Effect of Neuromuscular Electrical Stimulation on Masseter Muscle Thickness and Maximal Bite Force among Healthy Community-Dwelling Persons Aged 65 Years and Older: A Randomized, Double Blind, Placebo-Controlled Study
Abstract
1. Introduction
2. Materials and Methods
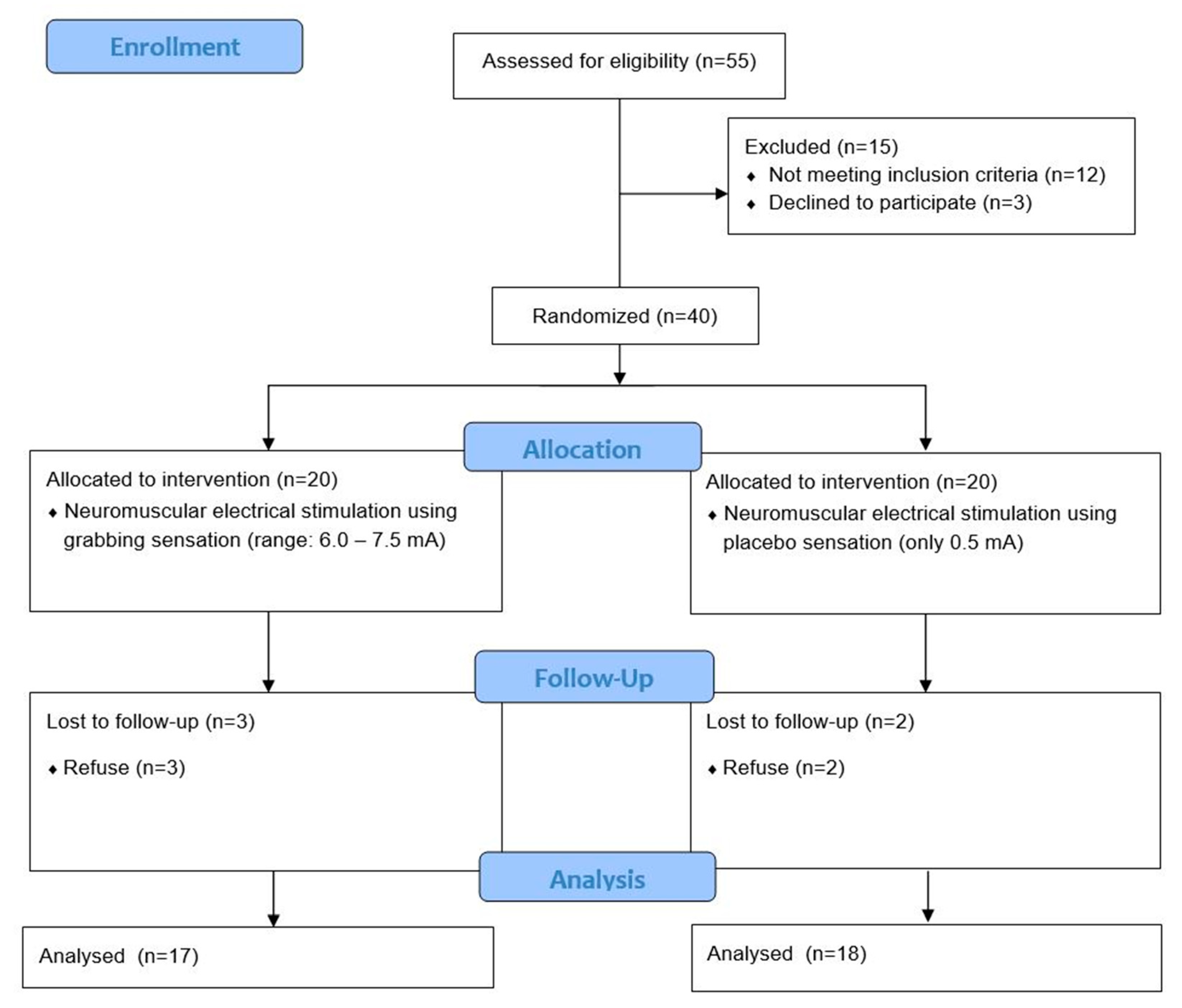
2.1. Study Design and Participants
2.2. Ethical Considerations
2.3. Intervention
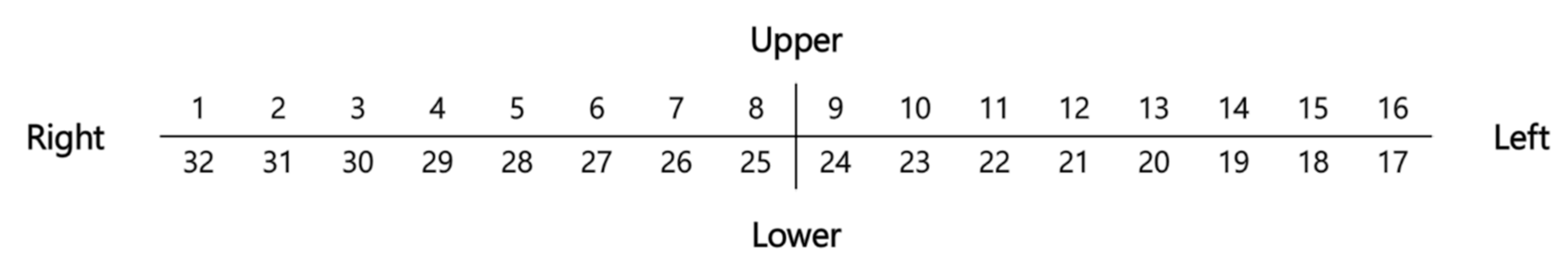
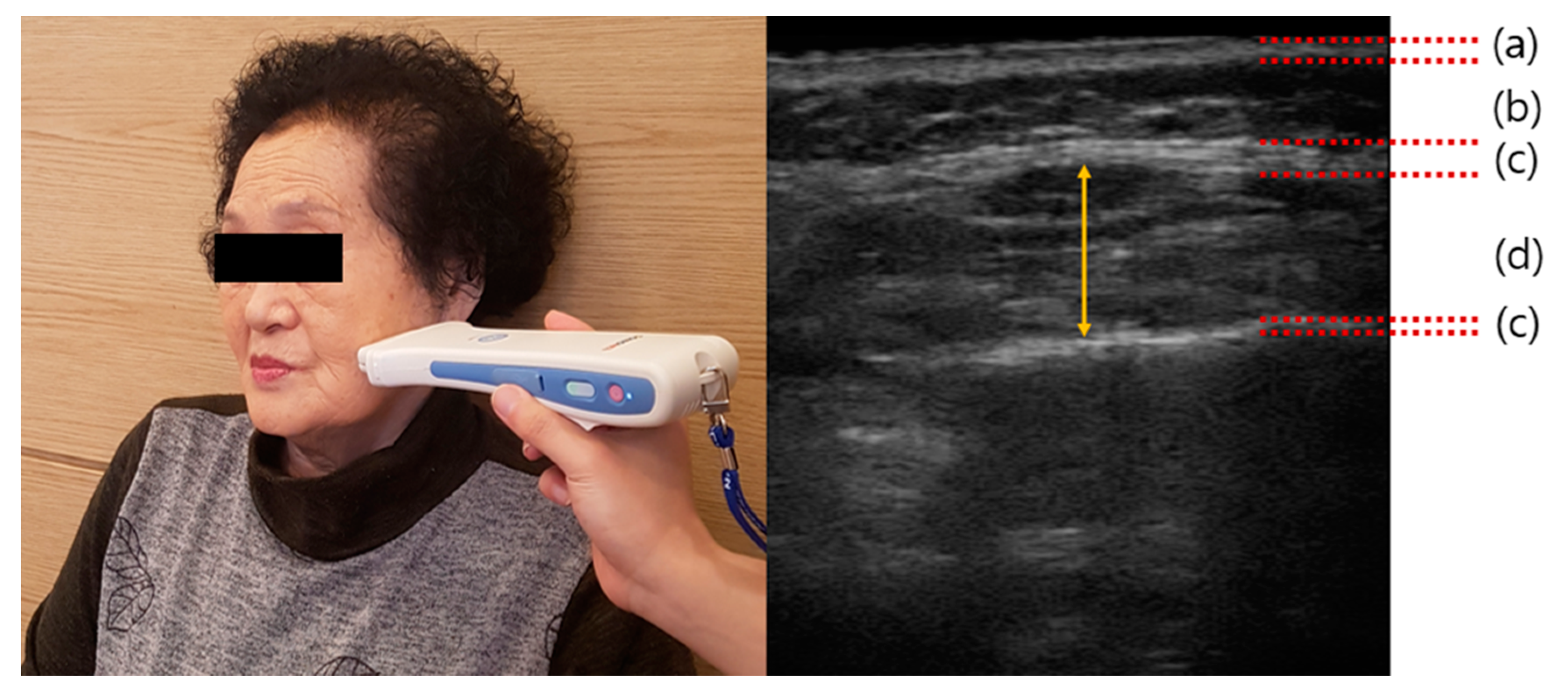
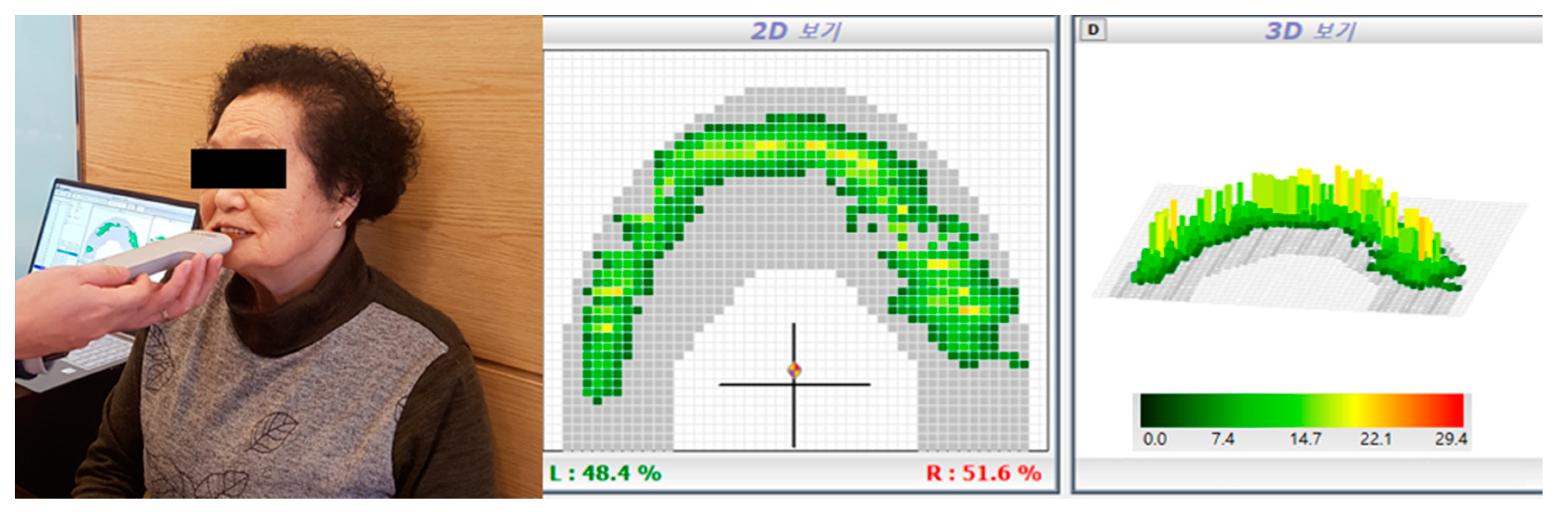
2.4. Outcome Measurement
2.5. Statistical Analysis
3. Results
3.1. General Characteristics of the Participants
3.2. Effect of Masseter Muscle Thickness
3.3. Effect of Maximal Bite Force
3.4. Reported Side Effects
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Ide, Y. Structural characterictics of the swallowing organ. Jpn. J. Rehabil. Med. 2010, 47, 683–690. [Google Scholar]
- Fukamizu, K.; Kodama, M.; Moriya, Y.; Yokoyama, M.; Murata, Y. The biting forces and the electromyographic analyses of the temporalis and masseter muscles in the dentulous mandibular positions. Nihon. Hotetsu. Shika. Gakkai. Zasshi. 1972, 16, 46–53. [Google Scholar] [CrossRef][Green Version]
- Hiraoka, K. Changes in masseter muscle activity associated with swallowing. J. Oral Rehabil. 2004, 31, 963–967. [Google Scholar] [CrossRef] [PubMed]
- Mishellany, A.; Woda, A.; Labas, R.; Peyron, M.A. The challenge of mastication: Preparing a bolus suitable for deglutition. Dysphagia 2006, 21, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Matsuo, K.; Kito, N.; Ogawa, K.; Izumi, A.; Masuda, Y. Effects of textured foods on masticatory muscle activity in older adults with oral hypofunction. J. Oral Rehabil. 2020, 47, 180–186. [Google Scholar] [CrossRef]
- Kang, H.K.; Kim, Y.R. Association between Dental Treatment, Quality of Life, and Activity Limitation According to Masticatory Discomfort: Evidence from the Korean National Health and Nutrition Examination Survey (2013–2015). Int. J. Environ. Res. Public Health 2020, 17, 547. [Google Scholar] [CrossRef]
