Randomised Controlled Feasibility Study of the MyHealthAvatar-Diabetes Smartphone App for Reducing Prolonged Sitting Time in Type 2 Diabetes Mellitus
Abstract
1. Introduction
2. Materials and Methods
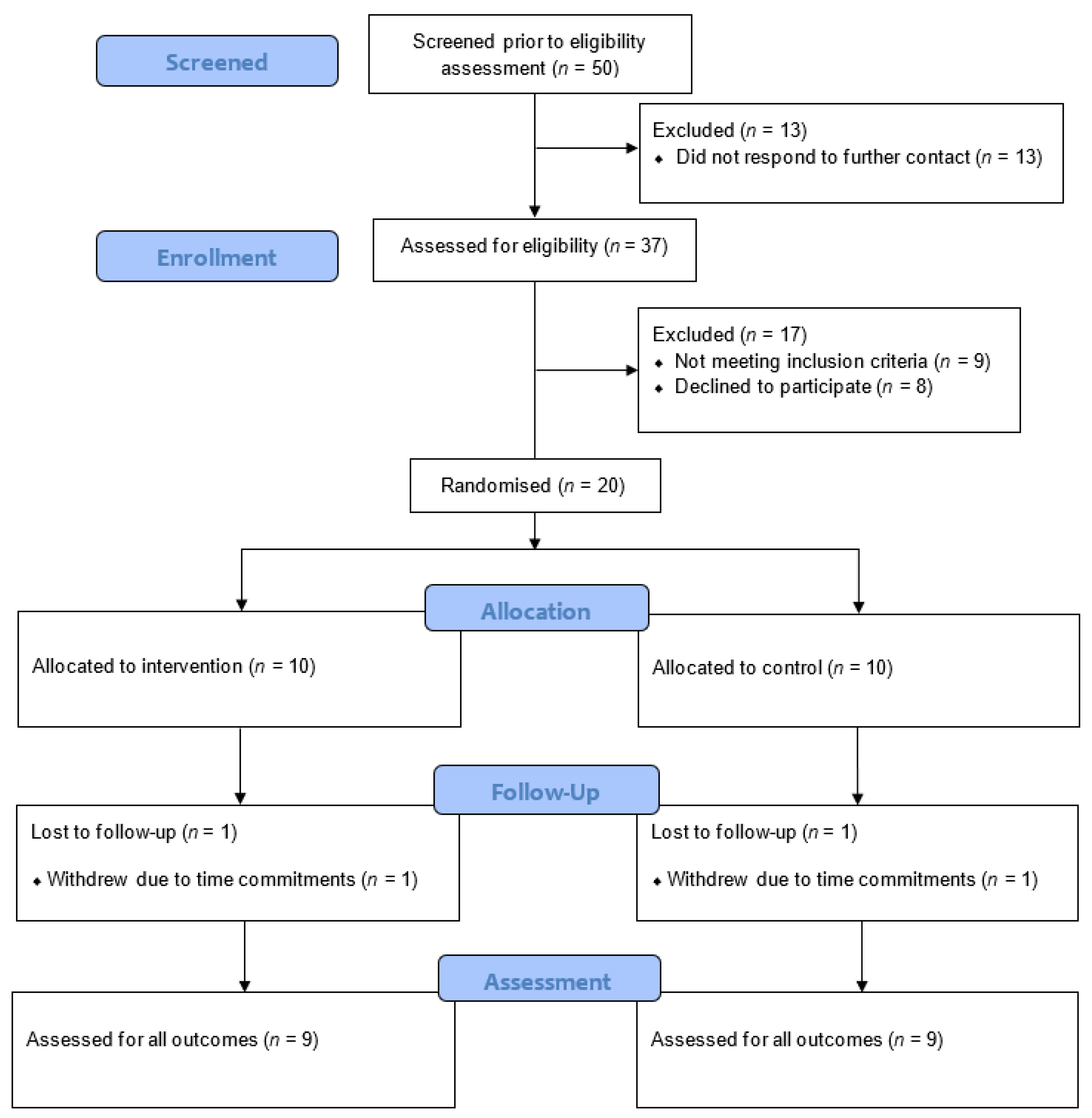
2.1. Study Design and Overview
2.2. Participants
2.3. Intervention
2.3.1. MyHealthAvatar-Diabetes App
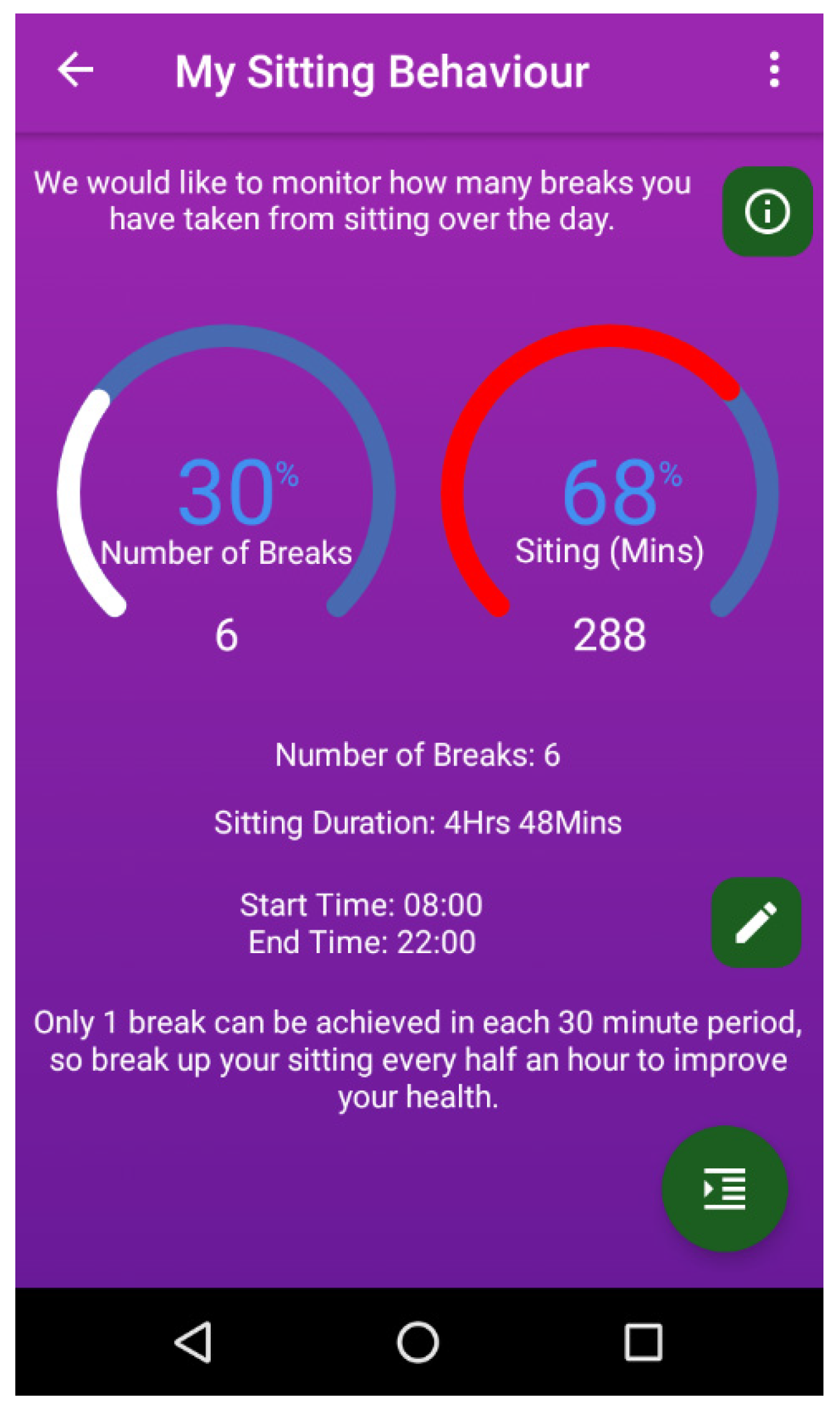
Sitting Behaviour Suite
Physical Activity Suite
Body Weight, Glucose, and Blood Pressure Suites
Medication Alerts, Mood, and Diabetes Information Suites
2.3.2. Text Message Support
2.4. Data Collection
2.5. Primary Outcomes (Feasibility and Acceptability)
2.6. Secondary Outcomes
2.6.1. Sitting, Standing, and Stepping
2.6.2. Anthropometry and Cardiometabolic Health
2.6.3. Determinants of Sitting Behaviour, Mood, and Wellbeing
2.7. Data Analysis
3. Results
3.1. Feasibility
3.2. Participants’ Views on Using the MyHealthAvatar-Diabetes App
3.2.1. Theme 1—Prompting Behaviour Change
3.2.2. Theme 2—Sense of Achievement
3.2.3. Theme 3—Technical Issues
3.2.4. Theme 4—Environmental Barriers
3.3. Changes in Sitting, Standing, and Stepping
3.4. Changes in Anthropometric and Cardiometabolic Outcomes
3.5. Changes in Determinants of Sitting Behaviour, Mood, and Wellbeing
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Data Access Statement
References
- Ogurtsova, K.; da Rocha Fernandes, J.D.; Huang, Y.; Linnenkamp, U.; Guariguata, L.; Cho, N.H.; Cavan, D.; Shaw, J.E.; Makaroff, L.E. IDF Diabetes Atlas: Global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res. Clin. Pract. 2017, 128, 40–50. [Google Scholar] [CrossRef] [PubMed]
