Adverse Childhood Experiences and Changing Levels of Psychosocial Distress Scores across Pregnancy in Kenyan Women
Abstract
1. Background
2. Materials and Methods
2.1. Data and Sample
2.2. Measures
2.3. Predictor: ACEs
2.4. Outcome Variables
2.5. Covariates
2.6. Statistical Methods
3. Results
3.1. Preliminary Analyses
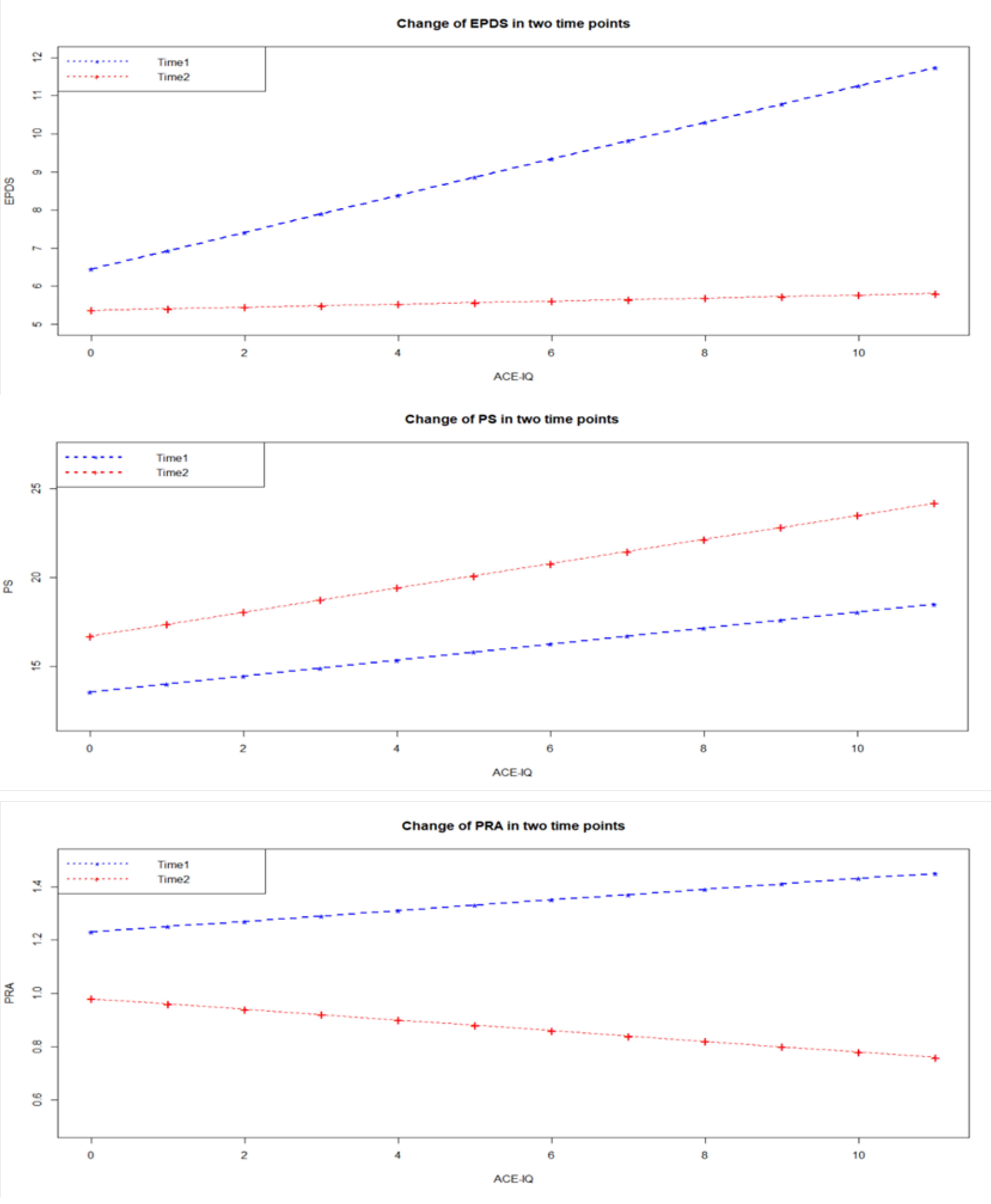
3.2. Hypothesis Testing
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kremer, P.; Ulibarri, M.; Ferraiolo, N.; Pinedo, M.; Vargas-Ojeda, A.C.; Burgos, J.L.; Ojeda, V.D. Association of Adverse Childhood Experiences with Depression in Latino Migrants Residing in Tijuana, Mexico. Perm. J. 2019, 23. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.V.; Gotman, N.; Yonkers, K.A. Early childhood adversity and pregnancy outcomes. Matern. Child Health J. 2016, 20, 790–798. [Google Scholar] [CrossRef]
- Herzog, J.I.; Schmahl, C. Adverse childhood experiences and the consequences on neurobiological, psychosocial, and somatic conditions across the lifespan. Front. Psychiatry 2018, 9, 420. [Google Scholar] [CrossRef] [PubMed]
- Rieder, A.D.; Roth, S.L.; Musyimi, C.; Ndetei, D.; Sassi, R.B.; Mutiso, V.; Hall, G.B.; Gonzalez, A. Impact of maternal adverse childhood experiences on child socioemotional function in rural Kenya: Mediating role of maternal mental health. Dev. Sci. 2019, 22, e12833. [Google Scholar] [CrossRef] [PubMed]
- Felitti, V.J.; Anda, R.F.; Nordenberg, D.; Williamson, D.F.; Spitz, A.M.; Edwards, V.; Koss, M.P.; Marks, J.S. Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults: The Adverse Childhood Experiences (ACE) Study. Am. J. Prev. Med. 1998, 14, 245–258. [Google Scholar] [CrossRef]
- Hughes, K.; Bellis, M.A.; Hardcastle, K.A.; Sethi, D.; Butchart, A.; Mikton, C.; Jones, L.; Dunne, M.P. The effect of multiple adverse childhood experiences on health: A systematic review and meta-analysis. Lancet Public Health 2017, 2, e356–e366. [Google Scholar] [CrossRef]
- Pesonen, A.K.; Räikkönen, K.; Heinonen, K.; Kajantie, E.; Forsén, T.; Eriksson, J.G. Reproductive traits following a parent–child separation trauma during childhood: A natural experiment during World War II. Am. J. Hum. Biol. Off. J. Hum. Biol. Assoc. 2008, 20, 345–351. [Google Scholar] [CrossRef]
- Angerud, K.; Annerback, E.M.; Tyden, T.; Boddeti, S.; Kristiansson, P. Adverse childhood experiences and depressive symptomatology among pregnant women. Acta Obstet. Gynecol. Scand. 2018, 97, 701–708. [Google Scholar] [CrossRef]
- Atzl, V.M.; Narayan, A.J.; Rivera, L.M.; Lieberman, A.F. Adverse childhood experiences and prenatal mental health: Type of ACEs and age of maltreatment onset. J. Fam. Psychol. 2019, 33, 304. [Google Scholar] [CrossRef]
- Chung, E.K.; Nurmohamed, L.; Mathew, L.; Elo, I.T.; Coyne, J.C.; Culhane, J.F. Risky health behaviors among mothers-to-be: The impact of adverse childhood experiences. Acad. Pediatr. 2010, 10, 245–251. [Google Scholar] [CrossRef]
