How Are Wearable Activity Trackers Adopted in Older Adults? Comparison between Subjective Adoption Attitudes and Physical Activity Performance
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Anthropometric Data
2.2. Activity Tracker Adoption Survey Instrument
2.3. Activity Tracker Used in This Study
2.4. Experiment Procedure
2.5. Data Analysis
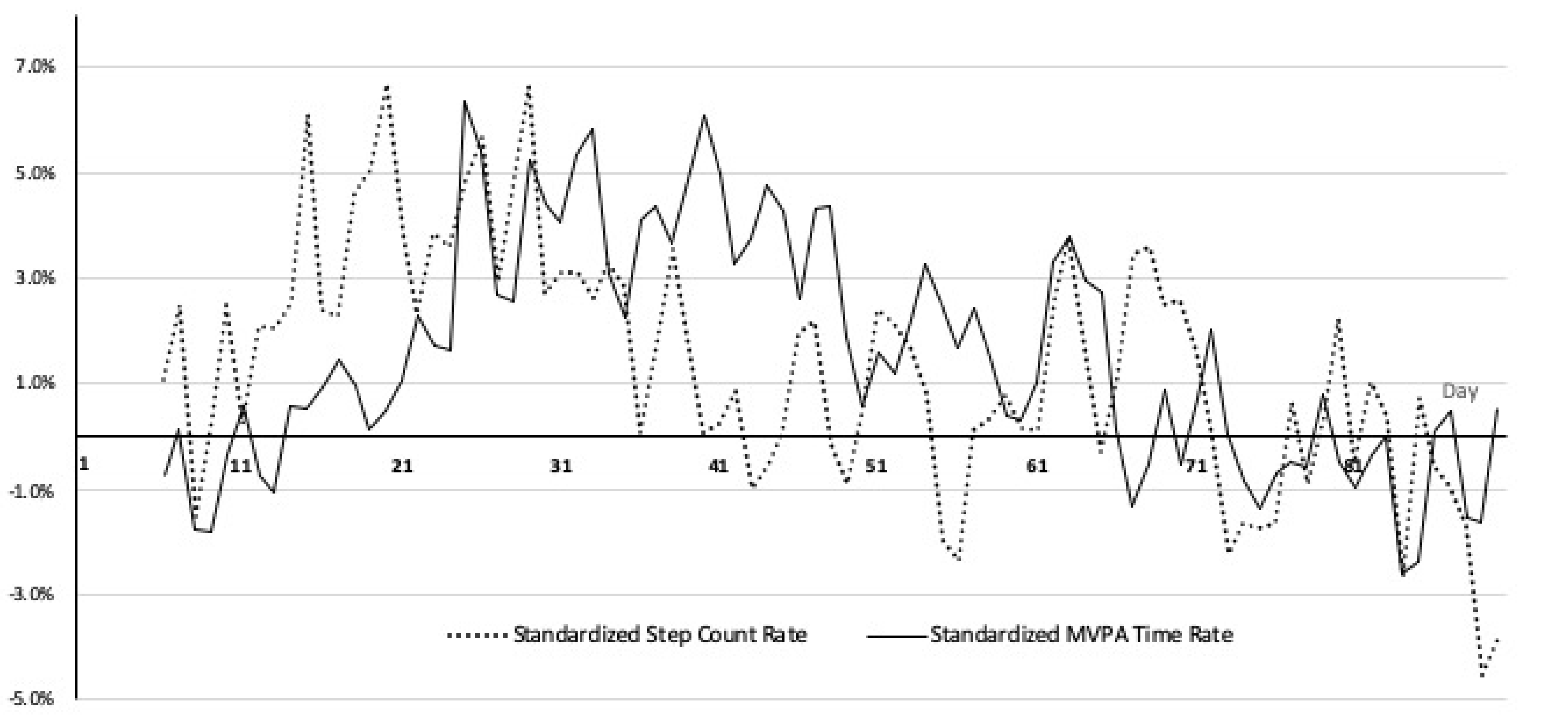
participant)/average step count per participant
participant)/average MVPA time per participant
3. Results
3.1. Demographic Data
3.2. Activity Tracker Adoption Attitudes Survey
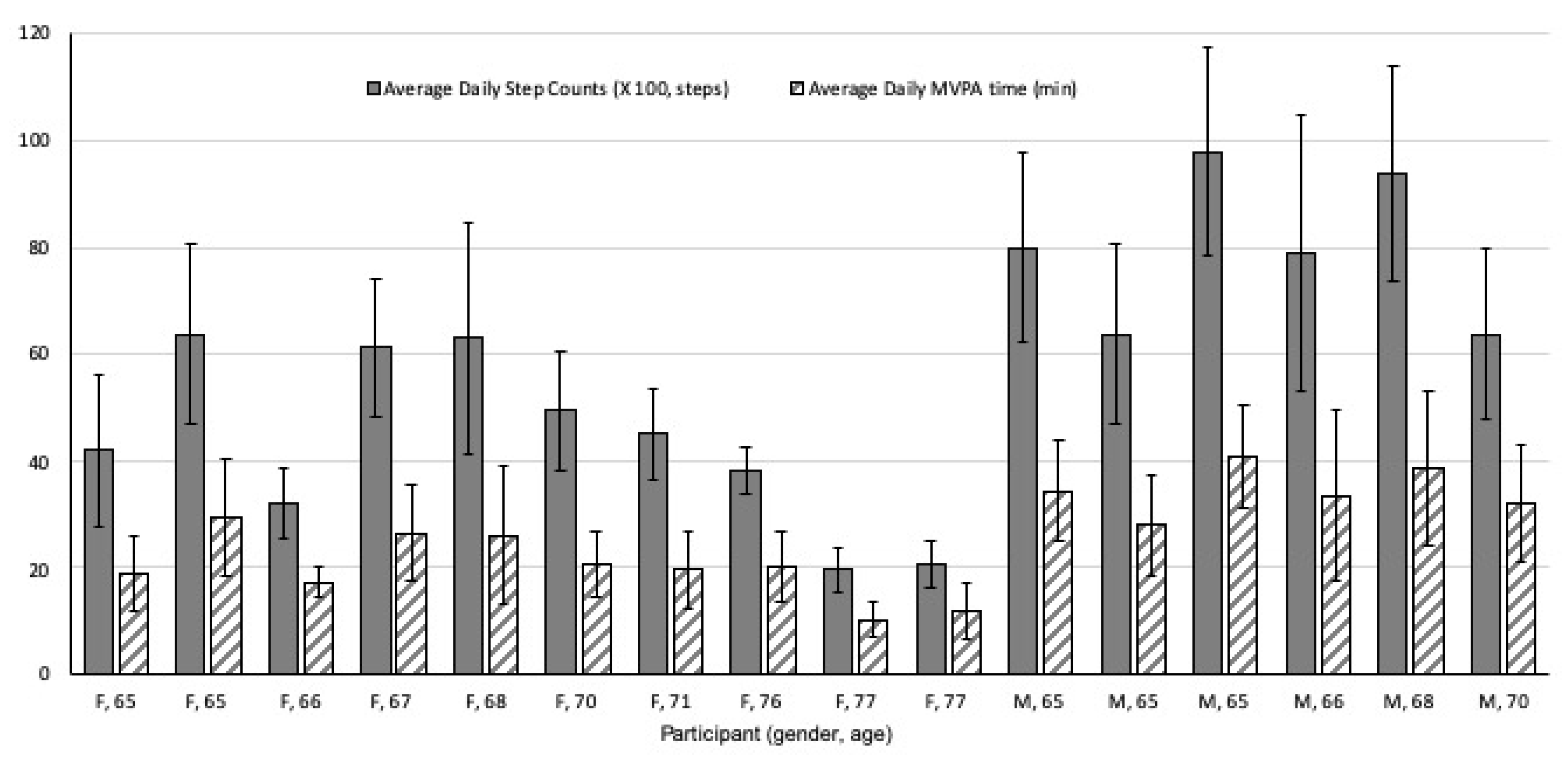
3.3. PA Performance Metrics
4. Discussion
4.1. Waning Patterns of Adoption Attitudes and PA Performance
