Studying Public Perception about Vaccination: A Sentiment Analysis of Tweets
Abstract
1. Introduction
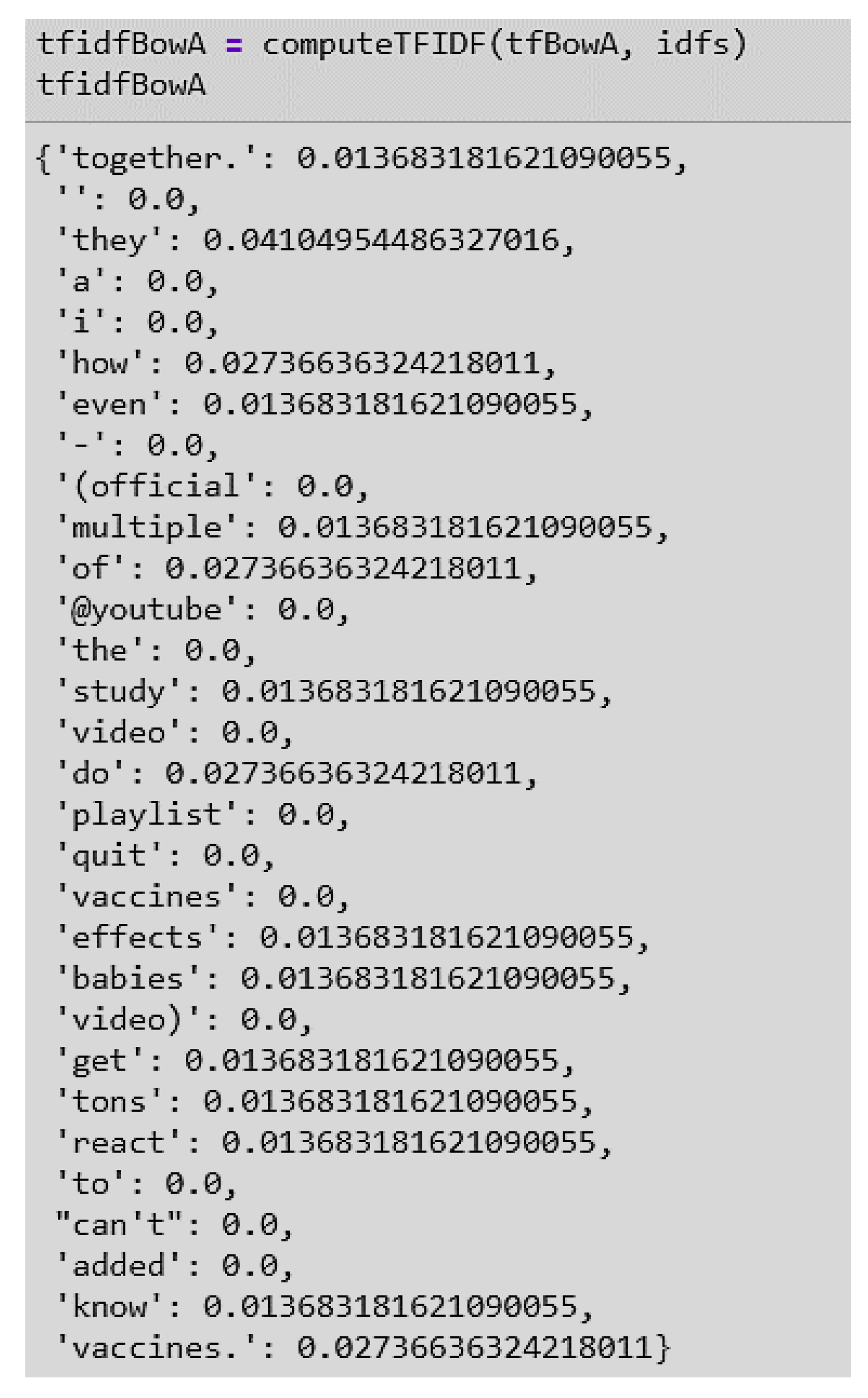
2. Background
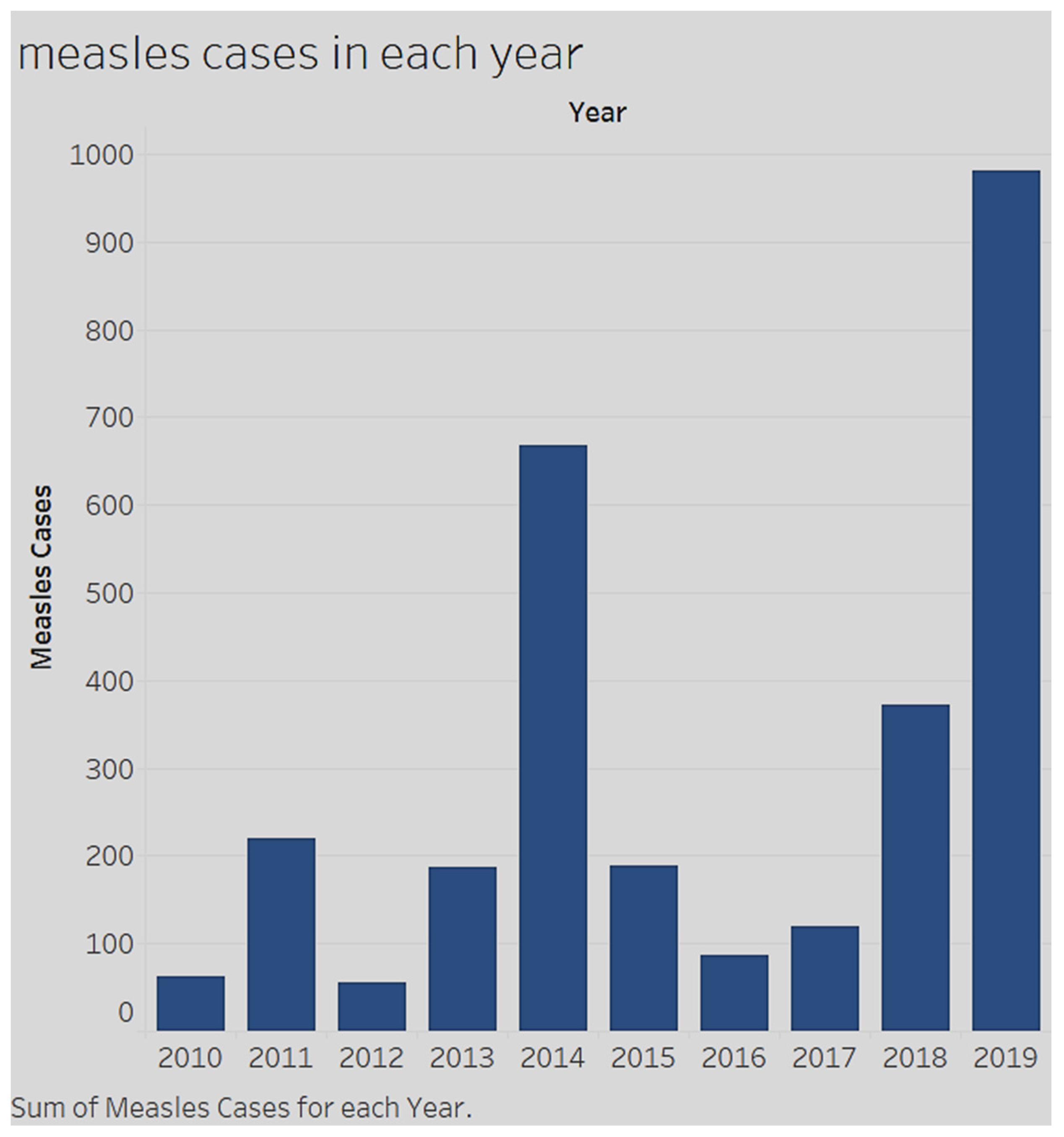
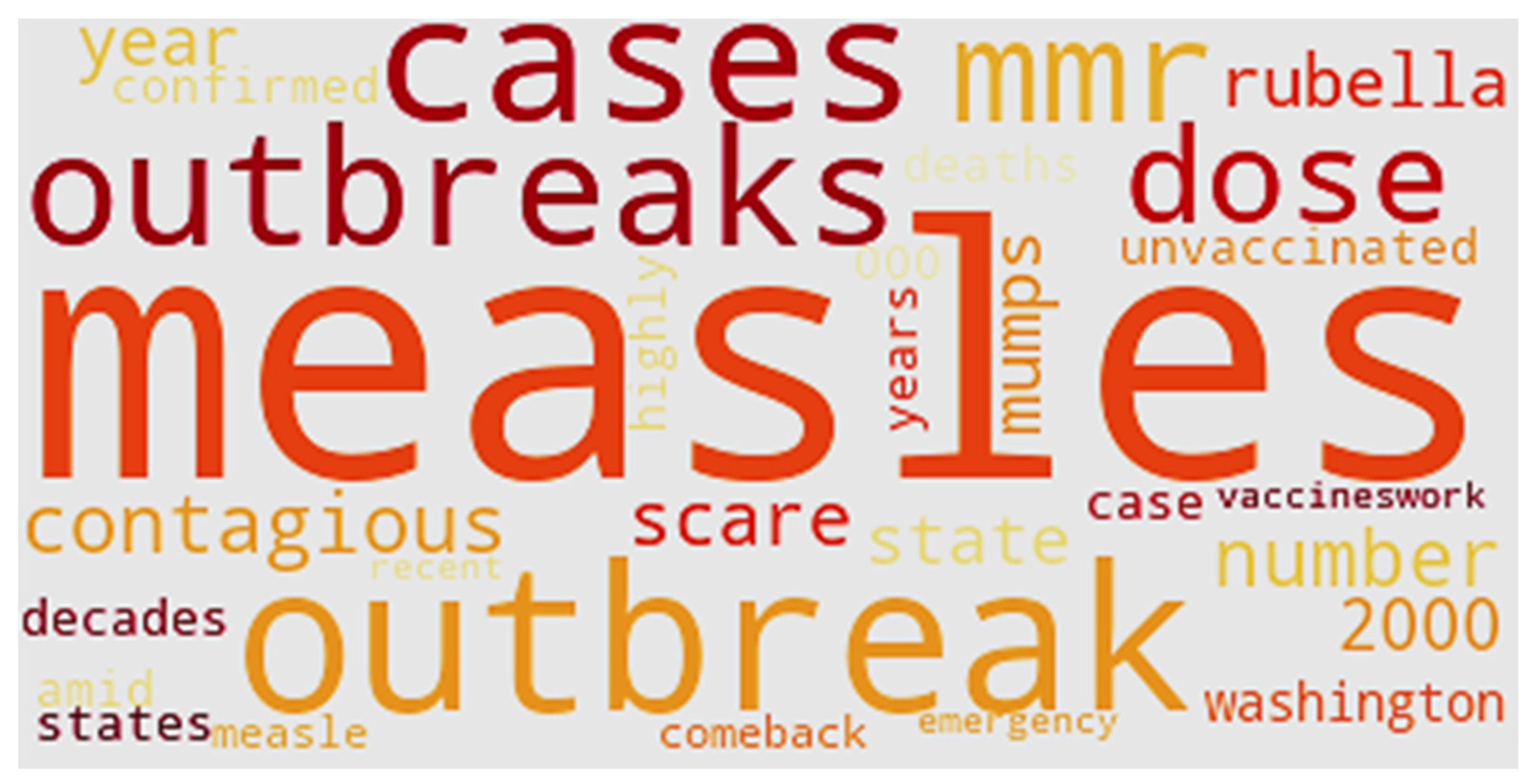
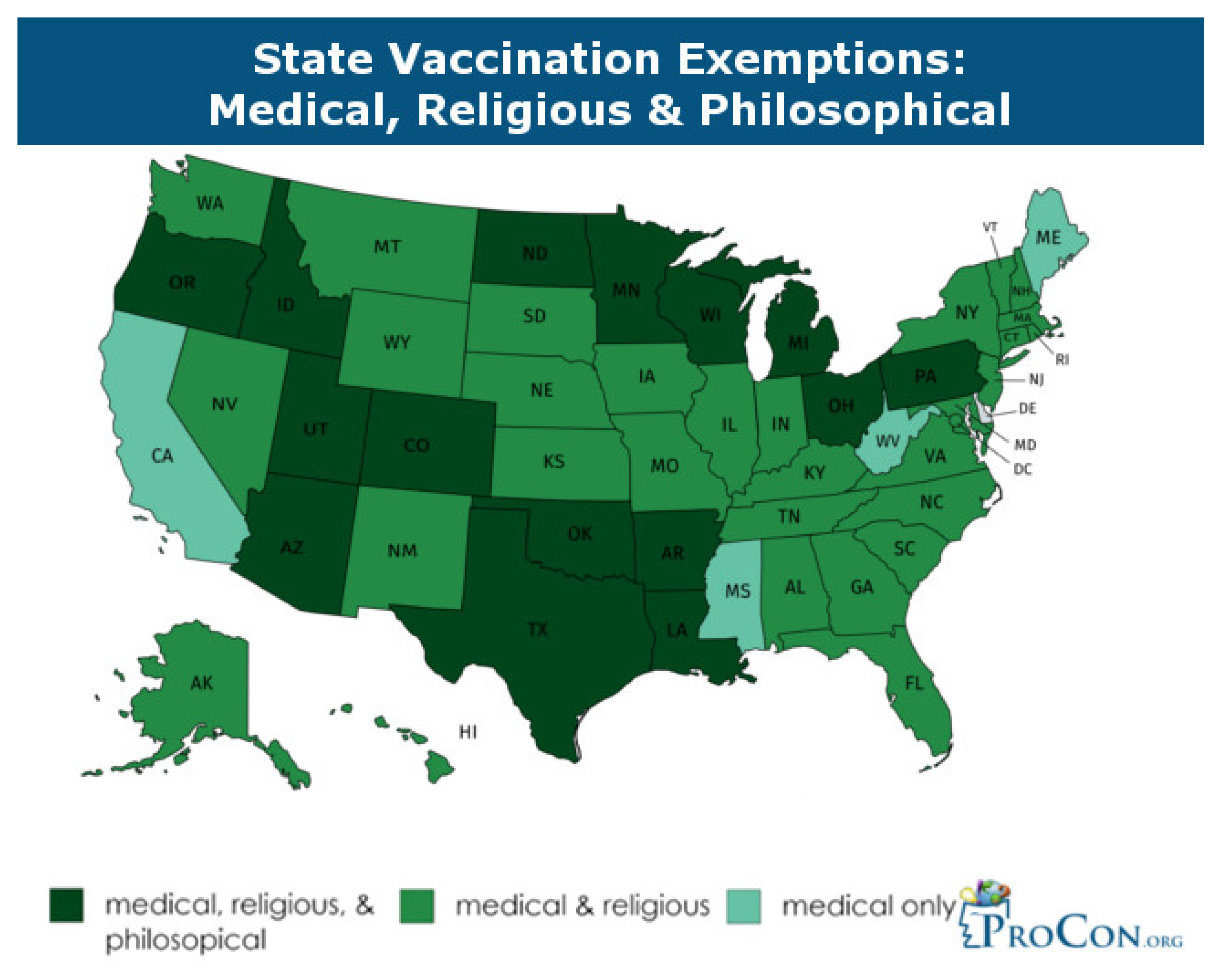
2.1. Increasing Incidence of Measles and Low Vaccination Rates
2.2. Sentiments towards Vaccination
2.3. Social Media and the Dissemination of (Mis)information
2.4. Sentiment Analysis
3. Methods
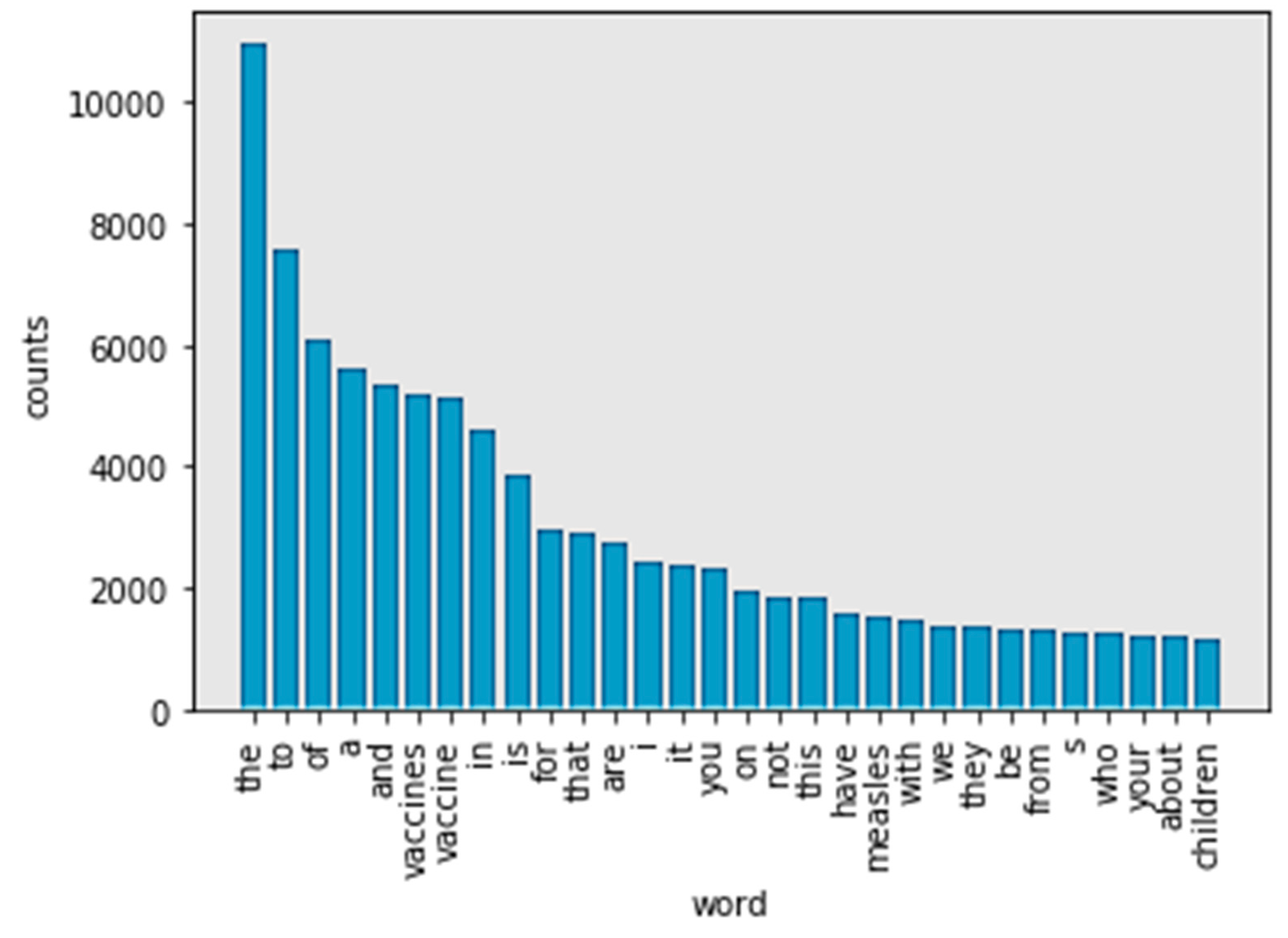
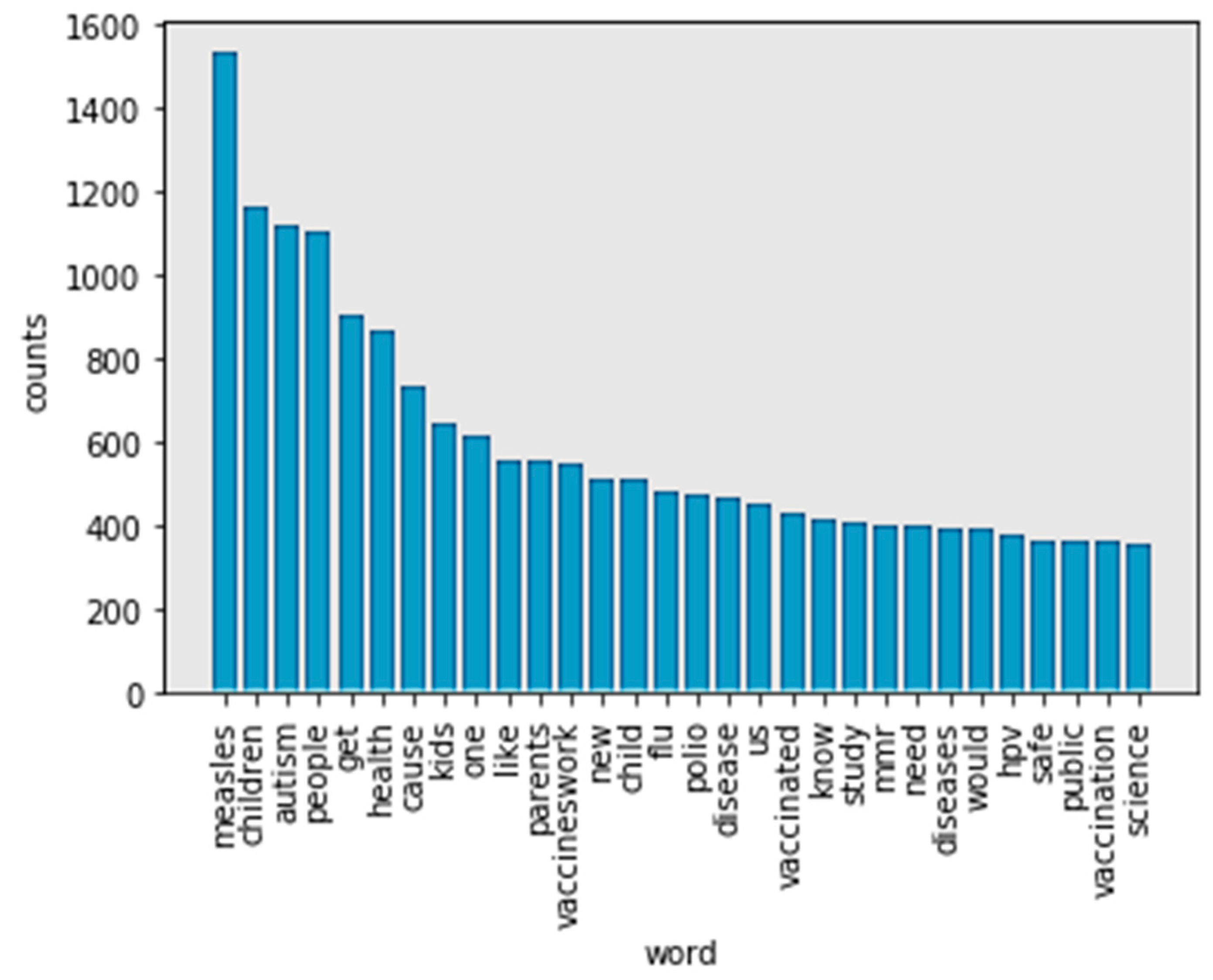
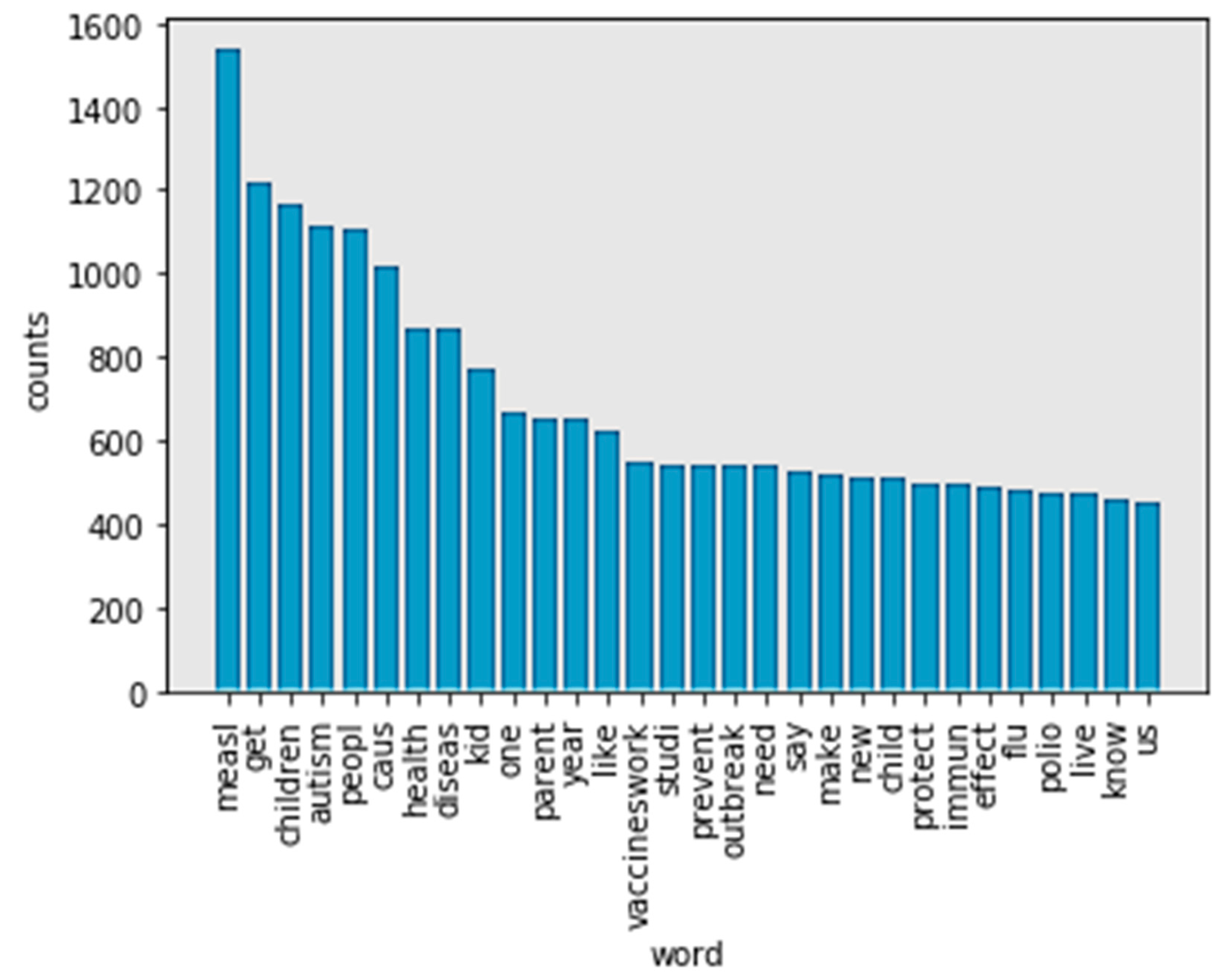
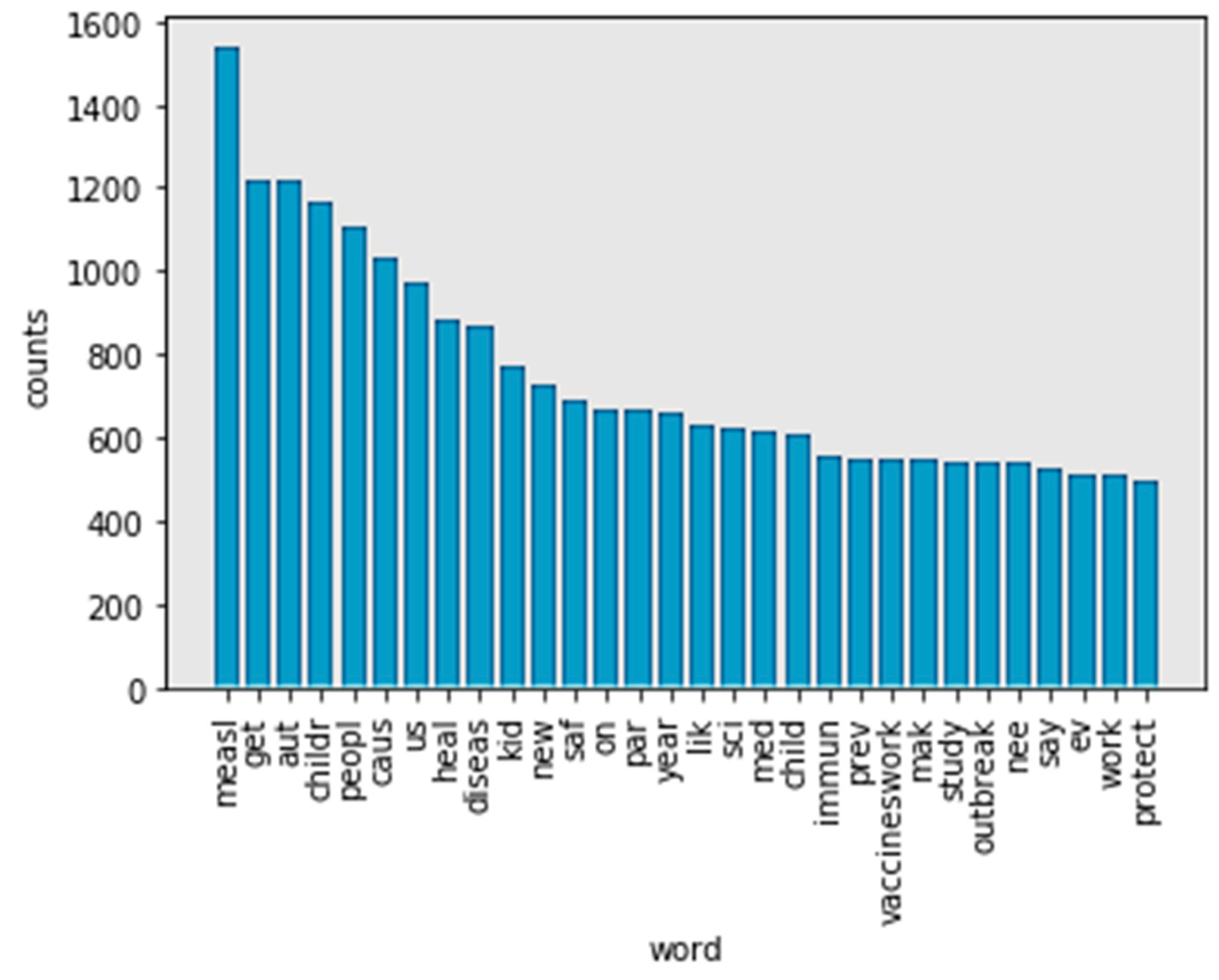
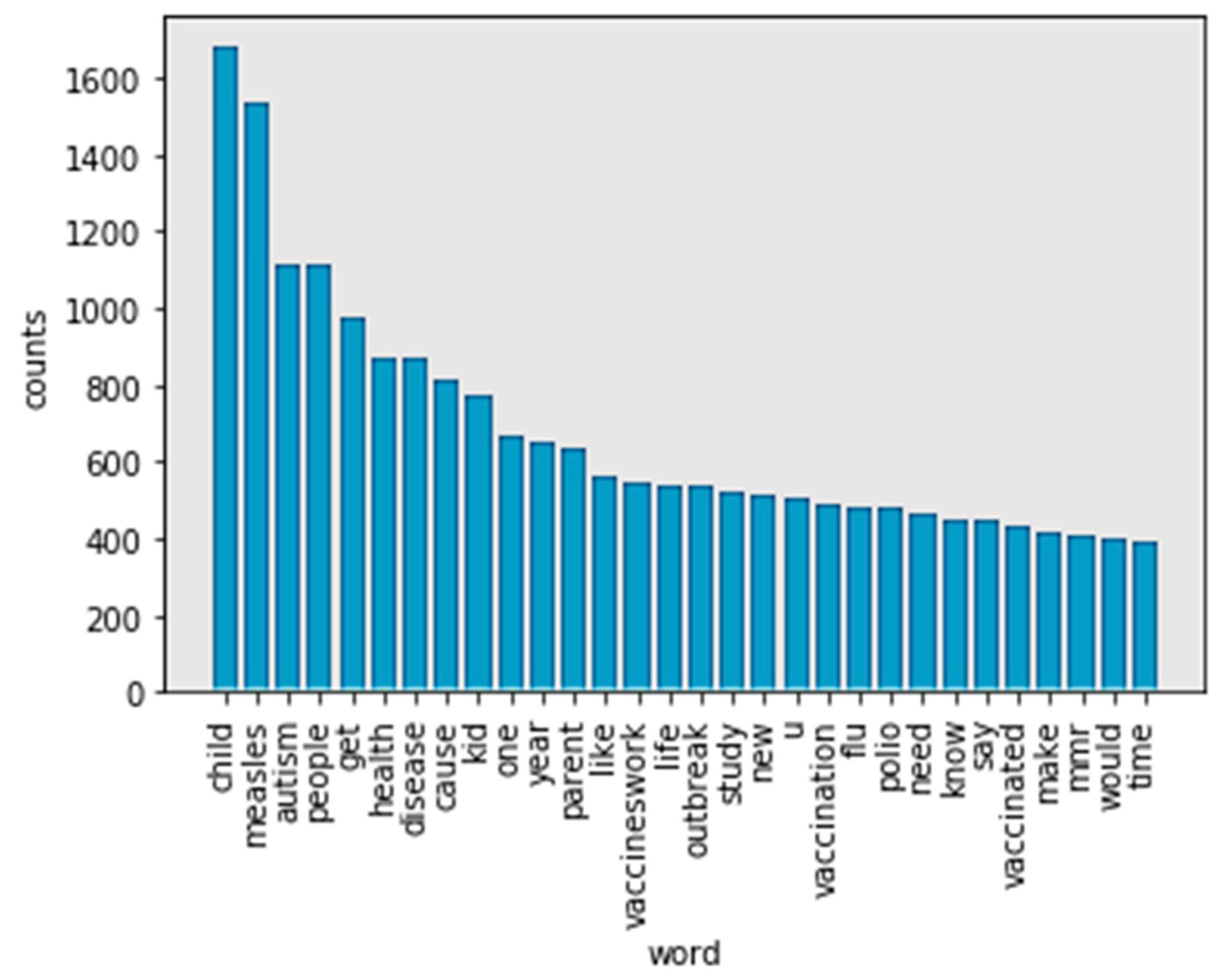
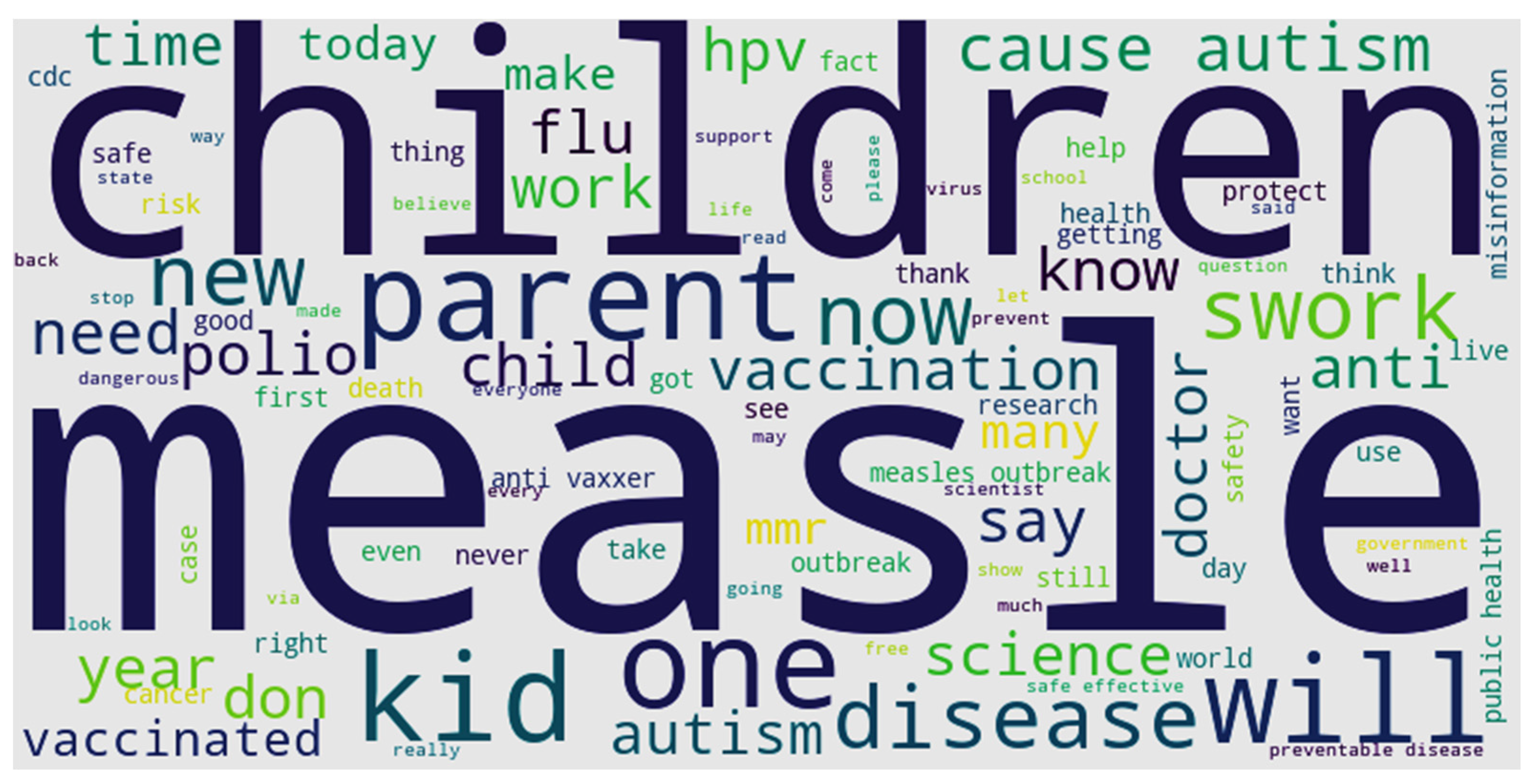
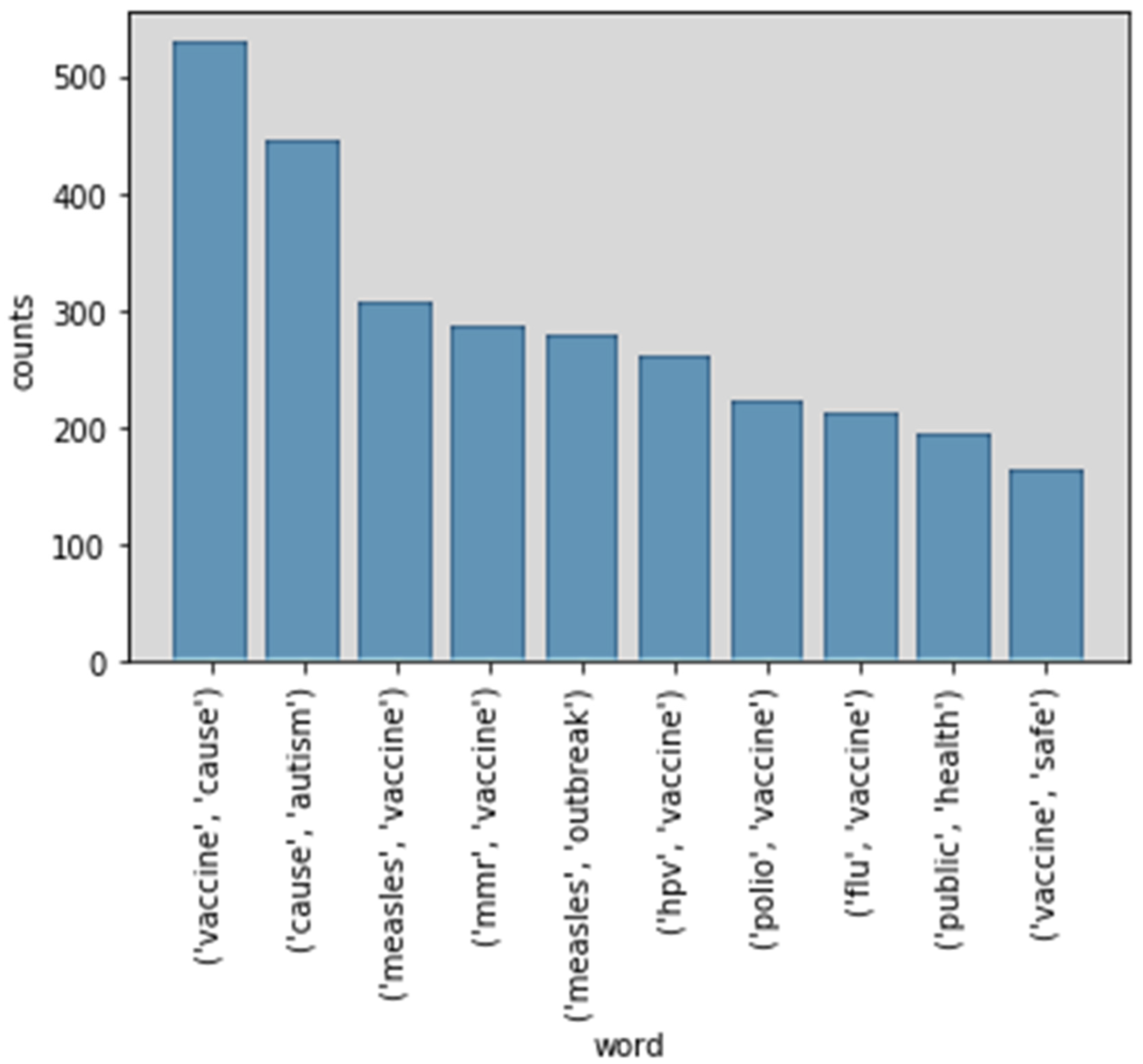
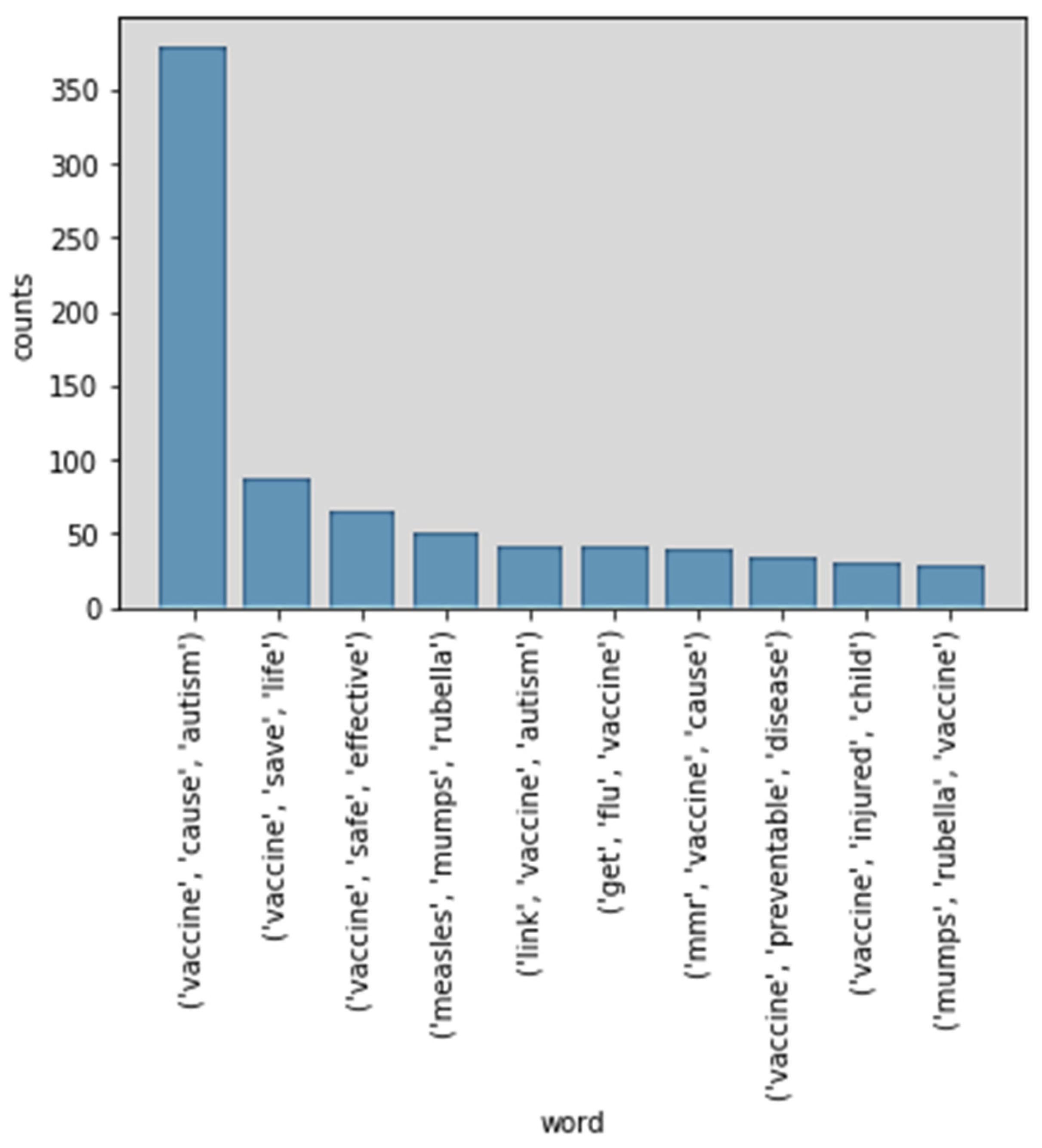
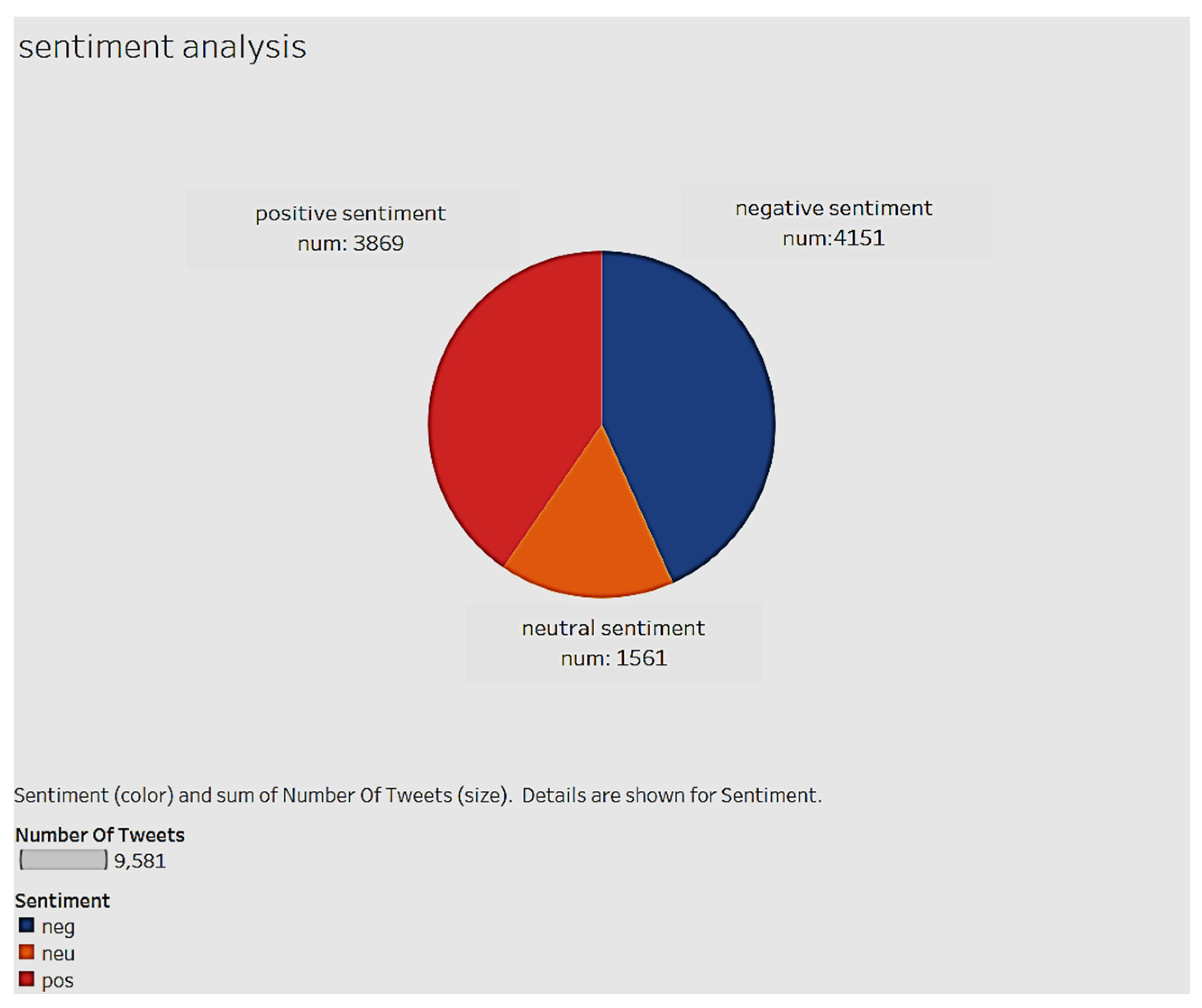
