Structural Quality of Services and Use of Family Planning Services in Primary Health Care Facilities in Ethiopia. How Do Public and Private Facilities Compare?
Abstract
1. Background
2. Methods
2.1. Design and Setting
2.2. Data Sources and Sample
2.3. Variables
2.4. Data Analysis
2.5. Ethical Consideration
3. Results
3.1. Description of Facility’s Location, Structure, and Provisions of Reproductive and Child Health Services in PHCU Facilities
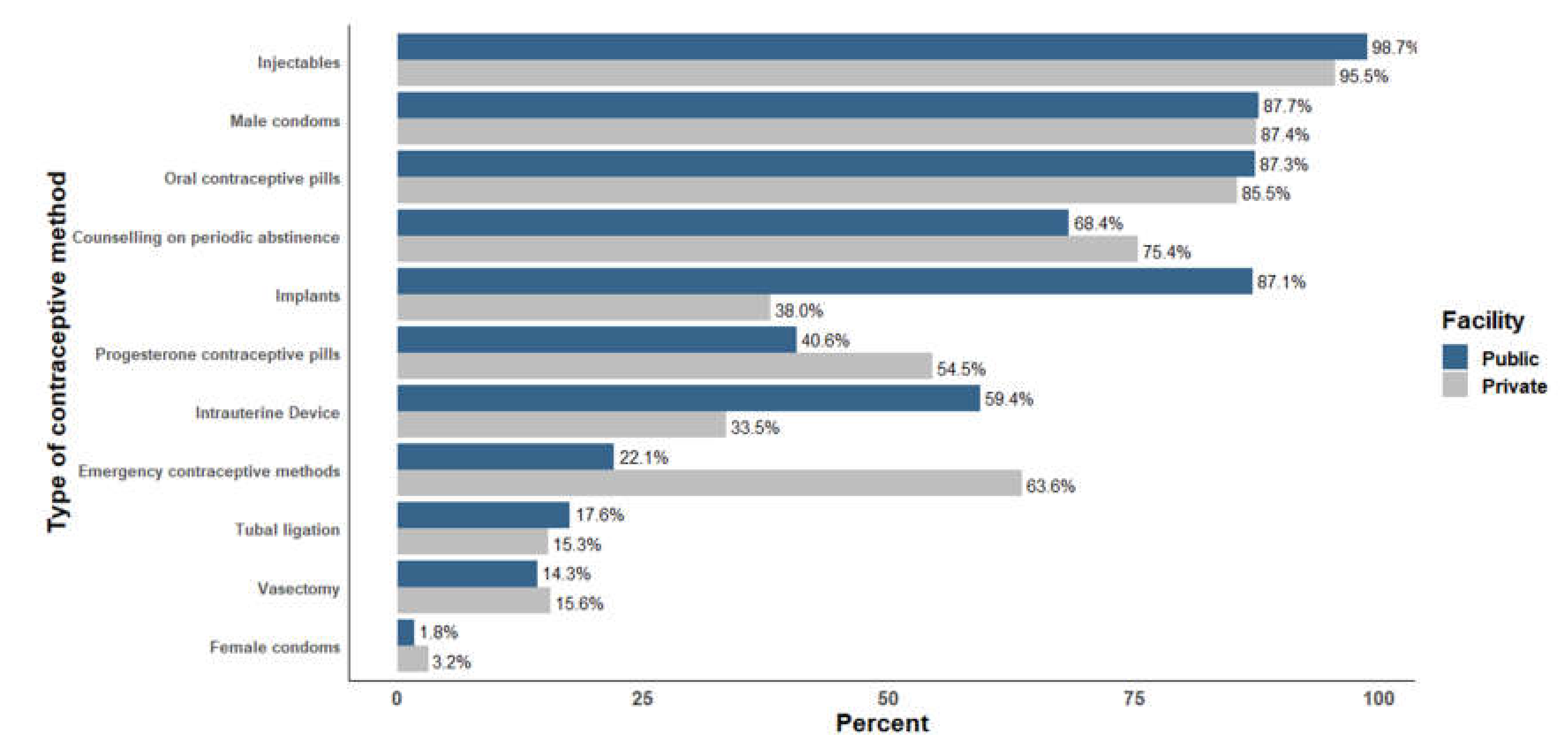
3.2. Structural Quality of FP Services in Public and Private PHCU Facilities
3.3. Association of Women’s Characteristics with Facility Type Where They Accessed FP Services
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ahmed, S.; Li, Q.; Liu, L.; Tsui, A.O. Maternal deaths averted by contraceptive use: An analysis of 172 countries. Lancet 2012, 380, 111–125. [Google Scholar] [CrossRef]
- Allen, H.A. The Role of Family Planning in Poverty Reduction. Obs. Gynecol. 2007, 110, 999–1002. [Google Scholar] [CrossRef] [PubMed]
- Amaral, G.; Foster, D.G.; Biggs, M.A.; Jasik, C.B.; Judd, S.; Brindis, C.D. Public Savings from the Prevention of Unintended Pregnancy: A Cost Analysis of Family Planning Services in California. Health Serv. Res. 2007, 42, 1960–1980. [Google Scholar] [CrossRef] [PubMed]
- Ethiopian Public Health Institute (EPHI) [Ethiopia]; ICF. Ethiopia Mini Demographic and Health Survey 2019: Key Indicators; EPHI: Addis Ababa, Ethiopia; ICF International: Rockville, MD, USA, 2019. [Google Scholar]
- Central Statistical Authority (CSA) [Ethiopia] and ORC Macro. Ethiopia Demographic and Health Survey 2000; CSA: Addis Ababa, Ethiopia; ORC Macro: Calverton, MD, USA, 2001. [Google Scholar]
- Central Statistical Authority (CSA) [Ethiopia] and ICF International. Ethiopian Demographic and Health Survey report 2011; CSA: Addis Ababa, Ethiopia; ICF International: Calverton, MD, USA, 2012. [Google Scholar]
- Central Statistical Authority (CSA) [Ethiopia] and ICF International. Ethiopia Demographic and Health Survey 2016; CSA: Addis Ababa, Ethiopia; ICF International: Rockville, MD, USA, 2016. [Google Scholar]
- Ali, M.M. Quality of care and contraceptive pill discontinuation in rural Egypt. J. Biosoc. Sci. 2001, 33, 161–172. [Google Scholar] [CrossRef] [PubMed]