- Ikebe, K.; Matsuda, K.; Kagawa, R.; Enoki, K.; Yoshida, M.; Maeda, Y.; Nokubi, T. Association of masticatory performance with age, gender, number of teeth, occlusal force and salivary flow in Japanese older adults: Is ageing a risk factor for masticatory dysfunction? Arch. Oral Biol. 2011, 56, 991–996. [Google Scholar] [CrossRef]
- Iyota, K.; Mizutani, S.; Oku, S.; Asao, M.; Futatsuki, T.; Inoue, R.; Imai, Y.; Kashiwazaki, H. A Cross-Sectional Study of Age-Related Changes in Oral Function in Healthy Japanese Individuals. Int. J. Environ. Res. Public Health 2020, 17, 1376. [Google Scholar] [CrossRef]
- Korea Institute for Health and Social Affairs. Report on the Korean National Older Adults Life Survey 2014; Ministry of Health Welfare: Seoul, Korea, 2015.
- Smith, L.; Tully, M.; Jacob, L.; Blackburn, N.; Adlakha, D.; Caserotti, P.; Soysal, P.; Veronese, N.; Sánchez, G.F.L.; Vancampfort, D.; et al. The Association between Sedentary Behavior and Sarcopenia among Adults Aged ≥65 Years in Low- and Middle-Income Countries. Int. J. Environ. Res. Public Health 2020, 17, 1708. [Google Scholar] [CrossRef]
- Miyazaki, A.; Mori, H. Frequent Karaoke Training Improves Frontal Executive Cognitive Skills, Tongue Pressure, and Respiratory Function in Elderly People: Pilot Study from a Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2020, 17, 1459. [Google Scholar] [CrossRef]
- Lin, C.S.; Wu, C.Y.; Wu, S.Y.; Chuang, K.H.; Lin, H.H.; Cheng, D.H.; Lo, W.L. Age-and sex-related differences in masseter size and its role in oral functions. J. Am. Dent. Assoc. 2017, 148, 644–653. [Google Scholar] [CrossRef] [PubMed]
- Wakabayashi, H. Presbyphagia and Sarcopenic Dysphagia: Association between Aging, Sarcopenia, and Deglutition Disorders. J. Frailty Aging 2014, 3, 97–103. [Google Scholar] [PubMed]
- Byeon, H. Predicting the Swallow-Related Quality of Life of the Elderly Living in a Local Community Using Support Vector Machine. Int. J. Environ. Res. Public Health 2019, 16, 4269. [Google Scholar] [CrossRef] [PubMed]