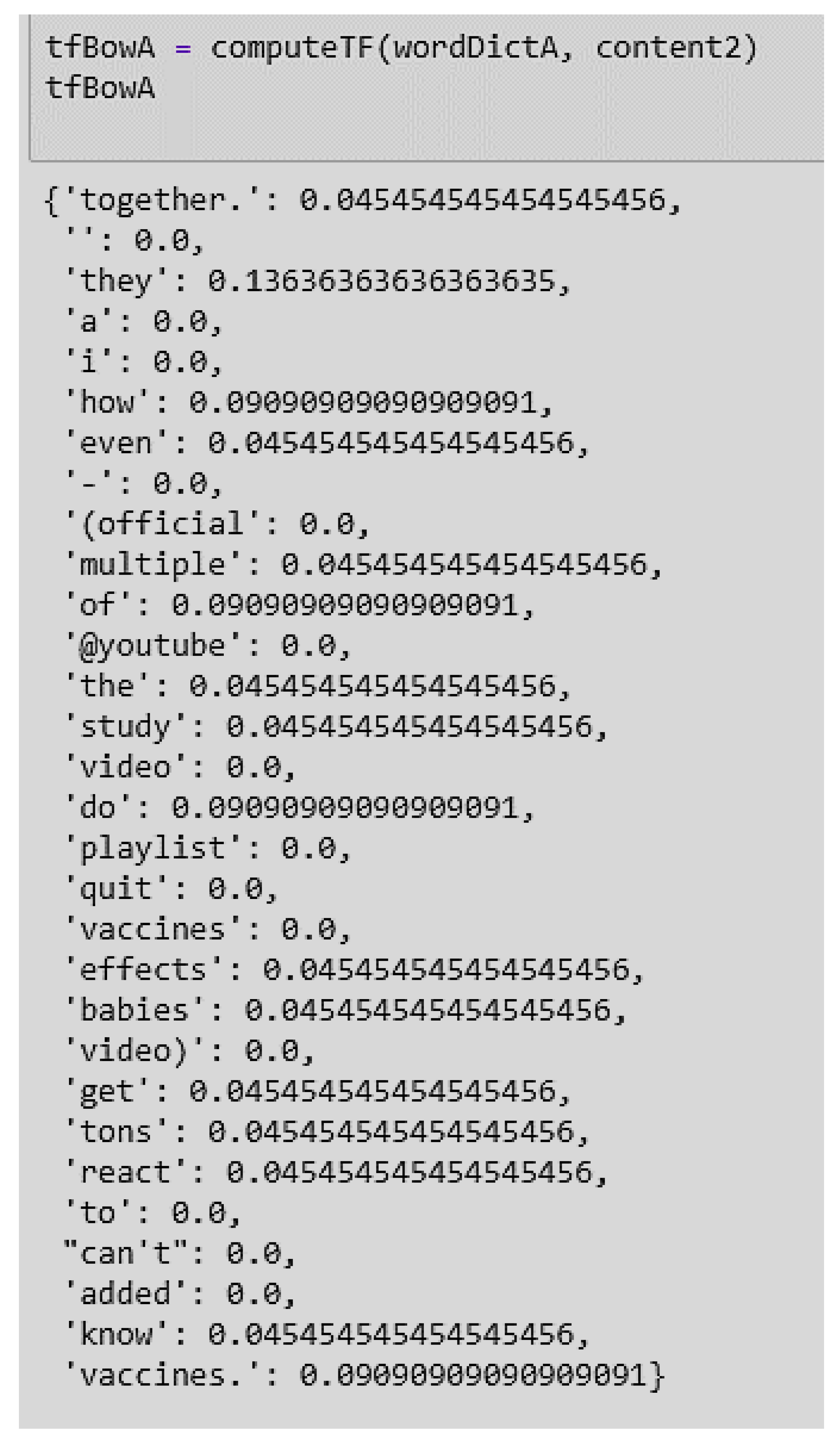
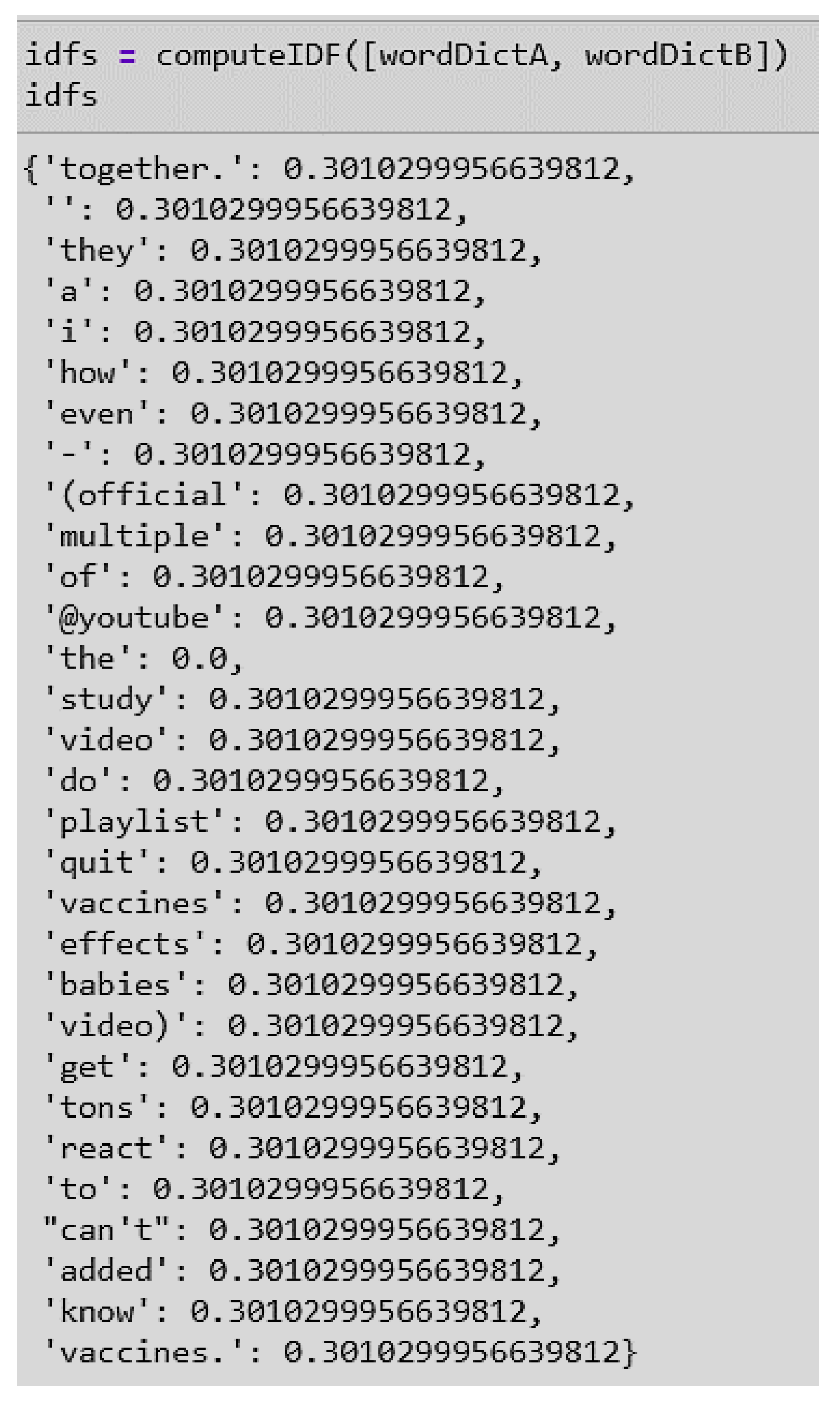
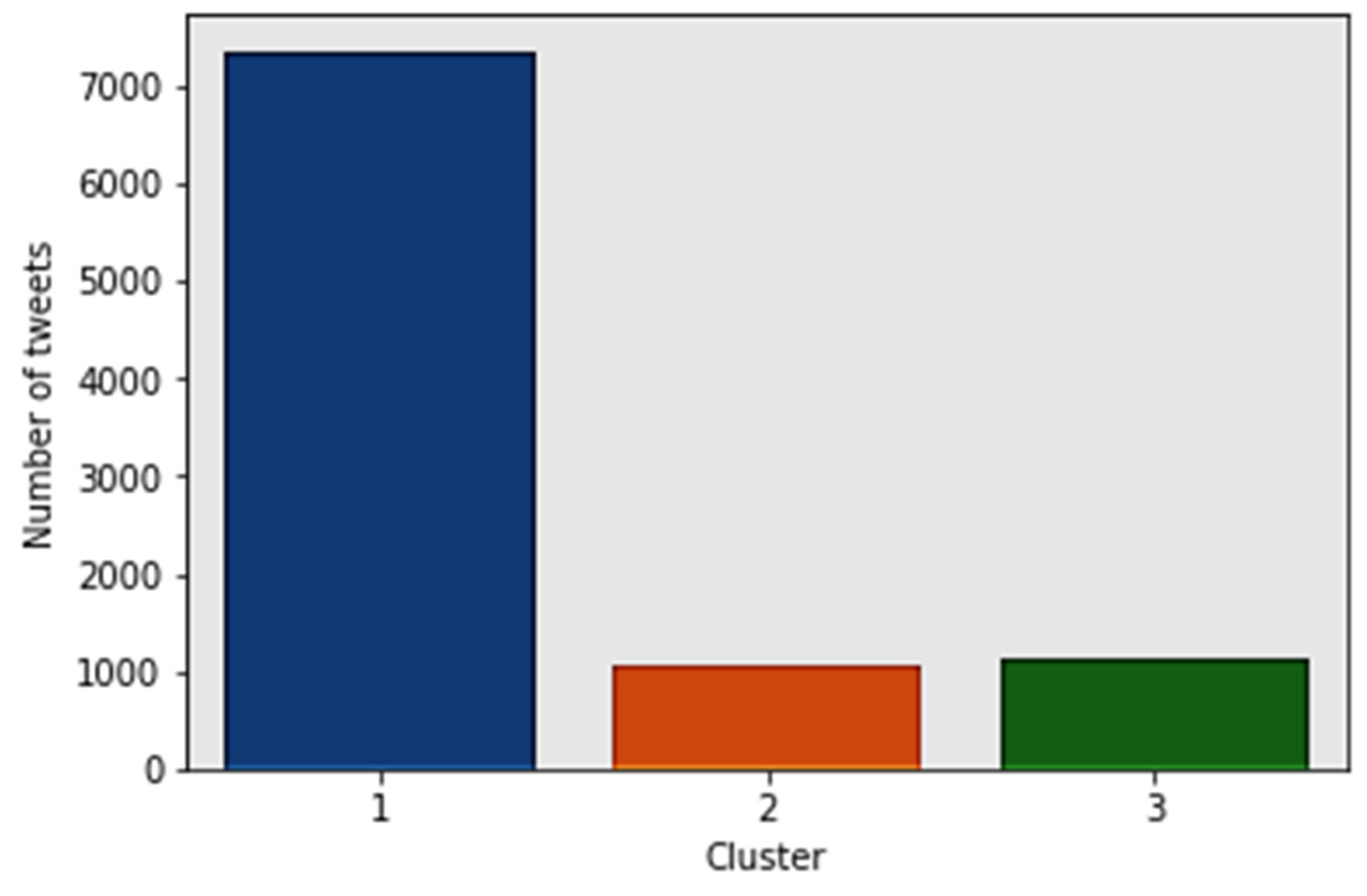
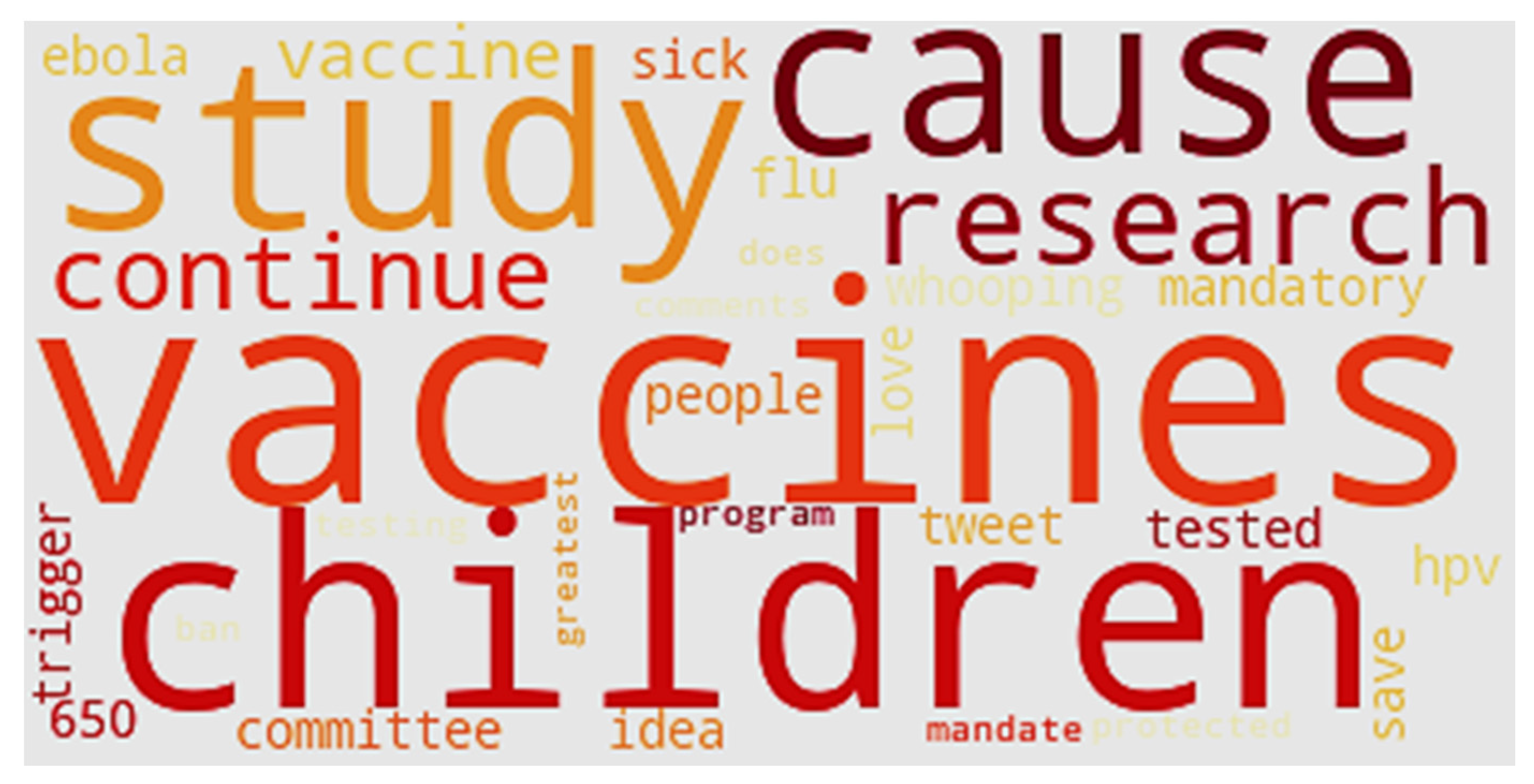
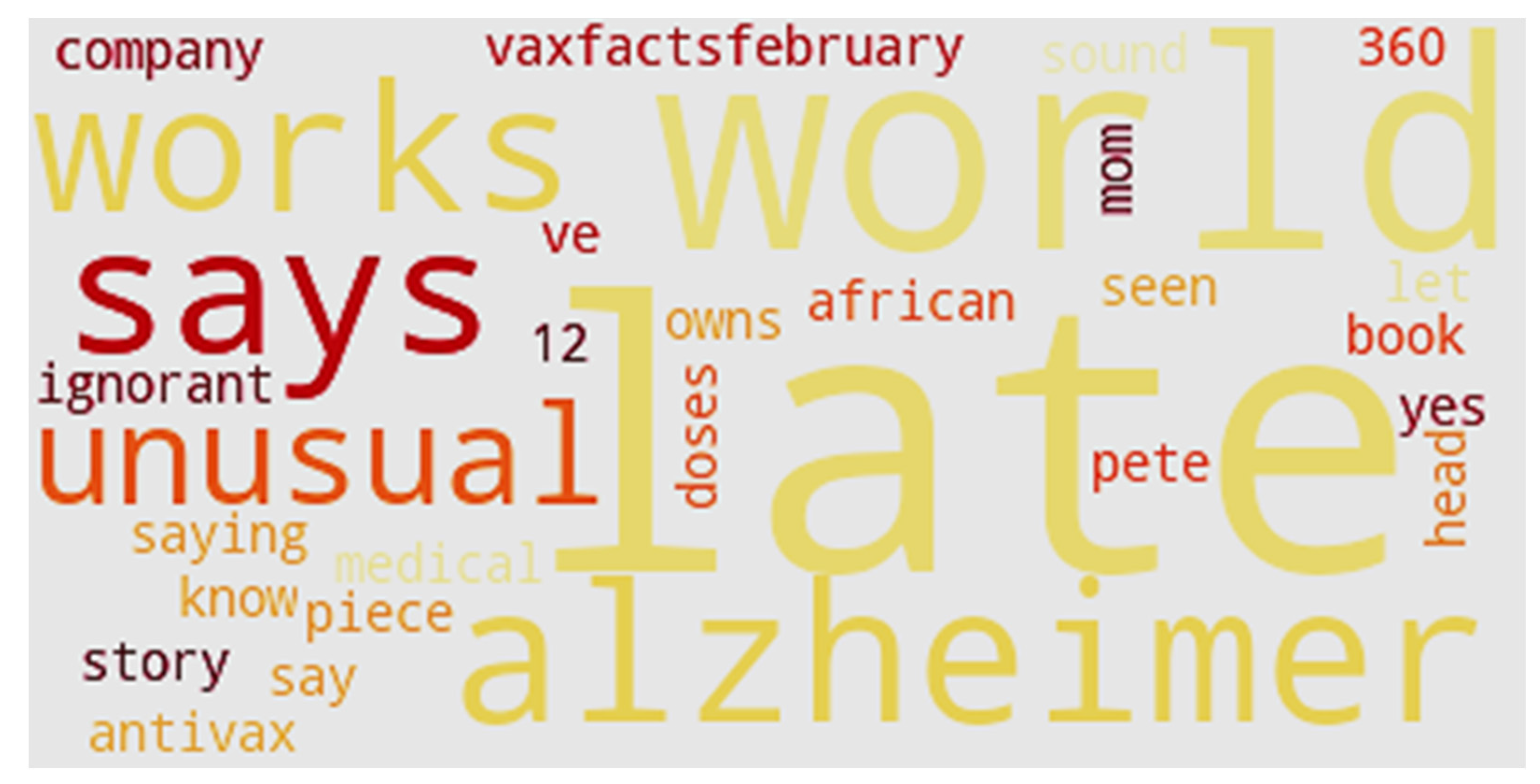
4. Results
5. Discussion
6. Scope and Limitations
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Cousins, S. Measles: A global resurgence. Lancet Infect. Dis. 2019, 19, 362. [Google Scholar] [CrossRef]
- Karasz, P.W.H.O. Warns of ‘Dramatic’ Rise in Measles in Europe. The New York Times. 30 August 2019. Available online: https://www.nytimes.com/2019/08/29/world/europe/measles-uk-czech-greece-albania.html?searchResultPosition=1 (accessed on 10 January 2020).
- Larson, K. WHO: Death Toll From Measles Outbreak in Congo Hits 6000. Associated Press. 7 January 2020. Available online: https://www.usnews.com/news/world/articles/2020-01-07/who-death-toll-from-measles-outbreak-in-congo-hits-6-000 (accessed on 10 January 2020).