- Blanc, A.; Curtis, S.; Croft, T. Monitoring contraceptive continuation: Links to fertility outcomes and quality of care. Stud. Fam. Plann. 2002, 33, 127–140. [Google Scholar] [CrossRef]
- RamaRao, S.; Mohanam, R. The quality of family planning programs: Concepts, measurements, interventions, and effects. Stud. Fam. Plann. 2003, 34, 227–248. [Google Scholar] [CrossRef]
- Jain, A.K. Fertility Reduction and the Quality of Family Planning Services. Stud. Fam. Plann. 1989, 20, 1–16. [Google Scholar] [CrossRef]
- Veney, J.; Magnani, R.; Gorbach, P. Measurement of the quality of family planning services. Popul. Res. Policy Rev. 1993, 12, 243–259. [Google Scholar] [CrossRef]
- Federal Ministry of Health (FMOH). National Guideline for Family Planning Services in Ethiopia; FMOH: Addis Ababa, Ethiopia, 2011. [Google Scholar]
- Federal Ministry of Health (FMOH). Ethiopia Health Sector Transformation Plan HSTP (2015/16 up to 2019/20); FMOH: Addis Ababa, Ethiopia, 2015. [Google Scholar]
- Federal Ministry of Health (FMOH). Costed Implementation Plan for Family Planning in Ethiopia, 2015/16–2020; FMOH: Addis Ababa, Ethiopia, 2016. [Google Scholar]
- Federal Ministry of Health (FMOH). National Reproductive Health Strategy (2016-2020); FMOH: Addis Ababa, Ethiopia, 2016. [Google Scholar]
- Federal Ministry of Health (FMOH); Harvard T.H. Chan School of Public Health; JSI Research & Training Institute. Strengthening Public Private Partnerships for More and Better Health Outcomes in Ethiopia: Expert Reviews and Case Studies; FMOH [Ethiopia]: Addis Ababa, Ethiopia; Harvard T.H. Chan School of Public Health, JSI Research & Training Institute, Inc.: Boston, MA, USA, 2015. [Google Scholar]
- Federal Ministry of Health (FMOH). Ethiopian National Health Care Quality Strategy (2016-2020): Transforming the Quality of Health Care in Ethiopia; FMOH: Addis Ababa, Ethiopia, 2016. [Google Scholar]
- Kruk, M.E.; Gage, A.D.; Arsenault, C.; Jordan, K.; Leslie, H.H.; Roder-DeWan, S.; English, M. High-quality health systems in the Sustainable Development Goals era: Time for a revolution. Lancet Glob. Health 2018, 6, e1196–e1252. [Google Scholar] [CrossRef]
- Bruce, J. Fundamental Elements of the Quality of Care: A Simple Framework. Stud. Fam. Plann. 1990, 21, 61–91. [Google Scholar] [CrossRef]
