Patient-Related Complexity of Care in Healthcare Organizations: A Management and Evaluation Model
Abstract
1. Introduction
- Definition of differentiated areas, based on the assistance modalities;
- Structuring by caring complexity;
- Gradual overcoming of the articulation by Operating Units.
- Operating theatre re-modulation. The hospitalization duration considered as a focal point has allowed introducing a new way to classify the hospitalizations. The average hospitalization duration can be used as an indicator of complexity, in order to reserve a part of the interventions and hospital beds for the cases resolvable within four days of the intervention (week surgery) and allowing its closure on the weekend [7];
- Modular-care model. It was born in a nursing team, in which the key figure is the nurse who plans, implements and supervises the care of assigned patients, collaborating with other professional healthcare figures [8];
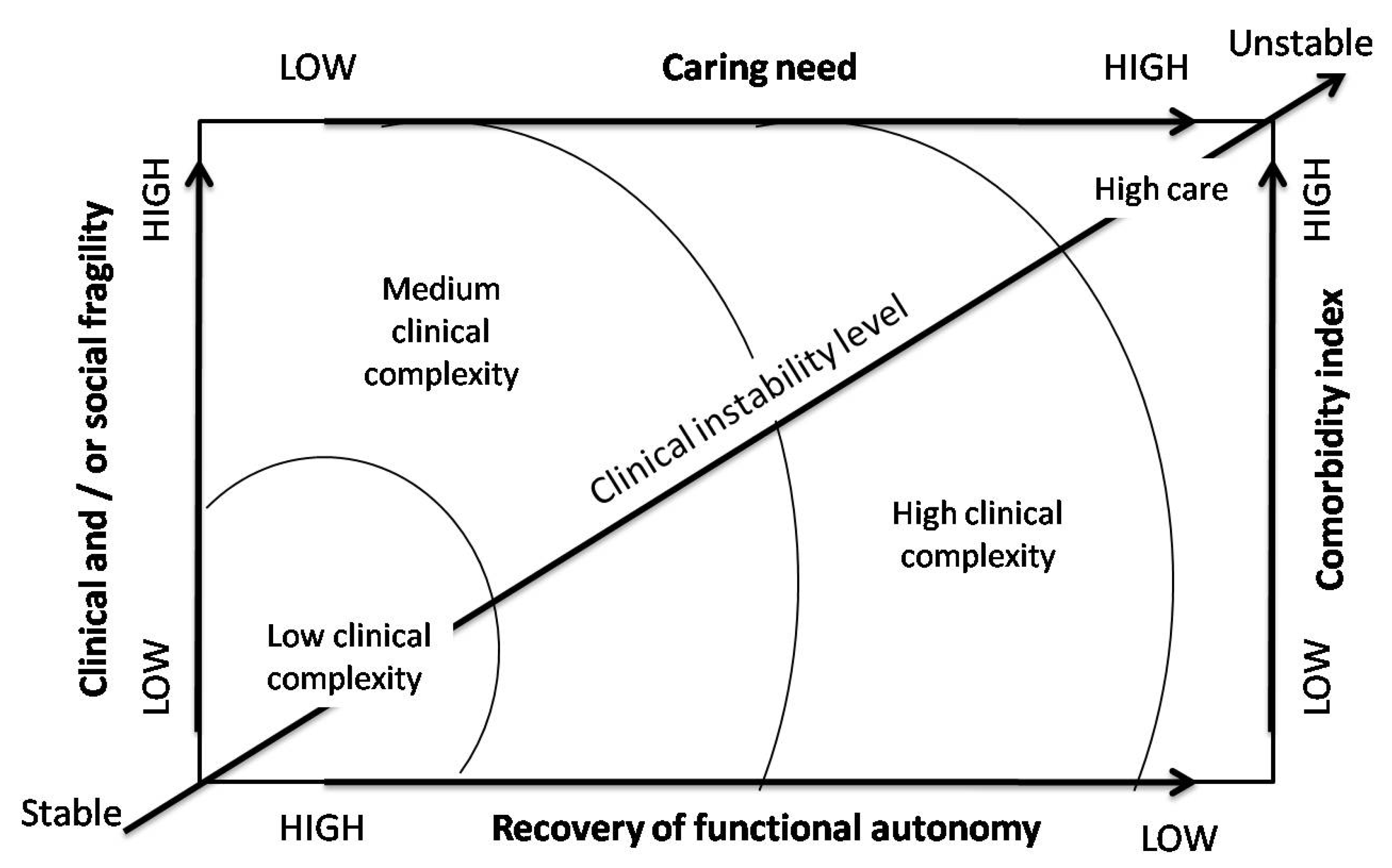
- Care complexity model. It aimed at responding to the need to increase both the complexity of patients with high degrees of clinical instability level and the increase in the care demand due to the significant presence of elderly patients with comorbidities [9].
- A new work organization allowing to take charge of the patient and his/her care path efficiently through the development of the digital medical record;
- A new operating unit organization, characterized by greater flexibility obtained through the maximum integration of skills, adequate levels of care and optimized volumes of activity;
- A new hospital flow organization envisaging an emergency classification and an improved flow organization, by complexity and care duration.
