Health, Functional and Nutritional Determinants of Falls Experienced in the Previous Year—A Cross-Sectional Study in a Geriatric Ward
Abstract
1. Introduction
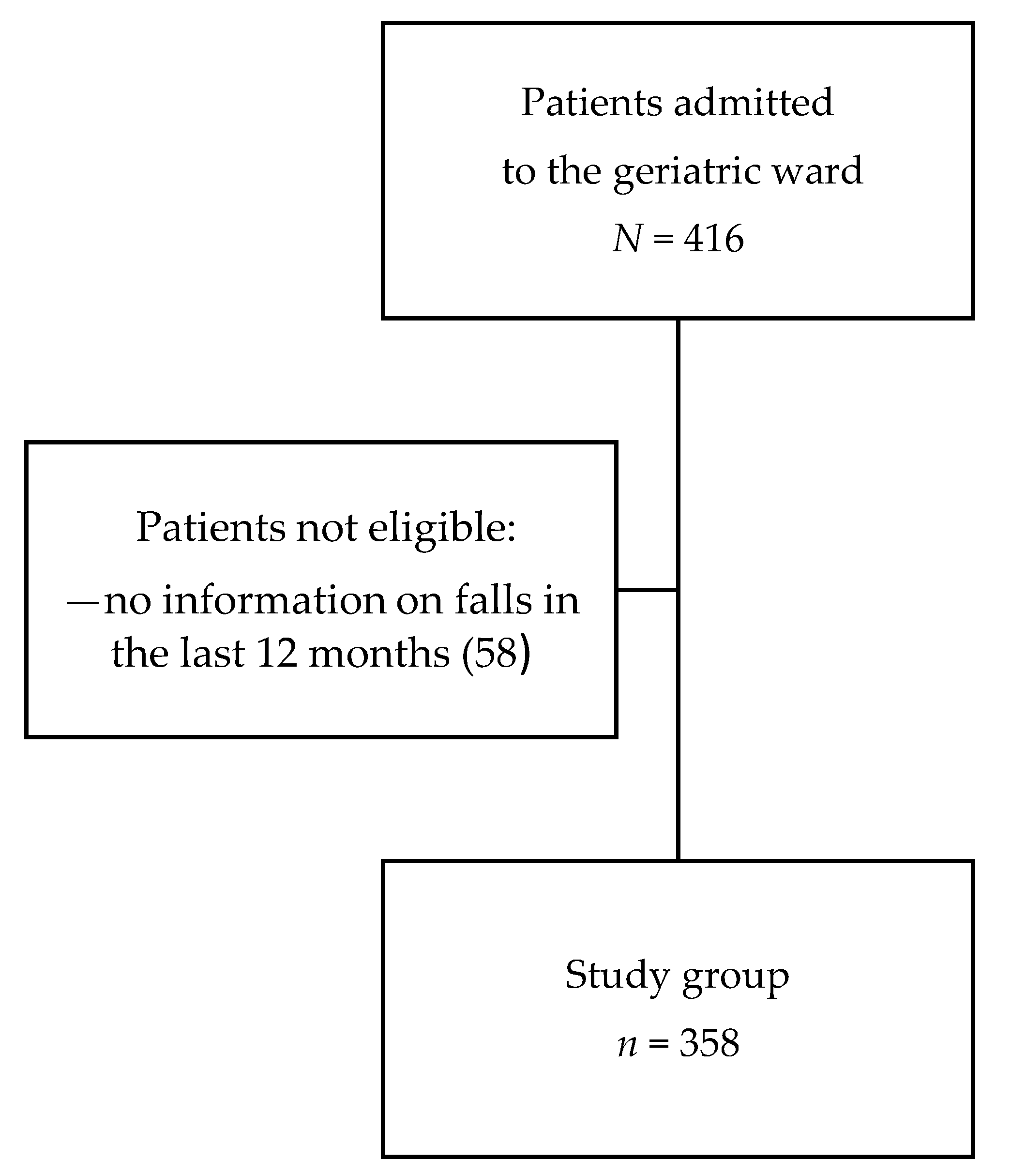
2. Materials and Methods
2.1. Patient Characteristics
2.2. Measurements
2.3. Study Parameters
2.4. Statistical Analysis
2.5. Ethics Approval
3. Results
3.1. Study Cohort Characteristics
3.2. Independent Predictors of Being a Faller
3.3. Study Participants and Nonparticipants
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| ACE-I | angiotensin converting enzyme inhibitor |
| AChE-I | acetylcholine esterase inhibitor |
| AMTS | abbreviated mental test score |
| ARB | angiotensin receptor blocker |
| BDA | benzodiazepines |
| BMI | body mass index |
| CFS | Clinical Frailty Scale |
| CKD-EPI | Chronic Kidney Disease Epidemiology Collaboration |
| CI | confidence interval |
| GDS | Geriatric Depression Scale |
| GFR | glomerular filtration rate |
| IADL | instrumental activities of daily living |
| IQR | interquartile range |
| KDOQI | Kidney Disease Outcome Quality Initiative |
| M | mean |
| Me | median |
| MNA-SF | Mini Nutritional Assessment Short Form |
| NSAIDs | non-steroidal anti-inflammatory drugs |
| NYHA | New York Heart Association |
| OARS | Older Americans Resources and Services |
| OR | odds ratio |
| POMA | Performance Oriented Mobility Assessment |
| SD | standard deviation |
| SSRI | selective serotonin reuptake inhibitors |
| TIA | transient ischemic attack |
| TUG | Timed Up-and-Go Test |
References
- Tabue-Teguo, M.; Grasset, L.; Avila-Funes, J.A.; Genuer, R.; Proust-Lima, C.; Peres, K.; Féart, C.; Amieva, H.; Harmand, G.-C.; Helmer, C.; et al. Prevalence and Co-Occurrence of Geriatric Syndromes in People Aged 75 Years and Older in France: Results From the Bordeaux Three-city Study. J. Gerontol. A Biol. Sci. Med. Sci. 2017, 73, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Wojszel, Z.B.; Bien, B. Falls amongst older people living in the community. Rocz. Akad. Med. Bialymst. 2004, 49, 280–284. [Google Scholar] [PubMed]
- Pandya, C.; Magnuson, A.; Dale, W.; Lowenstein, L.; Fung, C.; Mohile, S.G. Association of falls with health-related quality of life (HRQOL) in older cancer survivors: A population based study. J. Geriatr. Oncol. 2016, 7, 201–210. [Google Scholar] [CrossRef]
- Van Ancum, J.M.; Pijnappels, M.; Jonkman, N.H.; Scheerman, K.; Verlaan, S.; Meskers, C.G.M.; Maier, A.B. Muscle mass and muscle strength are associated with pre- and post-hospitalization falls in older male inpatients: A longitudinal cohort study. BMC Geriatr. 2018, 18, 116. [Google Scholar] [CrossRef] [PubMed]
