Organophosphate Pesticide Exposure and Breast Cancer Risk: A Rapid Review of Human, Animal, and Cell-Based Studies
Abstract
1. Introduction
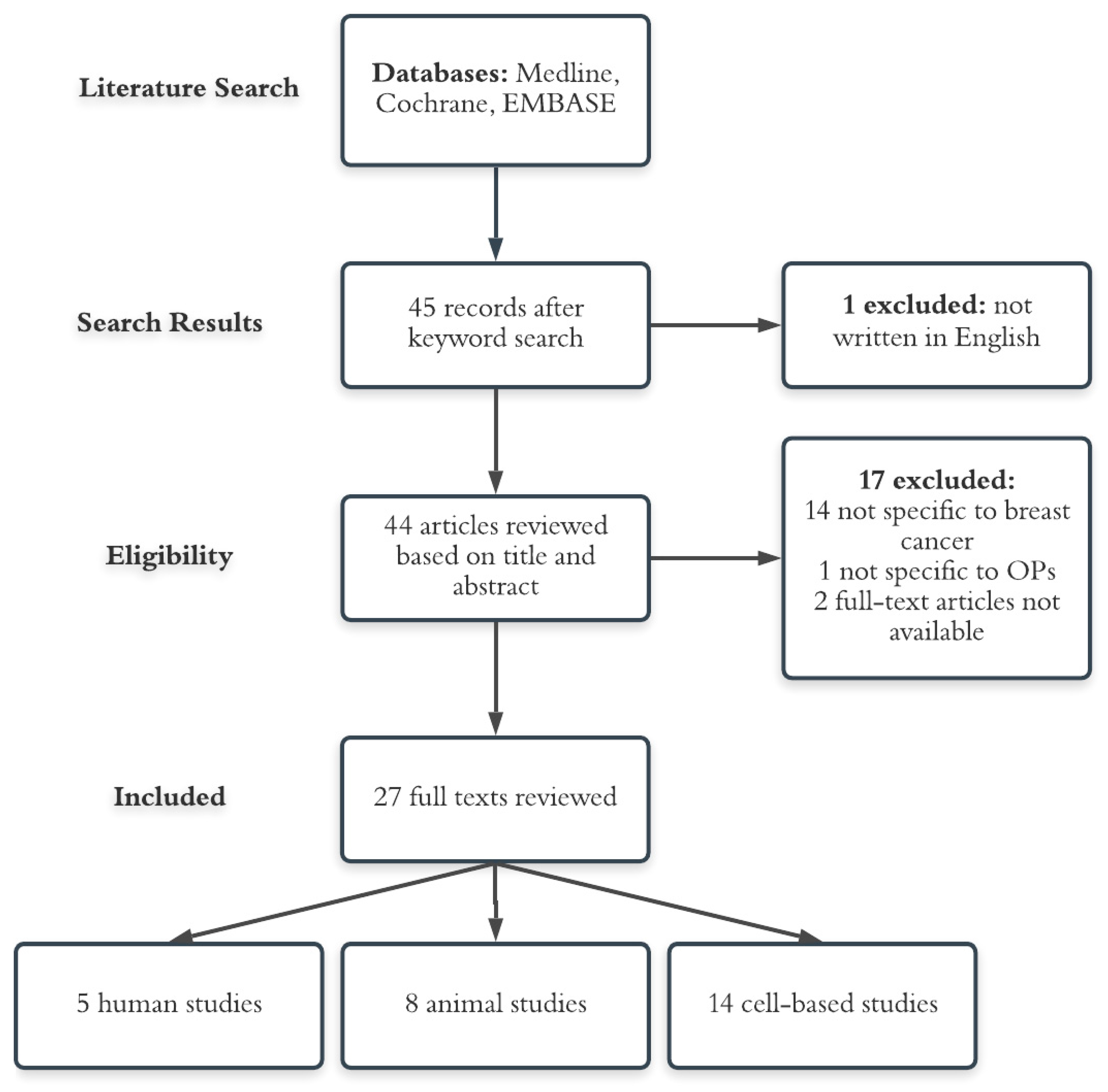
2. Methods
2.1. Study Design
2.2. Search Strategy and Inclusion/Exclusion Criteria
2.3. Data Extraction
2.4. Outcome Measures
3. Results
3.1. Human Studies
3.2. Animal Studies
3.3. Cell-Based Studies
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- DeSantis, C.E.; Ma, J.; Gaudet, M.M.; Newman, L.A.; Miller, K.D.; Goding Sauer, A.; Jemal, A.; Siegel, R.L. Breast cancer statistics, 2019. CA Cancer J. Clin. 2019, 69, 438–451. [Google Scholar] [CrossRef]
- Palmero, E.I.; Caleffi, M.; Schüler-Faccini, L.; Roth, F.L.; Kalakun, L.; Netto, C.B.O.; Skonieski, G.; Giacomazzi, J.; Weber, B.; Giugliani, R.; et al. Population prevalence of hereditary breast cancer phenotypes and implementation of a genetic cancer risk assessment program in southern Brazil. Genet. Mol. Biol. 2009, 32, 447–455. [Google Scholar] [CrossRef][Green Version]
- National Collaborating Centre for Cancer (UK). Familial Breast Cancer: Classification and Care of People at Risk of Familial Breast Cancer and Management of Breast Cancer and Related Risks in People with a Family History of Breast Cancer; NICE Clinical Guidelines; National Collaborating Centre for Cancer (UK): Cardiff, UK, 2013. [Google Scholar]
- Van Den Brandt, P.A.; Spiegelman, D.; Yaun, S.S.; Adami, H.O.; Beeson, L.; Folsom, A.R.; Fraser, G.; Goldbohm, R.A.; Graham, S.; Kushi, L.; et al. Pooled analysis of prospective cohort studies on height, weight, and breast cancer risk. Am. J. Epidemiol. 2000, 152, 514–527. [Google Scholar] [CrossRef]
- Monninkhof, E.M.; Elias, S.G.; Vlems, F.A.; Van Der Tweel, I.; Schuit, A.J.; Voskuil, D.W.; Van Leeuwen, F.E. Physical activity and breast cancer: A systematic review. Epidemiology 2007, 18, 137–157. [Google Scholar] [CrossRef] [PubMed]
- Key, J.; Hodgson, S.; Omar, R.Z.; Jensen, T.K.; Thompson, S.G.; Boobis, A.R.; Davies, D.S.; Elliott, P. Meta-analysis of studies of alcohol and breast cancer with consideration of the methodological issues. Cancer Causes Control 2006, 17, 759–770. [Google Scholar] [CrossRef]
- Baudry, J.; Assmann, K.E.; Touvier, M.; Allès, B.; Seconda, L.; Latino-Martel, P.; Ezzedine, K.; Galan, P.; Hercberg, S.; Lairon, D.; et al. Association of Frequency of Organic Food Consumption with Cancer Risk: Findings from the NutriNet-Santé Prospective Cohort Study. JAMA Intern. Med. 2018, 178, 1597–1606. [Google Scholar] [CrossRef] [PubMed]
- Global Organophosphate Pesticides Market | Growth, Trends, and Forecast (2018–2023). Available online: https://www.mordorintelligence.com/industry-reports/organophosphate-pesticides-market (accessed on 14 April 2020).