“The set of interventions carried out by nursing care and expressed in terms of the intensity and quantity of activities of the healthcare professional.”
“Assign the patient to the most appropriate operating unit considering his care needs related not only to the hospitalization type but also to his clinical condition and care dependence.”
- Sub-intensive;
- High care;
- Medium care (ordinary hospitalization and short-cycle hospitalization);
- Low care (rehabilitation, post-acute care).
Methodologies for the Evaluation of Clinical Care Complexity: National and International Review
- Documentation’s identification of the activities carried out;
- Patient’s profile identification;
- Assistance indicators’ identification.
- Criterion based on the indications contained in the assistance plans, on the documentation of the activities carried out and on the quantification of the need for assistance in terms of "time" (for example, Project Research of Nursing);
- Criterion based on the patient’s global need (for example, the Swiss Method);
- Criterion based on care dependency and indicators (for example, Patient Intensity for Nursing Index method).
2. Rationale of the Study
3. Objectives
- Verify the validity and reliability of the instruments chosen for measuring clinical severity and care dependence;
- Introduce the routine use of care intensity assessment tools to guide patient allocation.
4. Materials and Methods
- Training meetings for the drafting and implementation of the NEWS form in clinical care practice;
- Systematic monitoring of the clinical instability level (NEWS) and care dependency (ICD);
- Retrospective analysis of public records relating to hospitalizations between 15 January and 15 February 2020.
4.1. Study Design
4.2. Inclusion Criteria
4.3. Evaluation Tools
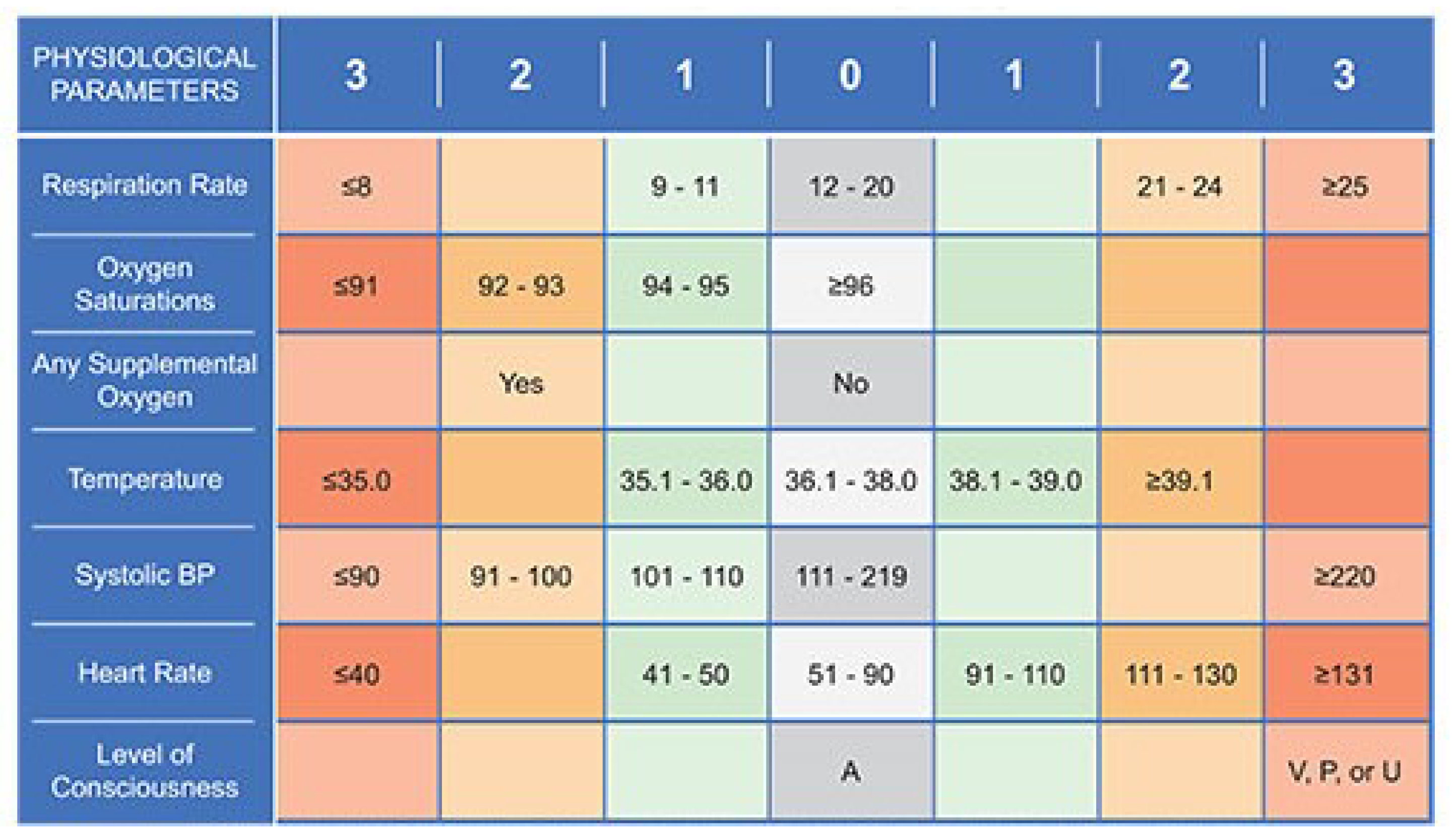
4.3.1. Clinical Instability Level (NEWS)
4.3.2. Care Dependence (mICD)
- High care dependence, range score 24–32;
- Average care dependence, range score 15–23;
- Low care dependence, range score 8–14;
4.4. Analysis
5. Results
5.1. Study Population
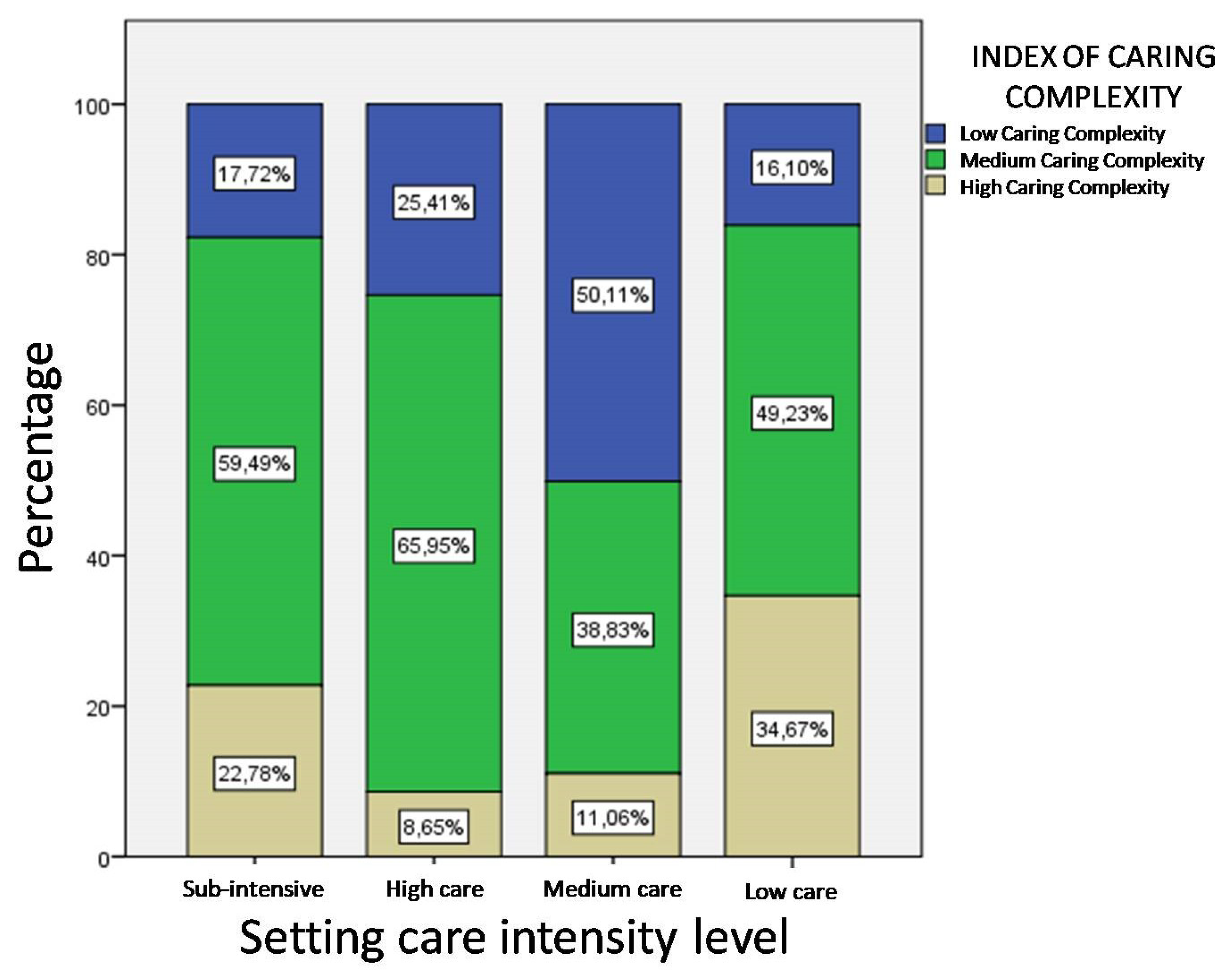
5.2. Level of Care Complexity by Settings
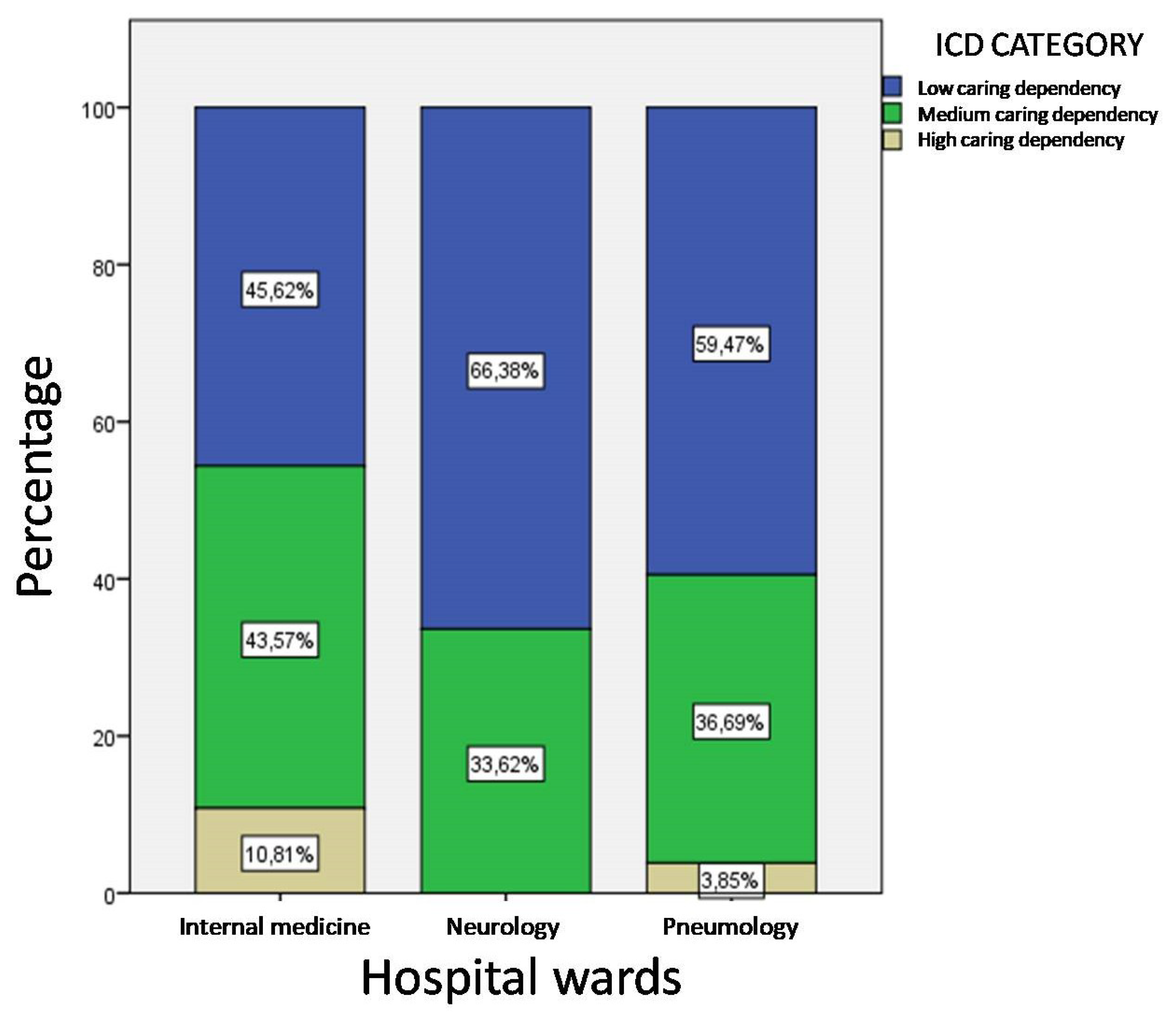
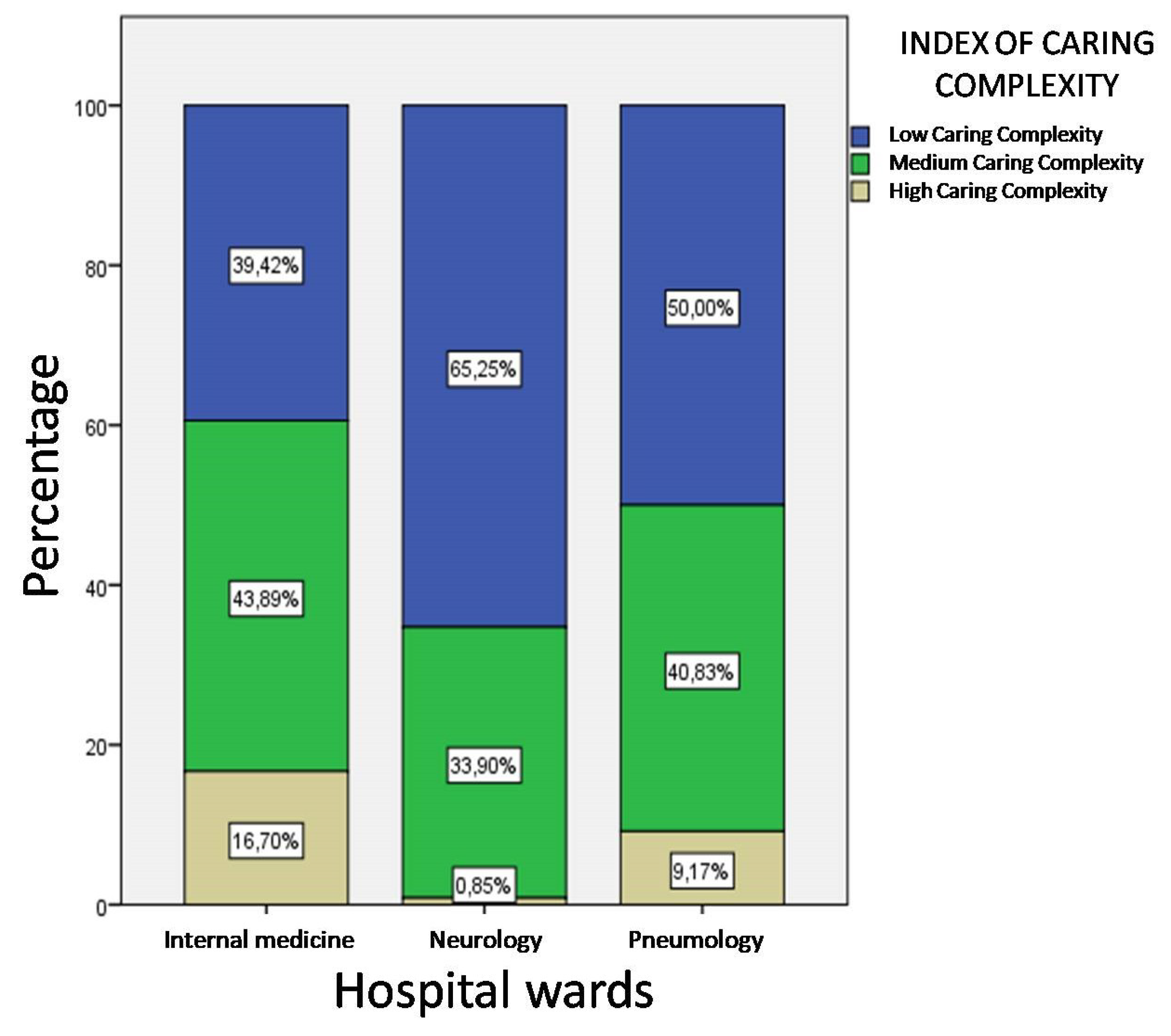
5.3. Level of Care Complexity by Hospital Wards
6. Discussion