- Kupferschmidt, K. Study pushes emergence of measles back to antiquity. Science 2020, 367, 11–12. [Google Scholar] [CrossRef]
- Hussain, A.; Ali, S.; Ahmed, M.; Hussain, S. The anti-vaccination movement: A regression in modern medicine. Cureus 2018, 10, 1–8. [Google Scholar] [CrossRef]
- Mitra, T.; Counts, S.; Pennebaker, J.W. Understanding anti-vaccination attitudes in social media. In Proceedings of the Tenth International AAAI Conference on Web and Social Media, Cologne, Germany, 17–20 May 2016. [Google Scholar]
- Numnark, S.; Ingsriswang, S.; Wichadakul, D. VaccineWatch: A monitoring system of vaccine messages from social media data. In Proceedings of the 8th International Conference on Systems Biology (ISB), Qingdao, China, 24–27 October 2014. [Google Scholar]
- Salathé, M.; Khandelwal, S. Assessing vaccination sentiments with online social media: Implications for infectious disease dynamics and control. PLoS Comput. Biol. 2011, 7, e1002199. [Google Scholar]
- The Statistics Portal. Twitter: Number of Monthly Active U.S. Users 2010–2018. Available online: https://www.statista.com/statistics/274564/monthly-active-twitter-users-in-the-united-states/ (accessed on 20 February 2020).
- Sewalk, K.C.; Tuli, G.; Hswen, Y.; Brownstein, J.S.; Hawkins, J.B. Using Twitter to examine Web-based patient experience sentiments in the United States: Longitudinal study. J. Med. Internet Res. 2018, 20, e10043. [Google Scholar] [CrossRef] [PubMed]
- Surian, D.; Nguyen, D.Q.; Kennedy, G.; Johnson, M.; Coiera, E.; Dunn, A.G. Characterizing Twitter discussions about HPV vaccines using topic modeling and community detection. J. Med. Internet Res. 2016, 18, e232. [Google Scholar] [CrossRef] [PubMed]
