Abstract
Metabolic syndrome is an important risk factor for cardiovascular disease, type 2 diabetes mellitus, and all-cause mortality. However, the relationship between napping and metabolic syndrome remains contradictory. The aim of this study was to evaluate the association between nap duration after lunch and prevalence of metabolic syndrome, and subgroup differences in the associations among a government employee population. A total of 5129 participants (mean age 39.4 years) were included in this study. Nap duration after lunch was self-reported, and metabolic syndrome was defined according to the Joint Interim Statement in 2009. Multivariate logistic regression models and adjusted restricted cubic spline functions were used to examine the association and dose-response relationship between nap duration after lunch and prevalence of metabolic syndrome. Of the participants, 17.3% had metabolic syndrome and 81.4% were habitual nappers. Adjusted odds ratio (OR) (95% confidence interval (CI)) of metabolic syndrome for longer nap duration (>90 min) per day was 1.77 (95% CI 1.09 to 2.89), compared with reference (~30 min). Results of stratification analyses indicated the association was found only among females (OR 3.02, 95% CI 1.38 to 6.57), participants without mood symptoms (OR 1.97, 95% CI 1.19 to 3.25), and those having longer night sleep duration (≥8 h) (OR 2.34, 95% CI 1.20 to 4.56). Longer nap duration was also associated with components of metabolic syndrome, including elevated waist circumference, elevated fasting plasma glucose, and elevated triglycerides. In conclusion, longer nap duration after lunch was associated with a higher prevalence of metabolic syndrome in females, people without mood symptoms, and people having longer night sleep duration.
1. Introduction
Metabolic syndrome is a constellation of metabolic abnormalities including central obesity, dyslipidemia, hyperglycemia, and hypertension [1,2,3]. It is an important risk factor for cardiovascular disease, type 2 diabetes mellitus, and all-cause mortality [4,5]. In the Americas, Europe, and India, at least one-fourth of adults suffer from this disorder [6]. In China, the prevalence of metabolic syndrome varies from 17.8% to 36.8% in females and 9.8% to 31.0% in males, depending on the criteria adopted [7,8,9,10,11]. Metabolic syndrome has become a serious public health problem, and enough attention should be given to its associated factors to prevent the syndrome.
Napping (siesta) is a ubiquitous behavior across the human lifespan. In China, napping around noon, which is also called wujiao in Chinese, is considered part of a healthy lifestyle and has been embedded into the culture [12]. A nap may offer benefits such as sleepiness reduction, memory consolidation, cognitive performance enhancement, boost in emotional stability, and endurance performance improvement [13,14,15]. However, in spite of the reported benefits, longer duration napping has also been associated with many negative outcomes. A study of older females in United States reported daily napping significantly increased the risk of death [16]. Moreover, longer day nap was associated with a risk of type 2 diabetes, hypertension, and cardiovascular disease, independent of covariates such as demographic characteristics, lifestyle, sleep quality, disease history, and family history [17,18,19]. In addition to outcomes related to metabolic syndrome, longer nap duration was also believed to increase risk of osteoporosis and renal hyperfiltration [20,21].
Association between nap duration and metabolic syndrome has been reported in several previous studies. Lin et al. conducted a cross-sectional study of 8547 subjects with a mean age of 56 years and reported that a nap of more than 60 min was associated with a higher prevalence of metabolic syndrome only in females [22]. The cross-sectional evidence from the Dongfeng-Tongji retiree cohort study suggested that longer daytime napping (≥90 min) was associated with metabolic syndrome in females [23,24]. Recently, a study of 1679 older adults by van der Pal et al. found a relationship different from the previous studies. They linked both daytime naps of ≤30 min and >30 min to metabolic syndrome, compared with those who did not nap [25]. In addition, a meta-analysis in 2016 showed that longer nap duration (≥60 min) was associated with a higher risk of metabolic syndrome and revealed a J-curve relation; however, the analysis included only two articles and pooled odds ratios (ORs) from different nap duration group (>60 and ≥90 min) into one [26]. The contradictory results can be attributed to differences in the populations, ages, and classifications of nap duration in these studies. The risk of prolonged napping may vary across occupations and age groups, and we cannot ascertain the risk of 61~90 min nap group if the >60 min group was not split. More detailed evidence from wider populations and age groups is needed to resolve these contradictions.
Government employees are physically inactive and therefore more susceptible to chronic diseases than the general population [27,28]; however, the relationship between napping and metabolic syndrome in this population is little known. Therefore, the present study conducted analyses aimed to find out the association of nap duration after lunch with prevalence of metabolic syndrome, and to assess their dose-response relationship and the subgroup differences in a Chinese government employee population.
2. Materials and Methods
2.1. Study Population
This paper presents a cross-sectional study in Changsha City, Hunan Province, which aimed to investigate chronic diseases in the government employee population. In China, government employees mainly include civil servants in government departments, employees of public institutions, and employees of state-owned enterprises. Government departments are organizations that exercise state authority and perform state administrative functions according to law; public institutions are social service organizations, such as universities and hospitals, set up by the government and engaged in education, science and technology, culture, health, etc.; and state-owned enterprises refer to commercial companies fully or largely controlled by the government.
