | 0.39 | 0.03 | 4.29 | 0.27 |
| Death | Odds Ratio | Std. Err. | z | p | (95% Confidence Intervals) | |
|---|---|---|---|---|---|---|
| Hospital Stay per age | 1.02 | 0.00 | 5.33 | 0.000 | 1.01 | 1.03 |
| <15 years | 0.05 | 0.03 | −5.30 | 0.000 | 0.02 | 0.15 |
| 15–65 years | 0.65 | 0.35 | −0.81 | 0.418 | 0.23 | 1.85 |
| >65 years | 2.05 | 1.09 | 1.36 | 0.175 | 0.73 | 5.81 |
| Gender (male) | 1.47 | 0.20 | 2.88 | 0.004 | 1.13 | 1.91 |
| From Emergency room | 1.92 | 1.13 | 1.11 | 0.269 | 0.60 | 6.07 |
| From External consultation | 0.94 | 0.65 | −0.09 | 0.930 | 0.24 | 3.65 |
| Allergic | 0.22 | 0.10 | −3.38 | 0.001 | 0.09 | 0.53 |
| Mixed type asthma | 3.33 | 1.68 | 2.37 | 0.018 | 1.23 | 8.97 |
| Non-Allergic/Unspecific | 1.36 | 0.17 | 2.42 | 0.015 | 1.06 | 1.74 |
| Status asthmaticus | 0.91 | 0.12 | −0.73 | 0.466 | 0.71 | 1.17 |
| Accurate initial diagnosis | 0.11 | 0.02 | −15.34 | 0.000 | 0.09 | 0.15 |
| First time Hospitalized | 1.94 | 0.43 | 3.02 | 0.003 | 1.26 | 2.98 |
| In-Hospital Infection | 9.26 | 3.46 | 5.96 | 0.000 | 4.45 | 19.25 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carrillo, G.; Mendez-Domínguez, N.; Datta-Banik, R.; Figueroa-Lopez, F.; Estrella-Chan, B.; Alvarez-Baeza, A.; Garza, N. Asthma Mortality and Hospitalizations in Mexico from 2010 to 2018: Retrospective Epidemiologic Profile. Int. J. Environ. Res. Public Health 2020, 17, 5071. https://doi.org/10.3390/ijerph17145071
Carrillo G, Mendez-Domínguez N, Datta-Banik R, Figueroa-Lopez F, Estrella-Chan B, Alvarez-Baeza A, Garza N. Asthma Mortality and Hospitalizations in Mexico from 2010 to 2018: Retrospective Epidemiologic Profile. International Journal of Environmental Research and Public Health. 2020; 17(14):5071. https://doi.org/10.3390/ijerph17145071
Chicago/Turabian StyleCarrillo, Genny, Nina Mendez-Domínguez, Rudradeep Datta-Banik, Fernando Figueroa-Lopez, Brandon Estrella-Chan, Alberto Alvarez-Baeza, and Norma Garza. 2020. "Asthma Mortality and Hospitalizations in Mexico from 2010 to 2018: Retrospective Epidemiologic Profile" International Journal of Environmental Research and Public Health 17, no. 14: 5071. https://doi.org/10.3390/ijerph17145071
APA StyleCarrillo, G., Mendez-Domínguez, N., Datta-Banik, R., Figueroa-Lopez, F., Estrella-Chan, B., Alvarez-Baeza, A., & Garza, N. (2020). Asthma Mortality and Hospitalizations in Mexico from 2010 to 2018: Retrospective Epidemiologic Profile. International Journal of Environmental Research and Public Health, 17(14), 5071. https://doi.org/10.3390/ijerph17145071