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Maniatopoulos, G.; Hunter, D.J.; Erskine, J.; Hudson, B. Implementing the New Care Models in the NHS: Reconfiguring the Multilevel Nature of Context to Make It Happen. In Transitions and Boundaries in the Coordination and Reform of Health Services; Springer: Berlin/Heidelberg, Germany, 2020; pp. 3–27. [Google Scholar]
- Durán, A.; Saltman, R.B. Hospital Governance. In Understanding Hospitals in Changing Health Systems; Springer: Berlin/Heidelberg, Germany, 2020; pp. 25–47. [Google Scholar]
- Horvat, A.; Filipovic, J. Healthcare system quality indicators: The complexity perspective. Total Qual. Manag. Bus. Excell. 2020, 31, 161–177. [Google Scholar] [CrossRef]
- Cavalieri, M.; Ferrante, L. Convergence, decentralization and spatial effects: An analysis of Italian regional health outcomes. Health Policy 2020, 124, 164–173. [Google Scholar] [CrossRef] [PubMed]
- Bordogna, M.T. Regional Health Systems and non-conventional medicine: The situation in Italy. EPMA J. 2011, 2, 411–423. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Croce, D.; Sebastiano, A.; Mazzei, B. Innovazioni nella progettazione degli assetti organizzativi in sanità. Sanità Pubblica Priv. 2007, 1, 26–31. [Google Scholar]
- Guerriero, F.; Guido, R. Operational research in the management of the operating theatre: A survey. Health Care Manag. Sci. 2011, 14, 89–114. [Google Scholar] [CrossRef]
- Seago, J.A. Evaluation of a hospital work redesign: Patient-focused care. JONA J. Nurs. Adm. 1999, 29, 31–38. [Google Scholar] [CrossRef]
- Tonelli, M.; Wiebe, N.; Manns, B.J.; Klarenbach, S.W.; James, M.T.; Ravani, P.; Pannu, N.; Himmelfarb, J.; Hemmelgarn, B.R. Comparison of the complexity of patients seen by different medical subspecialists in a universal health care system. JAMA Netw. Open 2018, 1, e184852. [Google Scholar] [CrossRef]
- Buchanan, D.A.; Fitzgerald, L.; Ketley, D. The Sustainability and Spread of Organizational Change: Modernizing Healthcare; Routledge: Abingdon, UK, 2006. [Google Scholar]
- Pakdil, F.; Harwood, T.N.; Isin, F.B. Implementing Lean Principles in the Healthcare Industry: A Theoretical and Practical Overview. In Delivering Superior Health and Wellness Management with IoT and Analytics; Springer: Berlin/Heidelberg, Germany, 2020; pp. 383–413. [Google Scholar]
- Moiset, C.; Vanzetta, M.; Vallicella, F. Misurare l’Assistenza: Un Modello si Sistema Informativo Della Performance Infermieristica; McGraw-Hill: New York, NY, USA, 2003. [Google Scholar]