- Donabedian, A. The quality of care: How can it be assessed? JAMA 1988, 260, 1743–1748. [Google Scholar] [CrossRef] [PubMed]
- Donabedian, A. The Definition of Quality and Approaches to Its Assessment; Health Administration Press: Ann Arbor, MI, USA, 1980. [Google Scholar]
- Tessema, G.A.; Mahmood, M.A.; Gomersall, J.S.; Assefa, Y.; Zemedu, T.G.; Kifle, M. Laurence CO: Client and facility level determinants of quality of care in family planning services in Ethiopia: Multilevel modelling. PLoS ONE 2017, 12, e0179167. [Google Scholar] [CrossRef] [PubMed]
- Guo, S.; Carvajal-Aguirre, L.; Victora, C.G.; Barros, A.J.; Wehrmeister, F.C.; Vidaletti, L.P.; Rutter, P. Equitable coverage? The roles of the private and public sectors in providing maternal, newborn and child health interventions in South Asia. BMJ Glob. Health 2019, 4, e001495. [Google Scholar] [CrossRef] [PubMed]
- Agha, S.; Do, M. The quality of family planning services and client satisfaction in the public and private sectors in Kenya. Int. J. Qual. Health Care 2009, 21, 87–96. [Google Scholar] [CrossRef]
- Javed, W.; Jabbar, A.; Mehboob, N.; Tafseer, M.; Memon, Z. Client Satisfaction: Does Private or Public Health Sector Make a Difference? Results from Secondary Data Analysis in Sindh, Pakistan. Int J Innov Res Sci Eng Technol 2015, 9, 1483–1488. [Google Scholar]
- Mpunga, D.; Lumbayi, J.; Dikamba, N.; Mwembo, A.; Ali Mapatano, M.; Wembodinga, G. Availability and Quality of Family Planning Services in the Democratic Republic of the Congo: High Potential for Improvement. Glob. Health Sci. Pract. 2017, 5, 274–285. [Google Scholar] [CrossRef]
- Barber, S.L.; Gertler, P.J.; Harimurti, P. Differences in access to high-quality outpatient care in Indonesia. Health Aff. (Millwood) 2007, 26 (Suppl. 2), w352–w366. [Google Scholar] [CrossRef]
- Peabody, J.W.; Rahman, O.; Fox, K.; Gertler, P. Quality of care in public and private primary health care facilities: Structural comparisons in Jamaica. Bull. Pan Am. Health Organ. 1994, 28, 122–141. [Google Scholar]
- Population Reference Bureau. 2018 World Population Data Sheet with a Special Focus on Changing Age Structures. Available online: https://www.prb.org/wp-content/uploads/2018/08/2018_WPDS.pdf (accessed on 18 February 2018).
