Harm Perceptions of the JUUL E-Cigarette in a Sample of Ever Users
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Measures
2.3. Data Analysis
3. Results
3.1. Participants
3.2. JUUL and Other Tobacco Use Patterns
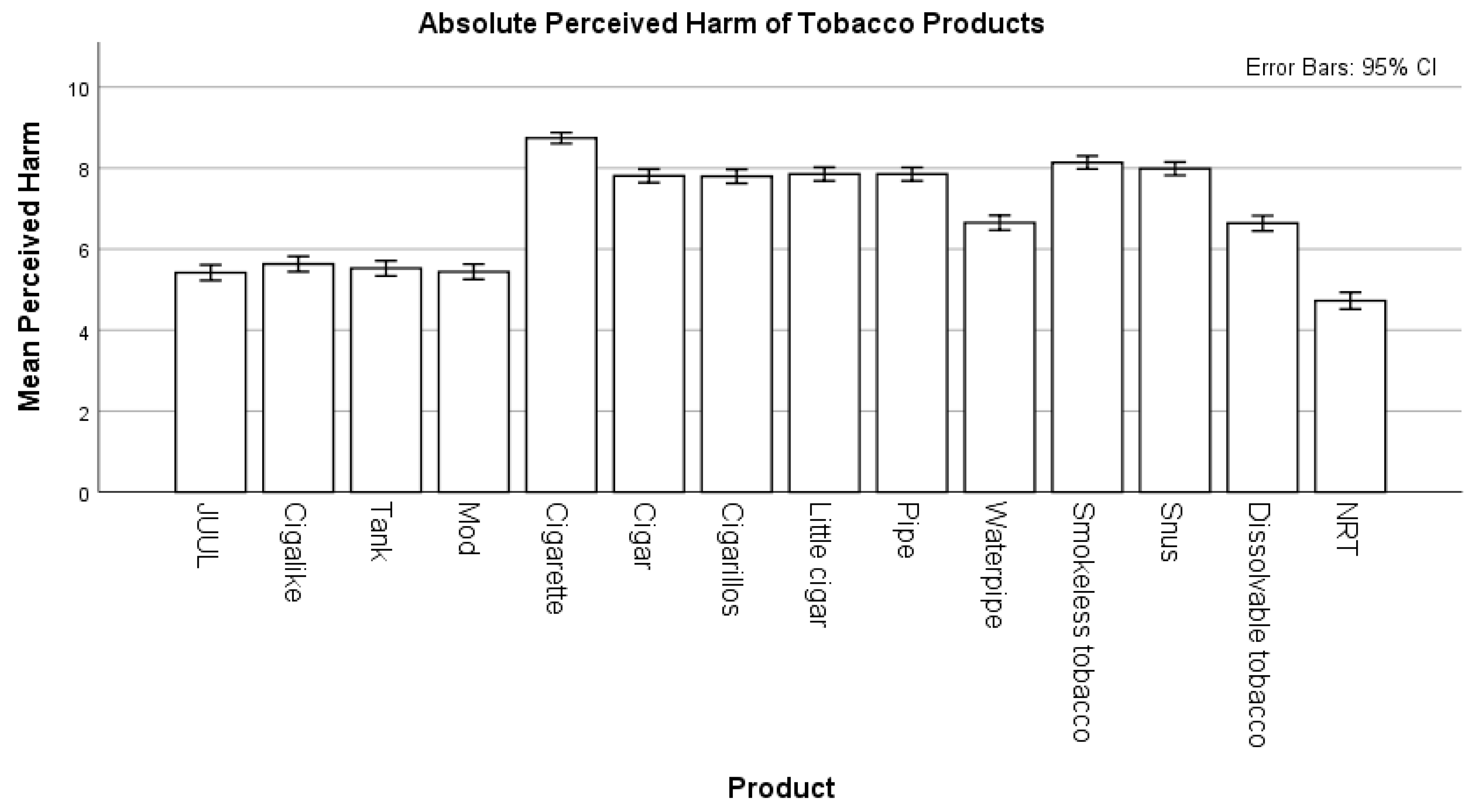
3.3. Absolute Harm Perceptions
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Jamal, A.; Phillips, E.; Gentzke, A.S.; Homa, D.M.; Babb, S.D.; King, B.A.; Neff, L.J. Current Cigarette Smoking Among Adults—United States, 2016. MMWR Morb. Mortal. Wkly. Rep. 2018, 67, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Sharapova, S.R.; Singh, T.; Agaku, I.T.; Kennedy, S.M.; King, B.A. Patterns of E-cigarette Use Frequency—National Adult Tobacco Survey, 2012–2014. Am. J. Prev. Med. 2018, 54, 284–288. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.W.; Asman, K.; Gentzke, A.S.; Cullen, K.A.; Holder-Hayes, E.; Reyes-Guzman, C.; Jamal, A.; Neff, L.; King, B.A. Tobacco Product Use Among Adults—United States, 2017. MMWR Morb. Mortal. Wkly. Rep. 2018, 67, 1225–1232. [Google Scholar] [CrossRef] [PubMed]
- King, B.A.; Alam, S.; Promoff, G.; Arrazola, R.; Dube, S.R. Awareness and Ever-Use of Electronic Cigarettes Among U.S. Adults, 2010–2011. Nicotine Tob. Res. 2013, 15, 1623–1627. [Google Scholar] [CrossRef]
- Huang, J.; Gwarnicki, C.; Xu, X.; Caraballo, R.S.; Wada, R.; Chaloupka, F.J. A comprehensive examination of own- and cross-price elasticities of tobacco and nicotine replacement products in the US. Prev. Med. 2018, 117, 107–114. [Google Scholar] [CrossRef]
- Bao, W.; Xu, G.; Lu, J.; Snetselaar, L.G.; Wallace, R.B. Letters: Research letter. JAMA J. Am. Med. Assoc. 2018, 319, 2039–2041. [Google Scholar] [CrossRef]
- Flouris, A.D.; Chorti, M.S.; Poulianiti, K.P.; Jamurtas, A.Z.; Kostikas, K.; Tzatzarakis, M.N.; Wallace Hayes, A.; Tsatsakis, A.M.; Koutedakis, Y. Acute impact of active and passive electronic cigarette smoking on serum cotinine and lung function. Inhal. Toxicol. 2013, 25, 91–101. [Google Scholar] [CrossRef]
- Wagener, T.L.; Siegel, M.; Borrelli, B. Electronic cigarettes: Achieving a balanced perspective. Addiction 2012, 107, 1545–1548. [Google Scholar] [CrossRef]
- Ambrose, B.K.; Rostron, B.L.; Johnson, S.E.; Portnoy, D.B.; Kaufman, A.R.; Choiniere, C.J. Perceptions of the Relative Harm of Cigarettes and E-cigarettes Among U.S. Youth. Am. J. Prev. Med. 2014, 47, S53–S60. [Google Scholar] [CrossRef]