From January 2018 to November 2018, a total of 6414 employees (21–60 years old) from 10 government organizations who agreed to answer the questionnaire online and performed health examinations were recruited via cluster sampling consecutively at the Health Management Center of the Third Xiangya Hospital. A digital self-reported questionnaire platform was established to collect information on participants’ nap and covariates. Recruited participants accessed the questionnaire with URLs sent by Short Messaging Service (SMS) and answered the questions via phone, tablet, or PC. Individuals with self-reported coronary heart disease or stroke (n = 19) and those who did not complete the survey or those with missing values on nap duration, metabolic syndrome components, or covariates (n = 1266) were excluded stepwise, leaving 5129 participants for the final analyses. Compared to characteristics of participants in the analyses, those excluded were more likely to be male, from government departments, with lower positions, higher rates of drinking, higher levels of waist circumference, higher levels of triglycerides, higher levels of high-density lipoprotein cholesterol (HDL-C), and higher levels of blood pressure, while fasting plasma glucose and other features were not statistically different between the two groups (Supplementary Table S1).
2.2. Ethics Approval and Informed Consent
The study was approved by the Ethics Committee of Xiangya School of Public Health, Central South University (No. XYGW-2016-10). Informed consent was obtained from all participants.
2.3. Assessment of Nap Duration
By asking the question, “If you have a habit of napping after lunch in the last six months, what is the average duration of your naps in minutes? (Fill in 0 if you don’t nap),” we collected the nap duration of participants and grouped them by every 30 min, creating the following groups: 0 min, ~30 min, ~60 min, ~90 min, and >90 min. We set the nap duration of ~30 min as a reference group.
2.4. Definition of Metabolic Syndrome
Metabolic syndrome was defined according to the Joint Interim Statement in 2009 [29,30]. Participants with three or more of the following abnormities can be diagnosed as metabolic syndrome:
- (1)
- Elevated waist circumference: ≥85 cm in males or ≥80 cm in females;
- (2)
- Elevated triglycerides (drug treatment for elevated triglycerides is an alternate indicator): ≥150 mg/dL (1.7 mmol/L);
- (3)
- Reduced HDL-C (drug treatment for reduced HDL-C is an alternate indicator): <40 mg/dL (1.0 mmol/L) in males or <50 mg/dL (1.3 mmol/L) in females;
- (4)
- Elevated blood pressure (antihypertensive drug treatment in a patient with a history of hypertension is an alternate indicator): systolic blood pressure ≥130 and/or diastolic blood pressure ≥85 mm Hg;
- (5)
- Elevated fasting plasma glucose (drug treatment of elevated glucose is an alternate indicator): ≥100 mg/dL (5.6 mmol/L).
2.5. Measurement Methods
The information needed to define metabolic syndrome was obtained from the measurements taken during a health examination. Waist circumference was measured at the midpoint between the lower rib and upper margin of the pelvic bone by a trained nurse using a tape. Sitting blood pressure was measured by a skilled physician using a corrected mercury sphygmomanometer after participants had rested for 15 min. Systolic blood pressure and diastolic blood pressure were measured three times, with a 30 s interval, and the average of three readings was calculated for recording. Blood pressure will be re-measured if the difference between the three measurements was greater than 5 mmHg. Blood samples were collected at 07:30–10:00 after a fasting period of 12 h and were stored at −20 °C until tested. Triglycerides and fasting plasma glucose levels were measured by enzymatic colorimetric method, and HDL-C concentration was determined by lipoprotein electrophoresis, both using a Chemistry system Autoanalyzer (Hitachi 7600-110; Tokyo, Japan) in the Medicine Laboratory Department of the Third Xiangya Hospital, which has been accredited by the Chinese Society of Laboratory Medicine.
2.6. Covariates
Covariates in this study included participants’ demographics, lifestyle habits, mood symptoms, sleep-related conditions, family histories, and diets, which were derived from the digital self-reported questionnaire.
Demographic factors included age, gender, affiliation type, marital status, and position level. Affiliations of participants were categorized as government department, public institution, and state-owned enterprise. Marital status was divided into married/cohabitating, unmarried, and divorced/widowed. Position levels were classified into primary title/staff member/clerk, intermediate title/section level, and senior title/division level or above.
Lifestyle habits included smoking status, drinking status, and physical activity. Smoking status was divided into current smoking and non-current smoking (including former smoking and non-smoking). Those who smoked at least one cigarette a day for more than six months were considered as current smoking. Drinking was dichotomized into current drinking versus non-current drinking, which included ever drinking and never drinking. Participants who drank alcohol at least once a week for at least six months were defined as current drinking. Physical activity was categorized into participation and non-participation, with the former having to exercise more than once a week on average.
We used depression and anxiety conditions to represent mood symptoms. Depression and anxiety were evaluated by Patient Health Questionnaire-2 (PHQ-2) and General Anxiety Disorder-2 (GAD-2), respectively. Participants with a score of three or more for PHQ-2 and/or GAD-2, or with a self-reported depression or anxiety diagnosis were considered to have mood symptoms [31,32].
Sleep-related conditions were measured using items of the Pittsburgh sleep quality index (PSQI) [33]. Night sleep duration was calculated as the interval between usual bedtime and usual getting-up time. Use of sleeping medication was grouped into using and not using during the past month. Night sleep quality was classified into good, fair, and bad.