- Leeners, B.; Görres, G.; Block, E.; Hengartner, M.P. Birth experiences in adult women with a history of childhood sexual abuse. J. Psychosom. Res. 2016, 83, 27–32. [Google Scholar] [CrossRef]
- Austin, M.-P.; Tully, L.; Parker, G. Examining the relationship between antenatal anxiety and postnatal depression. J. Affect. Disord. 2007, 101, 169–174. [Google Scholar] [CrossRef] [PubMed]
- Josefsson, A.; Angelsiöö, L.; Berg, G.; Ekström, C.-M.; Gunnervik, C.; Nordin, C.; Sydsjö, G. Obstetric, somatic, and demographic risk factors for postpartum depressive symptoms. Obstet. Gynecol. 2002, 99, 223–228. [Google Scholar] [PubMed]
- Rose, M.S.; Pana, G.; Premji, S. Prenatal maternal anxiety as a risk factor for preterm birth and the effects of heterogeneity on this relationship: A systematic review and meta-analysis. BioMed Res. Int. 2016, 2016, 8312158. [Google Scholar] [CrossRef] [PubMed]
- Kingston, D.; Tough, S.; Whitfield, H. Prenatal and postpartum maternal psychological distress and infant development: A systematic review. Child Psychiatry Hum. Dev. 2012, 43, 683–714. [Google Scholar] [CrossRef] [PubMed]
- Fisher, J.; Cabral de Mello, M.; Patel, V.; Rahman, A.; Tran, T.; Holton, S.; Holmes, W. Prevalence and determinants of common perinatal mental disorders in women in low- and lower-middle-income countries: A systematic review. Bull. World Health Organ. 2012, 90, 139H–149H. [Google Scholar] [CrossRef] [PubMed]
- Walker, S.P.; Wachs, T.D.; Grantham-McGregor, S.; Black, M.M.; Nelson, C.A.; Huffman, S.L.; Baker-Henningham, H.; Chang, S.M.; Hamadani, J.D.; Lozoff, B.; et al. Inequality in early childhood: Risk and protective factors for early child development. Lancet 2011, 378, 1325–1338. [Google Scholar] [CrossRef]
- Mbagaya, C.; Oburu, P.; Bakermans-Kranenburg, M.J. Child physical abuse and neglect in Kenya, Zambia and the Netherlands: A cross-cultural comparison of prevalence, psychopathological sequelae and mediation by PTSS. Int. J. Psychol. 2013, 48, 95–107. [Google Scholar] [CrossRef]
- National Center for Injury Prevention and Control, Division of Violence Prevention CDC and Prevention Kenya National Bureau of Statistics. Violence against Children in Kenya: Findings from a 2010 National Survey. Summary Report on the Prevalence of Sexual, Physical and Emotional Violence, Context of Sexual Violence, and Health and Behavioral Consequences of Violence Experienced in Childhood; UNICEF: Geneva, Switzerland, 2012; pp. 7–8. [Google Scholar]
- Belay, Y.A.; Moges, N.A.; Hiksa, F.F.; Arado, K.K.; Liben, M.L. Prevalence of Antenatal Depression and Associated Factors among Pregnant Women Attending Antenatal Care at Dubti Hospital: A Case of Pastoralist Region in Northeast Ethiopia. Depress. Res. Treat. 2018, 2018, 1659089. [Google Scholar] [CrossRef]