- Roberts, J.R.; Reigart, J.R. Recognition and Management of Pesticide Poisonings, 6th ed.; National Association of State Departments of Agriculture Research Foundation (NASDARF): Arlington, VA, USA, 2013; Chapter 5 Organophosphates. [Google Scholar]
- Lu, C.; Barr, D.B.; Pearson, M.A.; Waller, L.A. Dietary inake and its contribution to longitudinal organophosphorus pesticide exposure in urban/suburban children. Environ. Health Perspect. 2008, 116, 537–542. [Google Scholar] [CrossRef]
- US Environmental Protection Agency (EPA). Organophosphorus Cumulative Risk Assessment—2006 Update; This PDF contains the OP Cumulative Risk Assessment document without the appendices; National Service Center for Environmental Publications (NSCEP): Cincinatti, OH, USA, 2006.
- Barr, D.B.; Wong, L.Y.; Bravo, R.; Weerasekera, G.; Odetokun, M.; Restrepo, P.; Kim, D.G.; Fernandez, C.; Whitehead, R.D.; Perez, J.; et al. Urinary concentrations of dialkylphosphate metabolites of organophosphorus pesticides: National Health and Nutrition Examination Survey 1999–2004. Int. J. Environ. Res. Public Health 2011, 8, 3063–3098. [Google Scholar] [CrossRef] [PubMed]
- Colovic, M.B.; Krstic, D.Z.; Lazarevic-Pasti, T.D.; Bondzic, A.M.; Vasic, V.M. Acetylcholinesterase Inhibitors: Pharmacology and Toxicology. Curr. Neuropharmacol. 2013, 11, 315–335. [Google Scholar] [CrossRef]
- US Environmental Protection Agency Office of Pesticide Programs. Diazinon IRED Facts Pesticides; US Office of Prevention, Pesticides and Toxic Substances: Washington, DC, USA, 2006.
- US Environmental Protection Agency. Chlorpyrifos | Ingredients Used in Pesticide Products | US EPA. 2019. Available online: https://www.epa.gov/ingredients-used-pesticide-products/chlorpyrifos (accessed on 12 December 2019).
- Koutros, S.; Beane Freeman, L.E.; Lubin, J.H.; Heltshe, S.L.; Andreotti, G.; Barry, K.H.; Dellavalle, C.T.; Hoppin, J.A.; Sandler, D.P.; Lynch, C.F.; et al. Risk of total and aggressive prostate cancer and pesticide use in the Agricultural Health Study. Am. J. Epidemiol. 2013, 177, 59–74. [Google Scholar] [CrossRef] [PubMed]
- Hu, L.; Luo, D.; Zhou, T.; Tao, Y.; Feng, J.; Mei, S. The association between non-Hodgkin lymphoma and organophosphate pesticides exposure: A meta-analysis. Environ. Pollut. 2017, 231, 319–328. [Google Scholar] [CrossRef] [PubMed]
- Guyton, K.Z.; Loomis, D.; Grosse, Y.; El Ghissassi, F.; Benbrahim-Tallaa, L.; Guha, N.; Scoccianti, C.; Mattock, H.; Straif, K.; Blair, A.; et al. Carcinogenicity of tetrachlorvinphos, parathion, malathion, diazinon, and glyphosate. Lancet Oncol. 2015, 16, 490–491. [Google Scholar] [CrossRef]
- Manabe, M.; Kanda, S.; Fukunaga, K.; Tsubura, A.; Nishiyama, T. Evaluation of the estrogenic activities of some pesticides and their combinations using MtT/Se cell proliferation assay. Int. J. Hyg. Environ. Health 2006, 209, 413–421. [Google Scholar] [CrossRef] [PubMed]
- Ishihara, A.; Nishiyama, N.; Sugiyama, S.I.; Yamauchi, K. The effect of endocrine disrupting chemicals on thyroid hormone binding to Japanese quail transthyretin and thyroid hormone receptor. Gen. Comp. Endocrinol. 2003, 134, 36–43. [Google Scholar] [CrossRef]
- Gore, A.C. Environmental toxicant effects on neuroendocrine function. Endocrine 2001, 14, 235–246. [Google Scholar] [CrossRef]
- Stroup, D.F.; Berlin, J.A.; Morton, S.C.; Olkin, I.; Williamson, G.D.; Rennie, D.; Moher, D.; Becker, B.J.; Sipe, T.A.; Thacker, S.B. Meta-analysis of observational studies in epidemiology: A proposal for reporting. J. Am. Med. Assoc. 2000, 283, 2008–2012. [Google Scholar] [CrossRef]
- Atwood, D.; Pasiley-Jones, C. Pesticides Industry Sales and Usage 2008—2012; U.S. Environmental Protection Agency: Washington, DC, USA, 2017.
- Mills, P.K.; Yang, R. Breast Cancer Risk in Hispanic Agricultural Workers in California Hispanic Agricultural Workers in California. Int. J. Occup. Environ. Health 2005, 11, 1077–3525. [Google Scholar] [CrossRef]
- Engel, L.S.; Hill, D.A.; Hoppin, J.A.; Lubin, J.H.; Lynch, C.F.; Pierce, J.; Samanic, C.; Sandler, D.P.; Blair, A.; Alavanja, M.C. Pesticide use and breast cancer risk among farmers’ wives in the agricultural health study. Am. J. Epidemiol. 2005, 161, 121–135. [Google Scholar] [CrossRef]
- Lerro, C.C.; Koutros, S.; Andreotti, G.; Friesen, M.C.; Alavanja, M.C.; Blair, A.; Hoppin, J.A.; Sandler, D.P.; Lubin, J.H.; Ma, X.; et al. Organophosphate insecticide use and cancer incidence among spouses of pesticide applicators in the Agricultural Health Study. Occup. Environ. Med. 2015, 72, 736–744. [Google Scholar] [CrossRef]
- Engel, L.S.; Werder, E.; Satagopan, J.; Blair, A.; Hoppin, J.A.; Koutros, S.; Lerro, C.C.; Sandler, D.P.; Alavanja, M.C.; Beane Freeman, L.E. Insecticide Use and Breast Cancer Risk among Farmers’ Wives in the Agricultural Health Study. Environ. Health Perspect. 2017, 125, 097002. [Google Scholar] [CrossRef]
- Tayour, C.; Ritz, B.; Langholz, B.; Mills, P.K.; Wu, A.; Wilson, J.P.; Shahabi, K.; Cockburn, M. A case–control study of breast cancer risk and ambient exposure to pesticides. Environ. Epidemiol. 2019, 3, e070. [Google Scholar] [CrossRef]
- Calaf, G.M.; Garrido, F. Catechol estrogens as biomarkers for mammary gland cancer. Int. J. Oncol. 2011, 39, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Silinskas, K.C.; Okey, A.B. Protection by 1,1,1-trichloro-2,2-bis(p-chlorophenyl)ethane (DDT) against mammary tumors and leukemia during prolonged feeding of 7,12-dimethylbenz[a]anthracene to female rats. J. Natl. Cancer Inst. 1975, 55, 653–657. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Calaf, G.M.; Echiburú-Chau, C. Synergistic effect of malathion and estrogen on mammary gland carcinogenesis. Oncol. Rep. 2012, 28, 640–646. [Google Scholar] [CrossRef] [PubMed]
- Cabello, G.; Valenzuela, M.; Vilaxa, A.; Durán, V.; Rudolph, I.; Hrepic, N.; Calaf, G. A Rat Mammary Tumor Model Induced by the Organophosphorous Pesticides Parathion and Malathion, Possibly through Acetylcholinesterase Inhibition. Environ. Health Perspect. 2001, 109, 471–479. [Google Scholar] [CrossRef] [PubMed]