- Azzolino, D.; Damanti, S.; Bertagnoli, L.; Lucchi, T.; Cesari, M. Sarcopenia and swallowing disorders in older people. Aging Clin. Exp. Res. 2019, 31, 799–805. [Google Scholar] [CrossRef]
- Ohira, A.; Ono, Y.; Yano, N.; Takagi, Y. The effect of chewing exercise in preschool children on maximum bite force and masticatory performance. Int. J. Paediatr. Dent. 2012, 22, 146–153. [Google Scholar] [CrossRef]
- Shirai, M.; Kawai, N.; Hichijo, N.; Watanabe, M.; Mori, H.; Mitsui, S.N.; Yasue, A.; Tanaka, E. Effects of gum chewing exercise on maximum bite force according to facial morphology. Clin. Exp. Dent. Res. 2018, 4, 48–51. [Google Scholar] [CrossRef]
- Nakagawa, K.; Matsuo, K.; Takagi, D.; Morita, Y.; Ooka, T.; Hironaka, S.; Mukai, Y. Effects of gum chewing exercises on saliva secretion and occlusal force in community-dwelling elderly individuals: A pilot study. Geriatr. Gerontol. Int. 2017, 17, 48–53. [Google Scholar] [CrossRef]
- Takeda, K.; Tanino, G.; Miyasaka, H. Review of devices used in neuromuscular electrical stimulation for stroke rehabilitation. Med. Devices 2017, 10, 207–213. [Google Scholar] [CrossRef]
- Young, W. Electrical stimulation and motor recovery. Cell Transpl. 2015, 24, 429–446. [Google Scholar] [CrossRef]
- Bao, S.C.; Khan, A.; Song, R.; Tong, R.K. Rewiring the Lesioned Brain: Electrical Stimulation for Post-Stroke Motor Restoration. J. Stroke 2020, 22, 47–63. [Google Scholar] [CrossRef]
- Meng, P.; Zhang, S.; Wang, Q.; Wang, P.; Han, C.; Gao, J.; Yue, S. The effect of surface neuromuscular electrical stimulation on patients with post-stroke dysphagia. J. Back Musculoskelet. Rehabil. 2018, 31, 363–370. [Google Scholar] [CrossRef]
- Oh, D.H.; Park, J.S.; Kim, W.J. Effect of neuromuscular electrical stimulation on lip strength and closure function in patients with dysphagia after stroke. J. Phys. Ther. Sci. 2017, 29, 1974–1975. [Google Scholar] [CrossRef] [PubMed]
- Yanase, K.; Hasegawa, S.; Nakamura, M.; Yamauchi, T.; Nishishita, S.; Araki, K.; Umehara, J.; Fujita, K.; Sato, I.; Ibuki, S.; et al. Electrical Stimulation to the Infraspinatus on Thickening and Strength of the Shoulder. Int. J. Sports Med. 2018, 39, 828–834. [Google Scholar] [PubMed]