- Willett, J.G.; Bennett, M.; Hair, E.C.; Xiao, H.; Greenberg, M.S.; Harvey, E.; Cantrell, J.; Vallone, D. Recognition, use and perceptions of JUUL among youth and young adults. Tob. Control 2018, 28, 115–116. [Google Scholar] [CrossRef]
- Soneji, S.; Barrington-Trimis, J.L.; Wills, T.A.; Leventhal, A.M.; Unger, J.B.; Gibson, L.A.; Yang, J.W.; Primack, B.A.; Andrews, J.A.; Miech, R.A.; et al. Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults a systematic review and meta-analysis. JAMA Pediatr. 2017, 171, 788–797. [Google Scholar] [CrossRef] [PubMed]
- Leventhal, A.M.; Stone, M.D.; Andrabi, N.; Barrington-Trimis, J.; Strong, D.R.; Sussman, S.; Audrain-McGovern, J. Association of e-cigarette vaping and progression to heavier patterns of cigarette smoking. JAMA J. Am. Med. Assoc. 2016, 316, 1918–1920. [Google Scholar] [CrossRef] [PubMed]
- Leventhal, A.M.; Strong, D.R.; Kirkpatrick, M.G.; Unger, J.B.; Sussman, S.; Riggs, N.R.; Stone, M.D.; Khoddam, R.; Samet, J.M.; Audrain-McGovern, J. Association of electronic cigarette use with initiation of combustible tobacco product smoking in early adolescence. JAMA J. Am. Med. Assoc. 2015, 314, 700–707. [Google Scholar] [CrossRef]
- Brown, A.; Xing, C. Nicotine Salt Formulations for Aerosol Devices and Methods Thereof. U.S. Patent Application No. 9,215,895, 22 December 2015. [Google Scholar]
- Maloney, S.; Eversole, A.; Crabtree, M.; Soule, E.; Eissenberg, T.; Breland, A. Acute effects of JUUL and IQOS in cigarette smokers. Tob. Control 2020. [Google Scholar] [CrossRef] [PubMed]
- Barrington-Trimis, J.L.; Leventhal, A.M. Adolescents’ Use of “Pod Mod” E-Cigarettes—Urgent Concerns. N. Engl. J. Med. 2018, 379, 1099–1102. [Google Scholar] [CrossRef] [PubMed]
- Talih, S.; Salman, R.; El-Hage, R.; Karam, E.; Karaoghlanian, N.; El-Hellani, A.; Saliba, N.; Shihadeh, A. Characteristics and toxicant emissions of JUUL electronic cigarettes. Tob. Control 2019, 28, 678–680. [Google Scholar] [CrossRef]
- Vallone, D.M.; Bennett, M.; Xiao, H.; Pitzer, L.; Hair, E.C. Prevalence and correlates of JUUL use among a national sample of youth and young adults. Tob. Control 2018, 28, 603–609. [Google Scholar] [CrossRef]
- McKelvey, K.; Baiocchi, M.; Halpern-Felsher, B. Adolescents’ and Young Adults’ Use and Perceptions of Pod-Based Electronic Cigarettes. JAMA Netw. Open 2018, 1, e183535. [Google Scholar] [CrossRef]