- Ventura, C.; Nieto, M.R.R.; Bourguignon, N.; Lux-Lantos, V.; Rodriguez, H.; Cao, G.; Randi, A.; Cocca, C.; Núñez, M. Pesticide chlorpyrifos acts as an endocrine disruptor in adult rats causing changes in mammary gland and hormonal balance. J. Steroid Biochem. Mol. Biol. 2016, 156, 1–9. [Google Scholar] [CrossRef]
- Ventura, C.; Zappia, C.D.; Lasagna, M.; Pavicic, W.; Richard, S.; Bolzan, A.D.; Monczor, F.; Núñez, M.; Cocca, C. Effects of the pesticide chlorpyrifos on breast cancer disease. Implication of epigenetic mechanisms. J. Steroid Biochem. Mol. Biol. 2019, 186, 96–104. [Google Scholar] [CrossRef]
- Omran, O.M.; Omer, O.H. The effects of alpha-lipoic acid on breast of female albino rats exposed to malathion: Histopathological and immunohistochemical study. Pathol. Res. Pract. 2015, 211, 462–469. [Google Scholar] [CrossRef]
- Kang, H.G.; Jeong, S.H.; Cho, J.H.; Kim, D.G.; Park, J.M.; Cho, M.H. Chlropyrifos-methyl shows anti-androgenic activity without estrogenic activity in rats. Toxicology 2004, 199, 219–230. [Google Scholar] [CrossRef]
- Huggins, C.; Grand, L.C.; Brillantes, F.P. Critical Significance of Breast Structure in the Induction of Mammary Cancer in the Rat. Proc. Natl. Acad. Sci. USA 1959, 45, 1294–1300. [Google Scholar] [CrossRef]
- Russo, J.; Russo, I.H. DNA labeling index and structure of the rat mammary gland as determinants of its susceptibility to carcinogenesis. J. Natl. Cancer Inst. 1978, 61, 1451–1459. [Google Scholar] [PubMed]
- Calaf, G.M.; Roy, D. Cancer genes induced by malathion and parathion in the presence of estrogen in breast cells. Int. J. Mol. Med. 2008, 21, 261–268. [Google Scholar] [CrossRef] [PubMed]
- Calaf, G.M.; Echiburu-Chau, C.; Roy, D. Organophosphorous pesticides and estrogen induce transformation of breast cells affecting p53 and c-Ha-ras genes. Int. J. Oncol. 2009, 35, 1061–1068. [Google Scholar] [CrossRef] [PubMed]
- Gwinn, M.R.; Whipkey, D.L.; Tennant, L.B.; Weston, A. Differential gene expression in normal human mammary epithelial cells treated with malathion monitored by DNA microarrays. Environ. Health Perspect. 2005, 113, 1046–1051. [Google Scholar] [CrossRef][Green Version]
- Kjeldsen, L.S.; Ghisari, M.; Bonefeld-Jørgensen, E.C. Currently used pesticides and their mixtures affect the function of sex hormone receptors and aromatase enzyme activity. Toxicol. Appl. Pharmacol. 2013, 272, 453–464. [Google Scholar] [CrossRef]
- Chen, H.; Xiao, J.; Hu, G.; Zhou, J.; Xiao, H.; Wang, X. Estrogenicity of organophosphorus and pyrethroid pesticides. J. Toxicol. Environ. Health Part A 2002, 65, 1419–1435. [Google Scholar] [CrossRef]
- Farhadi, K.; Tahmasebi, R.; Biparva, P.; Maleki, R. In vitro study of the binding between chlorpyrfos and sex hormones using headspace solid-phase microextraction combined with high-performance liquid chromatography. Hum. Exp. Toxicol. 2015, 34, 819–827. [Google Scholar] [CrossRef]
- Rich, J.D.; Gabriel, S.M.; Schultz-Norton, J.R. In vitro effects of herbicides and insecticides on human breast cells. ISRN Toxicol. 2012, 2012. [Google Scholar] [CrossRef]
- Moyano, P.; García, J.; García, J.M.; Pelayo, A.; Muñoz-Calero, P.; Frejo, M.T.; Anadon, M.J.; Lobo, M.; Del Pino, J. Chlorpyrifos-induced cell proliferation in human breast cancer cell lines differentially mediated by estrogen and aryl hydrocarbon receptors and KIAA1363 enzyme after 24 h and 14 days exposure. Chemosphere 2020, 251, 126426. [Google Scholar] [CrossRef]
- Vinggaard, A.M.; Breinholt, V.; Larsen, J.C. Screening of selected pesticides for oestrogen receptor activation in vitro. Food Addit. Contam. 1999, 16, 533–542. [Google Scholar] [CrossRef]
- Medjakovic, S.; Zoechling, A.; Gerster, P.; Ivanova, M.M.; Teng, Y.; Klinge, C.M.; Schildberger, B.; Gartner, M.; Jungbauer, A. Effect of nonpersistent pesticides on estrogen receptor, androgen receptor, and aryl hydrocarbon receptor. Environ. Toxicol. 2014, 29, 1201–1216. [Google Scholar] [CrossRef] [PubMed]
- Ventura, C.; Núñez, M.; Miret, N.; Martinel Lamas, D.; Randi, A.; Venturino, A.; Rivera, E.; Cocca, C. Differential mechanisms of action are involved in chlorpyrifos effects in estrogen-dependent or -independent breast cancer cells exposed to low or high concentrations of the pesticide. Toxicol. Lett. 2012, 213, 184–193. [Google Scholar] [CrossRef] [PubMed]
- Dellai, A.; Dridi, D.; Sakouhi, S.; Robert, J.; Djelal, H.; Mosrati, R.; Cherif, A.; Mansour, H. Ben Cytotoxic effect of chlorpyrifos ethyl and its degradation derivatives by Pseudomonas peli strain isolated from the Oued Hamdoun River (Tunisia). Toxicol. Ind. Health 2013, 32, 707–713. [Google Scholar] [CrossRef] [PubMed]
- Ventura, C.; Venturino, A.; Miret, N.; Randi, A.; Rivera, E.; Núñez, M.; Cocca, C. Chlorpyrifos inhibits cell proliferation through ERK1/2 phosphorylation in breast cancer cell lines. Chemosphere 2015, 120, 343–350. [Google Scholar] [CrossRef] [PubMed]
- Nicolopoulou-Stamati, P.; Maipas, S.; Kotampasi, C.; Stamatis, P.; Hens, L. Chemical Pesticides and Human Health: The Urgent Need for a New Concept in Agriculture. Front. Public Health 2016, 4, 148. [Google Scholar] [CrossRef]
- Jaga, K.; Dharmani, C. Sources of exposure to and public health implications of organophosphate pesticides. Rev. Panam. Salud Publica 2003, 14, 171–185. [Google Scholar] [CrossRef]
- Alavanja, M.C.R.; Dosemeci, M.; Samanic, C.; Lubin, J.; Lynch, C.F.; Knott, C.; Barker, J.; Hoppin, J.A.; Sandler, D.P.; Coble, J.; et al. Pesticides and Lung Cancer Risk in the Agricultural Health Study Cohort. Am. J. Epidemiol. 2004, 160, 876–885. [Google Scholar] [CrossRef]
- Kamel, F.; Hoppin, J.A. Association of pesticide exposure with neurologic dysfunction and disease. Environ. Health Perspect. 2004, 112, 950–958. [Google Scholar] [CrossRef]
- Rothlein, J.; Rohlman, D.; Lasarev, M.; Phillips, J.; Muniz, J.; McCauley, L.A. Organophosphate pesticide exposure and neurobehavioral performance in agricultural and nonagricultural Hispanic workers. Environ. Health Perspect. 2006, 114, 691–696. [Google Scholar] [CrossRef]