- Moroni, P.; Colnaghi, E.; Bonfanti, M.; Casartelli, L.; Croce, D.; Foglia, E.; Porazzi, E. Nuovi “modelli modulari di cura”: L’intensità di cura a dimensione variabile. Il caso dell’Azienda ospedaliera di Desio e Vimercate. Sanità Pubblica Priv. 2011, 3, 46–57. [Google Scholar]
- Briani, S.; Cortesi, E. L’ospedale per intensità di cure: Aspetti teorici e problemi aperti. Ig. Sanità Pubblica 2007, 63, 19. [Google Scholar]
- Heath, I.; Rubinstein, A.; Stange, K.C.; Van Driel, M.L. Quality in primary health care: A multidimensional approach to complexity. BMJ 2009, 338, b1242. [Google Scholar] [CrossRef]
- Alessandri, M.; Bartolomei, C.; Bernardini, M.; Landini, G.; Laureano, R.; Lombardo, G. Medicina Interna e nuova organizzazione ospedaliera: La proposta della FADOI Toscana. Ital. J. Med. 2007, 1, 65–69. [Google Scholar]
- Nardi, R.; Arienti, V.; Nozzoli, C.; Mazzone, A. Organizzazione dell’ospedale per intensità di cure: Gli errori da evitare. Ital. J. Med. 2012, 6, 1–13. [Google Scholar] [CrossRef][Green Version]
- Cavaliere, B. Misurare la Complessità Assistenziale: Metodi eStrumenti per le Professioni Sanitarie; Maggioli: Rimini, Italy, 2009. [Google Scholar]
- Zúñiga, F.; Ausserhofer, D.; Hamers, J.P.; Engberg, S.; Simon, M.; Schwendimann, R. The relationship of staffing and work environment with implicit rationing of nursing care in Swiss nursing homes—A cross-sectional study. Int. J. Nurs. Stud. 2015, 52, 1463–1474. [Google Scholar] [CrossRef] [PubMed]
- Prescott, P.A.; Ryan, J.W.; Soeken, K.L.; Castorr, A.H.; Thompson, K.O.; Phillips, C.Y. The patient intensity for nursing index: A validity assessment. Res. Nurs. Health 1991, 14, 213–221. [Google Scholar] [CrossRef] [PubMed]
- Silvestro, A. La Complessità Assistenziale: Concettualizzazione, Modello di Analisi e Metodologia Applicativa; McGraw-Hill: New York, NY, USA, 2009. [Google Scholar]
- Moiset, C.; Vanzetta, M.; Vallicella, F. Misurare l’Assistenza: Il SIPI: Dalla Progettazione All’Attuazione; McGraw Hill: New York, NY, USA, 2009. [Google Scholar]
- Safford, M.M.; Allison, J.J.; Kiefe, C.I. Patient complexity: More than comorbidity. The vector model of complexity. J. Gen. Intern. Med. 2007, 22, 382–390. [Google Scholar] [CrossRef]
- Subbe, C.P.; Kruger, M.; Rutherford, P.; Gemmel, L. Validation of a modified Early Warning Score in medical admissions. QJM 2001, 94, 521–526. [Google Scholar] [CrossRef]