- Ali, S.; Stone, M.A.; Peters, J.L.; Davies, M.J.; Khunti, K. The prevalence of co-morbid depression in adults with Type 2 diabetes: A systematic review and meta-analysis. Diabet. Med. 2006, 23, 1165–1173. [Google Scholar] [CrossRef] [PubMed]
- Lloyd, A.; Sawyer, W.; Hopkinson, P. Impact of long-term complications on quality of life in patients with type 2 diabetes not using insulin. Value Health 2001, 4, 392–400. [Google Scholar] [CrossRef] [PubMed]
- Borg, R.; Kuenen, J.C.; Carstensen, B.; Zheng, H.; Nathan, D.M.; Heine, R.J.; Nerup, J.; Borch-Johnsen, K.; Witte, D.R. HbA(1)(c) and mean blood glucose show stronger associations with cardiovascular disease risk factors than do postprandial glycaemia or glucose variability in persons with diabetes: The A1C-Derived Average Glucose (ADAG) study. Diabetologia 2011, 54, 69–72. [Google Scholar] [CrossRef] [PubMed]
- Wilmot, E.G.; Edwardson, C.L.; Achana, F.A.; Davies, M.J.; Gorely, T.; Gray, L.J.; Khunti, K.; Yates, T.; Biddle, S.J.H. Sedentary time in adults and the association with diabetes, cardiovascular disease and death: Systematic review and meta-analysis. Diabetologia 2012, 55, 2895–2905. [Google Scholar] [CrossRef] [PubMed]
- Hamer, M.; Coombs, N.; Stamatakis, E. Associations between objectively assessed and self-reported sedentary time with mental health in adults: An analysis of data from the Health Survey for England. BMJ Open 2014, 4, e004580. [Google Scholar] [CrossRef]
- Bailey, D.P.; Hewson, D.J.; Champion, R.B.; Sayegh, S.M. Sitting Time and Risk of Cardiovascular Disease and Diabetes: A Systematic Review and Meta-Analysis. Am. J. Prev. Med. 2019, 57, 408–416. [Google Scholar] [CrossRef]
- Cooper, A.R.; Sebire, S.; Montgomery, A.A.; Peters, T.J.; Sharp, D.J.; Jackson, N.; Fitzsimons, K.; Dayan, C.M.; Andrews, R.C. Sedentary time, breaks in sedentary time and metabolic variables in people with newly diagnosed type 2 diabetes. Diabetologia 2012, 55, 589–599. [Google Scholar] [CrossRef]