- Costa, L.G. Current issues in organophosphate toxicology. Clin. Chim. Acta 2006, 366, 1–13. [Google Scholar] [CrossRef]
- Shakeel, M.K. Pesticides and Breast Cancer Risk: A Comparison Between Developed and Developing Countries Asian Pac. J. Cancer Prev. 2010, 11, 173–180. [Google Scholar]
- Werder, E.J. Herbicide, fumigant, and fungicide use and breast cancer risk among farmers’ wives" Environmental Epidemiology. Environ. Epidemiol. 2020, 4, e079. [Google Scholar]
- Kaur, N.; Swain, S.; Banerjee, B.; Sharma, T.; Krishnalata, T. Organochlorine pesticide exposure as a risk factor for breast cancer in young Indian women: A case–control study. South Asian J. Cancer 2019, 8, 212. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.; He, Y.; Xiao, J.; Huang, Y.; Li, A.; He, M.; Wu, K. Risk of breast cancer and adipose tissue concentrations of polychlorinated biphenyls and organochlorine pesticides: A hospital-based case-control study in Chinese women. Environ. Sci. Pollut. Res. 2019, 26, 32128–32136. [Google Scholar] [CrossRef] [PubMed]
- Schug, T.T.; Johnson, A.F.; Birnbaum, L.S.; Colborn, T.; Guillette, L.J.; Crews, D.P.; Collins, T.; Soto, A.M.; Vom Saal, F.S.; McLachlan, J.A.; et al. Minireview: Endocrine disruptors: Past lessons and future directions. Mol. Endocrinol. 2016, 30, 833–847. [Google Scholar] [CrossRef] [PubMed]
- Paleari, L.; Grozio, A.; Cesario, A.; Russo, P. The cholinergic system and cancer. Semin. Cancer Biol. 2008, 18, 211–217. [Google Scholar] [CrossRef]
- Egleton, R.D.; Brown, K.C.; Dasgupta, P. Nicotinic acetylcholine receptors in cancer: Multiple roles in proliferation and inhibition of apoptosis. Trends Pharmacol. Sci. 2008, 29, 151–158. [Google Scholar] [CrossRef]
- Linnoila, R.I. From nicotine to breast cancer, implications of cholinergic receptor pathway. J. Natl. Cancer Inst. 2010, 102, 1298–1299. [Google Scholar] [CrossRef]
- Brown, N.S.; Bicknell, R. Oxidative stress: Its effects on the growth, metastatic potential and response to therapy of breast cancer. Breast Cancer Res. 2001, 3, 323–327. [Google Scholar] [CrossRef] [PubMed]
- Brown, N.S.; Jones, A.; Fujiyama, C.; Harris, A.L.; Bicknell, R. Thymidine Phosphorylase Induces Carcinoma Cell Oxidative Stress and Promotes Secretion of Angiogenic Factors. Cancer Res. 2000, 60, 6298–6302. [Google Scholar]
- Kundu, N.; Zhang, S.; Fulton, A.M. Sublethal oxidative stress inhibits tumor cell adhesion and enhances experimental metastasis of murine mammary carcinoma. Clin. Exp. Metastasis 1995, 13, 16–22. [Google Scholar] [CrossRef] [PubMed]
- Hirohashi, S. Inactivation of the E-cadherin-mediated cell adhesion system in human cancers. Am. J. Pathol. 1998, 153, 333–339. [Google Scholar] [CrossRef]
- Hazan, R.B.; Kang, L.; Whooley, B.P.; Borgen, P.I.; Kang Brian Whooley, L.P. N-Cadherin Promotes Adhesion Between Invasive Breast Cancer Cells and the Stroma. Cell Adhes. Commun. 1997, 4, 399–411. [Google Scholar] [CrossRef] [PubMed]
- Scully, O.J.; Bay, B.-H.; Yip, G.; Yu, Y. Breast Cancer Metastasis. Cancer Genom. Proteom. 2012, 9, 311–320. [Google Scholar]
- Hamidi, H.; Ivaska, J. Every step of the way: Integrins in cancer progression and metastasis. Nat. Rev. Cancer 2018, 18, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Aneja, S.; Gross, C.P.; Soulos, P.R.; Yu, J.B. Geographical Information Systems: Applications and Limitations in Oncology Research. Practice 2011, 25, 1221–1225. [Google Scholar]
- Damalas, C.A.; Koutroubas, S.D. Farmers’ Exposure to Pesticides: Toxicity Types and Ways of Prevention. Toxics 2016, 4, 1. [Google Scholar] [CrossRef]
- van Hemmen, J.J.; Brouwer, D.H. Assessment of dermal exposure to chemicals. Sci. Total Environ. 1995, 168, 131–141. [Google Scholar] [CrossRef]
- VIES, J.E.; PETERSON, J.C. Surveillance of Occupational, Accidental, and Incidental Exposure to Organophosphate Pesticides Using Urine Alkyl Phosphate and Phenolic Metabolite Measurements. Ann. N. Y. Acad. Sci. 1997, 837, 257–268. [Google Scholar] [CrossRef]
- Simaremare, S.R.S.; Hung, C.C.; Hsieh, C.J.; Yiin, L.M. Relationship between organophosphate and pyrethroid insecticides in blood and their metabolites in urine: A pilot study. Int. J. Environ. Res. Public Health 2020, 17, 34. [Google Scholar] [CrossRef]
- Rose, R.L.; Hodgson, E. Metabolism of Toxicants. In A Textbook of Modern Toxicology; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2004; pp. 111–148. [Google Scholar]
- Kapka-Skrzypczak, L.; Cyranka, M.; Skrzypczak, M.; Kruszewski, M. Biomonitoring and biomarkers of organophosphate pesticides exposure—State of the art. Ann. Agric. Environ. Med. 2011, 18, 294–303. [Google Scholar] [PubMed]
- Hioki, K.; Ito, Y.; Oya, N.; Nakayama, S.F.; Isobe, T.; Ebara, T.; Shibata, K.; Nishikawa, N.; Nakai, K.; Kamida, T.; et al. Intra-individual variations of organophosphate pesticide metabolite concentrations in repeatedly collected urine samples from pregnant women in Japan. Environ. Health Prev. Med. 2019, 24, 7. [Google Scholar] [CrossRef] [PubMed]
- Jayatilaka, N.K.; Restrepo, P.; Davis, Z.; Vidal, M.; Calafat, A.M.; Ospina, M. Quantification of 16 urinary biomarkers of exposure to flame retardants, plasticizers, and organophosphate insecticides for biomonitoring studies. Chemosphere 2019, 235, 481–491. [Google Scholar] [CrossRef] [PubMed]
- McKelvey, W.; Jacobson, J.B.; Kass, D.; Barr, D.B.; Davis, M.; Calafat, A.M.; Aldous, K.M. Population-based biomonitoring of exposure to organophosphate and pyrethroid pesticides in New York city. Environ. Health Perspect. 2013, 121, 1349–1356. [Google Scholar] [CrossRef]
- Greshock, J.; Nathanson, K.; Martin, A.M.; Zhang, L.; Coukos, G.; Weber, B.L.; Zaks, T.Z. Cancer cell lines as genetic models of their parent histology: Analyses based on array comparative genomic hybridization. Cancer Res. 2007, 67, 3594–3600. [Google Scholar] [CrossRef]
- Tsuji, K.; Kawauchi, S.; Saito, S.; Furuya, T.; Ikemoto, K.; Nakao, M.; Yamamoto, S.; Oka, M.; Hirano, T.; Sasaki, K. Breast cancer cell lines carry cell line-specific genomic alterations that are distinct from aberrations in breast cancer tissues: Comparison of the CGH profiles between cancer cell lines and primary cancer tissues. BMC Cancer 2010, 10, 15. [Google Scholar] [CrossRef]