- Lega, F.; Mauri, C.; Prenestini, A. L’Ospedale tra Presente e Futuro: Analisi, Diagnosi e Linee di Cambiamento per il Sistema Ospedaliero Italiano; EGEA Spa: Milano, Italy, 2011. [Google Scholar]
- Alam, N.; Vegting, I.L.; Houben, E.; van Berkel, B.; Vaughan, L.; Kramer, M.H.; Nanayakkara, P.W. Exploring the performance of the National Early Warning Score (NEWS) in a European emergency department. Resuscitation 2015, 90, 111–115. [Google Scholar] [CrossRef]
- Smith, G.B.; Prytherch, D.R.; Meredith, P.; Schmidt, P.E.; Featherstone, P.I. The ability of the National Early Warning Score (NEWS) to discriminate patients at risk of early cardiac arrest, unanticipated intensive care unit admission, and death. Resuscitation 2013, 84, 465–470. [Google Scholar] [CrossRef]
- Kolic, I.; Crane, S.; McCartney, S.; Perkins, Z.; Taylor, A. Factors affecting response to national early warning score (NEWS). Resuscitation 2015, 90, 85–90. [Google Scholar] [CrossRef]
- Sbiti-Rohr, D.; Kutz, A.; Christ-Crain, M.; Thomann, R.; Zimmerli, W.; Hoess, C.; Henzen, C.; Mueller, B.; Schuetz, P. The National Early Warning Score (NEWS) for outcome prediction in emergency department patients with community-acquired pneumonia: Results from a 6-year prospective cohort study. BMJ Open 2016, 6, e011021. [Google Scholar] [CrossRef]
- Dijkstra, A.; Buist, G.; Moorer, P.; Dassen, T. Construct validity of the nursing care dependency scale. J. Clin. Nurs. 1999, 8, 380–388. [Google Scholar] [CrossRef] [PubMed]
- Dijkstra, A.; Tiesinga, L.J.; Plantinga, L.; Veltman, G.; Dassen, T.W. Diagnostic accuracy of the care dependency scale. J. Adv. Nurs. 2005, 50, 410–416. [Google Scholar] [CrossRef] [PubMed]
- Mathieu, G. Triage di Corridoio (Tri-Co): Strumento utile per migliorare la qualità dell’assistenza Triage in the Corridor (Tri-Co): A useful tool for improving the quality of care. Ital. J. Med. 2007, 1, 3–5. [Google Scholar] [CrossRef]
- Jones, M. NEWSDIG: The national early warning score development and implementation group. Clin. Med. 2012, 12, 501. [Google Scholar] [CrossRef] [PubMed]
- Piu, F. La documentazione infermieristica come strumento di misurazione della complessità assistenziale e di pianificazione dell’assistenza. Manag. Inferm. 2005, 2, 36–42. [Google Scholar]
- Royston, P. Approximating the Shapiro-Wilk W-test for non-normality. Stat. Comput. 1992, 2, 117–119. [Google Scholar] [CrossRef]