- Biratu, A.; Haile, D. Prevalence of antenatal depression and associated factors among pregnant women in Addis Ababa, Ethiopia: A cross-sectional study. Reprod. Health 2015, 12, 99. [Google Scholar] [CrossRef]
- Thompson, O.; Ajayi, I. Prevalence of Antenatal Depression and Associated Risk Factors among Pregnant Women Attending Antenatal Clinics in Abeokuta North Local Government Area, Nigeria. Depress. Res. Treat. 2016, 2016, 4518979. [Google Scholar] [CrossRef] [PubMed]
- Ashley, J.M.; Harper, B.D.; Arms-Chavez, C.J.; LoBello, S.G. Estimated prevalence of antenatal depression in the US population. Arch. Womens Ment. Health 2016, 19, 395–400. [Google Scholar] [CrossRef]
- Jairaj, C.; Fitzsimons, C.M.; McAuliffe, F.M.; O’Leary, N.; Joyce, N.; McCarthy, A.; Cassidy, E.; Donnelly, J.; Tully, E.; Imcha, M.; et al. A population survey of prevalence rates of antenatal depression in the Irish obstetric services using the Edinburgh Postnatal Depression Scale (EPDS). Arch. Womens Ment. Health 2019, 22, 349–355. [Google Scholar] [CrossRef] [PubMed]
- Choi, K.W.; Sikkema, K.J.; Vythilingum, B.; Geerts, L.; Faure, S.C.; Watt, M.H.; Roos, A.; Stein, D.J. Maternal childhood trauma, postpartum depression, and infant outcomes: Avoidant affective processing as a potential mechanism. J. Affect. Disord. 2017, 211, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Premji, S. Perinatal distress in women in low-and middle-income countries: Allostatic load as a framework to examine the effect of perinatal distress on preterm birth and infant health. Matern. Child Health J. 2014, 18, 2393–2407. [Google Scholar] [CrossRef]
- Wall, V.; Premji, S.S.; Letourneau, N.; McCaffrey, G.; Nyanza, E.C. Factors associated with pregnancy-related anxiety in Tanzanian women: A cross sectional study. BMJ Open 2018, 8, e020056. [Google Scholar] [CrossRef]
- Gelaye, B.; Rondon, M.B.; Araya, R.; Williams, M.A. Epidemiology of maternal depression, risk factors, and child outcomes in low-income and middle-income countries. Lancet Psychiatry 2016, 3, 973–982. [Google Scholar] [CrossRef]
- Osok, J.; Kigamwa, P.; Vander Stoep, A.; Huang, K.-Y.; Kumar, M. Depression and its psychosocial risk factors in pregnant Kenyan adolescents: A cross-sectional study in a community health Centre of Nairobi. BMC Psychiatry 2018, 18, 136. [Google Scholar] [CrossRef]
- Young-Wolff, K.C.; Alabaster, A.; McCaw, B.; Stoller, N.; Watson, C.; Sterling, S.; Ridout, K.K.; Flanagan, T. Adverse childhood experiences and mental and behavioral health conditions during pregnancy: The role of resilience. J. Women. Health 2019, 28, 452–461. [Google Scholar] [CrossRef]
- UNICEF. Situation Analysis of Children and Adolescents in Kenya 2014: Our Children, Our Future; UNICEF: Geneva, Switzerland, 2014. [Google Scholar]