- Bauer, C.M.; Groger, I.; Rupprecht, R.; Marcar, V.L.; Gassmann, K.G. Prediction of future falls in a community dwelling older adult population using instrumented balance and gait analysis. Z. Gerontol. Geriatr. 2016, 49, 232–236. [Google Scholar] [CrossRef] [PubMed]
- Trevisan, C.; Crippa, A.; Ek, S.; Welmer, A.K.; Sergi, G.; Maggi, S.; Manzato, E.; Bea, J.W.; Cauley, J.A.; Decullier, E.; et al. Nutritional Status, Body Mass Index, and the Risk of Falls in Community-Dwelling Older Adults: A Systematic Review and Meta-Analysis. J. Am. Med. Dir. Assoc. 2019, 20, 569–582 e7. [Google Scholar] [CrossRef]
- Hartog, L.C.; Schrijnders, D.; Landman, G.W.D.; Groenier, K.; Kleefstra, N.; Bilo, H.J.G.; van Hateren, K.J.J. Is orthostatic hypotension related to falling? A meta-analysis of individual patient data of prospective observational studies. Age Ageing 2017, 46, 568–575. [Google Scholar] [CrossRef]
- Parashos, S.A.; Bloem, B.R.; Browner, N.M.; Giladi, N.; Gurevich, T.; Hausdorff, J.M.; He, Y.; Lyons, K.E.; Mari, Z.; Morgan, J.C.; et al. What predicts falls in Parkinson disease?: Observations from the Parkinson’s Foundation registry. Neurol. Clin. Pract. 2018, 8, 214–222. [Google Scholar] [CrossRef]
- Ikutomo, H.; Nagai, K.; Tagomori, K.; Miura, N.; Nakagawa, N.; Masuhara, K. Incidence and Risk Factors for Falls in Women With End-Stage Hip Osteoarthritis. J. Geriatr. Phys. Ther. 2019, 42, 161–166. [Google Scholar] [CrossRef]
- Tanaka, T.; Matsumoto, H.; Son, B.K.; Imaeda, S.; Uchiyama, E.; Taniguchi, S.; Nishino, A.; Miura, T.; Tanaka, T.; Otsuki, T.; et al. Environmental and physical factors predisposing middle-aged and older Japanese adults to falls and fall-related fractures in the home. Geriatr. Gerontol. Int. 2018, 18, 1372–1377. [Google Scholar] [CrossRef]
- Sano, T.; Harada, M.; Sugawara, T.; Isaka, N.; Masuoka, A.; Mikami, A.; Shimamori, Y.; Kurosawa, N. Use of psychotropics and the risk of falls in hospitalized psychiatric patients. Yakugaku Zasshi 2013, 133, 897–903. [Google Scholar] [CrossRef] [PubMed]
- Tinetti, M.E.; Han, L.; Lee, D.S.; McAvay, G.J.; Peduzzi, P.; Gross, C.P.; Zhou, B.; Lin, H. Antihypertensive medications and serious fall injuries in a nationally representative sample of older adults. JAMA Intern. Med. 2014, 174, 588–595. [Google Scholar] [CrossRef] [PubMed]
- Yeung, S.S.Y.; Reijnierse, E.M.; Pham, V.K.; Trappenburg, M.C.; Lim, W.K.; Meskers, C.G.M.; Maier, A.B. Sarcopenia and its association with falls and fractures in older adults: A systematic review and meta-analysis. J. Cachexia Sarcopenia Muscle 2019, 10, 485–500. [Google Scholar] [CrossRef]
- Inouye, S.K.; Studenski, S.; Tinetti, M.E.; Kuchel, G.A. Geriatric syndromes: Clinical, research, and policy implications of a core geriatric concept. J. Am. Geriatr. Soc. 2007, 55, 780–791. [Google Scholar] [CrossRef] [PubMed]