- Spagnolli, W.; Peterlana, D.; Dorigoni, S.; Rigoni, M.; Torri, E.; Nollo, G. Intensity of medical care in internal medicine: Impact on outcomes from a trend analysis over six years. Ital. J. Med. 2019, 13, 95–102. [Google Scholar] [CrossRef]
- Ranhoff, A.H.; Rozzini, R.; Sabatini, T.; Cassinadri, A.; Boffelli, S.; Ferri, M.; Travaglini, N.; Ricci, A.; Morandi, A.; Trabucchi, M. Subintensive care unit for the elderly: A new model of care for critically ill frail elderly medical patients. Intern. Emerg. Med. 2006, 1, 197–203. [Google Scholar] [CrossRef]
- Micieli, G.; De Falco, F.A.; Consoli, D.; Inzitari, D.; Sterzi, R.; Tedeschi, G.; Toni, D. The role of emergency neurology in Italy: Outcome of a consensus meeting for a intersociety position. Neurol. Sci. 2012, 33, 297–304. [Google Scholar] [CrossRef]

| mICD | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Care Levels | Nutrition/Hydration | Elimination | Hygiene and Comfort | Mobilization | Diagnostic Procedures | Therapeutic Procedures | Sensory Perception | Skin Integrity | |
| 1 | Independent | Independent | Independent | Independent | Monitoring once a day | Oral therapy only or no therapy | Patient alert and oriented (no sedatives) | Patient with low risk of pressure ulcers (PU) (Braden > 16). Absence PU | |
| 2 | Help nutrition | Bladder/condom catheter | Intimate hygiene in bed but independent in the use of services | Walk with help | Vital parameters’ monitoring once per shift | Oral, i.m., e.v. | Occasional temporal-space disorientation (day and night sedatives) | Patient at risk of PU (Braden ≤ 16) not bedridden with mobilization program | |
| 3 | Fed patient | Occasional urinary and fecal incontinence | Hygiene in bed with patient help | Armchair mobilization | Vital parameters’ monitoring more than once per shift | Central Venous Catheter with non-continuous infusion | Constant disorientation temporal-space (sedatives day and night) | Bedridden patient with mobilization program and/or presence of PU up to the 2nd degree | |
| 4 | Total parental nutrition | Permanent urinary and fecal incontinence | Hygiene in bed without patient’s help | Bedridden | Constant vital parameters’ monitoring | Central Venous Catheter continuous/infusion 24 h | Sleepy state, coma or severe state of agitation (delirium) | Bedridden patient with mobilization program and/or presence of PU >2nd degree | |
| ICC | |||
|---|---|---|---|
| NEWS | ICD 8–14 0 | ICD 15–23 1 | ICD 24–32 2 |