- Mani, D.; Almuklass, A.M.; Amiridis, I.G.; Enoka, R.M. Neuromuscular electrical stimulation can improve mobility in older adults but the time course varies across tasks: Double-blind, randomized trial. Exp. Gerontol. 2018, 108, 269–275. [Google Scholar] [CrossRef] [PubMed]
- Acaröz, C.S.; Akoğlu, A.S.; Büğüşan, S.; Yüksel, F. Effects of neuromuscular electrical stimulation of quadriceps on the quadriceps strength and functional performance in nursing home residents: A comparison of short and long stimulation periods. Geriatr. Gerontol. Int. 2019, 19, 409–413. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.S.; Lee, J.H.; Kim, N.J. Effects of neuromuscular electrical stimulation on masticatory muscles in elderly stroke patients. J. Phys. Ther. Sci. 2015, 27, 2767–2770. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, A.P.; Costa, D.R.; Oliveira, A.I.; Carvalho, E.A.; Conti, P.C.; Costa, Y.M.; Bonjardim, L.R. Short-term transcutaneous electrical nerve stimulation reduces pain and improves the masticatory muscle activity in temporomandibular disorder patients: A randomized controlled trial. J. Appl. Oral Sci. 2017, 25, 112–120. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.W.; Kim, S.B.; Lee, J.H.; Lee, S.J.; Park, J.G.; Jang, K.W. Effects of Neuromuscular Electrical Stimulation for Masseter Muscle on Oral Dysfunction After Stroke. Ann. Rehabil. Med. 2019, 43, 11–18. [Google Scholar] [CrossRef]
- Schulz, K.F.; Altman, D.G.; Moher, D. CONSORT Group. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. BMJ 2010, 340, c332. [Google Scholar] [CrossRef]
- Yamaguchi, K.; Tohara, H.; Hara, K.; Nakane, A.; Yoshimi, K.; Nakagawa, K.; Minakuchi, S. Factors associated with masseter muscle quality assessed from ultrasonography in community-dwelling elderly individuals: A cross-sectional study. Arch. Gerontol. Geriatr. 2019, 82, 128–132. [Google Scholar] [CrossRef] [PubMed]