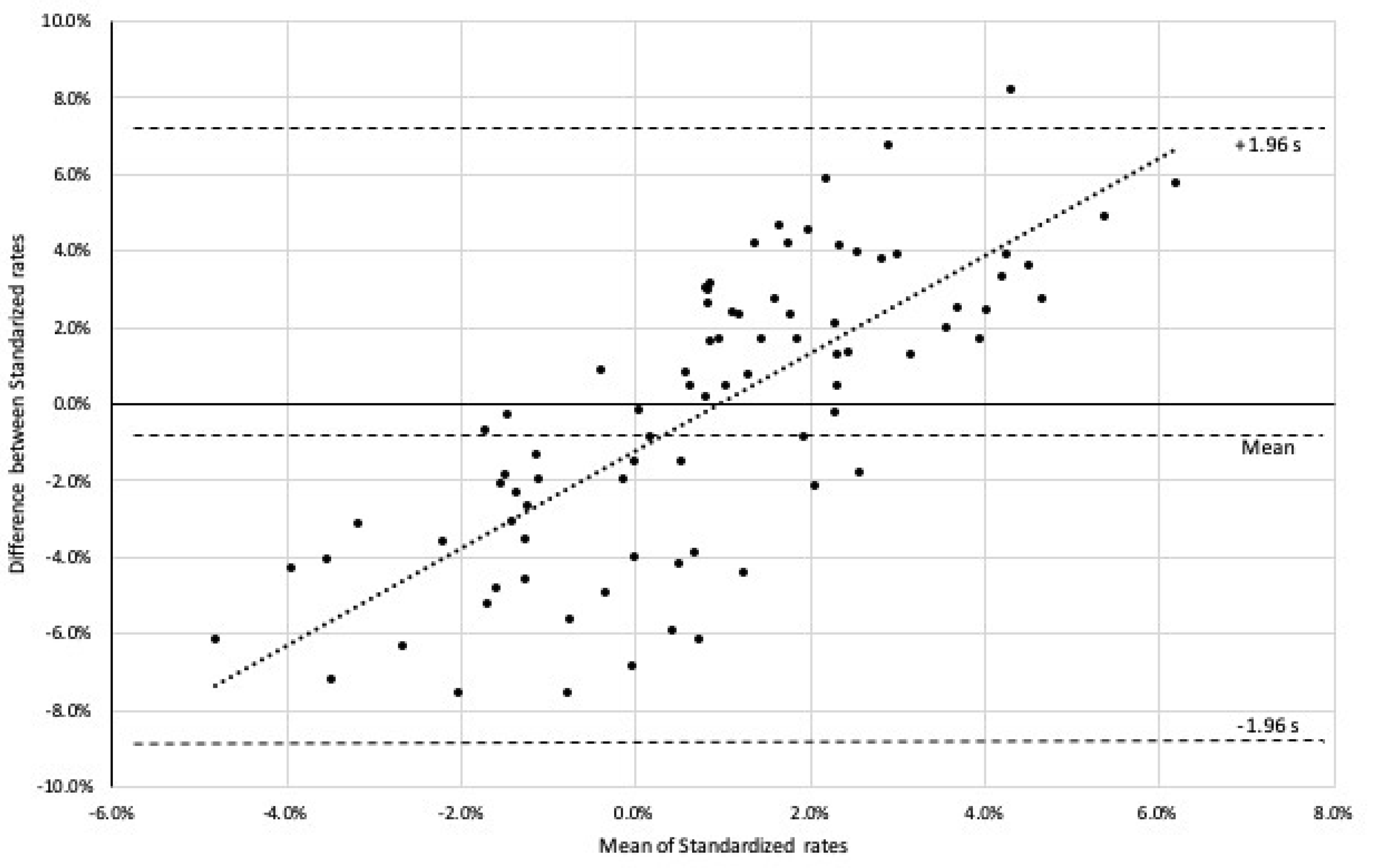
4.2. Different Onset and Duration of PA Performance Metrics
4.3. Strengths and Limitations of the Study
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Cooney, G.M.; Dwan, K.; Greig, C.A.; Lawlor, D.A.; Rimer, J.; Waugh, F.R.; McMurdo, M.; Mead, G.E. Exercise for depression. Cochrane Database Syst. Rev. 2013, 9, CD004366. [Google Scholar]
- Blumenthal, J.A.; Babyak, M.A.; Moore, K.A.; Craighead, W.E.; Herman, S.; Khatri, P.; Waugh, R.; Napolitano, M.A.; Forman, L.M.; Appelbaum, M. Effects of exercise training on older patients with major depression. Arch. Intern. Med. 1999, 159, 2349–2356. [Google Scholar] [CrossRef] [PubMed]
- Hales, C.M.; Carroll, M.D.; Fryar, C.D.; Ogden, C.L. Prevalence of Obesity Among Adults and Youth: United States, 2015–2016; US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics: Hyattsville, MD, USA, 2017.
- Harvey, J.A.; Chastin, S.F.; Skelton, D.A. How sedentary are older people? A systematic review of the amount of sedentary behavior. J. Aging Phys. Act. 2015, 23, 471–487. [Google Scholar] [CrossRef] [PubMed]
- US Department of Health and Human Service Physical Activity Guidelines for Americans: Be Active, Healthy, and Happy! Available online: https://www.hhs.gov/fitness/resource-center/facts-and-statistics/index.html (accessed on 8 November 2019).