- World Health Organization. Adverse Childhood Experiences International Questionnaire (ACE-IQ); World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Murphy, A.; Steele, M.; Dube, S.R.; Bate, J.; Bonuck, K.; Meissner, P.; Goldman, H.; Steele, H. Adverse Childhood Experiences (ACEs) questionnaire and Adult Attachment Interview (AAI): Implications for parent child relationships. Child Abuse Negl. 2014, 38, 224–233. [Google Scholar] [CrossRef]
- Bergink, V.; Kooistra, L.; Lambregtse-van den Berg, M.P.; Wijnen, H.; Bunevicius, R.; van Baar, A.; Pop, V. Validation of the Edinburgh Depression Scale during pregnancy. J. Psychosom. Res. 2011, 70, 385–389. [Google Scholar] [CrossRef] [PubMed]
- Cox, J.L.; Holden, J.M.; Sagovsky, R. Detection of postnatal depression: Development of the 10-item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry 1987, 150, 782–786. [Google Scholar] [CrossRef] [PubMed]
- Regmi, S.; Sligl, W.; Carter, D.; Grut, W.; Seear, M. A controlled study of postpartum depression among Nepalese women: Validation of the Edinburgh Postpartum Depression Scale in Kathmandu. Trop. Med. Int. Health 2002, 7, 378–382. [Google Scholar] [CrossRef] [PubMed]
- Rini, C.K.; Dunkel-Schetter, C.; Wadhwa, P.D.; Sandman, C.A. Psychological adaptation and birth outcomes: The role of personal resources, stress, and sociocultural context in pregnancy. Health Psychol. 1999, 18, 333. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A Global Measure of Perceived Stress. Am. Sociol. Assoc. 1983, 24, 385–396. [Google Scholar] [CrossRef]
- Baik, S.H.; Fox, R.S.; Mills, S.D.; Roesch, S.C.; Sadler, G.R.; Klonoff, E.A.; Malcarne, V.L. Reliability and validity of the Perceived Stress Scale-10 in Hispanic Americans with English or Spanish language preference. J. Health Psychol. 2019, 24, 628–639. [Google Scholar] [CrossRef]
- Hahn-Holbrook, J.; Dunkel Schetter, C.; Arora, C.; Hobel, C.J. Placental Corticotropin-Releasing Hormone Mediates the Association Between Prenatal Social Support and Postpartum Depression. Clin. Psychol. Sci. 2013, 1, 253–265. [Google Scholar] [CrossRef]
- Yim, I.S.; Glynn, L.M.; Dunkel Schetter, C.; Hobel, C.J.; Chicz-DeMet, A.; Sandman, C.A. Risk of Postpartum Depressive Symptoms With Elevated Corticotropin-Releasing Hormone in Human Pregnancy. Arch. Gen. Psychiatry 2009, 66. [Google Scholar] [CrossRef]
- Bowers, K.; Ding, L.; Gregory, S.; Yolton, K.; Ji, H.; Meyer, J.; Ammerman, R.T.; Van Ginkel, J.; Folger, A. Maternal distress and hair cortisol in pregnancy among women with elevated adverse childhood experiences. Psychoneuroendocrinology 2018, 95, 145–148. [Google Scholar] [CrossRef]
- Skjothaug, T.; Smith, L.; Wentzel-Larsen, T.; Moe, V. Prospective fathers’ adverse childhood experiences, pregnancy-related anxiety, and depression during pregnancy. Infant Ment. Health J. 2015, 36, 104–113. [Google Scholar] [CrossRef]
- Lara, M.A.; Navarrete, L.; Nieto, L.; Le, H.N. Childhood abuse increases the risk of depressive and anxiety symptoms and history of suicidal behavior in Mexican pregnant women. Braz. J. Psychiatry 2015, 37, 203–210. [Google Scholar] [CrossRef] [PubMed]