In addition, a family history of hypertension, cancer, or diabetes mellitus was considered to be present if either grandparents, parents or sibling had the disease. Diet frequency of coarse cereals, meat, poultry, aquatic products, egg products, vegetables, dairy products, fruits, and dessert was divided into the following five groups: daily, 4–6 days a week, 1–3 days a week, less than once a week, and rarely or never.
2.7. Statistical Analyses
The mean and standard deviation (SD) or proportion (%) of covariate characteristics were presented among participants with or without metabolic syndrome. Student t-tests were used for numerical variables to evaluate the differences of characteristics between groups, and chi-square tests were used for categorical variables. Logistic regression models were used to estimate ORs and corresponding 95% confidence intervals (CIs) of metabolic syndrome for each nap duration. In the main analysis, the full model was adjusted for demographic factors (age, gender, affiliation type, marital status, and position level), lifestyle habits (smoking status, drinking status, and physical activity), mood symptoms, and sleep-related covariates (night sleep duration hours, bedtime at night, use of sleeping medicine, and sleep quality).
To examine associations in different participants, analyses were explored across subgroups stratified by gender, mood symptoms, and night sleep duration (<7 h, 7~ h, and 8~ h). Furthermore, multivariable restricted cubic spline (RCS) functions with logistic regression models were performed to explore the curvilinear dose-response relationship of nap duration and prevalence of metabolic syndrome visually, with five knots located at nap duration quantiles of 5%, 27.5%, 50%, 72.5%, and 95% [34]. Logistic regression models were also used to test the relationships between nap duration and components of metabolic syndrome. Subgroup, RCS and components regression analyses were all fitted with the same covariates as in the main analysis.
In sensitivity analyses, four procedures were conducted to examine the robustness of the results. First, in addition to covariates in the main analysis, family history and diet frequency factors were further controlled, including family history of hypertension, cancer, and diabetes mellitus, and weekly frequency of eating coarse cereals, meat, poultry, aquatic products, egg products, vegetables, dairy products, fruits, and dessert. Second, because the method of dealing with missing data in analyses was listwise deletion and information of deleted data was not utilized, multivariate imputation by chained equations was further used, and the association between nap duration after lunch and prevalence of metabolic syndrome was reevaluated by pooling the results of five imputed data sets [35]. Third, we performed a multilevel logistic regression model, in which the individuals were level 1 and the government organizations were level 2, to account for different intercepts of 10 affiliations in regression. Fourth, we also adjusted potential confounders through propensity score stratifying analysis, in which propensity scores were calculated by logistic regression with dependent variable dichotomized by whether nap duration was greater than 90 min and were divided into six strata.
All analyses and plots were performed with packages “base” (version 4.0.0), “stats” (4.0.0), “tableone” (0.11.1), “rms” (5.1–4), “mice” (3.8.0), “lme4” (1.1–23), “MatchIt” (3.0.2), “forestplot” (1.9), “ggplot2” (3.3.0), and “ggpubr” (0.3.0) in R. P values < 0.05 (two-sided tests) were considered statistically significant.
3. Results
3.1. Characteristics of Participants
Of 5129 participants, the mean (SD) age was 39.4 (9.3) years, 59.0% were female, 17.3% had metabolic syndrome, and 81.4% were habitual nappers with a mean (SD) duration of 38.1 (25.6) minutes. Table 1 presents characteristics of study population according to whether they had metabolic syndrome. Subjects with metabolic syndrome tended to be older, male, married or cohabitating, and were more likely to have higher position and longer nap duration after lunch than those without metabolic syndrome. Besides, subjects with nap duration of >90 min had the highest prevalence of metabolic syndrome among all nap duration groups (Supplementary Table S2).

Table 1.
Characteristics of participants according to metabolic syndrome.
3.2. Association between Nap Duration after Lunch and Prevalence of Metabolic Syndrome
Figure 1 shows the association between nap duration after lunch and prevalence of metabolic syndrome when the duration was grouped by every 30 min. After adjusting for demographic factors, lifestyle habits, mood symptoms, and sleep-related characteristics, the OR of metabolic syndrome for participants with nap duration of >90 min was 1.77 (95% CI 1.09 to 2.89), compared with those with nap duration of ~30 min. The results were similar when fewer covariates were included (Supplementary Figure S1).
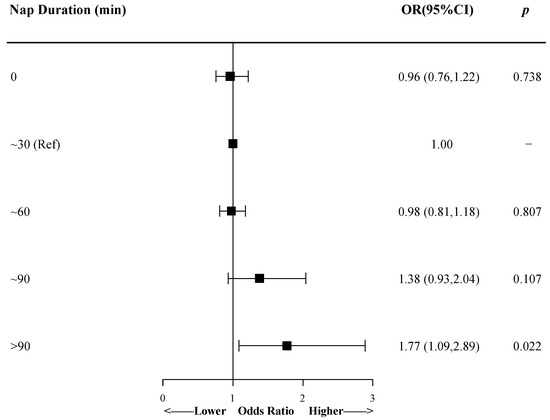
Figure 1.
The association between nap duration and prevalence of metabolic syndrome by logistic regression model. Model was adjusted for demographic factors, lifestyle habits, mood symptoms, and sleep-related characteristics. Small squares represent the point estimates of odds ratios, and horizontal lines represent 95% CIs. OR, odds ratio; CI, confidence interval; Ref, reference.