- Carroll, M.D.; Fakhouri, T.H.; Flegal, K.M.; Kit, B.K.; Ogden, C.L. Prevalence of obesity among older adults in the United States, 2007–2010. NCHS Data Brief. 2012, 106, 1–8. [Google Scholar]
- Visser, M.; Brychta, R.J.; Chen, K.Y.; Koster, A. Self-reported adherence to the physical activity recommendation and determinants of misperception in older adults. J. Aging Phys. Act. 2014, 22, 226–234. [Google Scholar] [CrossRef]
- Chodzko-Zajko, W.J.; Proctor, D.N.; Singh, M.A.F.; Minson, C.T.; Nigg, C.R.; Salem, G.J.; Skinner, J.S. Exercise and physical activity for older adults. Med. Sci. Sports Exerc. 2009, 41, 1510–1530. [Google Scholar] [CrossRef]
- Jefferis, B.J.; Sartini, C.; Lee, I.-M.; Choi, M.; Amuzu, A.; Gutierrez, C.; Casas, J.P.; Ash, S.; Lennnon, L.T.; Wannamethee, S.G. Adherence to physical activity guidelines in older adults, using objectively measured physical activity in a population-based study. BMC Public Health 2014, 14, 382–391. [Google Scholar] [CrossRef]
- Center for Disease Control and Prevention Adult Participation in Aerobic and Muscle-Strengthening Physical Activities —United States. 2011. Available online: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6217a2.htm (accessed on 4 November 2019).
- Theou, O.; Jakobi, J.M.; Vandervoort, A.A.; Jones, G.R. A comparison of physical activity (PA) assessment tools across levels of frailty. Arch. Gerontol. Geriatr. 2012, 54, e307–e314. [Google Scholar] [CrossRef]
- Gobbens, R.J.; Luijkx, K.G.; Wijnen-Sponselee, M.T.; Schols, J.M. In search of an integral conceptual definition of frailty: Opinions of experts. J. Am. Med. Dir. Assoc. 2010, 11, 338–343. [Google Scholar] [CrossRef] [PubMed]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G. Frailty in older adults: Evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M146–M157. [Google Scholar] [CrossRef]
- Mulasso, A.; Brustio, P.R.; Rainoldi, A.; Zia, G.; Feletti, L.; N’dja, A.; Del Signore, S.; Poggiogalle, E.; Luisi, F.; Donini, L.M. A comparison between an ICT tool and a traditional physical measure for frailty evaluation in older adults. BMC Geriatr. 2019, 19, 88–100. [Google Scholar] [CrossRef] [PubMed]
- Hakim, A.A.; Petrovitch, H.; Burchfiel, C.M.; Ross, G.W.; Rodriguez, B.L.; White, L.R.; Yano, K.; Curb, J.D.; Abbott, R.D. Effects of walking on mortality among nonsmoking retired men. N. Engl. J. Med. 1998, 338, 94–99. [Google Scholar] [CrossRef] [PubMed]
- Hupin, D.; Roche, F.; Gremeaux, V.; Chatard, J.-C.; Oriol, M.; Gaspoz, J.-M.; Barthélémy, J.-C.; Edouard, P. Even a low-dose of moderate-to-vigorous physical activity reduces mortality by 22% in adults aged≥ 60 years: A systematic review and meta-analysis. Br. J. Sports Med. 2015, 49, 1262–1267. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, N.; Miyazaki, H.; Shimada, M.; Nakagawa, N.; Sawada, S.S.; Nishimuta, M.; Kimura, Y.; Kawakami, R.; Nagayama, H.; Asai, H. Daily step count and all-cause mortality in a sample of Japanese elderly people: A cohort study. BMC Public Health 2018, 18, 540. [Google Scholar] [CrossRef]
- Tudor-Locke, C.; Craig, C.L.; Aoyagi, Y.; Bell, R.C.; Croteau, K.A.; De Bourdeaudhuij, I.; Ewald, B.; Gardner, A.W.; Hatano, Y.; Lutes, L.D. How many steps/day are enough? For older adults and special populations. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Tudor-Locke, C.; Johnson, W.D.; Katzmarzyk, P.T. Relationship between accelerometer-determined steps/day and other accelerometer outputs in US adults. J. Phys. Act. Health 2011, 8, 410–419. [Google Scholar] [CrossRef]
- Mercer, K.; Giangregorio, L.; Schneider, E.; Chilana, P.; Li, M.; Grindrod, K. Acceptance of commercially available wearable activity trackers among adults aged over 50 and with chronic illness: A mixed-methods evaluation. JMIR MHealth UHealth 2016, 4, e7. [Google Scholar] [CrossRef]
- Michie, S.; Abraham, C.; Whittington, C.; McAteer, J.; Gupta, S. Effective techniques in healthy eating and physical activity interventions: A meta-regression. Health Psychol. 2009, 28, 690–701. [Google Scholar] [CrossRef]
- Lyons, E.J.; Lewis, Z.H.; Mayrsohn, B.G.; Rowland, J.L. Behavior change techniques implemented in electronic lifestyle activity monitors: A systematic content analysis. J. Med. Internet Res. 2014, 16, e192. [Google Scholar] [CrossRef]
- Herrmann, L.K.; Kim, J. The fitness of apps: A theory-based examination of mobile fitness app usage over 5 months. Mhealth 2017, 3, 2–11. [Google Scholar] [CrossRef]
- Ledger, D.; McCaffrey, D. Inside Wearables: How the Science of Human Behavior Change Offers the Secret to Long-Term Engagement. Endeavour Partners LLC. 2014. Available online: http://endeavourpartners.net/assets/Wearables-and-the-Science-of-Human-Behavior-Change-EP4.pdf (accessed on 11 November 2019).