- Russell, C.; Katsampouris, E.; Mckeganey, N. Harm and Addiction Perceptions of the JUUL E-Cigarette Among Adolescents. Nicotine Tob. Res. 2020, 22, 713–721. [Google Scholar] [CrossRef]
- Strombotne, K.; Buckell, J.; Sindelar, J.L. Do JUUL and e-cigarette flavours change risk perceptions of adolescents? Evidence from a national survey. Tob. Control 2020. [Google Scholar] [CrossRef]
- Brose, L.S.; Brown, J.; Hitchman, S.C.; McNeill, A. Perceived relative harm of electronic cigarettes over time and impact on subsequent use. A survey with 1-year and 2-year follow-ups. Drug Alcohol Depend. 2015, 157, 106–111. [Google Scholar] [CrossRef] [PubMed]
- Busch, A.M.; Leavens, E.L.; Wagener, T.L.; Buckley, M.L.; Tooley, E.M. Prevalence, Reasons for Use, and Risk Perception of Electronic Cigarettes Among Post-Acute Coronary Syndrome Smokers. J. Cardiopulm. Rehabil. Prev. 2016, 36, 352–357. [Google Scholar] [CrossRef]
- Tackett, A.P.; Lechner, W.V.; Meier, E.; Grant, D.M.; Driskill, L.M.; Tahirkheli, N.N.; Wagener, T.L. Biochemically verified smoking cessation and vaping beliefs among vape store customers. Addiction 2015, 110, 868–874. [Google Scholar] [CrossRef] [PubMed]
- Pearson, J.L.; Richardson, A.; Niaura, R.S.; Vallone, D.M.; Abrams, D.B. e-Cigarette awareness, use, and harm perceptions in US adults. Am. J. Public Health 2012, 102, 1758–1766. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Guo, Y.; Liu, K.; Liu, Z.; Wang, X. E-Cigarette awareness, use, and harm perception among adults: A meta-analysis of observational studies. PLoS ONE 2016, 11, e0165938. [Google Scholar] [CrossRef] [PubMed]
- Andrews, J.A.; Hampson, S.E.; Severson, H.H.; Westling, E.; Peterson, M. Perceptions and Use of E-cigarettes across Time among Emerging Adults. Tob. Regul. Sci. 2016, 2, 70–81. [Google Scholar] [CrossRef]
- Leavens, E.L.; Meier, E.; Brett, E.I.; Stevens, E.M.; Tackett, A.P.; Villanti, A.C.; Wagener, T.L. Polytobacco use and risk perceptions among young adults: The potential role of habituation to risk. Addict. Behav. 2019, 90, 278–284. [Google Scholar] [CrossRef] [PubMed]
- Amazon Mechanical Turk. Amazon Mechanical Turk, Inc. Available online: https://mturk.com/ (accessed on 18 June 2020).
- National Institutes of Health U.S. Food and Drug Administration Opulation Assessment of Tobacco and Health (PATH) Study: Final Adult Baseline (Wave 1) Questionnaire; National Institutes of Health: Bethesda, MD, USA, 2013.