| First Author, Year Published | Study Design, Setting, Population, and Period | Exposure Assessment | OP | Exposure Category/ Level (Cases vs. Controls) | Results | Strengths | Weaknesses |
|---|---|---|---|---|---|---|---|
| Mills, 2005 [24] | Case control, Hispanic agricultural workers in California; Cases diagnosed 1988–1994 | Union work histories were linked to the Department of Pesticide Regulation (DPR) Pesticide-Use Reports (PURs) for relevant crop within a given month/year in a given county | Malathion | Low use (14 cases, 62 controls) | OR = 1.89 (95% CI: 0.72, 4.94) | Data based on registry information, so no reporting or selection bias. Assessed differential (high vs. medium vs. low) use of pesticides. | Possible undercount of breast cancer cases due to limited healthcare access by some UFW members. Relatively small sample size. No information on job tasks or protective clothing could have led to exposure misclassification. Unable to assess lifetime cumulative use. Did not analyze exposure from other sources. |
| Medium use (16 cases, 52 controls) | OR = 2.95 (95% CI: 1.07, 8.11) | ||||||
| High use (9 cases, 60 controls) | OR = 1.68 (95% CI: 0.50, 5.62) | ||||||
| Diazinon | Low use (9 cases, 53 controls) | OR = 0.78 (95% CI: 0.12, 4.48) | |||||
| Medium use (17 cases, 68 controls) | OR = 1.54 (95% CI: 0.22, 10.68) | ||||||
| High use (10 cases, 58 controls) | OR = 1.50 (95% CI: 0.18, 12.35) | ||||||
| Case control, Hispanic agricultural workers in California; Cases diagnosed 1995–2001 | Malathion | Low use (17 cases, 85 controls) | OR = 0.79 (95% CI: 0.40, 1.56) | ||||
| Medium use (18 cases, 95 controls) | OR = 0.68 (95% CI: 0.33, 1.43) | ||||||
| High use (14 cases, 87 controls) | OR = 0.50 (95% CI: 0.21, 1.23) | ||||||
| Diazinon | Low use (20 cases, 96 controls) | OR = 1.18 (95% CI: 0.27, 5.20) | |||||
| Medium use (21 cases, 8 controls) | OR = 1.42 (95% CI: 0.30, 6.81) | ||||||
| High use (13 cases, 91 controls) | OR = 0.76 (95% CI: 0.15, 3.92) | ||||||
| Engel, 2005 [25] | Cohort, spouses of pesticide applicators in Iowa and North Carolina; Enrollment period: 1993–1997 Follow-up period: 1993–2000 (mean 4.8 years) | Questionnaire; direct and indirect use at enrollment (n = 30,594) | Any OP use | Ever/never use (86 exposed cases, 7580 exposed controls) | RR = 1.0 (95% CI: 0.8, 1.3) | Prospective, longitudinal design, large sample size, comprehensive exposure assessment, extent of potential confounder control, and exploration of potential effect modulation, such as by family history. Little or no loss to follow-up. | Relatively short follow-up duration and the modest number of cases limited interpretation of the results. Number of exposed cases of premenopausal women was small. Few cases exposed to less commonly used pesticides. Unable to assess lifetime cumulative use. No data about the length of marriage; limited information about the extent of indirect exposure via husband’s use. Self-reported questionnaires may have introduced some reporting bias or inaccurate recall. |
| Premenopausal | RR = 1.1 (95% CI: 0.7, 1.7) | ||||||
| Postmenopausal | RR = 0.9 (95% CI: 0.7, 1.3) | ||||||
| Malathion | Ever/never use (63 exposed cases, 5706 exposed controls) | RR = 0.9 (95% CI: 0.7, 1.2) | |||||
| Premenopausal | RR = 0.9 (95% CI: 0.5, 1.5) | ||||||
| Postmenopausal | RR = 0.9 (95% CI: 0.6, 1.2) | ||||||
| Diazinon | Ever/never use (31 exposed cases, 2977 exposed controls) | RR = 1.0 (95% CI: 0.7, 1.5) | |||||
| Premenopausal | RR = 0.8 (95% CI: 0.4, 1.6) | ||||||
| Postmenopausal | RR = 1.1 (95% CI: 0.7, 1.8) | ||||||
| Chlorpyrifos | Ever/never use (16 exposed cases, 1162 exposed controls) | RR = 1.4 (95% CI: 0.9, 2.4) | |||||
| Premenopausal | RR = 2.2 (95% CI: 1.0, 4.9) | ||||||
| Postmenopausal | RR = 1.0 (95% CI: 0.5, 2.2) | ||||||
| Terbufos | Ever/never use (10 exposed cases, 838 exposed controls) | RR = 1.1 (95% CI: 0.6, 2.1) | |||||
| Premenopausal | RR = 2.6 (95% CI: 1.1, 5.9) | ||||||
| Postmenopausal | RR = 0.5 (95% CI: 0.2, 1.6) | ||||||
| Phorate | Ever/never use (6 exposed cases, 575 exposed controls) | RR = 0.8 (95% CI: 0.4, 1.8) | |||||
| Premenopausal | RR = 1.5 (95% CI: 0.5, 4.9) | ||||||
| Postmenopausal | RR = 0.6 (95% CI: 0.2, 2.0) | ||||||
| Lerro, 2015 [26] | Nested case case, spouses of pesticide applicators, Iowa and North Carolina; Enrollment period: 1993–1997 Follow-up period: 1993–2011 (mean 15.3 years) | Questionnaire; direct and indirect use at enrollment (n = 29,325) | Any OP use | Ever/never use (296 exposed cases, 763 non-exposed cases) | RR = 1.20 (95% CI: 1.01, 1.43) | Longitudinal design with regular linkage to population registries for cancer and mortality outcomes and little or no loss-to-follow-up. Large sample size, comprehensive exposure assessment, extent of potential confounder control, and exploration of potential effect modulation, such as by family history. | Only ~25% of participants reported ever use at enrollment. Only collected information on lifetime ever use, no information on duration or time period of use. Did not distinguish between occupational versus non-occupational use. Self-reported questionnaires may have introduced some reporting bias or inaccurate recall. Did not evaluate indirect exposure. |
| Premenopausal | RR = 1.02 (95% CI: 0.77, 1.36) | ||||||
| Postmenopausal | RR = 1.27 (95% CI: 1.00, 1.62) | ||||||
| Malathion | Ever/never use (223 exposed cases, 836 non-exposed cases) | RR = 1.05 (95% CI: 0.88, 1.26) | |||||
| Premenopausal | RR = 1.04 (95% CI: 0.78, 1.38) | ||||||
| Postmenopausal | RR = 1.03 (95% CI: 0.81, 1.30) | ||||||
| Chlorpyrifos | Ever/never use (50 exposed cases, 1009 non-exposed cases) | RR = 1.41 (95% CI: 1.00, 1.99) | |||||
| Premenopausal | RR = 1.36 (95% CI: 0.79, 2.34) | ||||||
| Postmenopausal | RR = 1.53 (95% CI: 0.96, 2.44) | ||||||
| Terbufos | Ever/never use (37 exposed cases, 1022 non-exposed cases) | RR = 1.52 (95% CI: 0.97, 2.36) | |||||