| NEWS 0–4 0 | Low | Medium | High |
| NEWS 5–6 1 | Medium | Medium | High |
| NEWS ≥7 2 | High | High | High |
| Age | ||||
|---|---|---|---|---|
| Hospital Wards | Average | N | Std. Deviation | 95% CI |
| Internal medicine | 80.23 | 349 | 12.250 | 79.47–80.52 |
| Neurology | 71.95 | 39 | 13.594 | 71.5–72.33 |
| Pneumology | 75.27 | 62 | 13.823 | 75.16–75.68 |
| Total | 78.83 | 450 | 12.856 | 78.23–79.11 |
| Age | ||||
|---|---|---|---|---|
| Setting Care Complexity Level | Average | N | Std. Deviation | 95% CI |
| Sub-intensive | 72 | 17 | 15.576 | 71.84–72.16 |
| High care | 80.39 | 23 | 11.696 | 80.2–80.56 |
| Medium care | 78.69 | 361 | 12.911 | 78.4–78.78 |
| Low care | 81.47 | 49 | 11.288 | 81.32–81.91 |
| Total | 78.83 | 450 | 12.856 | 78.51–79.12 |
| Sample Characteristics | Hospital Wards | Significance of Chi-Square | ||||||
|---|---|---|---|---|---|---|---|---|
| Internal Medicine | Neurology | Pneumology | ||||||
| N | % | N | % | N | % | |||
| Gender | Male | 173 | 49.6 | 13 | 33.3 | 30 | 48.4 | p < 0.1 |
| Female | 176 | 50.4 | 26 | 66.7 | 32 | 51.6 | ||
| Age classes | <60 | 24 | 6.9 | 9 | 23.1 | 6 | 9.7 | p < 0.001 |
| 61–70 | 41 | 11.7 | 6 | 15.4 | 6 | 9.7 | ||
| 71–80 | 81 | 23.2 | 13 | 33.3 | 29 | 46.8 | ||
| 81–90 | 139 | 39.8 | 10 | 25.6 | 15 | 24.2 | ||
| >90 | 64 | 18.3 | 1 | 2.6 | 6 | 9.7 | ||
| Setting care complexity level | Sub-intensive | 11 | 3.2 | 1 | 2.6 | 5 | 8.1 | p < 0.05 |
| High care | 10 | 2.9 | 5 | 12.8 | 8 | 12.9 | ||
| Medium care | 280 | 80.2 | 33 | 84.6 | 49 | 79 | ||
| Low care | 48 | 13.8 | 0 | 0 | 0 | 0 | ||
| Hospitalization days | 1–3 | 75 | 21.5 | 0 | 0 | 14 | 22.6 | p < 0.001 |
| 4–9 | 194 | 55.6 | 24 | 61.5 | 39 | 62.9 | ||
| 10–15 | 62 | 17.8 | 6 | 15.4 | 7 | 11.3 | ||
| >15 | 18 | 5.2 | 9 | 23.1 | 2 | 3.2 | ||
| Health Outcome | Hospital Wards | Significance of Chi-Square | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Internal Medicine | Neurology | Pneumology | Total | ||||||
| N | % | N | % | N | % | N | % | ||
| Ordinary discharge | 239 | 68.5 | 28 | 71.8 | 50 | 80.6 | 317 | 70.4 | p < 0.001 |
| Transfer to another ward | 7 | 2 | 2 | 5.1 | 1 | 1.6 | 10 | 2.2 | |
| Death | 40 | 11.50 | 0 | 0.00 | 1 | 1.60 | 41 | 9.10 | |
| Re-entry | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | |
| Other institute | 6 | 1.7 | 4 | 10.30 | 0 | 0.00 | 10 | 2.20 | |
| Hospice | 2 | 0.6 | 2 | 5.10 | 1 | 1.60 | 5 | 1.10 | |