- Mazur, K.; Wilczyński, K.; Szewieczek, J. Geriatric falls in the context of a hospital fall prevention program: Delirium, low body mass index, and other risk factors. Clin. Interv. Aging 2016, 11, 1253–1261. [Google Scholar] [PubMed]
- Milisen, K.; Coussement, J.; Arnout, H.; Vanlerberghe, V.; De Paepe, L.; Schoevaerdts, D.; Lambert, M.; Van Den Noortgate, N.; Delbaere, K.; Boonen, S.; et al. Feasibility of implementing a practice guideline for fall prevention on geriatric wards: A multicentre study. Int. J. Nurs. Stud. 2013, 50, 495–507. [Google Scholar] [CrossRef]
- Cameron, I.D.; Gillespie, L.D.; Robertson, M.C.; Murray, G.R.; Hill, K.D.; Cumming, R.G.; Kerse, N. Interventions for preventing falls in older people in care facilities and hospitals. Cochrane Database Syst. Rev. 2012, 12, Cd005465. [Google Scholar] [CrossRef]
- Aizenberg, D.; Weizman, A.; Weiss, A.; Akopian, M.; Amitai, M.; Beloosesky, Y. The Association in Elderly Hospitalized Patients, Between Psychotropic Drugs and Hip Fractures Resulting from Falls. Exp. Aging Res. 2015, 41, 546–555. [Google Scholar] [CrossRef]
- Avelino-Silva, T.J.; Farfel, J.M.; Curiati, J.A.E.; Amaral, J.R.G.; Campora, F.; Jacob-Filho, W. Comprehensive geriatric assessment predicts mortality and adverse outcomes in hospitalized older adults. BMC Geriatr. 2014, 14, 129. [Google Scholar] [CrossRef]
- Wojszel, Z.B.; Kasiukiewicz, A.; Magnuszewski, L. Health and Functional Determinants of Orthostatic Hypotension in Geriatric Ward Patients: A Retrospective Cross Sectional Cohort Study. J. Nutr. Health Aging 2019, 23, 509–517. [Google Scholar] [CrossRef]
- Tinetti, M.E. Performance-oriented assessment of mobility problems in elderly patients. J. Am. Geriatr. Soc. 1986, 34, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Podsiadlo, D.; Richardson, S. The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [PubMed]
- Roberts, H.C.; Denison, H.J.; Martin, H.J.; Patel, H.P.; Syddall, H.; Cooper, C.; Sayer, A.A. A review of the measurement of grip strength in clinical and epidemiological studies: Towards a standardised approach. Age Ageing 2011, 40, 423–429. [Google Scholar] [CrossRef] [PubMed]
- Mahoney, F.I.; Barthel, D.W. Functional Evaluation: The Barthel Index. Md. State Med. J. 1965, 14, 61–65. [Google Scholar]
- Fillenbaum, G.G.; Smyer, M.A. The development, validity, and reliability of the OARS multidimensional functional assessment questionnaire. J. Gerontol. 1981, 36, 428–434. [Google Scholar] [CrossRef]
- Hodkinson, H.M. Evaluation of a mental test score for assessment of mental impairment in the elderly. 1972. Age Ageing. 2012, 41 (Suppl. 3), iii35–iii40. [Google Scholar] [CrossRef] [PubMed]
- Yesavage, J.A. Geriatric Depression Scale. Psychopharmacol. Bull. 1988, 24, 709–711. [Google Scholar]