- Glanz, K.; Rimer, B.K.; Viswanath, K. (Kasisomayajula); Orleans, C.T. Health Behavior and Health Education: Theory; Jossey-Bass: San Francisco, CA, USA, 2008; ISBN 0470432489. [Google Scholar]
- Kozlowski, L.T.; Homish, D.L.; Homish, G.G. Daily users compared to less frequent users find vape as or more satisfying and less dangerous than cigarettes, and are likelier to use non-cig-alike vaping products. Prev. Med. Rep. 2017, 6, 111–114. [Google Scholar] [CrossRef]
- Shahab, L.; Goniewicz, M.L.; Blount, B.C.; Brown, J.; McNeill, A.; Alwis, K.U.; Feng, J.; Wang, L.; West, R. Nicotine, Carcinogen, and Toxin Exposure in Long-Term E-Cigarette and Nicotine Replacement Therapy Users. Ann. Intern. Med. 2017, 166, 390. [Google Scholar] [CrossRef]
- Goniewicz, M.L.; Knysak, J.; Gawron, M.; Kosmider, L.; Sobczak, A.; Kurek, J.; Prokopowicz, A.; Jablonska-Czapla, M.; Rosik-Dulewska, C.; Havel, C.; et al. Levels of selected carcinogens and toxicants in vapour from electronic cigarettes. Tob. Control 2014, 23, 133–139. [Google Scholar] [CrossRef]
- Goniewicz, M.L.; Smith, D.M.; Edwards, K.C.; Blount, B.C.; Caldwell, K.L.; Feng, J.; Wang, L.; Christensen, C.; Ambrose, B.; Borek, N.; et al. Comparison of Nicotine and Toxicant Exposure in Users of Electronic Cigarettes and Combustible Cigarettes. JAMA Netw. Open 2018, 1, e185937. [Google Scholar] [CrossRef] [PubMed]
- Wackowski, O.A.; Delnevo, C.D. Young Adults’ Risk Perceptions of Various Tobacco Products Relative to Cigarettes. Heal. Educ. Behav. 2016, 43, 328–336. [Google Scholar] [CrossRef] [PubMed]
- Villanti, A.C.; Cobb, C.O.; Cohn, A.M.; Williams, V.F.; Rath, J.M. Correlates of Hookah Use and Predictors of Hookah Trial in U.S. Young Adults. Am. J. Prev. Med. 2015, 48, 742–746. [Google Scholar] [CrossRef] [PubMed]
- Pokhrel, P.; Fagan, P.; Kehl, L.; Herzog, T.A. Receptivity to E-cigarette Marketing, Harm Perceptions, and E-cigarette Use. Am. J. Health Behav. 2015, 39, 121–131. [Google Scholar] [CrossRef] [PubMed]
- Choi, K.; Forster, J.L. Beliefs and experimentation with electronic cigarettes: A prospective analysis among young adults. Am. J. Prev. Med. 2014, 46, 175–178. [Google Scholar] [CrossRef] [PubMed]
- National Academies of Sciences, Engineering, and M. Public Health Consequences of E-Cigarettes; National Academies Press: Washington, DC, USA, 2018. [Google Scholar]
- Eckel, C.C.; Grossman, P.J. Chapter 113 Men, Women and Risk Aversion: Experimental Evidence. Handb. Exp. Econ. Results 2008, 1, 1061–1073. [Google Scholar] [CrossRef]
- Kraemer, J.D.; Strasser, A.A.; Lindblom, E.N.; Niaura, R.S.; Mays, D. Crowdsourced data collection for public health: A comparison with nationally representative, population tobacco use data. Prev. Med. 2017, 102, 93–99. [Google Scholar] [CrossRef]
- Kaufman, A.R.; Persoskie, A.; Twesten, J.; Bromberg, J. A review of risk perception measurement in tobacco control research. Tob. Control 2020, 29, s50–s58. [Google Scholar] [CrossRef]
| Variables | Never User | Daily | Non-Daily | Trier | ||||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | |
| JUUL | 0 | 0.0% | 90 | 10.8% | 246 | 29.4% | 501 | 59.9% |
| Cigalike | 165 | 20.0% | 46 | 5.6% | 149 | 18.1% | 464 | 56.3% |