- Healy, G.N.; Dunstan, D.W.; Salmon, J.; Cerin, E.; Shaw, J.E.; Zimmet, P.Z.; Owen, N. Breaks in sedentary time: Beneficial associations with metabolic risk. Diabetes Care 2008, 31, 661–666. [Google Scholar] [CrossRef]
- Bailey, D.P.; Maylor, B.D.; Orton, C.J.; Zakrzewski-Fruer, J.K. Effects of breaking up prolonged sitting following low and high glycaemic index breakfast consumption on glucose and insulin concentrations. Eur. J. Appl. Physiol. 2017, 117, 1299–1307. [Google Scholar] [CrossRef]
- Bailey, D.P.; Broom, D.R.; Chrismas, B.C.R.; Taylor, L.; Flynn, E.; Hough, J. Breaking up prolonged sitting time with walking does not affect appetite or gut hormone concentrations but does induce an energy deficit and suppresses postprandial glycaemia in sedentary adults. Appl. Physiol. Nutr. Metab. 2016, 41, 324–331. [Google Scholar] [CrossRef] [PubMed]
- Bailey, D.P.; Locke, C.D. Breaking up prolonged sitting with light-intensity walking improves postprandial glycemia, but breaking up sitting with standing does not. J. Sci. Med. Sport 2015, 18, 294–298. [Google Scholar] [CrossRef] [PubMed]
- Dempsey, P.C.; Larsen, R.N.; Sethi, P.; Sacre, J.W.; Straznicky, N.E.; Cohen, N.D.; Cerin, E.; Lambert, G.W.; Owen, N.; Kingwell, B.A.; et al. Benefits for Type 2 Diabetes of Interrupting Prolonged Sitting With Brief Bouts of Light Walking or Simple Resistance Activities. Diabetes Care 2016, 39, 964–972. [Google Scholar] [CrossRef] [PubMed]
- Champion, R.B.; Smith, L.R.; Smith, J.; Hirlav, B.; Maylor, B.D.; White, S.L.; Bailey, D.P. Reducing prolonged sedentary time using a treadmill desk acutely improves cardiometabolic risk markers in male and female adults. J. Sports Sci. 2018, 36, 2484–2491. [Google Scholar] [CrossRef]