- Rockwood, K.; Song, X.; MacKnight, C.; Bergman, H.; Hogan, D.B.; McDowell, I.; Mitnitski, A. A global clinical measure of fitness and frailty in elderly people. CMAJ 2005, 173, 489–495. [Google Scholar] [CrossRef]
- Kaiser, M.J.; Bauer, J.M.; Ramsch, C.; Uter, W.; Guigoz, Y.; Cederholm, T.; Thomas, D.R.; Anthony, P.; Charlton, K.E.; Maggio, M.; et al. Validation of the Mini Nutritional Assessment short-form (MNA-SF): A practical tool for identification of nutritional status. J. Nutr. Health Aging 2009, 13, 782–788. [Google Scholar] [CrossRef]
- Kaufmann, H. Consensus statement on the definition of orthostatic hypotension, pure autonomic failure, and multiple system atrophy. J. Neurol. Sci. 1996, 144, 218–219. [Google Scholar]
- Levey, A.S.; Stevens, L.A.; Schmid, C.H.; Zhang, Y.L.; Castro, A.F., 3rd; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; Greene, T.; et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 2009, 150, 604–612. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyere, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef] [PubMed]
- Okada, K.; Okada, M.; Kamada, N.; Yamaguchi, Y.; Kakehashi, M.; Sasaki, H.; Katoh, S.; Morita, K. Reduction of diuretics and analysis of water and muscle volumes to prevent falls and fall-related fractures in older adults. Geriatr. Gerontol. Int. 2017, 17, 262–269. [Google Scholar] [CrossRef] [PubMed]
- Sotoudeh, G.R.; Mohammadi, R.; Mosallanezhad, Z.; Viitasara, E.; Soares, J.J.F. The prevalence, circumstances and consequences of unintentional falls among elderly Iranians: A population study. Arch. Gerontol. Geriatr. 2018, 79, 123–130. [Google Scholar] [CrossRef] [PubMed]
- Zia, A.; Kamaruzzaman, S.B.; Tan, M.P. The consumption of two or more fall risk-increasing drugs rather than polypharmacy is associated with falls. Geriatr. Gerontol. Int. 2017, 17, 463–470. [Google Scholar] [CrossRef] [PubMed]
- Kalilani, L.; Asgharnejad, M.; Palokangas, T.; Durgin, T. Comparing the Incidence of Falls/Fractures in Parkinson’s Disease Patients in the US Population. PLoS ONE 2016, 11, e0161689. [Google Scholar] [CrossRef]
- Schrag, A.; Choudhury, M.; Kaski, D.; Gallagher, D.A. Why do patients with Parkinson’s disease fall? A cross-sectional analysis of possible causes of falls. NPJ Parkinsons Dis. 2015, 1, 15011. [Google Scholar] [CrossRef]
- Smith, T.O.; Higson, E.; Pearson, M.; Mansfield, M. Is there an increased risk of falls and fractures in people with early diagnosed hip and knee osteoarthritis? Data from the Osteoarthritis Initiative. Int. J. Rheum. Dis. 2018, 21, 1193–1201. [Google Scholar] [CrossRef]
- Zhang, X.M.; Cheng, A.S.K.; Dou, Q.; Zhang, W.; Zeng, Y. Comment on: “Sarcopenia and its association with falls and fractures in older adults: A systematic review and meta-analysis” by Yeung et al. J. Cachexia Sarcopenia Muscle 2020, 11, 330–331. [Google Scholar] [CrossRef]