- Radzikowski, J.; Stefanidis, A.; Jacobsen, K.H.; Croitoru, A.; Crooks, A.; Delamater, P.L. The measles vaccination narrative in Twitter: A quantitative analysis. Jmir Public Health Surveill. 2016, 2, e1. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.; Dredze, M. Vaccine images on twitter: Analysis of what images are shared. J. Med. Internet Res. 2018, 20, e130. [Google Scholar] [CrossRef]
- Zhou, X.; Coiera, E.; Tsafnat, G.; Arachi, D.; Ong, M.S.; Dunn, A.G. Using social connection information to improve opinion mining: Identifying negative sentiment about HPV vaccines on Twitter. Stud. Health Technol. Inf. 2015, 216, 761–765. [Google Scholar]
- Dredze, M.; Wood-Doughty, Z.; Quinn, S.C.; Broniatowski, D.A. Vaccine opponents’ use of Twitter during the 2016 US presidential election: Implications for practice and policy. Vaccine 2017, 35, 4670–4672. [Google Scholar] [CrossRef]
- Thakkar, N.; Gilani SS, A.; Hasan, Q.; McCarthy, K.A. Decreasing measles burden by optimizing campaign timing. Proc. Natl. Acad. Sci. USA 2019, 116, 11069–11073. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Chapter 7: Measles. Available online: https://www.cdc.gov/vaccines/pubs/surv-manual/chpt07-measles.html (accessed on 25 April 2020).
- Brown, D. In 2000, Measles Had Been Officially ‘Eliminated’ in the U.S. Will That Change? The Washington Post. 28 September 2019. Available online: https://www.washingtonpost.com/health/in-2000-measles-had-been-officially-eliminated-in-the-us-will-that-change/2019/09/27/56ac487a-deed-11e9-b199-f638bf2c340f_story.html (accessed on 10 January 2020).