- Ethiopian Public Health Institute (EPHI); Federal Ministry of Health (FMOH); ICF International. Ethiopia Service Provision Assessment Plus(ESPA+) Survey 2014; EPHI; FMOH: Addis Ababa, Ethiopia; ICF International: Rockville, MD, USA, 2014. [Google Scholar]
- The DHS Data Collection. Available online: http://dhsprogram.com/data/data-collection.cfm (accessed on 15 January 2018).
- Agha, S.; Keating, J. Determinants of the Choice of a Private Health Facility for Family Planning Services Among the Poor: Evidence From Three Countries; U.S. Agency for International Development (USAID): Bethesda, MD, USA, 2009.
- Nair, V.; Morankar, S.; Jira, C.; Tushune, K. Private Hospital Sector Development: An Exploratory Study on Providers Perspective in Addis Ababa, Ethiopia. Ethiop. J. Health Sci. 2011, 21 (Suppl. 1), 59–64. [Google Scholar]
- Thomas, M.; Dejene, M.; Kebede, F.; Stover, C. Private Health Sector Program Mid-Term Evaluation; U.S. Agency for International Development (USAID): Washington, DC, USA, 2012.
- Morgan, G.; Keesbury, J.; Speizer, I. Emergency Contraceptive Knowledge and Use among Urban Women in Nigeria and Kenya. Stud. Fam. Plann. 2014, 45, 59–72. [Google Scholar] [CrossRef]
- Campbell, O.M.; Benova, L.; Macleod, D.; Goodman, C.; Footman, K.; Pereira, A.L.; Lynch, C.A. Who, What, Where: An analysis of private sector family planning provision in 57 low- and middle-income countries. Trop. Med. Int. Health 2015, 20, 1639–1656. [Google Scholar] [CrossRef]
| Variables | OR 1 (95% CI) | |
|---|---|---|
| COR 1 (95% CI) | AOR (95% CI) 1,2 | |
| Availability of contraceptive methods | ||
| Availability of progesterone contraceptive pills | 1.73 (1.15, 2.60) * | 1.31 (0.83, 2.09) |
| Availability of IUD | 0.35 (0.22, 0.54) * | 0.22 (0.13, 0.38) * |
| Availability of implants | 0.10 (0.06, 0.16) * | 0.06 (0.03, 0.12) * |
| Availability of emergency contraceptive methods | 6.17 (3.98, 9.59) * | 3.81 (2.37, 6.10) * |
| Services provision environment | ||
| Health provider availability of twenty-four hours/seven days | 0.68 (0.42, 1.11) * | 0.35 (0.18, 0.69) * |
| Trained provider availability | 0.28 (0.19, 0.43) * | 0.23 (0.14,0.41) * |
| Quality assurance system | 0.10 (0.79, 1.79) * | 0.07 (0.02, 0.21) * |
| FP guidelines/protocols | 0.43 (0.04, 0.28) * | 0.33 (0.19, 0.54) * |
| Client chart/record to document the client’s clinical data | 0.23 (0.16, 0.37) * | 0.22 (0.13, 0.36) * |
| Supervision in the past six months | 0.75 (0.50, 1.15) * | 0.91 (0.57, 1.47) |
| Private room for providing counselling services | 1.16 (0.89, 3.18) * | 0.88 (0.46, 1.70) |
| Facility’s basic infrastructure | ||
| Availability of functional landline telephone | 3.43 (2.08, 5.69) * | 0.64 (0.30, 1.37) |
| Availability of functional cell phone | 9.18 (5.56, 15.15) * | 8.20 (4.95, 13.59) * |
| Access to email at least two hours on a day | 6.22 (2.68, 14.48) * | 2.01 (0.78, 5.50) |
| Availability of functional computer | 1.20 (0.75, 1.92) | 0.18 (0.07, 1.44) |