The subgroup analyses according to gender found a similar relationship in females, and the OR for longer nap duration (>90 min) obviously increased to 3.02 (95% CI 1.38 to 6.57), but the association was not observed in males (Figure 2). Moreover, females who did not nap had a higher OR (1.19, 95% CI 0.82 to 1.72) than males, though the difference was not significant. When the analysis was restricted to subjects without mood symptoms, the OR for >90 min group mildly increased to 1.97 (95% CI 1.19 to 3.25). However, it was not significant among participants with symptoms of anxiety and/or depression, and indeed the OR seemed to decrease as the nap duration increased. The association was significant only in people with ≥8 hours sleep at night (OR 2.34, 95% CI 1.20 to 4.56) when subgroup analyses were stratified by night sleep duration. There was no interaction between nap duration and gender, mood symptoms, or nighttime sleep duration (p > 0.05 for interaction).
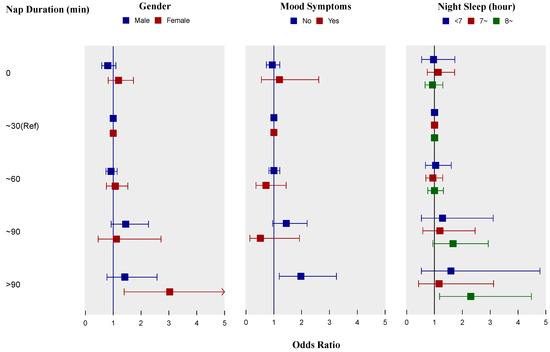
Figure 2.
Subgroup analyses of associations between nap duration and prevalence of metabolic syndrome by logistic regression models according to gender, mood symptoms, and night sleep hours. All three models were adjusted for age, affiliation, marital status, position level, smoking status, drinking status, physical activity, bedtime at night, use of sleeping medicine, and sleep quality, and were adjusted for gender, mood symptoms, and night sleep duration as appropriate. In subgroup analysis of participants with mood symptoms, the odds ratio for group of >90 min was absent because no participant in this group had metabolic syndrome. Small squares represent the point estimates of odds ratios and horizontal lines represent 95% confidence intervals. Ref, reference.
Figure 3 displays multivariate adjusted restricted cubic spline curve of all participants—the OR initially decreased and reached its lowest at a nap of about 15 min, and then it increased slightly until about 45 min, followed by a relatively rapid increase at longer nap duration. Females had a similar trough around 15 min, while ORs for all nap durations were not significant among males (Supplementary Figure S2).
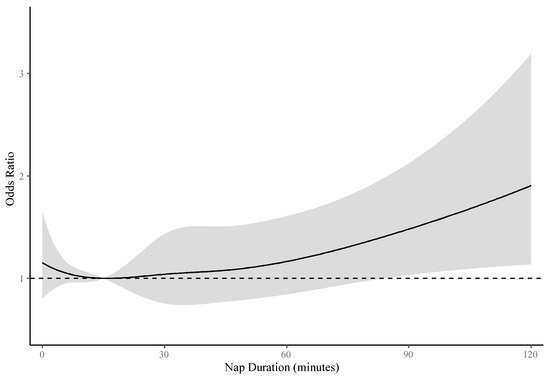
Figure 3.
The dose-response relationship between nap duration and prevalence of metabolic syndrome. The curve was estimated by restricted cubic spline function with five knots and logistic regression model adjusted for age, gender, affiliation, marital status, position level, smoking status, drinking status, physical activity, mood symptoms, night sleep duration hours, bedtime at night, use of sleeping medicine, and sleep quality. The reference was set to 15 min. The shadow represents 95% confidence intervals of odds ratios. The dotted line represents level of odds ratio equal to 1.
3.3. Associations between Nap Duration after Lunch and Metabolic Syndrome Components
Table 2 lists the multivariable logistic regression results of the associations between nap duration after lunch and metabolic syndrome components. For all participants, compared with ~30 min group, ORs of elevated waist circumference and elevated fasting plasma glucose for longer nap duration (>90 min) were 1.55 (95% CI 1.02 to 2.35) and 1.59 (95% CI 1.02 to 2.47), respectively. Of elevated triglycerides, ~90 min group also had an OR (1.48, 95% CI 1.04 to 2.11) with statistical significance, while associations of other components were not significant. For females, longer nap duration (>90 min) was associated with elevated waist circumference (OR 2.12, 95% CI 1.22, 3.70) and elevated fasting plasma glucose (OR 2.53, 95% CI 1.41, 4.53). For males, only ~90 min group had a statistically significant OR (1.87, 95% CI 1.21, 2.91) of elevated triglycerides.

Table 2.
Adjusted odds ratios (ORs) of components of metabolic syndrome for nap duration groups.
3.4. Sensitivity Analyses
The results of the sensitivity analyses showed that the association of longer nap duration (>90 min) with metabolic syndrome was consistent before (OR 1.77, 95% CI 1.09 to 2.89) and after (OR 1.79, 95% CI 1.08 to 2.96) additional adjusting for family history and diet frequency. It also did not change substantially in multiple imputation (OR 1.69, 95% CI 1.06 to 2.69) and multilevel model (OR 1.73, 95% CI 1.06 to 2.82). After adjusting confounders by propensity score, the OR of metabolic syndrome for >90 min nap group was 1.65 (95% CI 1.08–2.52), compared with 0~90 min group (Supplementary Table S3).