- AARP Building a Better Tracker: Older Consumers Weigh in on Activity and Sleep Monitoring Devices 2015. Available online: https://www.aarp.org/content/dam/aarp/home-and-family/personal-technology/2015-07/innovation-50-project-catalyst-tracker-study-AARP.pdf (accessed on 1 March 2020).
- Fox, S.; Duggan, M. Health online 2013. Washington, DC: Pew Research Center. Available online: http://www.pewinternet.org/Reports/2013/Health-online.aspx (accessed on 10 March 2020).
- Karapanos, E.; Gouveia, R.; Hassenzahl, M.; Forlizzi, J. Wellbeing in the making: Peoples’ experiences with wearable activity trackers. Psychol. Well Being 2016, 6, 4. [Google Scholar] [CrossRef] [PubMed]
- Ridgers, N.D.; McNarry, M.A.; Mackintosh, K.A. Feasibility and effectiveness of using wearable activity trackers in youth: A systematic review. JMIR MHealth UHealth 2016, 4, e129. [Google Scholar] [CrossRef]
- Preusse, K.C.; Mitzner, T.L.; Fausset, C.B.; Rogers, W.A. Older adults’ acceptance of activity trackers. J. Appl. Gerontol. 2017, 36, 127–155. [Google Scholar] [CrossRef] [PubMed]
- Schlomann, A. A case study on older adults’ long-term use of an activity tracker. Gerontechnology 2017, 16, 115–124. [Google Scholar] [CrossRef]
- Rasche, P.; Wille, M.; Theis, S.; Schäefer, K.; Schlick, C.M.; Mertens, A. Activity tracker and elderly. In Proceedings of the 2015 IEEE International Conference on Computer and Information Technology; Ubiquitous Computing and Communications; Dependable, Autonomic and Secure Computing, Pervasive Intelligence and Computing, Liverpool, UK, 26–28 October 2015; IEEE: Piscataway, NJ, USA, 2015; pp. 1411–1416. [Google Scholar]
- Lazar, A.; Koehler, C.; Tanenbaum, J.; Nguyen, D.H. Why we use and abandon smart devices. In Proceedings of the 2015 ACM International Joint Conference on Pervasive and Ubiquitous Computing, New York, NY, USA, 12–16 September 2015; ACM: New York, NY, USA, 2015; pp. 635–646. [Google Scholar]
- King, W.R.; He, J. A meta-analysis of the technology acceptance model. Inf. Manag. 2006, 43, 740–755. [Google Scholar] [CrossRef]
- Venkatesh, V.; Thong, J.Y.; Xu, X. Unified theory of acceptance and use of technology: A synthesis and the road ahead. J. Assoc. Inf. Syst. 2016, 17, 328–376. [Google Scholar] [CrossRef]
- Paffenbarger, R.; Wing, A.; Hyde, R. Paffenbarger physical activity questionnaire. Am. J. Epidemiol. 1978, 108, 161–175. [Google Scholar] [CrossRef]
- Pecoraro, R.E.; Inui, T.S.; Chen, M.S.; Plorde, D.K.; Heller, J.L. Validity and reliability of a self-administered health history questionnaire. Public Health Rep. 1979, 94, 231–238. [Google Scholar]
- Li, H.; Wu, J.; Gao, Y.; Shi, Y. Examining individuals’ adoption of healthcare wearable devices: An empirical study from privacy calculus perspective. Int. J. Med. Inf. 2016, 88, 8–17. [Google Scholar] [CrossRef]
- Tudor-Locke, C.; Schuna, J.M., Jr.; Barreira, T.V.; Mire, E.F.; Broyles, S.T.; Katzmarzyk, P.T.; Johnson, W.D. Normative steps/day values for older adults: NHANES 2005–2006. J. Gerontol. Ser. Biomed. Sci. Med. Sci. 2013, 68, 1426–1432. [Google Scholar] [CrossRef]
- McMahon, S.K.; Lewis, B.; Oakes, M.; Guan, W.; Wyman, J.F.; Rothman, A.J. Older adults’ experiences using a commercially available monitor to self-track their physical activity. JMIR MHealth UHealth 2016, 4, e35–e45. [Google Scholar] [CrossRef] [PubMed]
- Bland, J.M.; Altman, D.G. Measuring agreement in method comparison studies. Stat. Methods Med. Res. 1999, 8, 135–160. [Google Scholar] [CrossRef]