- Shaw, G.Y.; Sechtem, P.R.; Searl, J.; Keller, K.; Rawi, T.A.; Dowdy, E. Transcutaneous neuromuscular electrical stimulation (VitalStim) curative therapy for severe dysphagia: Myth or reality? Ann. Otol. Rhinol. Laryngol. 2007, 116, 36–44. [Google Scholar] [CrossRef] [PubMed]
- Freed, M.L.; Freed, L.; Chatburn, R.L.; Christian, M. Electrical stimulation for swallowing disorders caused by stroke. Respir. Care 2001, 46, 466–474. [Google Scholar] [PubMed]
- Farina, D.; Merletti, R.; Enoka, R.M. The extraction of neural strategies from the surface EMG. J. Appl. Physiol. 2004, 96, 1486–1495. [Google Scholar] [CrossRef] [PubMed]
- Rau, G.; Schulte, E.; Disselhorst-Klug, C. From cell to movement: To what answers does EMG really contribute? J. Electromyogr. Kinesiol. 2004, 14, 611–617. [Google Scholar] [CrossRef]
- Wheeler, K.M.; Chiara, T.; Sapienza, C.M. Surface electromyographic activity of the submental muscles during swallow and expiratory pressure threshold training tasks. Dysphagia 2007, 22, 108–116. [Google Scholar] [CrossRef]
- Nozoe, M.; Kanai, M.; Kubo, H.; Takeuchi, Y.; Kobayashi, M.; Yamamoto, M.; Furuichi, A.; Yamazaki, M.; Shimada, S.; Mase, K. Efficacy of neuromuscular electrical stimulation for preventing quadriceps muscle wasting in patients with moderate or severe acute stroke: A pilot study. NeuroRehabilitation 2017, 41, 143–149. [Google Scholar] [CrossRef]
- Mizuno, T. Combined Effects of Static Stretching and Electrical Stimulation on Joint Range of Motion and Muscle Strength. J. Strength Cond. Res. 2019, 33, 2694–2703. [Google Scholar] [CrossRef]
- Lee, D.; Lee, G. Effect of afferent electrical stimulation with mirror therapy on motor function, balance, and gait in chronic stroke survivors: A randomized controlled trial. Eur. J. Phys. Rehabil. Med. 2019, 55, 442–449. [Google Scholar] [CrossRef]
- Gondin, J.; Guette, M.; Ballay, Y.; Martin, A. Electromyostimulation training effects on neural drive and muscle architecture. Med. Sci. Sports Exerc. 2005, 37, 1291–1299. [Google Scholar] [CrossRef]