- Henwood, T.; Hassan, B.; Swinton, P.; Senior, H.; Keogh, J. Consequences of sarcopenia among nursing home residents at long-term follow-up. Geriatr. Nurs. 2017, 38, 406–411. [Google Scholar] [CrossRef]
- Schaap, L.A.; van Schoor, N.M.; Lips, P.; Visser, M. Associations of Sarcopenia Definitions, and Their Components, With the Incidence of Recurrent Falling and Fractures: The Longitudinal Aging Study Amsterdam. J. Gerontol. A Biol. Sci. Med. Sci. 2017, 73, 1199–1204. [Google Scholar] [CrossRef] [PubMed]
- Sim, M.; Prince, R.L.; Scott, D.; Daly, R.M.; Duque, G.; Inderjeeth, C.A.; Zhu, K.; Woodman, R.J.; Hodgson, J.M.; Lewis, J.R. Utility of four sarcopenia criteria for the prediction of falls-related hospitalization in older Australian women. Osteoporos. Int. 2019, 30, 167–176. [Google Scholar] [CrossRef] [PubMed]
- Booth, F.W.; Roberts, C.K.; Laye, M.J. Lack of exercise is a major cause of chronic diseases. Compr. Physiol. 2012, 2, 1143–1211. [Google Scholar]
- Demangeat, J.L.; Geldreich, M.A.; Kessler, B.; Kohlbecker, C.; Sure, M.C.; Jeanmougin, C. Putting into place devices for prevention of falls at the hospital center at Haguenau. Rech. Soins. Infirm. 2009, 99, 26–42. [Google Scholar] [CrossRef]
| Characteristic | All | Fallers | Non-Fallers | p1 | Missing Values |
|---|---|---|---|---|---|
| n (%) | 358 (100.0) | 157 (43.9) | 201 (56.15) | ||
| Age (y), Me (IQR) | 82 (76–86) | 82 (77–86) | 82 (76–85) | 0.23 | – |
| Age (75+), n (%) | 298 (83.2) | 136 (86.6) | 162 (80.6) | 0.13 | – |
| Sex (F), n (%) | 279 (77.9) | 123 (78.3) | 156 (77.6) | 0.86 | – |
| Residence (rural), n (%) | 68 (19.0) | 28 (17.8) | 40 (19.9) | 0.68 | – |
| Number of chronic diseases, Me (IQR) | 5.0 (3.0–6.0) | 5.0 (3.0–6.0) | 4.0 (3.0–6.0) | 0.02 | – |
| Multimorbidity, n (%) | 200 (55.9) | 96 (26.8) | 104 (51.7) | 0.07 | – |
| Number of drugs, Me (IQR) | 7.0 (5.0–9.0) | 7.0 (5.5–9.5) | 7.0 (5.0–9.0) | 0.25 | 8 |
| Polypharmacy, n (%) | 281 (80.3) | 126 (82.9) | 155 (78.3) | 0.34 | 8 |
| Hospitalization in the last year, n (%) | 102 (28.6) | 45 (28.7) | 57 (28.5) | 0.97 | 1 |
| Chronic diseases | |||||
| Parkinson’s disease, n (%) | 41 (11.5) | 28 (17.8) | 13 (6.5) | <0.001 | – |
| Dementia, n (%) | 102 (28.5) | 48 (30.1) | 54 (26.9) | 0.44 | – |
| Hypertension, n (%) | 288 (80.5) | 128 (81.5) | 160 (79.6) | 0.64 | – |
| Ischemic heart disease, n (%) | 195 (54.5) | 87 (55.4) | 108 (53.7) | 0.75 | – |
| Myocardial infarction, n (%) | 36 (10.0) | 17 (10.8) | 19 (9.5) | 0.66 | – |
| Atrial fibrillation, n (%) | 82 (22.9) | 36 (22.9) | 46 (22.9) | 0.99 | – |
| Chronic cardiac failure, n (%) | 135 (37.7) | 66 (42) | 69 (34.3) | 0.14 | – |