| Premenopausal | RR = 1.25 (95% CI: 0.61, 2.54) | ||||||
| Postmenopausal | RR = 1.73 (95% CI: 0.93, 3.21) | ||||||
| Diazinon | Ever/never use (118 exposed cases, 941 non-exposed cases) | RR = 1.14 (95% CI: 0.93, 1.38) | |||||
| Premenopausal | RR = 1.01 (95% CI: 0.73, 1.40) | ||||||
| Postmenopausal | RR = 1.11 (95% CI: 0.85, 1.45) | ||||||
| Engel, 2017 [27] | Cohort study, spouses of pesticide applicators, Iowa & North Carolina; Enrollment period: 1993–1997 Follow-up period: 1993–2011 (mean 14.7 years) | Questionnaire, direct and indirect use at enrollment and at 5-y follow-up interview; ever vs. never use (n = 30,594) | Any OP use | Ever/never use (300 exposed cases, 7389 exposed controls) | HR = 1.1 (95% CI: 0.9, 1.2) | Large sample size, direct and indirect exposure assessment of many pesticides before breast cancer diagnosis, extent of potential confounder control, and exploration of potential effect modulation, such as by family history. Long follow-up period including detailed data. | Few women reported use at follow-up. No cumulative assessment available except for in post enrollment period. Limited exposed cases for some OPs. Unable to assess early lifetime exposure. Self-reported questionnaires may have introduced some reporting bias or inaccurate recall. |
| Premenopausal | HR = 1.1 (95% CI: 0.8, 1.6) | ||||||
| Postmenopausal | HR = 1.0 (95% CI: 0.9, 1.2) | ||||||
| Chlorpyrifos | Ever/never use (51 exposed cases, 1130 exposed controls) | HR = 1.4 (95% CI: 1.0, 2.0) | |||||
| Premenopausal | HR = 1.9 (95% CI: 1.0, 3.8) | ||||||
| Postmenopausal | HR = 1.3 (95% CI: 0.9, 1.9) | ||||||
| Diazinon | Ever/never use (118 exposed cases, 2,902 exposed controls) | HR = 1.1 (95% CI: 0.9, 1.3) | |||||
| Premenopausal | HR = 1.1 (95% CI: 0.6, 1.8) | ||||||
| Postmenopausal | HR = 1.1 (95% CI: 0.8, 1.3) | ||||||
| Malathion | Ever/never use (226 exposed cases, 5561 exposed controls) | HR = 1.0 (95% CI: 0.8, 1.2) | |||||
| Premenopausal | HR = 0.9 (95% CI: 0.6, 1.4) | ||||||
| Postmenopausal | HR = 1.0 (95% CI: 0.8, 1.2) | ||||||
| Phorate | Ever/never use (22 exposed cases, 561 exposed controls) | HR = 1.1 (95% CI: 0.7, 1.8) | |||||
| Premenopausal | HR = 2.5 (95% CI: 1.0, 6.2) | ||||||
| Postmenopausal | HR = 0.9 (95% CI: 0.5, 1.6) | ||||||
| Terbufos | Ever/never use (37 exposed cases, 814 exposed controls) | HR = 1.5 (95% CI: 1.0, 2.1) | |||||
| Premenopausal | HR = 2.6 (95% CI: 1.3, 5.4) | ||||||
| Postmenopausal | HR = 1.2 (95% CI: 0.8, 1.9) | ||||||
| Tayour, 2019 [28] | Case control, Non-Hispanic white residents or workers in the California Central Valley | Geographical Information System (GIS)-based method which combines California PUR data, California Department of Water Resources (DWR) land use surveys, and geocoded addresses with ambient pesticide exposure within 500 m of residences or workplaces | Chlorpyrifos | Exposed at residences only (17 cases, 9 controls) | OR = 3.91 (95% CI: 1.29, 11.85) | Use of address histories and registry data reduce potential of recall bias and exposure misclassification. Controlled for known breast cancer risk factors. | Smaller study (155 cases, 150 controls) without dose-response data. Breast cancer cases participating in study were limited to surviving cases and lower stage breast cancers. |
| Exposed at workplaces only (21 cases, 18 controls) | OR = 2.90 (95% CI: 1.12, 7.54) | ||||||
| Exposed at both residences and workplaces (82 cases, 64 controls) | OR = 2.27 (95% CI: 1.18, 4.38) | ||||||
| Diazinon | Exposed at residences only (8 cases, 9 controls) | OR = 1.06 (95% CI: 0.32, 3.50) | |||||
| Exposed at workplaces only (18 cases, 17 controls) | OR = 1.23 (95% CI: 0.47, 3.26) | ||||||
| Exposed at both residences and workplaces (92 cases, 79 controls) | OR 1.30 (95% CI: 0.69, 2.45) |
| OP | First Author, Year Published | Animal Model/ Strain | Treatment | Outcome Measures | Main Findings | Suggested Mechanism(s) | Additional Notes |
|---|---|---|---|---|---|---|---|
| Chlorpyrifos | Kang, 2004 [36] | 20-day-old Sprague-Dawley rats | Injected sc with 2, 10, 50, or 250 mg/kg chlorpyrifos, 2 μg/kg 17ß-estradiol per day for 3 days | Circulating hormone levels | No difference in circulating estradiol levels in group treated with chlorpyrifos compared to group treated with vehicle alone. | Chlorpyrifos can potentially act as an endocrine disruptor. | |
| Chlorpyrifos | Ventura, 2016 [33] | 40-day-old virgin female Sprague-Dawley rats | Ingested orally 0.01 or 1 mg/kg/day for 100 days | Cholinesterase activity; number of ducts and lobular buds; percent of hyperplastic ducts and lobular adenosis; cell proliferation; PCNA staining; PgR and ERa expression; co-repressor of estrogen receptor activity expression; circulating hormone levels | AChE activity not affected; decreased BChE activity; increased number of ducts in 0.01/mg/kg/day treatment group compared to controls treated with vehicle alone; no change in number of lobular buds; increased percentage of hyperplastic ducts in 1/mg/kg/day and 0.01/mg/kg/day treatment groups; increased percentage of lobular adenosis in 0.01 mg/kg/day; no changes observed for 1 mg/kg/day; increased cell proliferation in 1/mg/kg/day and 0.01/mg/kg/day treatment groups; increased PgR expression at both doses; no changes in ERa expression; decreased co-repressors of estrogen receptor activity for 0.1 mg/kg/day treatment group; decreased serum estradiol and progesterone for 1 mg/kg/day treatment group; decreased serum LH at both doses; no change in FSH; 1 mg/kg/day prevented an LH increase after ovariectomy. | Chlorpyrifos is a potential endocrine disruptor and may induce cellular proliferation and other mammary cell disruptions. | 0.01 mg/kg/day is the Acceptable Daily Intake level; 1 mg/kg/day is the No Observed Adverse Effects level. |