4. Discussion
The present study suggested that longer nap duration after lunch (>90 min) was associated with a higher prevalence of metabolic syndrome (OR 1.77, 95% CI 1.09 to 2.89). Subgroup analyses suggested the association was found only in females (OR 3.02, 95% CI 1.38 to 6.57), participants without mood symptoms (OR 1.97, 95% CI 1.19 to 3.25), and those having longer night sleep duration (OR 2.34, 95% CI 1.20 to 4.56). The nap duration with a lower prevalence of metabolic syndrome appeared to be less than 45 min. Our findings also indicated that longer nap duration was associated with the components of metabolic syndrome, including elevated waist circumference, elevated fasting plasma glucose, and elevated triglycerides.
Napping is traditionally believed to be a good habit and beneficial to health; however, recent studies have shown that longer naps can be harmful. A result pooled by Yamada et al. from 11 cohort studies showed that napping for at least 60 min a day was associated with higher incidence of cardiovascular disease and elevated all-cause mortality compared with not napping [36]. Daytime napping also tended to be a risk factor of diabetes mellitus and hypertension [17,18,37]. Several studies have examined the relationship between daytime nap and risk of metabolic syndrome. The main finding of the present study was consistent with the cross-sectional result of the Dongfeng-Tongji retiree cohort study that napping more than 90 min was associated with a higher prevalence of metabolic syndrome only in females [23]. However, our results have not found a relationship between <90 min nap and metabolic syndrome yet, in contrast to studies conducted by Lin et al. and van der Pal et al. [22,25]. The five-year follow-up study of the Dongfeng-Tongji cohort did not performed gender-specific analyses, and there was no statistically significant association observed between nap and the incidence of metabolic syndrome components [24]. Overall, this study suggested that only longer nap duration after lunch was associated with metabolic syndrome prevalence rather than any duration.
The biological mechanisms linking longer nap duration to metabolic syndrome remain unclear. However, there are several possible speculations. Mistimed sleep during the daytime might induce circadian misalignment, and sequentially result in metabolic and endocrine abnormalities, leading to obesity, hyperglycemia, high triglycerides, and insulin resistance, the major role in metabolic syndrome development [38,39,40]. Furthermore, longer sleep duration may also be associated with an increase in levels of systemic inflammatory markers (e.g., C-reactive protein, interleukin-6) [41]. These markers can contribute to blood pressure, waist circumference, and insulin sensitivity and then form metabolic syndrome [42,43,44,45]. In addition, sleep apnea may prolong a nap after lunch, and 50–60% of people with metabolic syndrome also suffer from obstructive sleep apnea syndrome. Sleep apnea can lead to insulin resistance, endothelial dysfunction, and increased arterial rigidity with mechanisms such as sympathetic hyperactivity, inflammation, oxidative stress, and disruption of cortisol secretion [46].
In subgroup analyses of this study, the association was found only in females, participants without mood symptoms, and longer nighttime sleep group (≥8 h), but not in other groups. Males and females have different types and levels of sex hormones, and their bodies respond differently to them. Those may result in gender differences in glucose homeostasis, prediabetic syndromes and progression of diabetes [47]. The discrepancies in two mood symptoms subgroups can share the same reason as those in nighttime sleep duration subgroups. Anxiety and depression are associated with sleep disturbance [48,49], so the night sleep of those with mood symptoms may be shorter and worse than others. This could attenuate the effect of napping in causing metabolic syndrome, though the duration and quality of night sleep were adjusted to some extent in this study.
The present study added to the evidence of association and dose-response relationship between nap duration and prevalence of metabolic syndrome in government employee population. However, there still exist several potential limitations. First, this was a cross-sectional study that could not ascertain the sequence of excessive napping after lunch and metabolic syndrome emerging. Napping could be a sign or manifestation of poor health, which unfortunately was not evaluated in this study. Thus, causality needs to be confirmed in cohort studies. Second, self-reported nap duration after lunch in this study was not as accurate as objective measurement. Moreover, the employed population may not tell the truth about long naps, especially after lunch, which would underestimate the association. Third, although we have adjusted for a large range of covariates in analyses, uninvolved residual confounders such as preclinical disease, sleep apnea, and other sleep disorder could still introduce biases and obscure results. Fourth, we could not ascertain the OR for those with mood symptoms and napping more than 90 min in subgroup analysis, although there appeared to be a negative correlation between napping duration and prevalence of metabolic syndrome. This need to be further determined by larger sample studies. Finally, the study was conducted among government employee adults in China, who were characterized by prolonged sedentary time, lack of physical activity, relatively high prevalence of chronic diseases, and high level of fatigue. This population may be heterogeneous with general employees and other populations. There may also be heterogeneity among the 10 government organizations in this study. Therefore, caution is needed when extrapolating the findings to other populations. The main strengths of this study included the relatively large sample of middle-aged individuals, adjusting for a large number of covariates, and the online questionnaire platform. We were the first to perform subgroup analyses by emotional symptoms and to use RCS analyses to show the dose-response relationship between nap duration after lunch and metabolic syndrome. Moreover, four sensitivity analyses were conducted to verify the value and reliability of the results.