| NYHA class I/II, n (%) | 67 (18.7) | 32 (20.4) | 35 (17.4) | ||
| NYHA class III/IV, n (%) | 68 (19) | 34 (21.7) | 34 (16.9) | ||
| Peripheral arterial disease, n (%) | 75 (20.1) | 42 ( 26.8) | 33 (16.4) | 0.02 | – |
| Stroke/ TIA, n (%) | 41 (11.5) | 23 (14.7) | 18 (9.0) | 0.09 | – |
| Osteoarthritis, n (%) | 278 (77.7) | 130 (82.8) | 148 (73.6) | 0.04 | – |
| Osteoporosis, n (%) | 65 (18.2) | 27 (17.2) | 38 (18.9) | 0.68 | – |
| Diabetes, n (%) | 104 (21.9) | 50 (31.9) | 54 (26.9) | 0.30 | – |
| Chronic kidney disease, n (%) | 186 (52.0) | 82 (52.2) | 104 (51.7) | 0.93 | – |
| Orthostatic hypotension, n (%) | 51 (15.7) | 25 (16.6) | 26 (15.0) | 0.70 | 34 |
| Vitamin B12, pg/mL, Me (IQR) | 332.6 (242.2–430.2) | 331.3 (222.1–422.2) | 337.30 (256.9–431.6) | 0.10 | 35 |
| Na, mmol/L, Me (IQR) | 140.0 (138.0–141.0) | 140.0 (138.0–141.0) | 140.0 (138.0–141.0) | 0.94 | 10 |
| eGFR, mL/min/1.73 m2, M (SD) | 58.3 (16.7) | 58.2 (16.8) | 58.4 (16.7) | 0.91 | 10 |
| Serum creatinine, mmol/L, Me (IQR) | 86.6 (74.3–105.2) | 85.75 (72.5–105.2) | 87.52 (76.0–103.4) | 0.76 | 10 |
| Hemoglobin, mmol/L, Me (IQR) | 7.8 (7.2–8.5) | 7.9 (7.2–8.4) | 7.93 (7.2–8.5) | 0.83 | 11 |
| Anemia, n (%) | 149(42.9) | 72 (46.2) | 77 (40.3) | 0.27 | 11 |
| Medications | |||||
| α1-blockers, n (%) | 21 (6.0) | 8 (5.3) | 13 (6.6) | 0.60 | 9 |
| Thyroid hormones, n (%) | 26 (7.5) | 11 (7.2) | 15 (7.6) | 0.89 | 9 |
| Antithyroid drugs, n (%) | 2 (06) | – | 2 (1.0) | 0.51 | 9 |
| Quetiapine, n (%) | 38 (10.9) | 22 (14.5) | 16 (8.1) | 0.06 | 9 |
| Neuroleptics, n (%) | 49 (14.0) | 25 (16.5) | 24 (12.2) | 0.26 | 9 |
| Vitamin D, n (%) | 79 (22.6) | 29 (19.0) | 50 (25.4) | 0.16 | 9 |
| ACE-Is/ ARBs, n (%) | 231 (66.2) | 95 (62.5) | 136 (69.0) | 0.21 | 9 |
| Memantine, n (%) | 11 (3.2) | 3 (2.0) | 8 (4.0) | 0.27 | 9 |
| AChE-Is, n (%) | 35 (10.0) | 17(11.2) | 18 (9.1) | 0.53 | 9 |
| ß-blockers, n (%) | 222 (63.6) | 98 (64.5) | 124 (63.0) | 0.77 | 9 |
| Calcium channel blockers, n (%) | 102 (29.2) | 46 (30.3) | 56 (28.4) | 0.70 | 9 |
| Digoxin, n (%) | 24 (6.9) | 13 (8.6) | 11 (5.6) | 0.28 | 9 |
| Diuretics, n (%) | 165 (47.3) | 65 (42.8) | 100 (50.8) | 0.14 | 9 |
| Lipid lowering drugs, n (%) | 125 (35.8) | 51 (33.6) | 74 (37.6) | 0.44 | 9 |
| BDA, n (%) | 40 (11.4) | 22 (14.4) | 18 (9.1) | 0.13 | 8 |
| SSRI, n (%) | 98 (28.0) | 49 (32.2) | 49 (24.9) | 0.13 | 9 |
| NSAIDs, n (%) | 24 (6.9) | 12 (7.9) | 12 (6.1) | 0.53 | 9 |
| Characteristic | All | Fallers | Non-Fallers | p1 | Missing Values |
|---|---|---|---|---|---|
| n (%) | 358 (100.0) | 157 (43.9) | 201 (56.15) | ||
| Barthel index, Me (IQR) | 95 (80–100) | 90 (75–95) | 95 (85–100) | 0.004 | 6 |
| IADL, Me (IQR) | 8.0 (5.0–11.0) | 7.0 (4.0–10.5) | 9.0 (6.0–12.0) | 0.01 | 10 |
| AMTS, Me (IQR) | 8.0 (6.0–9.0) | 8.0 (7.0–9.0) | 8.0 (6.0–9.0) | 0.58 | 21 |