| Access to water supply | 5.25 (2.89, 9.57) * | 3.37 (1.72, 6.59) * |
| Availability electricity supply/generator | 1.52 (1.02, 2.26) * | 1.11 (0.69, 1.76) |
| FP services equipment | ||
| Availability of stethoscope | 9.17 (4.28, 19.61) * | 7.88 (3.49, 17.73) * |
| Availability of examination light | 8.1 (5.04, 13.07) * | 8.19 (4.86, 13.79) * |
| Availability of exam couch | 19.01 (8.27, 43.72) * | 14.11 (5.84, 34.08) * |
| Availability of sample FP methods | 1.44 (0.95, 2.17) | 0.87 (0.55, 1.37) |
| Pelvic model for demonstrating IUD use demonstration | 0.56 (0.31, 1.01) * | 0.39 (0.21, 0.76) * |
| Model for demonstrating condom use | 1.03 (0.61, 1.71) * | 0.40 (0.21, 0.76) * |
| Availability of additional maternal and child health services | ||
| Antenatal care services | 0.06 (0.03,0.13) * | 0.05 (0.02, 0.10) * |
| Normal delivery services | 0.28 (0.18,0.43) * | 0.15 (0.08, 0.30) * |
| Under-five health services | 0.18 (0.06, 0.56) * | 0.15 (0.05, 0.45) * |
| Services for the prevention of mother-to-child transmission of HIV | 0.48 (0.30, 0.77) * | 0.15 (0.08, 0.32) * |
| Diagnosis and treat for STI | 13.5 (7.70, 23.8) * | 8.51 (4.64, 15.61) * |
| Women Characteristics | Private (n = 586) | Public (n = 3110) |
|---|---|---|
| Frequency (%) | Frequency (%) | |
| Age in Years | ||
| 15–24 | 200 (34.1) | 737 (23.7) |
| 25–34 | 278 (47.5) | 1467 (47.2) |
| 35+ | 108 (18.4) | 906 (29.1) |
| Marital Status | ||
| Currently married/in union | 58 (9.9) | 222 (7.1) |
| Not currently married | 528 (90.1) | 2888 (92.9) |
| Place of Residence | ||
| Urban | 291 (49.4) | 561 (18.0) |
| Rural | 297 (50.6) | 2549 (82.0) |
| Religion | ||
| Orthodox | 336 (57.4) | 1603 (51.6) |
| Muslim | 134 (22.9) | 629 (20.2) |
| Protestant | 109 (18.6) | 833 (26.8) |
| Other/missing | 7 (1.1) | 45 (1.4) |
| Highest Educational Status | ||
| None | 196 (33.4) | 1773 (57.0) |
| Primary | 213 (36.5) | 969 (31.1) |
| Secondary+ | 177 (30.1) | 368 (11.8) |
| Partner’s Educational Status( n = 3416) $ | ||
| None | 125 (23.6) | 1237 (42.8) |
| Primary | 216 (41.0) | 1161 (40.2) |
| Secondary+ | 187 (35.4) | 490 (7.0) |
| Working/Occupational Status | ||
| Not working | 206 (35.1) | 1445 (46.5) |
| Working/employed * | 380 (64.9) | 1664 (53.5) |
| Wealth Index | ||
| Poor | 85 (14.6) | 990 (31.8) |
| Middle | 89 (15.1) | 679 (21.8) |
| Rich | 412 (70.3) | 1440 (46.3) |
| Number of Living Children | ||
| 0 | 142 (24.1) | 241 (7.8) |
| 1–2 | 231 (39.4) | 1120 (36.0) |
| 3–4 | 142 (24.1) | 906 (29.1) |
| 5+ | 72 (12.3) | 842 (27.1) |
| Exposure to FP Media | ||
| No | 293 (50.0) | 2174 (69.9) |
| Yes | 293 (50.0) | 936 (30.1) |
| Decision Making Power in the Household | ||
| No | 176 (30.2) | 1021 (32.8) |
| Yes | 410 (69.8) | 2089 (67.2) |
| Women Characteristics | OR1 (95% CI) | |
|---|---|---|
| COR 1 (95% CI) | AOR 1 (95% CI) | |
| Age in Years | ||
| 15–24 | 1 | 1 |