5. Conclusions
In summary, this study demonstrated that napping for more than 90 min per day was associated with an increased prevalence of metabolic syndrome in a Chinese government employee population. In subgroup analyses, the association was found only in females, participants without mood symptoms, and those having longer night sleep duration. People napping less than 45 min seemed to have a lower prevalence of metabolic syndrome. The longitudinal relationship between nap duration and risk of metabolic syndrome needs to be further confirmed in this population.
Supplementary Materials
The following are available online at https://www.mdpi.com/1660-4601/17/12/4268/s1, Figure S1. The association between nap duration and prevalence of metabolic syndrome by three logistic regression models.; Figure S2. The dose-response relationship between nap duration and metabolic syndrome by gender.; Table S1. Characteristics of included participants and excluded participants.; Table S2. Characteristics of participants according to nap duration.; Table S3. Sensitivity analyses of adjustment for more variables, multiple imputation, multilevel model, and propensity score stratifying.
Author Contributions
Conceptualization, J.H. and S.X.; formal analysis, J.H. and F.O.; investigation, J.H., F.O., D.Q., and D.L.; data curation, D.Q. and F.O.; writing—original draft preparation, J.H. and Y.D.; writing—review and editing, all authors; project administration, D.L. All authors read and approved the final manuscript.
Funding
This research was supported by the National Key Research and Development Program of China (grant number: 2016YFC0900802). The sponsor had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Acknowledgments
The authors would like to thank the staff of the Health Management Center of the Third Xiangya Hospital for their work in participants recruitment and the investigators of this study for their efforts in data collection.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| SMS | Short Messaging Service; |
| HDL-C | high-density lipoprotein cholesterol; |
| PHQ-2 | Patient Health Questionnaire-2 |
| GAD-2 | General Anxiety Disorder-2 |
| PSQI | Pittsburgh sleep quality index |
| SD | standard deviation |
| OR | odds ratio |
| CIs | confidence intervals |
| RCS | restricted cubic spline |
| WC | waist circumference |
| TG | triglycerides |
| SBP | systolic blood pressure |
| DBP | diastolic blood pressure |
| FPG | fasting plasma glucose |
| BP | blood pressure |
References
- Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z. The metabolic syndrome. Lancet 2005, 365, 1415–1428. [Google Scholar] [CrossRef]
- Sarafidis, P.A.; Nilsson, P.M. The metabolic syndrome: A glance at its history. J. Hypertens. 2006, 24, 621–626. [Google Scholar] [CrossRef] [PubMed]
- Cameron, A.J.; Shaw, J.E.; Zimmet, P.Z. The metabolic syndrome: Prevalence in worldwide populations. Endocrinol. Metab. Clin. North. Am. 2004, 33, 351–375. [Google Scholar] [CrossRef] [PubMed]
- Galassi, A.; Reynolds, K.; He, J. Metabolic syndrome and risk of cardiovascular disease: A meta-analysis. Am. J. Med. 2006, 119, 812–819. [Google Scholar] [CrossRef] [PubMed]
- Grundy, S.M.; Cleeman, J.I.; Daniels, S.R.; Donato, K.A.; Eckel, R.H.; Franklin, B.A.; Gordon, D.J.; Krauss, R.M.; Savage, P.J.; Smith, S.C., Jr.; et al. Diagnosis and management of the metabolic syndrome: An American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 2005, 112, 2735–2752. [Google Scholar] [CrossRef] [PubMed]
- Grundy, S.M. Metabolic syndrome pandemic. Arter. Thromb. Vasc. Biol. 2008, 28, 629–636. [Google Scholar] [CrossRef] [PubMed]
- Gu, D.; Reynolds, K.; Wu, X.; Chen, J.; Duan, X.; Reynolds, R.F.; Whelton, P.K.; He, J. Prevalence of the metabolic syndrome and overweight among adults in China. Lancet 2005, 365, 1398–1405. [Google Scholar] [CrossRef]
- Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002, 106, 3143–3421. [CrossRef]
- Li, R.; Li, W.; Lun, Z.; Zhang, H.; Sun, Z.; Kanu, J.S.; Qiu, S.; Cheng, Y.; Liu, Y. Prevalence of metabolic syndrome in Mainland China: A meta-analysis of published studies. BMC Public Health 2016, 16, 296. [Google Scholar] [CrossRef]
- Lu, J.; Wang, L.; Li, M.; Xu, Y.; Jiang, Y.; Wang, W.; Li, J.; Mi, S.; Zhang, M.; Li, Y.; et al. Metabolic Syndrome among Adults in China: The 2010 China Noncommunicable Disease Surveillance. J. Clin. Endocrinol. Metab. 2017, 102, 507–515. [Google Scholar] [CrossRef]