| GDS, Me (IQR) | 6.0 (3.0–10.0) | 7.0 (3.0–10.0) | 6.0 (3.0–9.0) | 0.34 | 34 |
| Handgrip, kg, Me (IQR) | 18.4 (14.1–23.0) | 18.1 (13.9–22.3) | 18.8 (14.3–24.3) | 0.22 | 32 |
| men, kg, Me (IQR) | 26 (21.0–32.3) | 26.1 (21.5–29.6) | 30.0 (23.0–35.5) | 0.047 | 12 |
| women, kg, Me (IQR) | 16.7 (12.9–20.5) | 16.8 (12.7–19.9) | 17.3 (13.5–21.3) | 0.2 | 20 |
| Dynapenia, n (%) | 143 (43.9) | 73 (47.4) | 70 (40.7) | 0.26 | 32 |
| Severe dynapenia, n (%) | 95 (32.8) | 48 (36.4) | 47 (29.7) | 0.26 | 68 |
| Gait speed, m/s, Me (IQR) | 0.65 (0.40–0.95) | 0.60 (0.37–0.86) | 0.71 (0.43–1.05) | 0.01 | 49 |
| Gait speed ≤ 0.8 m/s, n (%) | 200 (64.7) | 103 (71.0) | 97 (59.1) | 0.03 | 49 |
| POMA, Me (IQR) | 23.0 (18.0–28.0) | 22.0 (17.0–28.0) | 25.0 (19.0–28.0) | 0.005 | 49 |
| TUG, s, Me (IQR) | 17.1 (11.7–27.2) | 17.4 (13.0–28.3) | 16.5 (11.3–25.2) | 0.25 | 64 |
| TUG ≥ 20 s, n (%) | 121 (41.2) | 55 (41.7) | 66 (40.7) | 0.91 | 64 |
| CFS, Me (IQR) | 4.0 (4.0–5.0) | 5.0 (4.0–5.0) | 4.0 (4.0–5.0) | 0.03 | – |
| Severe frailty, n (%) | 58 (16.2) | 31 (19.7) | 27 (13.4) | 0.11 | – |
| Urinary incontinence, n (%) | 146 (41.4) | 78 (49.7) | 68 (34.7) | 0.004 | 5 |
| BMI, kg/m2, M (SD) | 29.35 (5.99) | 29.33 (5.97) | 29.37 (6.02) | 0.92 | 34 |
| BMI < 24 kg/m2, n (%) | 59 (18.2) | 26 (18.7) | 33 (17.9) | 0.84 | 34 |
| BMI > 30 kg/m2, n (%) | 136 (42.0) | 57 (41.0) | 79 (42.7) | 0.76 | 34 |
| MAC, cm, M (SD) | 28.2 (4.0) | 28.1 (4.0) | 28.3 (3.9) | 0.82 | 47 |
| MAC ≤ 22 cm, n (%) | 73 (23.5) | 35 (23.8) | 38 (23.2) | 0.89 | 47 |
| CC, cm, M (SD) | 34.8 (4.5) | 34.6 (4.7) | 35.0(4.4) | 0.50 | 47 |
| CC < 31 cm, n (%) | 53 (17.0) | 29 (19.7) | 24 (14.6) | 0.23 | 47 |
| Albumin, g/L, M (SD) | 39.3 (3.7) | 39.0 (4.0) | 39.5 (4.0) | 0.03 | 24 |
| MNA-SF, Me (IQR) | 12.0 (10.0–13.0) | 12.0 (9.0–13.0) | 13.0 (10.0–14.0) | 0.04 | 10 |
| MNA-SF score < 8, n (%) | 46 (13.2) | 21 (13.6) | 25 (12.9) | 0.84 | 10 |
| Predictors | OR (95% CI) | p |
|---|---|---|
| Age, 75+ years | 1.17 (0.54–2.53) | 0.69 |
| Multimorbidity | 1.01 (0.52–1.98) | 0.97 |
| Chronic cardiac failure | 1.67 (0.88–3.14) | 0.12 |
| Peripheral arterial disease | 0.90 (0.41–2.00) | 0.80 |
| Stroke/TIA | 1.82 (0.71–4.67) | 0.22 |
| Parkinson’s disease | 2.82 (1.07–7.45) | 0.04 |
| Osteoarthritis | 2.08 (1.02–4.23) | 0.04 |
| POMA | 0.95 (0.87–1.02) | 0.16 |
| Barthel index | 1.01 (0.98–1.03) | 0.53 |
| IADL | 0.99 (0.89–1.12) | 0.96 |
| Gait speed | 0.78 (0.18–3.39) | 0.69 |
| CFS | 0.76(0.50–1.16) | 0.21 |
| Urinary incontinence | 1.37 (0.75–2.49) | 0.31 |
| MNA-SF | 1.02 (0.91–1.15) | 0.73 |
| Albumin | 1.00 (0.92–1.09) | 0.96 |
| Vitamin B12 | 0.99 (0.99–1.00) | 0.12 |
| Quetiapine | 1.66 (0.64–4.31) | 0.30 |
| Vitamin D | 1.08 (0.54–2.17) | 0.82 |