- Paffenbarger, J.R.; Blair, S.N.; Lee, I.-M.; Hyde, R.T. Measurement of physical activity to assess health effects in free-living populations. Med. Sci. Sports Exerc. 1993, 25, 60–70. [Google Scholar] [CrossRef] [PubMed]
- Samuels, T.Y.; Raedeke, T.D.; Mahar, M.T.; Karvinen, K.H.; DuBose, K.D. A randomized controlled trial of continuous activity, short bouts, and a 10,000 step guideline in inactive adults. Prev. Med. 2011, 52, 120–125. [Google Scholar] [CrossRef]
- Nahum-Shani, I.; Smith, S.N.; Spring, B.J.; Collins, L.M.; Witkiewitz, K.; Tewari, A.; Murphy, S.A. Just-in-time adaptive interventions (JITAIs) in mobile health: Key components and design principles for ongoing health behavior support. Ann. Behav. Med. 2018, 52, 446–462. [Google Scholar] [CrossRef] [PubMed]
- Munson, S.A.; Consolvo, S. Exploring goal-setting, rewards, self-monitoring, and sharing to motivate physical activity. In Proceedings of the 2012 6th International Conference on Pervasive Computing Technologies for Healthcare (Pervasivehealth) and Workshops, San Diego, CA, USA, 12 April 2012; IEEE: Piscataway, NJ, USA, 2012; pp. 25–32. [Google Scholar]
- Sung, J.; Christensen, H.I.; Grinter, R.E. Robots in the wild: Understanding long-term use. In Proceedings of the 4th ACM/IEEE International Conference on Human Robot Interaction, New York, NY, USA, 15 March 2009; ACM: New York, NY, USA, 2009; pp. 45–52. [Google Scholar]
- Mutsuddi, A.U.; Connelly, K. Text messages for encouraging physical activity Are they effective after the novelty effect wears off? In Proceedings of the 2012 6th International Conference on Pervasive Computing Technologies for Healthcare (PervasiveHealth) and Workshops, San Diego, CA, USA, 21–24 May 2012; IEEE: Piscataway, NJ, USA, 2012; pp. 33–40. [Google Scholar]
- Le Hello, C.; Trombert, B.; Morel, A.; Chieh, A.; Brouard, B.; Boissier, C. Performance analysis of walking of 10,000 regular users of a connected activity tracker. JMV J. Médecine Vasc. 2018, 43, 231–237. [Google Scholar] [CrossRef]
- Newton, R.L.; Dubbert, P.M.; Johnson, W.D.; Hickson, D.A.; Ainsworth, B.; Carithers, T.; Taylor, H.; Wyatt, S.; Tudor-Locke, C. Pedometer determined physical activity tracks in African American adults: The Jackson Heart Study. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 44–51. [Google Scholar] [CrossRef] [PubMed]
- Feito, Y.; Hornbuckle, L.M.; Reid, L.A.; Crouter, S.E. Effect of ActiGraph’s low frequency extension for estimating steps and physical activity intensity. PLoS ONE 2017, 12, e0188242. [Google Scholar] [CrossRef]
- Lee, J.-M.; Kim, Y.; Bai, Y.; Gaesser, G.A.; Welk, G.J. Validation of the SenseWear mini armband in children during semi-structure activity settings. J. Sci. Med. Sport 2016, 19, 41–45. [Google Scholar] [CrossRef]
- An, H.-S.; Jones, G.C.; Kang, S.-K.; Welk, G.J.; Lee, J.-M. How valid are wearable physical activity trackers for measuring steps? Eur. J. Sport Sci. 2017, 17, 360–368. [Google Scholar] [CrossRef]
- Fokkema, T.; Kooiman, T.J.; Krijnen, W.P.; VAN, C.D.S.; DE, M.G. Reliability and Validity of Ten Consumer Activity Trackers Depend on Walking Speed. Med. Sci. Sports Exerc. 2017, 49, 793–800. [Google Scholar] [CrossRef] [PubMed]
- Sears, T.; Alvalos, E.; Lawson, S.; McAlister, I.; Eschbach, L.C.; Bunn, J. Wrist-worn physical activity trackers tend to underestimate steps during walking. Int. J. Exerc. Sci. 2017, 10, 764–773. [Google Scholar]
- Nielson, R.; Vehrs, P.R.; Fellingham, G.W.; Hager, R.; Prusak, K.A. Step counts and energy expenditure as estimated by pedometry during treadmill walking at different stride frequencies. J. Phys. Act. Health 2011, 8, 1004–1013. [Google Scholar] [CrossRef]