- Li, Y.; Zhao, L.; Yu, D.; Wang, Z.; Ding, G. Metabolic syndrome prevalence and its risk factors among adults in China: A nationally representative cross-sectional study. PLoS ONE 2018, 13, e0199293. [Google Scholar] [CrossRef]
- Lucassen, E.A. To nap or not to nap: Is the Wujiao a healthy habit? Sleep Med. 2013, 14, 929–930. [Google Scholar] [CrossRef]
- Lovato, N.; Lack, L. The Effects of Napping on Cognitive Functioning. Prog Brain Res 2010, 185, 155–166. [Google Scholar] [CrossRef]
- Mantua, J.; Spencer, R.M.C. Exploring the nap paradox: Are mid-day sleep bouts a friend or foe? Sleep Med. 2017, 37, 88–97. [Google Scholar] [CrossRef] [PubMed]
- Blanchfield, A.W.; Lewis-Jones, T.M.; Wignall, J.R.; Roberts, J.B.; Oliver, S.J. The influence of an afternoon nap on the endurance performance of trained runners. Eur. J. Sport Sci. 2018, 18, 1177–1184. [Google Scholar] [CrossRef] [PubMed]
- Stone, K.L.; Ewing, S.K.; Ancoli-Israel, S.; Ensrud, K.E.; Redline, S.; Bauer, D.C.; Cauley, J.A.; Hillier, T.A.; Cummings, S.R. Self-reported sleep and nap habits and risk of mortality in a large cohort of older women. J. Am. Geriatr. Soc. 2009, 57, 604–611. [Google Scholar] [CrossRef]
- Chen, G.C.; Liu, M.M.; Chen, L.H.; Xu, J.Y.; Hidayat, K.; Li, F.R.; Qin, L.Q. Daytime napping and risk of type 2 diabetes: A meta-analysis of prospective studies. Sleep Breath 2018, 22, 815–824. [Google Scholar] [CrossRef]
- Cao, Z.; Shen, L.; Wu, J.; Yang, H.; Fang, W.; Chen, W.; Yuan, J.; Wang, Y.; Liang, Y.; Wu, T. The effects of midday nap duration on the risk of hypertension in a middle-aged and older Chinese population: A preliminary evidence from the Tongji-Dongfeng Cohort Study, China. J. Hypertens. 2014, 32, 1993–1998, discussion 1998. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.; Tang, K.; Chen, F.; Wei, S.; Lin, F.; Yao, J.; Chen, L.; Huang, H.; Liang, J.; Li, L.; et al. Afternoon nap and nighttime sleep with risk of micro- and macrovascular disease in middle-aged and elderly population. Int. J. Cardiol. 2015, 187, 553–555. [Google Scholar] [CrossRef]
- Chen, G.; Chen, L.; Wen, J.; Yao, J.; Li, L.; Lin, L.; Tang, K.; Huang, H.; Liang, J.; Lin, W.; et al. Associations between sleep duration, daytime nap duration, and osteoporosis vary by sex, menopause, and sleep quality. J. Clin. Endocrinol. Metab. 2014, 99, 2869–2877. [Google Scholar] [CrossRef]
- Lin, M.; Su, Q.; Wen, J.; Wei, S.; Yao, J.; Huang, H.; Liang, J.; Li, L.; Lin, W.; Lin, L.; et al. Self-reported sleep duration and daytime napping are associated with renal hyperfiltration in general population. Sleep Breath 2018, 22, 223–232. [Google Scholar] [CrossRef] [PubMed]
- Lin, D.; Sun, K.; Li, F.; Qi, Y.; Ren, M.; Huang, C.; Tang, J.; Xue, S.; Li, Y.; Yan, L. Association between habitual daytime napping and metabolic syndrome: A population-based study. Metabolism 2014, 63, 1520–1527. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Xu, G.; Shen, L.; Zhang, Y.; Song, L.; Yang, S.; Yang, H.; Liang, Y.; Wu, T.; Wang, Y. Daily sleep duration and risk of metabolic syndrome among middle-aged and older Chinese adults: Cross-sectional evidence from the Dongfeng-Tongji cohort study. BMC Public Health 2015, 15, 178. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Xu, Z.; He, M.; Yang, H.; Li, X.; Min, X.; Zhang, C.; Xu, C.; Angileri, F.; Légaré, S.; et al. Sleep Duration and Midday Napping with 5-Year Incidence and Reversion of Metabolic Syndrome in Middle-Aged and Older Chinese. Sleep 2016, 39, 1911–1918. [Google Scholar] [CrossRef] [PubMed]
- Van der Pal, K.C.; Koopman, A.D.M.; Lakerveld, J.; van der Heijden, A.A.; Elders, P.J.; Beulens, J.W.; Rutters, F. The association between multiple sleep-related characteristics and the metabolic syndrome in the general population: The New Hoorn study. Sleep Med. 2018, 52, 51–57. [Google Scholar] [CrossRef]
- Yamada, T.; Shojima, N.; Yamauchi, T.; Kadowaki, T. J-curve relation between daytime nap duration and type 2 diabetes or metabolic syndrome: A dose-response meta-analysis. Sci. Rep. 2016, 6, 38075. [Google Scholar] [CrossRef]
- Sun, L.; Jiang, X.; Zhao, X.; Zhang, Y.; Xu, Y.; Shang, L. Physical activity level and associated factors among civil servants in Xi’an, China. J. Sci. Med. Sport 2016, 19, 647–653. [Google Scholar] [CrossRef]