- Vivodtzev, I.; Debigaré, R.; Gagnon, P.; Mainguy, V.; Saey, D.; Dubé, A.; Paré, M.È.; Bélanger, M.; Maltais, F. Functional and muscular effects of neuromuscular electrical stimulation in patients with severe COPD: A randomized clinical trial. Chest 2012, 141, 716–725. [Google Scholar] [CrossRef]
- Park, J.S.; Oh, D.H.; Hwang, N.K.; Lee, J.H. Effects of neuromuscular electrical stimulation in patients with Parkinson’s disease and dysphagia: A randomized, single-blind, placebo-controlled trial. NeuroRehabilitation 2018, 42, 457–463. [Google Scholar] [CrossRef] [PubMed]
- Park, J.S.; Oh, D.H.; Hwang, N.K.; Lee, J.H. Effects of neuromuscular electrical stimulation combined with effortful swallowing on post-stroke oropharyngeal dysphagia: A randomised controlled trial. J. Oral Rehabil. 2016, 43, 426–434. [Google Scholar] [CrossRef] [PubMed]
- Dupont-Versteegden, E.E. Apoptosis in muscle atrophy: Relevance to sarcopenia. Exp. Gerontol. 2005, 40, 473–481. [Google Scholar] [CrossRef] [PubMed]
- Nilwik, R.; Snijders, T.; Leenders, M.; Groen, B.B.; van Kranenburg, J.; Verdijk, L.B.; van Loon, L.J. The decline in skeletal muscle mass with aging is mainly attributed to a reduction in type II muscle fiber size. Exp. Gerontol. 2013, 48, 492–498. [Google Scholar] [CrossRef]
- Brunner, F.; Schmid, A.; Sheikhzadeh, A.; Nordin, M.; Yoon, J.; Frankel, V. Effects of aging on Type II muscle fibers: A systematic review of the literature. J. Aging Phys. Act. 2007, 15, 336–348. [Google Scholar] [CrossRef]

| Experimental Group | Placebo Group | |
|---|---|---|
| Number of subjects | 17 | 18 |
| Gender (male/female) | 7/10 | 10/8 |
| Age (year) | 72.4 ± 4.1 | 73.3 ± 4.7 |
| Height (cm) | 166.2 ± 5.8 | 165.1 ± 7.5 |
| Weight (kg) | 64.2 ± 7.3 | 65.3 ± 6.5 |
| Total number of teeth remaining | 23.5 ± 2.2 | 23.2 ± 2.1 |
| Masseter muscle thickness | 7.36 ± 0.50 | 7.60 ± 0.49 |
| Maximum occlusal force | 261.13 ± 9.84 | 265.87 ± 9.97 |
| Stimulation intensity (mA) | 7.3 ± 3.5 | 0.5 |
| Experimental Group (n = 17) | Placebo Group (n = 18) | Intergroup p-Values | |||||
|---|---|---|---|---|---|---|---|
| Before | After | p-Value | Before | After | p-Value | ||