- Midorikawa, T.; Tanaka, S.; Kaneko, K.; Koizumi, K.; Ishikawa-Takata, K.; Futami, J.; Tabata, I. Evaluation of Low-Intensity Physical Activity by Triaxial Accelerometry. Obesity 2007, 15, 3031–3038. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, J.E.; Hickey, A.; Mavilia, M.; Tedesco, J.; John, D.; Keadle, S.K.; Freedson, P.S. Validation of the Fitbit wireless activity tracker for prediction of energy expenditure. J. Phys. Act. Health 2015, 12, 149–154. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, T.; Rowlands, A.V.; Olds, T.; Maher, C. The validity of consumer-level, activity monitors in healthy adults worn in free-living conditions: A cross-sectional study. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 42–51. [Google Scholar] [CrossRef]
- Alharbi, M.; Straiton, N.; Smith, S.; Neubeck, L.; Gallagher, R. Data management and wearables in older adults: A systematic review. Maturitas 2019, 124, 100–110. [Google Scholar] [CrossRef]
- Melanson, E.L.; Knoll, J.R.; Bell, M.L.; Donahoo, W.T.; Hill, J.O.; Nysse, L.J.; Lanningham-Foster, L.; Peters, J.C.; Levine, J.A. Commercially available pedometers: Considerations for accurate step counting. Prev. Med. 2004, 39, 361–368. [Google Scholar] [CrossRef]
- Webber, S.C.; Magill, S.M.; Schafer, J.L.; Wilson, K.C. GT3X+ accelerometer, Yamax pedometer, and SC-StepMX pedometer step count accuracy in community-dwelling older adults. J. Aging Phys. Act. 2014, 22, 334–341. [Google Scholar] [CrossRef]
- Magistro, D.; Brustio, P.R.; Ivaldi, M.; Esliger, D.W.; Zecca, M.; Rainoldi, A.; Boccia, G. Validation of the ADAMO Care Watch for step counting in older adults. PLoS ONE 2018, 13, e0190753. [Google Scholar] [CrossRef]
| Male | Female | |
|---|---|---|
| Age (years) | 67.5 ± 2.5 | 71 ± 6 |
| Height (cm) | 175.8 ± 6.7 | 164.6 ± 5.9 |
| Weight (kg) | 81.7 ± 5.77 | 69.1 ± 5.45 |
| BMI (kg/m2) | 26.47 ± 3.78 | 25.34 ± 3.79 |
| Race | ||
| Caucasian/White | 2 | 4 |
| Hispanic | 4 | 5 |
| Black | - | 1 |
| Constructs | Survey Items | Beginning (1st Week) | Middle (7th Week) | Ending (13rd Week) |
|---|---|---|---|---|
| Health information sensitivity | I feel comfortable with the type of health information the activity tracker request from me. | 6.5 (1.43) | 6.1 (1.29)) | 6.2 (1.52) |
| I do not feel the activity tracker gathers highly personal health information about me. | 6.1 (1.79) | 5.9 (1.95) | 6.0 (1.66) | |
| The health information I should provide to the activity tracker is not sensitive to me. | 5.9 (1.49 | 5.7 (1.36) | 5.8 (1.55) | |
| Legislative protection | I believe that I would be protected from the misuse of my physical activity. | 5.3 (1.89) | 5.7 (1.36) | 5.6 (1.67) |
| I believe that the practices of how activity trackers collect, use, and protect my private health information should be governed and interpreted. | 5.7 (1.55) | 5.5 (1.78) | 5.4 (1.88) | |
| I believe that the violation of the health information I provided to activity trackers should be able to be addressed. | 4.5 (1.33) | 4.4 (1.40) | 4.5 (1.39) | |
| Perceived privacy risk | It would be assured to disclose my physical activity information to activity tracker vendors. | 4.6 (1.75) | 4.7 (1.56) | 4.5 (1.65) |
| There would be low potential for loss associated with disclosing my physical activity information to activity tracker vendors. | 3.9 (1.28) | 3.7 (1.58) | 3.7 (1.62) | |