- Loprinzi, P.D. Accelerometer-determined sedentary and physical activity estimates among older adults with diabetes: Considerations by demographic and comorbidity characteristics. J. Aging Phys. Act. 2014, 22, 432–440. [Google Scholar] [CrossRef] [PubMed]
- Colberg, S.R.; Sigal, R.J.; Yardley, J.E.; Riddell, M.C.; Dunstan, D.W.; Dempsey, P.C.; Horton, E.S.; Castorino, K.; Tate, D.F. Physical Activity/Exercise and Diabetes: A Position Statement of the American Diabetes Association. Diabetes Care 2016, 39, 2065–2079. [Google Scholar] [CrossRef]
- Cowan, L.T.; van Wagenen, S.A.; Brown, B.A.; Hedin, R.J.; Seino-Stephan, Y.; Hall, P.C.; West, J.H. Apps of steel: Are exercise apps providing consumers with realistic expectations? A content analysis of exercise apps for presence of behavior change theory. Health Educ. Behav. 2013, 40, 133–139. [Google Scholar] [CrossRef]
- Ajzen, I. The theory of planned behavior. Organ. Behav. Human Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Jennings, C.A.; Vandelanotte, C.; Caperchione, C.M.; Mummery, W.K. Effectiveness of a web-based physical activity intervention for adults with Type 2 diabetes-a randomised controlled trial. Prev. Med. 2014, 60, 33–40. [Google Scholar] [CrossRef]
- Bert, F.; Giacometti, M.; Gualano, M.R.; Siliquini, R. Smartphones and health promotion: A review of the evidence. J. Med. Syst. 2014, 38, 9995. [Google Scholar] [CrossRef]
- Statista, Smartphone adoption in the United Kingdom (UK) from 2011 to 2018. Available online: https://www.statista.com/statistics/271460/smartphone-adoption-in-the-united-kingdom-uk/ (accessed on 2 August 2019).