- Sundaram, M.E.; Guterman, L.B.; Omer, S.B. The true cost of measles outbreaks during the post elimination era. JAMA 2019, 321, 1155. [Google Scholar] [CrossRef]
- National Institute of Health. Decline in Measles Vaccination is Causing a Preventable Global Resurgence of the Disease. Available online: https://www.nih.gov/news-events/news-releases/decline-measles-vaccination-causing-preventable-global-resurgence-disease (accessed on 25 April 2020).
- Centers for Disease Control and Prevention. Transmission of Measles. Available online: https://www.cdc.gov/measles/transmission.html (accessed on 25 April 2020).
- Centers for Disease Control and Prevention. Measles Cases and Outbreaks. Available online: https://www.cdc.gov/measles/cases-outbreaks.html (accessed on 25 April 2020).
- Centers for Disease Control and Prevention. National Updates on Measles Cases and Outbreaks—United States, January 1–Octoer 1, 2019. Available online: https://www.cdc.gov/mmwr/volumes/68/wr/mm6840e2.htm (accessed on 25 April 2020).
- Avila, J.D. Connecticut’s Measles Vaccination Rates Keep Falling. The Wall Street Journal. 29 August 2019. A9A. Available online: https://www.wsj.com/articles/connecticuts-measles-vaccination-rates-keep-falling-11567109137 (accessed on 10 January 2020).
- Morbidity and Mortality Weekly Report (2 May 2019). Increase in Measles Cases—United States, 1 January–26 April 2019. Available online: https://www.cdc.gov/mmwr/volumes/68/wr/mm6817e1.htm (accessed on 25 April 2020).
- Gonzales, R. CDC Reports Largest U.S. Measles Outbreak Since Year 2000. Available online: https://www.npr.org/2019/04/24/716953746/cdc-reports-largest-u-s-measles-outbreak-since-year-2000 (accessed on 25 April 2020).
- Jost, M.; Luzi, D.; Metzler, S.; Miran, B.; Mutsch, M. Measles associated with international travel in the region of the Americas, Australia and Europe, 2001–2013: A systematic review. Travel Med. Infect. Dis. 2015, 13, 10–18. [Google Scholar] [CrossRef]
- CDC Notes from the field: Measles outbreak among members of a religious community—Brooklyn, New York, March-June 2013. MMWR 2013, 62, 752–753.
- Salmon, D.A.; Haber, M.; Gangarosa, E.J.; Phillips, L.; Smith, N.J.; Chen, R.T. Health consequences of religious and philosophical exemptions from immunization laws: Individual and societal risk of measles. JAMA 1999, 282, 47–53. [Google Scholar] [CrossRef]
- Wombwell, E.; Fangman, M.T.; Yoder, A.K. Religious Barriers to Measles Vaccination. J. Commun. Health 2015, 40, 597–604. [Google Scholar] [CrossRef]
- Fiebelkorn, P.A.; Redd, S.B.; Gallagher, K.; Rota, P.A.; Rota, J.; Bellini, W.; Seward, J. Measles in the United States during the post elimination era. J. Infect. Dis. 2010, 202, 1520–1528. [Google Scholar] [CrossRef]
- Opel, D.J.; Omer, S.B. Measles, mandates, and making vaccination the default option. JAMA Pediatrics 2015, 169, 303–304. [Google Scholar] [CrossRef]
- Phadke, V.K.; Bednarczyk, R.A.; Salmon, D.A.; Omer, S.B. Association between vaccine refusal and vaccine-preventable diseases in the United States: A review of measles and pertussis. JAMA 2016, 315, 1149–1158. [Google Scholar] [CrossRef]
- Stanley-Becker, I. Officials in anti-vaccination ‘hotspot’ near Portland declare an emergency over measles outbreak. The Washington Post, 23 January 2019. [Google Scholar]
- Jackson, M.A.; Harrison, C. On the Brink: Why the US is in Danger of Losing Measles Elimination Status. Mol. Med. 2019, 116, 260. [Google Scholar]
- Papania, M.J.; Wallace, G.S.; Rota, P.A.; Icenogle, J.P.; Fiebelkorn, A.P.; Armstrong, G.L.; Hao, L. Elimination of endemic measles, rubella, and congenital rubella syndrome from the Western hemisphere: The US experience. JAMA Pediatrics 2014, 168, 148–155. [Google Scholar] [CrossRef]
- Patel, M.; Lee, A.D.; Clemmons, N.S.; Redd, S.B.; Poser, S.; Blog, D.; Arciuolo, R.J. National update on measles cases and outbreaks—United States, January 1–October 1, 2019. Morb. Mortal. Wkly. Rep. 2019, 68, 893. [Google Scholar] [CrossRef]
- Cao, L.; Zheng, J.; Cao, L.; Cui, J.; Xiao, Q. Evaluation of the impact of Shandong illegal vaccine sales incident on immunizations in China. Hum. Vaccines Immunother. 2018, 14, 1672–1678. [Google Scholar] [CrossRef]
- Wang, L.D.; Lam, W.W.; Wu, J.T.; Liao, Q.; Fielding, R. Chinese immigrant parents’ vaccination decision making for children: A qualitative analysis. BMC Public Health 2014, 14, 133. [Google Scholar] [CrossRef]
- Zhou, M.; Qu, S.; Zhao, L.; Kong, N.; Campy, K.S.; Wang, S. Trust collapse caused by the Changsheng vaccine crisis in China. Vaccine 2019, 37, 3419. [Google Scholar] [CrossRef]
- Hendriks, J.; Liang, Y.; Zeng, B. China’s emerging vaccine industry. Hum. Vaccines 2010, 6, 602–607. [Google Scholar] [CrossRef]
- Kaddar, M.; Milstien, J.; Schmitt, S. Impact of BRICS? investment in vaccine development on the global vaccine market. Bull. World Health Organ. 2014, 92, 436–446. [Google Scholar] [CrossRef]
- Levin, C.E.; Sharma, M.; Olson, Z.; Verguet, S.; Shi, J.F.; Wang, S.M.; Kim, J.J. An extended cost-effectiveness analysis of publicly financed HPV vaccination to prevent cervical cancer in China. Vaccine 2015, 33, 2830–2841. [Google Scholar] [CrossRef]
- Yiming, L.; Zaiping, J. Lessons from the Chinese defective vaccine case. Lancet Infect. Dis. 2019, 19, 245. [Google Scholar] [CrossRef]
- Yuan, X. China’s vaccine production scare. Lancet 2018, 392, 371. [Google Scholar] [CrossRef]
- Clemmons, N.S.; Gastanaduy, P.A.; Fiebelkorn, A.P.; Redd, S.B.; Wallace, G.S. Measles—United States, 4 January–2 April 2015. Mmwr. Morb. Mortal. Wkly. Rep. 2015, 64, 373. [Google Scholar]
- Majumder, M.S.; Cohn, E.L.; Mekaru, S.R.; Huston, J.E.; Brownstein, J.S. Substandard vaccination compliance and the 2015 measles outbreak. JAMA Pediatrics 2015, 169, 494–495. [Google Scholar] [CrossRef]
- Olive, J.K.; Hotez, P.J.; Damania, A.; Nolan, M.S. The state of the antivaccine movement in the United States: A focused examination of nonmedical exemptions in states and counties. PLoS Med. 2018, 15, 1–10. [Google Scholar]
- Lambert, P.H.; Siegrist, C.A. Science, medicine, and the future: Vaccines and vaccination. Br. Med. J. 1997, 315, 1595–1598. [Google Scholar] [CrossRef]
- Leo, O.; Cunningham, A.; Stern, P.L. Vaccine immunology. Perspect. Vaccinol. 2011, 1, 25–59. [Google Scholar] [CrossRef][Green Version]
- Siegrist, C.A. Vaccine immunology. Vaccines 2008, 5, 17–36. [Google Scholar]
- Bart, K.J.; Orenstein, W.A.; Hinman, A.R. The current status of immunization principles: Recommendations for use and adverse reactions. J. Allergy Clin. Immunol. 1987, 79, 296–315. [Google Scholar] [CrossRef]
- Edsall, G. Principles of active immunization. Annu. Rev. Med. 1966, 17, 39. [Google Scholar] [CrossRef]
- Grabenstein, J.D.; Nevin, R.L. Mass immunization programs: Principles and standards. In Mass Vaccination: Global Aspects—Progress and Obstacles; Springer: Berlin/Heidelberg, Germany, 2006; pp. 31–51. [Google Scholar]
- Biss, E. Sentimental Medicine: Why We Still Fear Vaccines. Harper’s Magazine. January 2013. Available online: https://harpers.org/archive/2013/01/sentimental-medicine/ (accessed on 20 January 2020).
- Gidengil, C.; Chen, C.; Parker, A.M.; Nowak, S.; Matthews, L. Beliefs around childhood vaccines in the United States: A systematic review. Vaccine 2019, 37, 6793–6802. [Google Scholar] [CrossRef]
- Sobo, E.J. What is herd immunity, and how does it relate to pediatric vaccination uptake? US parent perspectives. Soc. Sci. Med. 2016, 165, 187–195. [Google Scholar] [CrossRef]
- Bechtol, Z. Launching a community-wide flu vaccination plan. Fam. Pract. Manag. 2008, 15, 19. [Google Scholar] [PubMed]
- Ruderfer, D.; Krilov, L.R. Vaccine-preventable outbreaks: Still with us after all these years. Pediatric Ann. 2015, 44, e76–e81. [Google Scholar] [CrossRef] [PubMed]
- Dube, E.; Vivion, M.; MacDonald, N.E. Vaccine hesitancy, vaccine refusal and the anti-vaccine movement: Influence, impact and implications. Expert Rev. Vaccines 2015, 14, 99–117. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, R.M.; Targonski, P.V.; Poland, G.A. A taxonomy of reasoning flaws in the anti-vaccine movement. Vaccine 2007, 25, 3146–3152. [Google Scholar] [CrossRef]
- Poland, G.A.; Jacobson, R.M. Understanding those who do not understand: A brief review of the anti-vaccine movement. Vaccine 2001, 19, 2440–2445. [Google Scholar] [CrossRef]
- Calvert, N.; Cutts, F.; Miller, E.; Brown, D.; Munro, J. Measles in secondary school children: Implications for vaccination policy. Commun. Dis. Rep. Cdr Rev. 1990, 4, R70–R73. [Google Scholar]
- Hodge, J.G., Jr.; Gostin, L.O. School vaccination requirements: Historical, social, and legal perspectives. Ky. Law J. 2001, 90, 831. [Google Scholar]
- Hoffman, J. How anti-vaccine sentiment took hold in U.S. The New York Times, 24 September 2019; A1. [Google Scholar]
- Coleman-Brueckheimer, K.; Dein, S. Health care behaviors and beliefs in Hasidic Jewish populations: A systematic review of the literature. J. Relig. Health 2011, 50, 422–436. [Google Scholar] [CrossRef]
- Schmidt, K. Measles and Vaccination: A Resurrected Disease, A Conflicted Response. J. Christ. Nurs. 2019, 36, 214–221. [Google Scholar] [CrossRef]
- Tanne, J.H. US county bars unvaccinated children from public spaces amid measles emergency. BMJ Br. Med. J. 2019, 364. [Google Scholar] [CrossRef] [PubMed]
- Vielkind, J. Vaccination foes move to stop law. The Wall Street Journal, 15 August 2019; A8A. [Google Scholar]
- Otterman, S. Thousands of anti-vaccine parents face an ultimatum. The New York Times, 4 September 2019; A19. [Google Scholar]
- Pluviano, S.; Watt, C.; Della Sala, S. Misinformation lingers in memory: Failure of three pro-vaccination strategies. PLoS ONE 2017, 12, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Reuters. US Measles Outbreak Now Worst since 1994 after 60 New Cases Reported. The Guardian. 27 May 2019. Available online: https://www.theguardian.com/us-news/2019/may/27/us-measles-outbreak-worst-since-1994 (accessed on 10 January 2020).