| There would not be much uncertainty associated with giving my physical activity information to activity tracker vendors. | 4.3 (1.44) | 4.4 (1.51) | 4.5 (1.29) | |
| Personal innovativeness | If I heard about a new technology, I would look for ways to experiment with it. | 4.9 (1.62) | 4.7 (1.54) | 4.7 (1.77) |
| Among my peers, I am usually the first to try out new technologies. | 4.9 (1.62) | 3.8 (1.51) | 3.9 (1.66) | |
| In general, I like to experiment with new technologies. | 3.7 (1.71) | 3.8 (1.44) | 3.6 (1.52) | |
| Perceived informativeness | Activity trackers are good sources of personal health information. | 5.8 (1.89) | 4.5 (1.21) | 3.9 (1.37) |
| Activity trackers supply relevant health information. | 5.9 (1.78 | 4.3 (1.32) | 4.0 (1.41) | |
| Activity trackers are informative about my personal health information. | 5.8 (1.73) | 4.3 (1.29) | 3.5 (1.38) | |
| Functional congruence | Activity trackers are (expected to be) comfortable. | 5.0 (1.69) | 3.7 (0.98) | 3.4 (0.75) |
| Activity trackers are (expected to be) durable. | 5.8 (1.47) | 5.0 (1.35) | 4.5(1.33) | |
| Activity trackers are (expected to be) priced appropriately considering their quality. | 5.2 (1.52) | 5.0 (1.60) | 4.6 (1.48) | |
| Perceived benefit | Using an activity tracker would improve my access to my health information. | 5.6 (1.31) | 4.8 (1.33) | 4.7 (1.24) |
| Using an activity tracker would improve my ability to manage my health. | 5.7 (1.49) | 5.1 (1.39) | 4.8 (1.47) | |
| Using an activity tracker would improve the quality of my healthcare. | 4.8 (1.29) | 4.2 (1.30) | 4.0 (1.37) | |
| Adoption intention(Self-efficacy) | I will be able to achieve most of the health goals that I have set. | 5.5 (1.77) | 3.0 (1.04) | 2.4 (0.85) |
| I can obtain desirable health outcomes that are important to me by activity tracker use. | 4.9 (1.48) | 3.1 (1.25) | 2.7 (0.89) | |
| I am confident that I can exercise effectively with an activity tracker. | 5.1 (1.25) | 3.2 (1.07) | 2.7 (0.77) | |
| Actual adoption behavior | I use an activity tracker to stay on the path of healthy living. | 5.3 (1.30) | 4.2 (1.13) | 3.4 (0.91) |
| I often use an activity tracker to get health information. | 4.7 (1.33) | 3.2 (0.96) | 2.6 (0.76) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, B.C.; Xie, J.; Ajisafe, T.; Kim, S.-H. How Are Wearable Activity Trackers Adopted in Older Adults? Comparison between Subjective Adoption Attitudes and Physical Activity Performance. Int. J. Environ. Res. Public Health 2020, 17, 3461. https://doi.org/10.3390/ijerph17103461
Lee BC, Xie J, Ajisafe T, Kim S-H. How Are Wearable Activity Trackers Adopted in Older Adults? Comparison between Subjective Adoption Attitudes and Physical Activity Performance. International Journal of Environmental Research and Public Health. 2020; 17(10):3461. https://doi.org/10.3390/ijerph17103461
Chicago/Turabian StyleLee, Byung Cheol, Junfei Xie, Toyin Ajisafe, and Sung-Hee Kim. 2020. "How Are Wearable Activity Trackers Adopted in Older Adults? Comparison between Subjective Adoption Attitudes and Physical Activity Performance" International Journal of Environmental Research and Public Health 17, no. 10: 3461. https://doi.org/10.3390/ijerph17103461
APA StyleLee, B. C., Xie, J., Ajisafe, T., & Kim, S.-H. (2020). How Are Wearable Activity Trackers Adopted in Older Adults? Comparison between Subjective Adoption Attitudes and Physical Activity Performance. International Journal of Environmental Research and Public Health, 17(10), 3461. https://doi.org/10.3390/ijerph17103461