- Research2Guidance, 325,000 Mobile Health Apps Available in 2017. Available online: https://research2guidance.com/325000-mobile-health-apps-available-in-2017/ (accessed on 2 August 2019).
- Arrogi, A.; Bogaerts, A.; Seghers, J.; Devloo, K.; Vanden, A.V.; Geurts, L.; Wauters, J.; Boen, F. Evaluation of stAPP: A smartphone-based intervention to reduce prolonged sitting among Belgian adults. Health Promot. Int. 2019, 34, 16–27. [Google Scholar] [CrossRef] [PubMed]
- Bond, D.S.; Thomas, J.G.; Raynor, H.A.; Moon, J.; Sieling, J.; Trautvetter, J.; Leblond, T.; Wing, R.R. B-MOBILE--a smartphone-based intervention to reduce sedentary time in overweight/obese individuals: A within-subjects experimental trial. PLoS ONE 2014, 9, e100821. [Google Scholar] [CrossRef] [PubMed]
- Pellegrini, C.A.; Hoffman, S.A.; Daly, E.R.; Murillo, M.; Iakovlev, G.; Spring, B. Acceptability of smartphone technology to interrupt sedentary time in adults with diabetes. Transl. Behav. Med. 2015, 5, 307–314. [Google Scholar] [CrossRef]
- Miller, W.; Rollnick, S. Motivational Interviewing: Helping People Change; Guilford Press: New York, NY, USA, 2012. [Google Scholar]
- Whitmore, J. Coaching for Performance: GROWing People, Performance and Purpose; Nicholas Brealey Publishing: London, UK, 2002. [Google Scholar]
- Michie, S.; Richardson, M.; Johnston, M.; Abraham, C.; Francis, J.; Hardeman, W.; Eccles, M.P.; Cane, J.; Wood, C.E. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Ann. Behav. Med. 2013, 46, 81–95. [Google Scholar] [CrossRef] [PubMed]
- Eldridge, S.M.; Chan, C.L.; Campbell, M.J.; Bond, C.M.; Hopewell, S.; Thabane, L.; Lancaster, G.A.; O’Cathain, A.; Altman, D.; Bretz, F.; et al. CONSORT 2010 statement: Extension to randomised pilot and feasibility trials. BMJ 2016, 355, 5239. [Google Scholar] [CrossRef]
- Deng, Z.; Zhao, Y.; Parvinzamir, F.; Zhao, X.; Wei, H.; Liu, M.; Zhang, X.; Dong, F.; Liu, E.; Clapworthy, C. MyHealthAvatar: A Lifetime Visual Analytics Companion for Citizen Well-being. In International Conference on Technologies for E-Learning and Digital Entertainmentdoi; Springer International Publishing: Cham, Switzerland, 2016. [Google Scholar]
- David, R.; Dong, F.; Braun, Y.; Graf, N. MyHealthAvatar survey: Scenario based user needs and requirements. In Proceedings of the 2014 6th International Advanced Research Workshop on In Silico Oncology and Cancer Investigation—The CHIC Project Workshop (IARWISOCI), Athens, Greece, 3–4 November 2014. [Google Scholar]
- Henpraserttae, A.; Thiemjarus, S.; Marukatat, S. Accurate Activity Recognition Using a Mobile Phone Regardless of Device Orientation and Location. In Proceedings of the 2011 International Conference on Body Sensor Networks, Dallas, TX, USA, 23–25 May 2011. [Google Scholar]
- Watson, D.; Clark, L.A.; Tellegen, A. Development and validation of brief measures of positive and negative affect: The PANAS scales. J. Pers. Soc. Psychol. 1988, 54, 1063–1070. [Google Scholar] [CrossRef]