- Eggertson, L. Lancet retracts 12-year-old article linking autism to MMR vaccines. Can. Med. Assoc. J. 2010, 182, E199. [Google Scholar] [CrossRef] [PubMed]
- Flaherty, D.K. The vaccine-autism connection: A public health crisis caused by unethical medical practices and fraudulent science. Ann. Pharmacother. 2011, 45, 1302–1304. [Google Scholar] [CrossRef] [PubMed]
- Godlee, F.; Smith, J.; Marcovitch, H. Wakefield’s article linking MMR vaccine and autism was fraudulent. Br. Med. J. 2011. [Google Scholar] [CrossRef]
- Wakefield, A.J.; Murch, S.H.; Anthony, A.; Linnell, J.; Casson, D.M.; Malik, M.; Valentine, A. Retracted: Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children. Lancet 1998, 351, 637–641. [Google Scholar] [CrossRef]
- Deer, B. Wakefield’s “autistic enterocolitis” under the microscope. Br. Med. J. 2010, 340, c1127. [Google Scholar] [CrossRef][Green Version]
- Deer, B. How the case against the MMR vaccine was fixed. Br. Med. J. 2011, 342, c5347. [Google Scholar] [CrossRef]
- Deer, B. How the vaccine crisis was meant to make money. Br. Med. J. 2011, 342, c5258. [Google Scholar] [CrossRef]
- Deer, B. The Lancet’s two days to bury bad news. Br. Med. J. 2011, 342, c7001. [Google Scholar] [CrossRef]
- Wakefield, A.J.; Murch, S.H.; Anthony, A. Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children (Retraction of 351, 637, 1998). Lancet 2010, 375, 445. [Google Scholar]
- Horton, R. A statement by the editors of The Lancet. Lancet 2004, 363, 820–821. [Google Scholar] [CrossRef]
- Murch, S.H.; Anthony, A.; Casson, D.H.; Malik, M.; Berelowitz, M.; Dhillon, A.P.; Walker-Smith, J.A. Retraction of an interpretation. Lancet 2004, 363, 750. [Google Scholar] [CrossRef]
- Kylstra, C. Celebrities and ‘vaccine hesitancy’. The New York Times, 24 August 2019; A23. [Google Scholar]
- Kata, A. A postmodern Pandora’s box: Anti-vaccination misinformation on the Internet. Vaccine 2010, 28, 1709–1716. [Google Scholar] [CrossRef]
- Tafuri, S.; Gallone, M.S.; Cappelli, M.G.; Martinelli, D.; Prato, R.; Germinario, C. Addressing the anti-vaccination movement and the role of HCWs. Vaccine 2014, 32, 4860–4865. [Google Scholar] [CrossRef]
- Myers, M.; Pineda, D. Misinformation about vaccines. In Vaccines for Biodefense and Emerging and Neglected Diseases; Barrett, A.D.T., Stanberry, L.R., Eds.; Elsevier: Amsterdam, The Netherlands, 2009; pp. 255–270. [Google Scholar]
- Zoon, K.C. Science and the Regulation of Biological Products; U.S. Food and Drug Administration: Washington, DC, USA, 2008. Available online: https://www.fda.gov/about-fda/histories-product-regulation/science-and-regulation-biological-products (accessed on 15 January 2020).
- Jansen, V.A.; Stollenwerk, N.; Jensen, H.J.; Ramsay, M.E.; Edmunds, W.J.; Rhodes, C.J. Measles outbreaks in a population with declining vaccine uptake. Science 2003, 301, 804. [Google Scholar] [CrossRef]
- Lernout, T.; Kissling, E.; Hutse, V.; Top, G. Clusters of measles cases in Jewish orthodox communities in Antwerp, epidemiologically linked to the United Kingdom: A preliminary report. Wkly. Releases 2007, 12, 3308. [Google Scholar] [CrossRef]
- Richard, J.L.; Spicher, V.M. Ongoing measles outbreak in Switzerland: Results from November 2006 to July 2007. Wkly. Releases 2007, 12, 3241. [Google Scholar] [CrossRef]
- Wichmann, O.; Hellenbrand, W.; Sagebiel, D.; Santibanez, S.; Ahlemeyer, G.; Vogt, G.; van Treeck, U. Large measles outbreak at a German public school, 2006. Pediatric Infect. Dis. J. 2007, 26, 782–786. [Google Scholar] [CrossRef] [PubMed]
- Gust, D.A.; Strine, T.W.; Maurice, E.; Smith, P.; Yusuf, H.; Wilkinson, M.; Schwartz, B. Under immunization among children: Effects of vaccine safety concerns on immunization status. Pediatrics 2004, 114, e16–e22. [Google Scholar] [CrossRef]
- Gust, D.A.; Kennedy, A.; Shui, I.; Smith, P.J.; Nowak, G.; Pickering, L.K. Parent attitudes toward immunizations and healthcare providers: The role of information. Am. J. Prev. Med. 2005, 29, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Shelby, A.; Ernst, K. Story and science: How providers and parents can utilize storytelling to combat anti-vaccine misinformation. Hum. Vaccines Immunother. 2013, 9, 1795–1801. [Google Scholar] [CrossRef] [PubMed]
- Mayer, M.; Till, J.E. The Internet: A modern Pandora’s box? Qual. Life Res. 1996, 5, 568–571. [Google Scholar] [CrossRef] [PubMed]
- Bean, S.J. Emerging and continuing trends in vaccine opposition website content. Vaccine 1996, 29, 1874–1880. [Google Scholar] [CrossRef]
- Kata, A. Anti-vaccine activists, Web 2.0, and the postmodern paradigm–An overview of tactics and tropes used online by the anti-vaccination movement. Vaccine 2012, 30, 3778–3789. [Google Scholar] [CrossRef]
- Dunn, A.G.; Leask, J.; Zhou, X.; Mandl, K.D.; Coiera, E. Associations between exposure to and expression of negative opinions about human papillomavirus vaccines on social media: An observational study. J. Med. Internet Res. 2015, 17, e144. [Google Scholar] [CrossRef]
- Christakis, N.A.; Fowler, J.H. The spread of obesity in a large social network over 32 years. N. Engl. J. Med. 2007, 357, 370–379. [Google Scholar] [CrossRef]
- Christakis, N.A.; Fowler, J.H. The collective dynamics of smoking in a large social network. N. Engl. J. Med. 2008, 358, 2249–2258. [Google Scholar] [CrossRef]
- Greenwood, S.; Perrin, A.; Duggan, M. Social Media Update 2016; Pew Research Center: Washington, DC, USA, 2016; Available online: www.pewinternet.org/2016/11/11/social-media-update-2016/ (accessed on 20 January 2020).
- Centola, D. The spread of behavior in an online social network experiment. Science 2010, 329, 1194–1197. [Google Scholar] [CrossRef] [PubMed]
- Pang, B.; Lee, L. A sentimental education: Sentiment analysis using subjectivity summarization based on minimum cuts. In Proceedings of the 42nd annual meeting on Association for Computational Linguistics, Barcelona, Spain, 21–26 July 2004; p. 271. [Google Scholar]
- Turney, P.D. Thumbs up or thumbs down? Semantic orientation applied to unsupervised classification of reviews. In Proceedings of the 40th Annual Meeting on Association for Computational Linguistics, Philadelphia, PA, USA, 7–12 July 2002; pp. 417–424. [Google Scholar]
- Hu, M.; Liu, B. Mining and summarizing customer reviews. In Proceedings of the tenth ACM SIGKDD International Conference on Knowledge Discovery and Data Mining, Seattle, WA, USA, 22–25 August 2004; pp. 168–177. [Google Scholar]
- Kim, S.M.; Hovy, E. Determining the sentiment of opinions. In Proceedings of the 20th International Conference on Computational Linguistics, Stroudsburg, PA, USA, 23–27 August 2004; p. 1367. [Google Scholar]
- Wilson, T.; Hoffmann, P.; Somasundaran, S.; Kessler, J.; Wiebe, J.; Choi, Y.; Patwardhan, S. OpinionFinder: A system for subjectivity analysis. In Proceedings of the HLT/EMNLP 2005 Interactive Demonstrations, Vancouver, BC, Canada, 7 October 2005; pp. 34–35. [Google Scholar]
- Agarwal, A.; Biadsy, F.; Mckeown, K.R. Contextual phrase-level polarity analysis using lexical affect scoring and syntactic n-grams. In Proceedings of the 12th Conference of the European Chapter of the Association for Computational Linguistics, Athens, Greece, 30 March–2 April 2009; pp. 24–32. [Google Scholar]
- Du, J.; Xu, J.; Song, H.Y.; Tao, C. Leveraging machine learning-based approaches to assess human papillomavirus vaccination sentiment trends with Twitter data. BMC Med. Inf. Decis. Mak. 2017, 17, 69. [Google Scholar] [CrossRef] [PubMed]
- Raghupathi, V.; Zhou, Y.; Raghupathi, W. Legal Decision Support: Exploring Big Data Analytics Approach to Modeling Pharma Patent Validity Cases. IEEE Access. 2018, 6, 41518–41528. [Google Scholar] [CrossRef]
- Raghupathi, V.; Zhou, Y.; Raghupathi, W. Exploring Big Data Analytic Approach to Social Media Cancer Blog Analysis. Int. J. Healthc. Inf. Syst. Inform. 2019, 14, 1–20. [Google Scholar] [CrossRef]
- Glanz, J.M.; Wagner, N.M.; Narwaney, K.J.; Kraus, C.R.; Shoup, J.A.; Xu, S.; Daley, M.F. Web-based social media intervention to increase vaccine acceptance: A randomized controlled trial. Pediatrics 2017, 140, e20171117. [Google Scholar] [CrossRef]
- Gu, Z.; Badger, P.; Su, J.; Zhang, E.; Li, X.; Zhang, L. A vaccine crisis in the era of social media. Natl. Sci. Rev. 2018, 5, 8–10. [Google Scholar] [CrossRef]
- Schiff, A. The Letter to Amazon CEO Regarding Anti-Vaccine Misinformation. Available online: https://schiff.house.gov/news/press-releases/schiff-sends-letter-to-amazon-ceo-regarding-anti-vaccine-misinformation (accessed on 12 January 2020).
- Del Vicario, M.; Bessi, A.; Zollo, F.; Petroni, F.; Scala, A.; Caldarelli, G.; Quattrociocchi, W. The spreading of misinformation online. Proc. Natl. Acad. Sci. USA 2016, 113, 554–559. [Google Scholar] [CrossRef]
- Dredze, M.; Broniatowski, D.A.; Hilyard, K.M. Zika vaccine misconception: A social media analysis. Vaccine 2016, 34, 3441. [Google Scholar] [CrossRef]
- Dredze, M.; Broniatowski, D.A.; Smith, M.C.; Hilyard, K.M. Understanding vaccine refusal: Why we need social media now. Am. J. Prev. Med. 2016, 50, 550–552. [Google Scholar] [CrossRef]
- Kang, G.J.; Ewing-Nelson, S.R.; Mackey, L.; Schlitt, J.T.; Marathe, A.; Abbas, K.M.; Swarap, S. Semantic network analysis of vaccine sentiment in online social media. Vaccine 2017, 35, 3621–3638. [Google Scholar] [CrossRef]
- Raghunathan, R.; Trope, Y. Walking the tightrope between feeling good and being accurate: Mood as a resource in processing persuasive messages. J. Personal. Soc. Psychol. 2017, 83, 510–525. [Google Scholar] [CrossRef]
- Xu, Z.; Guo, H. Using Text Mining to Compare Online Pro- and Anti-Vaccine Headlines: Word Usage, Sentiments, and Online Popularity. Commun. Stud. 2017, 69, 103–122. [Google Scholar] [CrossRef]

© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Raghupathi, V.; Ren, J.; Raghupathi, W. Studying Public Perception about Vaccination: A Sentiment Analysis of Tweets. Int. J. Environ. Res. Public Health 2020, 17, 3464. https://doi.org/10.3390/ijerph17103464
Raghupathi V, Ren J, Raghupathi W. Studying Public Perception about Vaccination: A Sentiment Analysis of Tweets. International Journal of Environmental Research and Public Health. 2020; 17(10):3464. https://doi.org/10.3390/ijerph17103464
Chicago/Turabian StyleRaghupathi, Viju, Jie Ren, and Wullianallur Raghupathi. 2020. "Studying Public Perception about Vaccination: A Sentiment Analysis of Tweets" International Journal of Environmental Research and Public Health 17, no. 10: 3464. https://doi.org/10.3390/ijerph17103464
APA StyleRaghupathi, V., Ren, J., & Raghupathi, W. (2020). Studying Public Perception about Vaccination: A Sentiment Analysis of Tweets. International Journal of Environmental Research and Public Health, 17(10), 3464. https://doi.org/10.3390/ijerph17103464