- Leeners, B.; Richter-Appelt, H.; Imthurn, B.; Rath, W. Influence of childhood sexual abuse on pregnancy, delivery, and the early postpartum period in adult women. J. Psychosom. Res. 2006, 61, 139–151. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Value |
|---|---|
| Age M (SD) | 30.55 (4.32) |
| Range | 22–47 |
| Education n (%) | |
| Secondary/High school completed | 9 (4.2) |
| College/University completed | 160 (74.4) |
| Post graduate degree | 46 (21.4) |
| Marital Status n (%) | |
| Married | 174 (80.9) |
| Not married | 41 (19.1) |
| Working status n (%) | |
| Government employee | 34 (15.8) |
| Non-government employee | 105 (48.8) |
| Self-employed | 50 (23.3) |
| Student | 10 (4.7) |
| Homemaker | 9 (4.2) |
| Unemployed (able to work) | 7 (3.3) |
| Annual Family Income n (%) | |
| KES 40,001–100,000 | 36 (16.7) |
| KES 100,001–200,000 | 86 (40.0) |
| More than KES 200,001 | 87 (40.5) |
| Ethnicity n (%) | |
| Kikuyu | 93 (43.3) |
| Kalenjin | 10 (4.7) |
| Kamba | 20 (9.3) |
| Luhya | 23 (10.7) |
| Luo | 20 (9.3) |
| Other | 49 (22.8) |
| Health Behaviors n (%) | |
| Alcohol | |
| Never | 209 (97.2) |
| Monthly or less | 5 (2.3) |
| 2–3 times per week | 1 (0.5) |
| Smoking | 1 (0.5) |
| Pica | 3 (1.4) |
| Childhood Experience | n (Prevalence %) |
|---|---|
| Neglect | |
| Emotional neglect | 181 (84.2) |
| Physical neglect | 12 (5.6) |
| Psychological Distress of Family Members | |
| Alcohol or drug abuse in household | 24 (11.2) |
| Incarcerated household member | 7 (3.3) |
| Mentally ill household member | 5 (2.3) |
| Parental death or divorce | 54 (25.1) |
| Violence at Home | |
| Household member treated violently | 140 (65.1) |
| Emotional abuse | 109 (50.7) |
| Physical abuse | 167 (77.7) |
| Sexual Violence | |
| Contact sexual abuse | 38 (17.7) |
| Violence in Community | |
| Bullying | 94 (43.7) |
| Community violence | 171 (79.5) |
| Collective violence | 28 (13) |
| Scores at Enrolment | Scores at Follow-Up | |||||||
|---|---|---|---|---|---|---|---|---|
| Time | ACE-IQ Score | Anxiety | Depressive Symptoms | Stress | Anxiety | Depressive Symptoms | Stress | |
| Enrolment | ACE-IQ binary | 1.00 | ||||||
| Anxiety | 0.02 | 1.00 | ||||||
| Depressive Symptoms | 0.23 * | 0.05 | 1.00 | |||||
| Perceived Stress | 0.18 * | 0.02 | 0.67 * | 1.00 | ||||
| Follow Up | Anxiety | −0.04 | 0.07 | −0.18 * | −0.07 | 1.00 | ||
| Depressive Symptoms | 0.01 | −0.07 | 0.19 * | 0.14 | 0.03 | 1.00 | ||
| Perceived Stress | 0.07 | −0.08 | 0.21 * | 0.25 * | −0.05 | 0.33 * | 1.00 | |
| Time 1 (n = 215) | Time 1 * (n = 169) | Time 2 (n = 169) | Paired Comparison (T2-T1) (n = 169) | |||
|---|---|---|---|---|---|---|
| Scale | Mean (SD) | Mean (SD) | Mean (SD) | Mean (Std Err) | t (df = 167) | p-Value |
| Anxiety | 1.3 (1.33) | 1.3 (1.36) | 1.1 (1.04) | −0.21 (0.13) | −1.70 | 0.091 |
| Depression | 8.6 (4.33) | 8.8 (4.37) | 5.6 (2.78) | −3.04 (0.36) | −8.44 | <0.001 |