- Chater, A. The power of language and emotion in specialist obesity services. Eur. Health Psychol. 2016, 18, 184–188. [Google Scholar]
- Chater, A. Seven steps to help patients overcome a ‘Fear of Finding Out—FOFO’. Nurs. Stand. 2018, 33, 24–25. [Google Scholar] [CrossRef]
- Chater, A.; Courtenay, M. Community nursing and antibiotic stewardship: The importance of communication and training. Br. J. Community Nurs. 2019, 24, 338–342. [Google Scholar] [CrossRef]
- Lyden, K.; Kozey Keadle, S.L.; Staudenmayer, J.W.; Freedson, P.S. Validity of two wearable monitors to estimate breaks from sedentary time. Med. Sci. Sports Exerc. 2012, 44, 2243–2252. [Google Scholar] [CrossRef]
- Grant, P.M.; Ryan, C.G.; Tigbe, W.W.; Granat, M.H. The validation of a novel activity monitor in the measurement of posture and motion during everyday activities. Br. J. Sports Med. 2006, 40, 992–997. [Google Scholar] [CrossRef] [PubMed]
- Winkler, E.A.H.; Bodicoat, D.H.; Healy, G.N.; Bakrania, K.; Yates, T.; Owen, N.; Dunstan, D.W.; Edwardson, C.L. Identifying adults’ valid waking wear time by automated estimation in activPAL data collected with a 24 h wear protocol. Physiol. Meas. 2016, 37, 1653–1668. [Google Scholar] [CrossRef] [PubMed]
- Harrington, D.M.; Welk, G.J.; Donnelly, A.E. Validation of MET estimates and step measurement using the ActivPAL physical activity logger. J. Sports Sci. 2011, 29, 627–633. [Google Scholar] [CrossRef] [PubMed]
- Ajzen, I. From Intentions to Actions: A Theory of Planned Behavior. In Action Control; Kuhl, J., Beckmann, J., Eds.; Springer: Berlin/Heidelberg, Germany, 1985; pp. 11–39. [Google Scholar]
- Francis, J.; Eccles, M.P.; Johnston, M.; Walker, A.E.; Grimshaw, J.M.; Foy, R.; Kaner, E.F.S.; Smith, L.; Bonetti, D. Constructing Questionnaires Based on the Theory of Planned Behaviour: A Manual for Health Services Researchers; Centre for Health Services Research, University of Newcastle upon Tyne: Newcastle upon Tyne, UK, 2004. [Google Scholar]
- Tinkler, L. Measuring National Well-being: Personal Well-being in the UK, 2014 to 2015. Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/wellbeing/bulletins/measuringnationalwellbeing/2015-09-23 (accessed on 2 June 2020).
- Tennant, R.; Hiller, L.; Fishwick, R.; Platt, S.; Joseph, S.; Weich, S.; Parkinson, J.; Secker, J.; Stewart-Brown, S. The Warwick-Edinburgh Mental Well-being Scale (WEMWBS): Development and UK validation. Health Qual. Life Outcomes 2007, 5, 63. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Lancaster, G.A.; Dodd, S.; Williamson, P.R. Design and analysis of pilot studies: Recommendations for good practice. J. Eval. Clin. Pract. 2004, 10, 307–312. [Google Scholar] [CrossRef]