| Chlorpyrifos | Ventura, 2019 [34] | 40-day-old virgin female Sprague-Dawley | Ingested orally 0.1 or 1 mg/kg/day + 50 mg/kg body weight NMU at 50, 80, and 110 days old | Mammary tumor incidence; tumor doubling time; latency period, number of tumors per rat; steroid hormone receptor expression levels; DNA methylation and HDAC levels | Increased tumor incidence in both 0.01 and 1 mg/kg/day treatment groups at 110 days but no difference at 150 days; reduced latency period in tumor formation at both doses; increased number of tumors per rat in both treatment groups; no effect on tumor doubling time; decreased ERa and PgR expression; no effect on CDKN1B and BRCA1 promoter methylation levels; increased HDAC mRNA levels in 0.1 mg/kg/day treatment group. | Chlorpyrifos is a potential endocrine disruptor and may alter mammary gland structures. | |
| Malathion | Silinskas, 1975 [30] | 36-day-old female Sprague-Dawley rats | Treated with DMBA, a chemical carcinogen, for 230 days, with or without pre-treatment with 250 ppm malathion via ingestion for 14 days | Mammary gland tumorigenesis; mean latency period; number of tumors per rat; tumor growth | 29/29 rats treated with malathion + DMBA developed mammary tumors, compared to 26/28 rats treated with DMBA alone; rats treated with malathion + DMBA had a shorter mean latency period and higher number of tumors per rat; rats treated with malathion + DMBA had more actively growing tumors. | Malathion inhibits steroid degradation via hydroxylation and may enhance hormone dependent DMBA action. | |
| Malathion | Cabello, 2001 [32] | 16-day-old and 39-day-old, virgin female Sprague-Dawley rats | Injected sc with 17 mg/100 g bw malathion with or without 250 µg/100 g bw atropine, an anticholinergic drug, twice a day for five days | Mammary gland tumorigenesis; density of terminal end buds; density of alveolar buds | 17/70 malathion-treated rats developed mammary tumors compared to 0/70 control saline-treated rats; 39-day-old malathion-treated rats had increased density of TEBs and decreased density of ABs compared to control; 39-day-old atropine + malathion-treated rats had decreased density of TEBs and increased density of ABs compared to malathion-treated rats; no difference in density of TEBs or ABs in 16-day-old treated rats compared to control. | Increased cholinergic stimulation alters enzymatic pathways controlling the cell cycle, promoting TEB proliferation and preventing differentiation into ABs, as seen in mammary carcinogenesis | Different age groups were treated since previous studies demonstrated that rats at different age groups treated with DMBA displayed significantly different results [37,38]. |
| Malathion | Calaf, 2011 [29] | 39-day-old virgin female Sprague-Dawley rats | Injected sc with malathion 22 mg/100 g bw, with or without 17ß-estradiol 30 µg/100 g bw, twice a day for 5 days | Number of proliferative ducts per mm2; average number of secretory lobules per mm2 | Increased average number of proliferative ducts per mm2in malathion-treated rats compared to control and rats treated with estrogen only; estrogen-treated rats had an increased number of secretory lobules compared to other groups. | Malathion may act as an estrogen agonist, enhancing the effects on mammary structures when treated in combination with estrogen. | Specific peaks of catechol estrogens 2-CE and 4-CE in rats with mammary tumors indicated potential usefulness as mammary cancer biomarkers. |
| Malathion | Calaf, 2012 [31] | 39-day-old virgin female Sprague-Dawley rats | Injected sc with malathion 22 mg/100 g bw, with or without 17ß-estradiol 30 µg/100 g bw, or with or without atropine 250 µg/100 g bw, twice a day for 5 days | Number of lobules; number of ducts; immunohistological markers | Increased average number of ducts and lobules in estrogen + malathion treated rats compared to control and atropine-treated rats; increased CYP1A1, mutant p53, c-myc, and c-fos expression; malathion + estrogen displayed synergism; atropine counter-acted effects of malathion. | AChE inhibition; oxidative stress. | |
| Malathion | Omran, 2015 [33], [35] | 39-day-old female Wistar albino rats | Injected ip with 170 mg/kg bw malathion, with or without α-lipoic acid 20 mg/kg bw, twice a day for 5 days | Mammary gland tumorigenesis; immunohistological markers; biochemical markers | 6/10 rats treated with malathion developed mammary ductal carcinomas compared to 0/10 rats in the control group and 1/10 rats treated with malathion and α-lipoic acid; decreased BAX, increased PCNA, and increased mutant p53 protein expression in malathion treated group; decreased FSH, estradiol and progesterone secretion; decreased catalase and superoxide mutase activity; α-lipoic acid, an antioxidant, counteracted effects induced by malathion (as measured by catalase). | Decreased apoptotic signaling; free radical generation; inhibition of pituitary gonadotropin secretion. |
| OP | First Author, Year Published | Cell Line(s) | Treatment | Outcome Measures | Main Findings | Proposed Mechanism(s) |
|---|---|---|---|---|---|---|
| Chlorpyrifos | Vinggaard, 1999 [47] | MCF-7 | Treated with 0.001, 0.01, 1, and 10 uM chlorpyrifos for 6 days. For cell proliferation assays; 0.24–500 uM final concentration for 4 days | Cell proliferation; estrogen receptor activation | Chlorpyrifos did not induce cell proliferation or exhibit estrogen receptor activation. | |
| Chlorpyrifos | Rich, 2012 [45] | MCF-7, MDA-MB-231, and MCF-10A | Treated with 10, 100, 1000, and 10000 nM chlorpyrifos for 48 h | Cell viability | Decreased cell viability by 37% in MCF-7 lines treated with 10,000 nM but this was not statistically significant | May involve estrogen receptor. |
| Chlorpyrifos | Ventura, 2012 [49] | MCF-7 and MDA-MB-231 | Treated with 0.05, 0.5, 5, or 50 uM chlorpyrifos for 10 days | Cell proliferation; ROS production; ERα transactivation; cell cycle protein distribution in G1-S and S phase | 0.05 uM induced cell proliferation while 50 uM induced S-phase arrest in MCF-7; 50 uM induced G2/M phase arrest in MDA-MB-231 | Induces cellular proliferation by acting as an estrogen agonist and activating the ERα pathway. Induces cell cycle arrest, possibly by directly altering MT polymerization or by altering redox balance. |