| Diuretics | 0.69 (0.39–1.21) | 0.19 |
| BDA | 1.29 (0.54–3.08) | 0.56 |
| SSRI | 1.30 (0.69–2.46) | 0.42 |
| Parameter | Participants | Nonparticipants | p1 |
|---|---|---|---|
| No. (%) of patients | 358 (86.1) | 58 (13.9) | |
| Age, years, Me (IQR) | 84 (78.8–87.3) | 82 (76–86) | 0.22 |
| Age, 75+, n (%) | 298 (83.2) | 52 (89.7) | 0.22 |
| Gender, women, n (%) | 279 (77.9) | 43 (74.1) | 0.52 |
| Barthel index, Me (IQR) | 95 (80–100) | 42.5 (15–70) | <0.001 |
| IADL, Me (IQR) | 8 (5.0–11.0) | 0.0 (0.0–4.0) | <0.001 |
| POMA, Me (IQR) | 23 (18–28) | 8.0 (8.0–15.0) | <0.001 |
| CFS, Me (IQR) | 4.0 (4.0–5.0) | 6.0 (6.0–7.0) | <0.001 |
| Not able to walk, n(%) | 18 (5.2) | 25 (47.2) | <0.001 |
| Severe frailty, n (%) | 58 (16.2) | 44 (75.9) | <0.001 |
| Sarcopenia, n (%) | 143 (43.9) | 21 (87.5) | <0.001 |
| Urinary incontinence, n (%) | 146 (41.4) | 47 (81.0) | <0.001 |
| Dementia, n (%) | 102 (28.5) | 31 (53.4) | <0.001 |
| AMTS, Me (IQR) | 8 (6.0–9.0) | 6.5 (3.0–8.75) | <0.001 |
| Neuroleptics, n (%) | 49 (14.0) | 18 (31.6) | 0.001 |
| Parkinson’s disease, n (%) | 41 (11.5) | 14 (24.1) | 0.008 |
| TIA/stroke, n (%) | 41 (11.5) | 15 (25.9) | 0.003 |
| MNA-SF<8, n (%) | 46 (13.2) | 26 (46.4) | <0.001 |
| Albumin, g/L, M (SD) | 36.6 (3.6) | 39.3 (3.7) | <0.001 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Magnuszewski, L.; Swietek, M.; Kasiukiewicz, A.; Kuprjanowicz, B.; Baczek, J.; Beata Wojszel, Z. Health, Functional and Nutritional Determinants of Falls Experienced in the Previous Year—A Cross-Sectional Study in a Geriatric Ward. Int. J. Environ. Res. Public Health 2020, 17, 4768. https://doi.org/10.3390/ijerph17134768
Magnuszewski L, Swietek M, Kasiukiewicz A, Kuprjanowicz B, Baczek J, Beata Wojszel Z. Health, Functional and Nutritional Determinants of Falls Experienced in the Previous Year—A Cross-Sectional Study in a Geriatric Ward. International Journal of Environmental Research and Public Health. 2020; 17(13):4768. https://doi.org/10.3390/ijerph17134768
Chicago/Turabian StyleMagnuszewski, Lukasz, Marta Swietek, Agnieszka Kasiukiewicz, Bartlomiej Kuprjanowicz, Jan Baczek, and Zyta Beata Wojszel. 2020. "Health, Functional and Nutritional Determinants of Falls Experienced in the Previous Year—A Cross-Sectional Study in a Geriatric Ward" International Journal of Environmental Research and Public Health 17, no. 13: 4768. https://doi.org/10.3390/ijerph17134768
APA StyleMagnuszewski, L., Swietek, M., Kasiukiewicz, A., Kuprjanowicz, B., Baczek, J., & Beata Wojszel, Z. (2020). Health, Functional and Nutritional Determinants of Falls Experienced in the Previous Year—A Cross-Sectional Study in a Geriatric Ward. International Journal of Environmental Research and Public Health, 17(13), 4768. https://doi.org/10.3390/ijerph17134768