| MMT (mm) | 7.36 ± 0.50 | 8.34 ± 0.61 | 0.001 * | 7.60 ± 0.49 | 7.69 ± 0.45 | 0.087 | 0.002 † |
| MOF (newton) | 261.13 ± 9.84 | 275.20 ± 9.43 | 0.001 * | 265.87 ± 9.97 | 266.60 ± 9.67 | 0.065 | 0.019 † |
| Experimental Group | Placebo Group | Intergroup p-Value | Cohen’s d (Interpretation) | |
|---|---|---|---|---|
| Δ MMT (mm) | 0.98 ± 0.61 | 0.08 ± 0.18 | <0.001 † | 2.6 (large effect) |
| Δ MOF (newton) | 11.07 ± 4.34 | 0.73 ± 1.43 | <0.001 † | 2.0 (large effect) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, M.-Y.; Lee, G.; Jung, Y.-J.; Park, J.-S. Effect of Neuromuscular Electrical Stimulation on Masseter Muscle Thickness and Maximal Bite Force among Healthy Community-Dwelling Persons Aged 65 Years and Older: A Randomized, Double Blind, Placebo-Controlled Study. Int. J. Environ. Res. Public Health 2020, 17, 3783. https://doi.org/10.3390/ijerph17113783
Chang M-Y, Lee G, Jung Y-J, Park J-S. Effect of Neuromuscular Electrical Stimulation on Masseter Muscle Thickness and Maximal Bite Force among Healthy Community-Dwelling Persons Aged 65 Years and Older: A Randomized, Double Blind, Placebo-Controlled Study. International Journal of Environmental Research and Public Health. 2020; 17(11):3783. https://doi.org/10.3390/ijerph17113783
Chicago/Turabian StyleChang, Moon-Young, Gihyoun Lee, Young-Jin Jung, and Ji-Su Park. 2020. "Effect of Neuromuscular Electrical Stimulation on Masseter Muscle Thickness and Maximal Bite Force among Healthy Community-Dwelling Persons Aged 65 Years and Older: A Randomized, Double Blind, Placebo-Controlled Study" International Journal of Environmental Research and Public Health 17, no. 11: 3783. https://doi.org/10.3390/ijerph17113783
APA StyleChang, M.-Y., Lee, G., Jung, Y.-J., & Park, J.-S. (2020). Effect of Neuromuscular Electrical Stimulation on Masseter Muscle Thickness and Maximal Bite Force among Healthy Community-Dwelling Persons Aged 65 Years and Older: A Randomized, Double Blind, Placebo-Controlled Study. International Journal of Environmental Research and Public Health, 17(11), 3783. https://doi.org/10.3390/ijerph17113783