- Lallukka, T.; Lahelma, E.; Rahkonen, O.; Roos, E.; Laaksonen, E.; Martikainen, P.; Head, J.; Brunner, E.; Mosdol, A.; Marmot, M.; et al. Associations of job strain and working overtime with adverse health behaviors and obesity: Evidence from the Whitehall II Study, Helsinki Health Study, and the Japanese Civil Servants Study. Soc. Sci. Med. 2008, 66, 1681–1698. [Google Scholar] [CrossRef]
- Alberti, K.G.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.C.; James, W.P.; Loria, C.M.; Smith, S.C., Jr.; et al. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009, 120, 1640–1645. [Google Scholar] [CrossRef]
- Zhou, B.F. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults--study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed. Environ. Sci. Bes 2002, 15, 83–96. [Google Scholar]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The Patient Health Questionnaire-2: Validity of a two-item depression screener. Med. Care 2003, 41, 1284–1292. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.; Monahan, P.O.; Löwe, B. Anxiety disorders in primary care: Prevalence, impairment, comorbidity, and detection. Ann. Intern. Med. 2007, 146, 317–325. [Google Scholar] [CrossRef] [PubMed]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Desquilbet, L.; Mariotti, F. Dose-response analyses using restricted cubic spline functions in public health research. Stat. Med. 2010, 29, 1037–1057. [Google Scholar] [CrossRef]
- Groenwold, R.H.; Donders, A.R.; Roes, K.C.; Harrell, F.E., Jr.; Moons, K.G. Dealing with missing outcome data in randomized trials and observational studies. Am. J. Epidemiol. 2012, 175, 210–217. [Google Scholar] [CrossRef] [PubMed]
- Yamada, T.; Hara, K.; Shojima, N.; Yamauchi, T.; Kadowaki, T. Daytime Napping and the Risk of Cardiovascular Disease and All-Cause Mortality: A Prospective Study and Dose-Response Meta-Analysis. Sleep 2015, 38, 1945–1953. [Google Scholar] [CrossRef] [PubMed]
- Guo, V.Y.; Cao, B.; Wong, C.K.H.; Yu, E.Y.T. The association between daytime napping and risk of diabetes: A systematic review and meta-analysis of observational studies. Sleep Med. 2017, 37, 105–112. [Google Scholar] [CrossRef]
- Shi, S.Q.; Ansari, T.S.; McGuinness, O.P.; Wasserman, D.H.; Johnson, C.H. Circadian disruption leads to insulin resistance and obesity. Curr. Biol. 2013, 23, 372–381. [Google Scholar] [CrossRef]
- Gamble, K.L.; Berry, R.; Frank, S.J.; Young, M.E. Circadian clock control of endocrine factors. Nat. Rev. Endocrinol. 2014, 10, 466–475. [Google Scholar] [CrossRef]
- Poggiogalle, E.; Jamshed, H.; Peterson, C.M. Circadian regulation of glucose, lipid, and energy metabolism in humans. Metabolism 2018, 84, 11–27. [Google Scholar] [CrossRef]
- Irwin, M.R.; Olmstead, R.; Carroll, J.E. Sleep Disturbance, Sleep Duration, and Inflammation: A Systematic Review and Meta-Analysis of Cohort Studies and Experimental Sleep Deprivation. Biol. Psychiatry 2016, 80, 40–52. [Google Scholar] [CrossRef] [PubMed]
- Sesso, H.D.; Buring, J.E.; Rifai, N.; Blake, G.J.; Gaziano, J.M.; Ridker, P.M. C-reactive protein and the risk of developing hypertension. JAMA 2003, 290, 2945–2951. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.; Joseph, L.; Pilote, L. Obesity and C-reactive protein in various populations: A systematic review and meta-analysis. Obes. Rev. Off. J. Int. Assoc. Study Obes. 2013, 14, 232–244. [Google Scholar] [CrossRef]
- Lorenzo, C.; Festa, A.; Hanley, A.J.; Rewers, M.J.; Escalante, A.; Haffner, S.M. Novel Protein Glycan-Derived Markers of Systemic Inflammation and C-Reactive Protein in Relation to Glycemia, Insulin Resistance, and Insulin Secretion. Diabetes Care 2017, 40, 375–382. [Google Scholar] [CrossRef] [PubMed]
- Cornier, M.A.; Dabelea, D.; Hernandez, T.L.; Lindstrom, R.C.; Steig, A.J.; Stob, N.R.; Van Pelt, R.E.; Wang, H.; Eckel, R.H. The metabolic syndrome. Endocr. Rev. 2008, 29, 777–822. [Google Scholar] [CrossRef] [PubMed]
- Borel, A.L. Sleep Apnea and Sleep Habits: Relationships with Metabolic Syndrome. Nutrients 2019, 11, 2628. [Google Scholar] [CrossRef]
- Mauvais-Jarvis, F. Gender differences in glucose homeostasis and diabetes. Physiol. Behav. 2018, 187, 20–23. [Google Scholar] [CrossRef]
- Ford, D.E.; Kamerow, D.B. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA 1989, 262, 1479–1484. [Google Scholar] [CrossRef]
- Breslau, N.; Roth, T.; Rosenthal, L.; Andreski, P. Sleep disturbance and psychiatric disorders: A longitudinal epidemiological study of young adults. Biol. Psychiatry 1996, 39, 411–418. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).