- Maylor, B.D.; Edwardson, C.L.; Zakrzewski-Fruer, J.K.; Champion, R.B.; Bailey, D.P. Efficacy of a multicomponent intervention to reduce workplace sitting time in office workers: A cluster randomized controlled trial. J. Occup. Environ. Med. 2018, 60, 787–795. [Google Scholar] [CrossRef]
- Healy, G.N.; Eakin, E.G.; Owen, N.; Lamontagne, A.D.; Moodie, M.; Winkler, E.A.H.; Fjeldsoe, B.S.; Wiesner, G.; Willenberg, L.; Dunstan, D.W. A cluster randomized controlled trial to reduce office workers’ sitting time: Effect on activity outcomes. Med. Sci. Sports Exerc. 2016, 48, 1787–1797. [Google Scholar] [CrossRef]
- Gardner, B.; Smith, L.; Lorencatto, F.; Hamer, M.; Biddle, S.J.H. How to reduce sitting time? A review of behaviour change strategies used in sedentary behaviour reduction interventions among adults. Health Psychol. Rev. 2016, 10, 89–112. [Google Scholar] [CrossRef]
- Edwardson, C.L.; Yates, T.; Biddle, S.J.H.; Davies, M.J.; Dunstan, D.W.; Esliger, D.W.; Gray, L.J.; Jackson, B.; O’Connell, S.E.; Waheed, G.; et al. Effectiveness of the Stand More AT (SMArT) Work intervention: Cluster randomised controlled trial. BMJ 2018, 363, 3870. [Google Scholar] [CrossRef]
| Characteristic | Control Group | Intervention Group |
|---|---|---|
| Age | 55 (6) | 57 (7) |
| Male (n) | 6 | 3 |
| Female (n) | 3 | 6 |
| Body mass index (kg/m2) | 29.9 (4.7) | 31.1 (6.4) |
| Body fat % | 31.3 (7.8) | 36.9 (9.9) |
| Waist circumference (cm) | 107.2 (11.6) | 104.6 (14.9) |
| Resting systolic blood pressure (mmHg) | 134 (18) | 136 (17) |
| Resting diastolic blood pressure (mmHg) | 83 (11) | 84 (9) |
| Fasting glucose (mmol/L) | 6.57 (1.77) | 5.76 (0.99) |
| 2-h glucose (mmol/L) | 11.64 (3.06) | 10.23 (1.86) |
| Variable | Control Baseline | Control Follow-Up | Within-Group Differences | Intervention Baseline | Intervention Follow-Up | Within-Group Differences | Between-Group Differences | Cohen’s d |
|---|---|---|---|---|---|---|---|---|
| Waking wear time (min) | 959.5 (61.7) | 948.2 (70.2) | −11.3 (87.1) | 936.3 (54.7) | 914.6 (55.5) | −21.7 (28.2) | −10.4 (92.6) | 0.16 |
| % Sitting | 56.8 (13.9) | 53.2 (13.8) | −0.7 (6.2) | 68.2 (8.9) | 66.1 (9.6) | −2.1 (7.3) | −1.4 (10.1) | 0.21 |
| % Standing | 31.2 (11.4) | 33.4 (12.5) | 2.1 (7.4) | 21.6 (5.6) | 24.0 (6.6) | 2.5 (5.2) | 0.4 (9.8) | 0.06 |
| % Stepping | 12.0 (3.8) | 10.5 (3.5) | −1.5 (3.1) | 10.3 (4.2) | 9.9 (3.5) | −0.4 (2.6) | 1.1 (4.4) | 0.38 |
| % Light stepping | 4.9 (1.5) | 4.5 (1.6) | −0.4 (1.4) | 3.5 (1.1) | 3.9 (1.2) | 0.3 (0.8) | 0.7 (1.7) | 0.61 |
| % MVPA stepping | 7.0 (2.4) | 6.0 (2.2) | −1.1 (2.0) | 6.7 (3.3) | 6.0 (2.5) | −0.7 (2.0) | −0.4 (3.2) | 0.20 |
| Breaks in sitting per day | 53.8 (19.2) | 49.3 (15.6) | −4.4 (15.7) | 47.2 (9.9) | 51.6 (14.8) | 4.3 (6.5) | 8.8 (16.9) | 0.72 |
| Prolonged sitting bouts per day | 5.0 (1.6) | 4.7 (2.1) | −0.3 (1.6) | 5.7 (1.1) | 5.8 (1.4) | 0.1 (1.3) | 0.4 (2.5) | 0.27 |
| Steps per day | 8742.7 (2827.4) | 7492.2 (2796.1) | −1250.4 (2467.5) | 7772.7 (3689.8) | 7109.3 (2986.7) | −663.3 (2318.1) | 587.1 (3330.0) | 0.25 |