| Stress | 15.7 (5.21) | 15.8 (5.21) | 17.8 (4.27) | 2.07 (0.45) | 4.60 | <0.001 |
| Model Predictors | Anxiety (PRA) | Depression (EPDS) | Perceived Stress (PS) | |||
|---|---|---|---|---|---|---|
| Estimate | p-Value | Estimate | p-Value | Estimate | p-Value | |
| Constant | 1.23 (0.23) | <0.01 | 6.46 (0.73) | <0.01 | 13.57 (0.88) | <0.01 |
| Time | −0.25 (0.3) | 0.05 | −1.09 (0.83) | 0.05 | 3.14 (1.07) | <0.01 |
| ACE-IQ | 0.02 (0.04) | 0.72 | 0.48 (0.14) | <0.01 | 0.45 (0.17) | 0.01 |
| Time * ACE-IQ | −0.04 (0.06) | 0.48 | −0.44 (0.16) | <0.01 | 0.23 (0.21) | 0.12 |
| Estimate | p-Value | |
|---|---|---|
| (a) PRA | ||
| (Intercept) | 1.29 (0.09) | <0.01 |
| Time | −0.20 (0.12) | 0.10 |
| Mentally ill household member | 0.91 (0.61) | 0.14 |
| Time * Mentally ill household member | −2.00 (0.74) | 0.01 |
| (b) EPDS | ||
| (Intercept) | 7.96 (0.36) | <0.01 |
| Time | −2.58 (0.41) | <0.01 |
| Contact sexual abuse | 2.24 (0.76) | <0.01 |
| Parental death or divorce | 1.67 (0.67) | 0.01 |
| Time * Contact sexual abuse | −1.41 (0.88) | 0.11 |
| Time * Parental death or divorce | −1.16 (0.76) | 0.13 |
| (c) PS | ||
| (Intercept) | 15.61 (0.35) | <0.01 |
| Time | 2.19 (0.43) | <0.01 |
| Mentally ill household member | 6.19 (2.33) | 0.01 |
| Time * Mentally ill household member | 5.59 (2.62) | 0.03 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Samia, P.; Premji, S.; Tavangar, F.; Yim, I.S.; Wanyonyi, S.; Merali, M.; Musana, W.; Omuse, G.; Forcheh, N.; Dosani, A.; et al. Adverse Childhood Experiences and Changing Levels of Psychosocial Distress Scores across Pregnancy in Kenyan Women. Int. J. Environ. Res. Public Health 2020, 17, 3401. https://doi.org/10.3390/ijerph17103401
Samia P, Premji S, Tavangar F, Yim IS, Wanyonyi S, Merali M, Musana W, Omuse G, Forcheh N, Dosani A, et al. Adverse Childhood Experiences and Changing Levels of Psychosocial Distress Scores across Pregnancy in Kenyan Women. International Journal of Environmental Research and Public Health. 2020; 17(10):3401. https://doi.org/10.3390/ijerph17103401
Chicago/Turabian StyleSamia, Pauline, Shahirose Premji, Farideh Tavangar, Ilona S. Yim, Sikolia Wanyonyi, Mohamoud Merali, Wangira Musana, Geoffrey Omuse, Ntonghanwah Forcheh, Aliyah Dosani, and et al. 2020. "Adverse Childhood Experiences and Changing Levels of Psychosocial Distress Scores across Pregnancy in Kenyan Women" International Journal of Environmental Research and Public Health 17, no. 10: 3401. https://doi.org/10.3390/ijerph17103401
APA StyleSamia, P., Premji, S., Tavangar, F., Yim, I. S., Wanyonyi, S., Merali, M., Musana, W., Omuse, G., Forcheh, N., Dosani, A., Letourneau, N., & MIGHT Consortium. (2020). Adverse Childhood Experiences and Changing Levels of Psychosocial Distress Scores across Pregnancy in Kenyan Women. International Journal of Environmental Research and Public Health, 17(10), 3401. https://doi.org/10.3390/ijerph17103401