| Integrated home care | 3 | 0.9 | 0 | 0.00 | 0 | 0.00 | 3 | 0.7 | |
| Transfer to higher care level | 11 | 3.2 | 0 | 0.00 | 2 | 3.2 | 13 | 2.9 | |
| Transfer to lower care level | 41 | 11.7 | 3 | 7.7 | 7 | 11.3 | 51 | 11.3 | |
| Total | 369 | 100.00 | 39 | 100.00 | 62 | 100.00 | 450 | 100.00 | |
| Setting Care Complexity Level | Clinical Instability Level (NEWS) | Significance of Chi-Square | |||||
|---|---|---|---|---|---|---|---|
| Stable Patient (Score 1–4) | Unstable Patient (Score 5–6) | Critical Conditions (Score ≥ 7) | |||||
| N. | % | N. | % | N. | % | ||
| Sub-intensive | 31 | 39.2 | 35 | 44.3 | 13 | 17.6 | p < 0.05 |
| High care | 123 | 66.5 | 55 | 29.7 | 7 | 3.8 | |
| Medium care | 1888 | 82.2 | 269 | 11.7 | 140 | 6.1 | |
| Low care | 205 | 63.5 | 67 | 19.5 | 55 | 16.8 | |
| Total | 2247 | 77.9 | 422 | 14.6 | 215 | 7.5 | |
| Setting Care Complexity Level | Care Dependence Levels (mICD) | Significance of Chi-Square | |||||
|---|---|---|---|---|---|---|---|
| Low (Score 8–16) | Medium (Score 17–25) | High (Score ≥ 26) | |||||
| N. | % | N. | % | N. | % | ||
| Sub-intensive | 30 | 38.0 | 44 | 55.7 | 5 | 6.3 | p < 0.05 |
| High care | 59 | 31.9 | 117 | 63.2 | 9 | 4.9 | |
| Medium care | 1289 | 56.1 | 855 | 37.2 | 153 | 6.7 | |
| Low care | 58 | 18.0 | 182 | 56.3 | 83 | 25.7 | |
| Total | 1436 | 49.8 | 1198 | 41.5 | 250 | 8.7 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salvatore, F.P.; Fanelli, S. Patient-Related Complexity of Care in Healthcare Organizations: A Management and Evaluation Model. Int. J. Environ. Res. Public Health 2020, 17, 3463. https://doi.org/10.3390/ijerph17103463
Salvatore FP, Fanelli S. Patient-Related Complexity of Care in Healthcare Organizations: A Management and Evaluation Model. International Journal of Environmental Research and Public Health. 2020; 17(10):3463. https://doi.org/10.3390/ijerph17103463
Chicago/Turabian StyleSalvatore, Fiorella Pia, and Simone Fanelli. 2020. "Patient-Related Complexity of Care in Healthcare Organizations: A Management and Evaluation Model" International Journal of Environmental Research and Public Health 17, no. 10: 3463. https://doi.org/10.3390/ijerph17103463
APA StyleSalvatore, F. P., & Fanelli, S. (2020). Patient-Related Complexity of Care in Healthcare Organizations: A Management and Evaluation Model. International Journal of Environmental Research and Public Health, 17(10), 3463. https://doi.org/10.3390/ijerph17103463