| Variable | Control Baseline | Control Follow-up | Within-Group Differences | Intervention Baseline | Intervention Follow-Up | Within-Group Differences | Between-Group Differences | Cohen’s d |
|---|---|---|---|---|---|---|---|---|
| Weight (kg) | 90.2 (19.9) | 90.5 (19.2) | 0.2 (1.7) | 89.6 (20.3) | 90.0 (21.7) | 0.4 (2.8) | 0.1 (3.0) | 0.09 |
| Body fat % | 31.3 (7.8) | 31.5 (7.8) | 0.3 (1.5) | 36.9 (9.9) | 35.9 (9.2) | −0.9 (2.6) | −1.2 (3.2) | 0.57 |
| Body mass index (kg/m2) | 29.9 (4.7) | 29.9 (4.6) | 0.1 (0.6) | 31.1 (6.4) | 31.2 (6.9) | 0.1 (1.1) | 0.0 (1.1) | 0.00 |
| Waist circumference (cm) | 107.2 (11.6) | 107.9 (11.6) | 0.7 (3.6) | 104.6 (14.9) | 104.7 (14.1) | 0.1 (2.1) | −0.6 (3.7) | 0.20 |
| Heart rate (bpm) | 66.7 (10.9) | 65.9 (10.0) | −0.8 (5.4) | 63.0 (13.8) | 61.6 (9.8) | −1.4 (7.6) | −0.7 (12.2) | 0.09 |
| Systolic blood pressure (mmHg) | 134.0 (18.1) | 135.6 (20.3) | 1.6 (12.4) | 136.3 (17.2) | 138.2 (20.7) | 1.9 (13.3) | 0.3 (23.2) | 0.02 |
| Diastolic blood pressure (mmHg) | 83.3 (10.7) | 84.3 (13.2) | 1.0 (7.5) | 83.8 (9.5) | 82.4 (9.8) | −1.3 (9.5) | −2.3 (13.5) | 0.27 |
| Fasting blood glucose (mmol/L) | 6.55 (1.76) | 6.73 (2.66) | 0.19 (1.30) | 5.75 (1.01) | 5.66 (1.20) | −0.09 (0.66) | −0.28 (1.30) | 0.27 |
| 2-h blood glucose (mmol/L) | 11.47 (2.96) | 11.22 (3.74) | −0.25 (1.78) | 10.46 (1.67) | 9.56 (1.20) | −0.90 (1.26) | −0.65 (2.69) | 0.42 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bailey, D.P.; Mugridge, L.H.; Dong, F.; Zhang, X.; Chater, A.M. Randomised Controlled Feasibility Study of the MyHealthAvatar-Diabetes Smartphone App for Reducing Prolonged Sitting Time in Type 2 Diabetes Mellitus. Int. J. Environ. Res. Public Health 2020, 17, 4414. https://doi.org/10.3390/ijerph17124414
Bailey DP, Mugridge LH, Dong F, Zhang X, Chater AM. Randomised Controlled Feasibility Study of the MyHealthAvatar-Diabetes Smartphone App for Reducing Prolonged Sitting Time in Type 2 Diabetes Mellitus. International Journal of Environmental Research and Public Health. 2020; 17(12):4414. https://doi.org/10.3390/ijerph17124414
Chicago/Turabian StyleBailey, Daniel P., Lucie H. Mugridge, Feng Dong, Xu Zhang, and Angel M. Chater. 2020. "Randomised Controlled Feasibility Study of the MyHealthAvatar-Diabetes Smartphone App for Reducing Prolonged Sitting Time in Type 2 Diabetes Mellitus" International Journal of Environmental Research and Public Health 17, no. 12: 4414. https://doi.org/10.3390/ijerph17124414
APA StyleBailey, D. P., Mugridge, L. H., Dong, F., Zhang, X., & Chater, A. M. (2020). Randomised Controlled Feasibility Study of the MyHealthAvatar-Diabetes Smartphone App for Reducing Prolonged Sitting Time in Type 2 Diabetes Mellitus. International Journal of Environmental Research and Public Health, 17(12), 4414. https://doi.org/10.3390/ijerph17124414