| Chlorpyrifos | Dellai, 2013 [50] | MCF-7 | Treated with 0–200 µg/mL chlorpyrifos, with and without P. peli up to 4 days | Cell viability; cell proliferation | Decreased cell proliferation up to 50% in dose-dependent manner; this was attenuated by the addition of P. peli | P. peli metabolizes chlorpyrifos, reducing its cytotoxic effects. |
| Chlorpyrifos | Medjakovic, 2014 [48] | MCF-7 and MDA-MB-231 | Treated with 10 uM and 100 uM chlorpyrifos for 24, 48, and 72 h | ERα transactivation; cell growth | Did not transactivate ERa; weakly inhibited cell growth | Can act as a potential estrogen agonist. |
| Chlorpyrifos | Farhadi, 2015 [44] | N/A | 0.75 to 142.62 uM chlorpyrifos + either estrone, 17β-estradiol, and DES | Binding of chlorpyrifos to estrogens | Exhibited high-affinity specific binding for estrone and estradiol and an intermediate affinity binding site for DES under near physiological conditions | Chlorpyrifos may act as an endocrine disruptor by binding to sex hormones. |
| Chlorpyrifos | Ventura, 2015 [51] | MCF-7 and MDA-MB-231 | Treated with 50 uM chlorpyrifos for different times, depending on assay | Cell proliferation; ROS and RNS production; catalase and SOD activity lipid peroxidation; ERK1/2 phosphorylation | Decreased cell proliferation; increased ROS production in both cell lines and increased RNS production in MDA-MB-231; increased catalase activity in both cell lines and decreased SOD activity in MCF-7; increased lipid peroxidation in MCF-7 cells; increased ERK1/2 phosphorylation in both lines. | Increases H2O2 levels, inducing phosphorylation of ERK1/2, which leads to inhibition of cellular proliferation and apoptosis. |
| Chlorpyrifos | Moyano, 2020 [46] | MCF-7 and MDA-MB-231 | Treated with 0.01 to 100 uM chlorpyrifos and its derivative CPFO for 24 h and 14 days | cell proliferation; KIAA1363 enzyme, AhR, Era, and CYP1A1 expression | CPF and its derivative CPFO altered KIAA1363 enzyme, AhR, ERa and CYP1A1 expression, increased cell proliferation in both cell lines through ERa activation in MCF-7 cell lines after 24 h and through KIAA1363 overexpression and AhR activation in both cell lines at both 24 h and 14 days | In addition to acting as an ERa agonist, CPF can alter the expression of the KIAA1363 enzyme leading to cellular proliferation. |
| Dimethoate | Chen, 2002 [43] | MCF-7 | Treated with a 10−11 to 10−6 M dimethoate and 10−9 M estradiol for 144 h | Cell proliferation; ER-competitive binding | Did not significantly increase cell proliferation or inhibit binding of estradiol | Can act as an estrogen agonist and induce mammary cell proliferation but did not display estrogenic activity. |
| Malathion | Chen, 2002 [43] | MCF-7 | Treated with 10−11 to 10−6 M malathion and 10−9 M estradiol for 144 h | Cell proliferation; ER competitive binding | Did not significantly increase cell proliferation or inhibit binding of estradiol | Can act as an estrogen agonist by inducing cellular proliferation and inhibiting the binding of estradiol to the ER but did not display estrogenic activity. |
| Malathion | Gwinn, 2005 [41] | Normal human mammary epithelial cells from 4 strains in their 6th passage | Treated with mixture of 50 µL/mL malathion for 6 and 24 h | Cell viability; changes in gene expression | Did not significantly affect cell viability; increased expression of AKR1C1, AKR1C2, EBBP and decreased expression of PLAT, CPF, RFC3, TYMS, BUB1, and AI859865 in all four cell strains | Alters carcinogen and steroid metabolism, DNA replication, and cell cycle progression. |
| Malathion | Calaf, 2008 [39] | MCF-10F in their 44th passage | Treated for 20 passages with malathion (100 ng/mL) with or without 10−8 M estradiol | Anchorage independent growth; invasive capabilities; gene expression | Cells treated with malathion with or without estradiol had increased anchorage independent growth and invasive capabilities and increased expression of cyclins, CDK-4, IGFBP3, IGFBP5, keratin-18, c-Ha-ras, HSP 27, MCM2, and TP53 | Increases cholinergic stimulation, altering gene expression of proteins important for cell cycle regulation. |
| Malathion | Calaf, 2009 [40] | MCF-10F in their 20th passage | Treated with malathion (2 µL/mL) with or without 10−8 M estradiol for 2 weeks | Anchorage independent growth; invasive capabilities; mutant p53 and c-Ha-ras protein expression; MSI and LOH | Cells treated with malathion with or without estradiol had increased anchorage independent growth and invasive capabilities, increased expression of mutant p53 and c-Ha-ras; increased MSI and LOH | Induces malignant transformation through genomic instability of p53 and c-Ha-ras. |
| Malathion | Kjeldsen, 2013 [42] | MVLN (MCF-7 derivative) | Treated with 10−9 to 10−4 M malathion for 18–24 h | ER transactivation | Treatment with 10−5 M malathion weakly induced ER transactivity | Can act as a potential agonist, activating the ER signaling pathway. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, K.J.; Lee, J.; Park, H.L. Organophosphate Pesticide Exposure and Breast Cancer Risk: A Rapid Review of Human, Animal, and Cell-Based Studies. Int. J. Environ. Res. Public Health 2020, 17, 5030. https://doi.org/10.3390/ijerph17145030
Yang KJ, Lee J, Park HL. Organophosphate Pesticide Exposure and Breast Cancer Risk: A Rapid Review of Human, Animal, and Cell-Based Studies. International Journal of Environmental Research and Public Health. 2020; 17(14):5030. https://doi.org/10.3390/ijerph17145030
Chicago/Turabian StyleYang, Kailynn June, Jennifer Lee, and Hannah Lui Park. 2020. "Organophosphate Pesticide Exposure and Breast Cancer Risk: A Rapid Review of Human, Animal, and Cell-Based Studies" International Journal of Environmental Research and Public Health 17, no. 14: 5030. https://doi.org/10.3390/ijerph17145030
APA StyleYang, K. J., Lee, J., & Park, H. L. (2020). Organophosphate Pesticide Exposure and Breast Cancer Risk: A Rapid Review of Human, Animal, and Cell-Based Studies. International Journal of Environmental Research and Public Health, 17(14), 5030. https://doi.org/10.3390/ijerph17145030