| 25–34 | 0.69 (0.51, 0.96) ** | 1.02 (0.65, 1.64) |
| 35+ | 0.44 (0.29,0.56) *** | 1.07 (0.56, 2.06) |
| Place of Residence | ||
| Urban | 4.44 (3.05, 6.46) *** | 3.91 (1.71, 4.95) *** |
| Rural | 1 | 1 |
| Religion | ||
| Orthodox | 1 | 1 |
| Muslim | 1.02 (0.67, 1.53) | 1.63 (1.07, 2.48) * |
| Protestant | 0.62 (0.41, 0.96) * | 0.93 (0.56, 1.53) |
| Other/missing | 0.70 (0.16, 3.02) | 1.24 (0.25, 6.28) |
| Highest Educational Status | ||
| None | 1 | 1 |
| Primary | 1.99 (1.41, 2.83) *** | 1.8 (0.71, 1.65) |
| Secondary+ | 4.34 (2.97, 6.33) *** | 0.91 (0.52, 1.60) |
| Partner’s Educational Status (n = 3416) $ | ||
| None | 1 | 1 |
| Primary | 1.85 (1.26, 2.72) ** | 1.49 (0.99, 2.23) |
| Secondary+ | 3.79 (2.44, 5.87) *** | 1.64 (1.01, 2.70) * |
| Working/Occupational Status | ||
| Not working | 1 | 1 |
| Working $ | 1.60 (1.18, 2.17) ** | 1.35 (1.01, 1.96) * |
| Wealth Index | ||
| Poor | 1 | 1 |
| Middle | 1.51 (0.97, 2.37) *** | 1.54 (0.96, 2.47) |
| Rich | 3.31 (2.21, 4.96) *** | 1.51 (0.90, 2.54) |
| Number of Living Children | ||
| 0 | 1 | 1 |
| 1–2 | 0.35 (0.22, 0.55) *** | 0.27 (0.15, 0.47) ** |
| 3–4 | 0.27 (0.17, 0.42) *** | 0.23 (0.11, 0.46) ** |
| 5+ | 0.14 (0.08, 0.26) *** | 0.18 (0.08, 0.41) ** |
| Exposure to FP Media | ||
| No | 1 | 1 |
| Yes | 2.33 (1.70, 3.19) *** | 0.97 (0.66, 1.44) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tessema, G.A.; Mahmood, M.A.; Gomersall, J.S.; Assefa, Y.; Zemedu, T.G.; Kifle, M.; Laurence, C.O. Structural Quality of Services and Use of Family Planning Services in Primary Health Care Facilities in Ethiopia. How Do Public and Private Facilities Compare? Int. J. Environ. Res. Public Health 2020, 17, 4201. https://doi.org/10.3390/ijerph17124201
Tessema GA, Mahmood MA, Gomersall JS, Assefa Y, Zemedu TG, Kifle M, Laurence CO. Structural Quality of Services and Use of Family Planning Services in Primary Health Care Facilities in Ethiopia. How Do Public and Private Facilities Compare? International Journal of Environmental Research and Public Health. 2020; 17(12):4201. https://doi.org/10.3390/ijerph17124201
Chicago/Turabian StyleTessema, Gizachew Assefa, Mohammad Afzal Mahmood, Judith Streak Gomersall, Yibeltal Assefa, Theodros Getachew Zemedu, Mengistu Kifle, and Caroline O. Laurence. 2020. "Structural Quality of Services and Use of Family Planning Services in Primary Health Care Facilities in Ethiopia. How Do Public and Private Facilities Compare?" International Journal of Environmental Research and Public Health 17, no. 12: 4201. https://doi.org/10.3390/ijerph17124201
APA StyleTessema, G. A., Mahmood, M. A., Gomersall, J. S., Assefa, Y., Zemedu, T. G., Kifle, M., & Laurence, C. O. (2020). Structural Quality of Services and Use of Family Planning Services in Primary Health Care Facilities in Ethiopia. How Do Public and Private Facilities Compare? International Journal of Environmental Research and Public Health, 17(12), 4201. https://doi.org/10.3390/ijerph17124201