| Tank | 201 | 24.7% | 85 | 10.5% | 134 | 16.5% | 393 | 48.3% |
| Mod | 276 | 34.2% | 93 | 11.5% | 101 | 12.5% | 338 | 41.8% |
| Cigarette | 144 | 17.4% | 244 | 29.5% | 112 | 13.5% | 327 | 39.5% |
| Cigar | 507 | 61.0% | 7 | 0.8% | 36 | 4.3% | 281 | 33.8% |
| Cigarillos | 556 | 67.3% | 15 | 1.8% | 38 | 4.6% | 217 | 26.3% |
| Little Cigar | 682 | 82.7% | 11 | 1.3% | 28 | 3.4% | 104 | 12.6% |
| Pipe | 711 | 85.6% | 10 | 1.2% | 12 | 1.4% | 98 | 11.8% |
| Waterpipe | 421 | 50.6% | 7 | 0.8% | 66 | 7.9% | 338 | 40.6% |
| Smokeless Tobacco | 580 | 70.1% | 25 | 3.0% | 31 | 3.7% | 191 | 23.1% |
| Snus | 685 | 83.2% | 5 | 0.6% | 30 | 3.6% | 103 | 12.5% |
| Variables | N | Mean | Std. Deviation | Mean Difference from JUUL | p |
|---|---|---|---|---|---|
| JUUL | 839 | 5.42 | 2.850 | ||
| Cigalike | 839 | 5.63 | 2.793 | −0.215 | 0.924 |
| Tank | 839 | 5.53 | 2.779 | −0.108 | 1.000 |
| Mod | 839 | 5.44 | 2.781 | −0.023 | 1.000 |
| Cigarette | 839 | 8.74 | 1.997 | −3.324 * | <0.001 |
| Cigar | 839 | 7.81 | 2.473 | −2.389 * | <0.001 |
| Cigarillos | 839 | 7.80 | 2.533 | −2.379 * | <0.001 |
| Little cigar | 839 | 7.85 | 2.481 | −2.433 * | <0.001 |
| Pipe | 839 | 7.85 | 2.457 | −2.431 * | <0.001 |
| Waterpipe | 839 | 6.65 | 2.695 | −1.234 * | <0.001 |
| Smokeless tobacco | 839 | 8.14 | 2.376 | −2.721 * | <0.001 |
| Snus | 839 | 7.98 | 2.409 | −2.567 * | <0.001 |
| Dissolvable tobacco | 839 | 6.64 | 2.785 | −1.219 * | <0.001 |
| NRT | 839 | 4.72 | 3.079 | 0.692 * | <0.001 |
| Variables | Unstandardized Coefficients | Standardized Coefficients | t | Sig. | |
|---|---|---|---|---|---|
| B | Std. Error | Beta | |||
| (Constant) | 3.96 | 0.48 | - | 10.94 | <0.001 |
| Female | 0.42 | 0.20 | 0.07 | 2.14 | 0.03 |
| Age | 0.02 | 0.01 | 0.06 | 1.83 | 0.07 |
| Race a | |||||
| Black | 0.21 | 0.32 | 0.02 | 0.67 | 0.51 |
| Other/More than One | −0.29 | 0.29 | −0.03 | −1.01 | 0.32 |
| Current use ≥1 product other than JUUL | −0.50 | 0.21 | −0.08 | −2.32 | 0.02 |
| JUUL Use b | |||||
| Non-Daily | 0.75 | 0.35 | 0.12 | 2.15 | 0.03 |
| Triers | 1.24 | 0.32 | 0.21 | 3.83 | <0.001 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stevens, E.M.; Hébert, E.T.; Tackett, A.P.; Leavens, E.L.S.; Wagener, T.L. Harm Perceptions of the JUUL E-Cigarette in a Sample of Ever Users. Int. J. Environ. Res. Public Health 2020, 17, 4755. https://doi.org/10.3390/ijerph17134755
Stevens EM, Hébert ET, Tackett AP, Leavens ELS, Wagener TL. Harm Perceptions of the JUUL E-Cigarette in a Sample of Ever Users. International Journal of Environmental Research and Public Health. 2020; 17(13):4755. https://doi.org/10.3390/ijerph17134755
Chicago/Turabian StyleStevens, Elise M., Emily T. Hébert, Alayna P. Tackett, Eleanor L. S. Leavens, and Theodore L. Wagener. 2020. "Harm Perceptions of the JUUL E-Cigarette in a Sample of Ever Users" International Journal of Environmental Research and Public Health 17, no. 13: 4755. https://doi.org/10.3390/ijerph17134755
APA StyleStevens, E. M., Hébert, E. T., Tackett, A. P., Leavens, E. L. S., & Wagener, T. L. (2020). Harm Perceptions of the JUUL E-Cigarette in a Sample of Ever Users. International Journal of Environmental Research and Public Health, 17(13), 4755. https://doi.org/10.3390/ijerph17134755






