The Effect of Heart Rate Variability Biofeedback Training on Mental Health of Pregnant and Non-Pregnant Women: A Randomized Controlled Trial
Abstract
1. Introduction
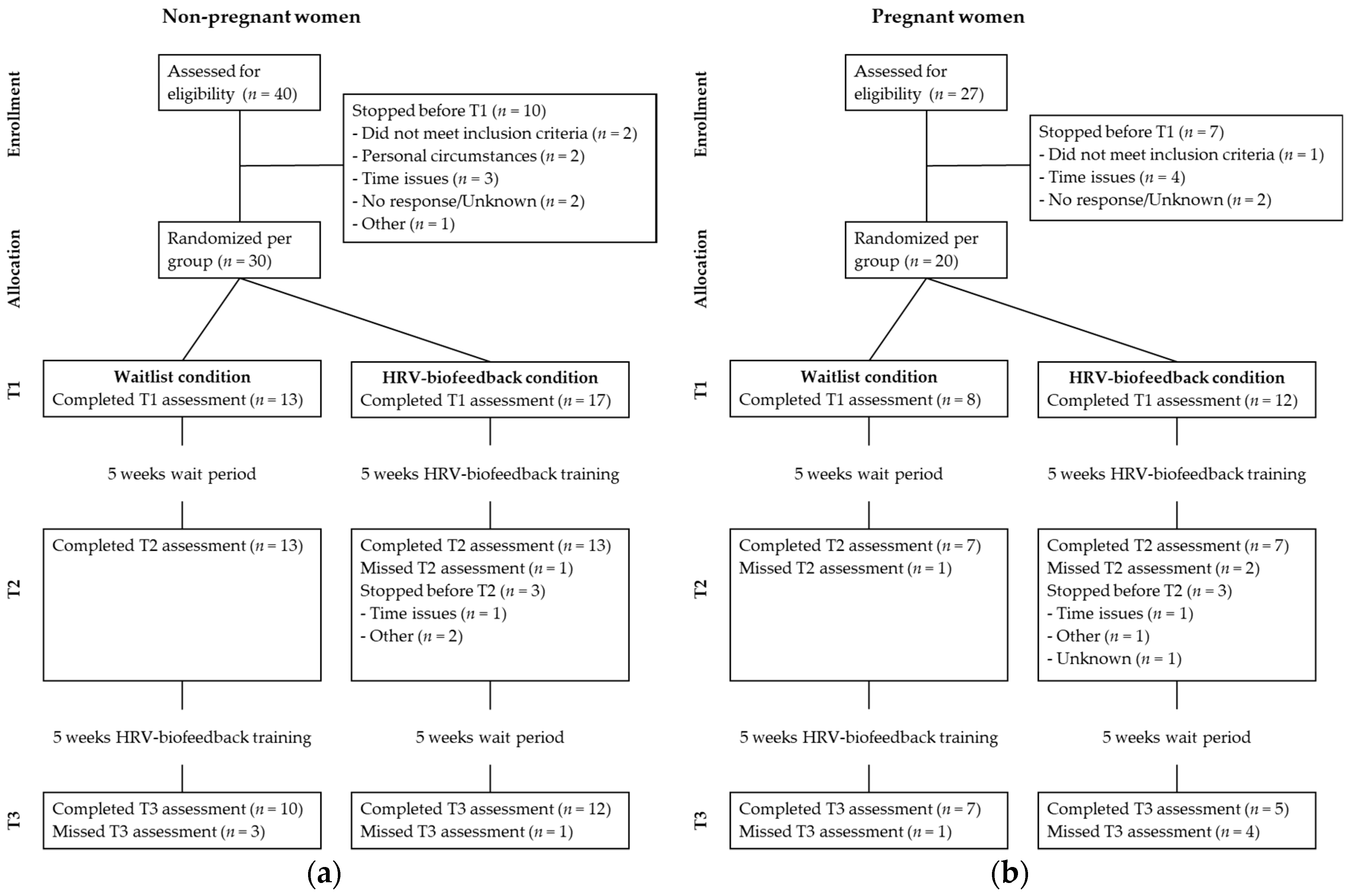
2. Materials and Methods
2.1. Participants and Recruitment
2.2. Experimental Procedures
2.3. Outcome Measures
2.4. Stress-Reducing Intervention
2.5. HRV-Biofeedback
2.6. Treatment Adherence
2.7. Statistical Analyses
3. Results
3.1. Sample Characteristics
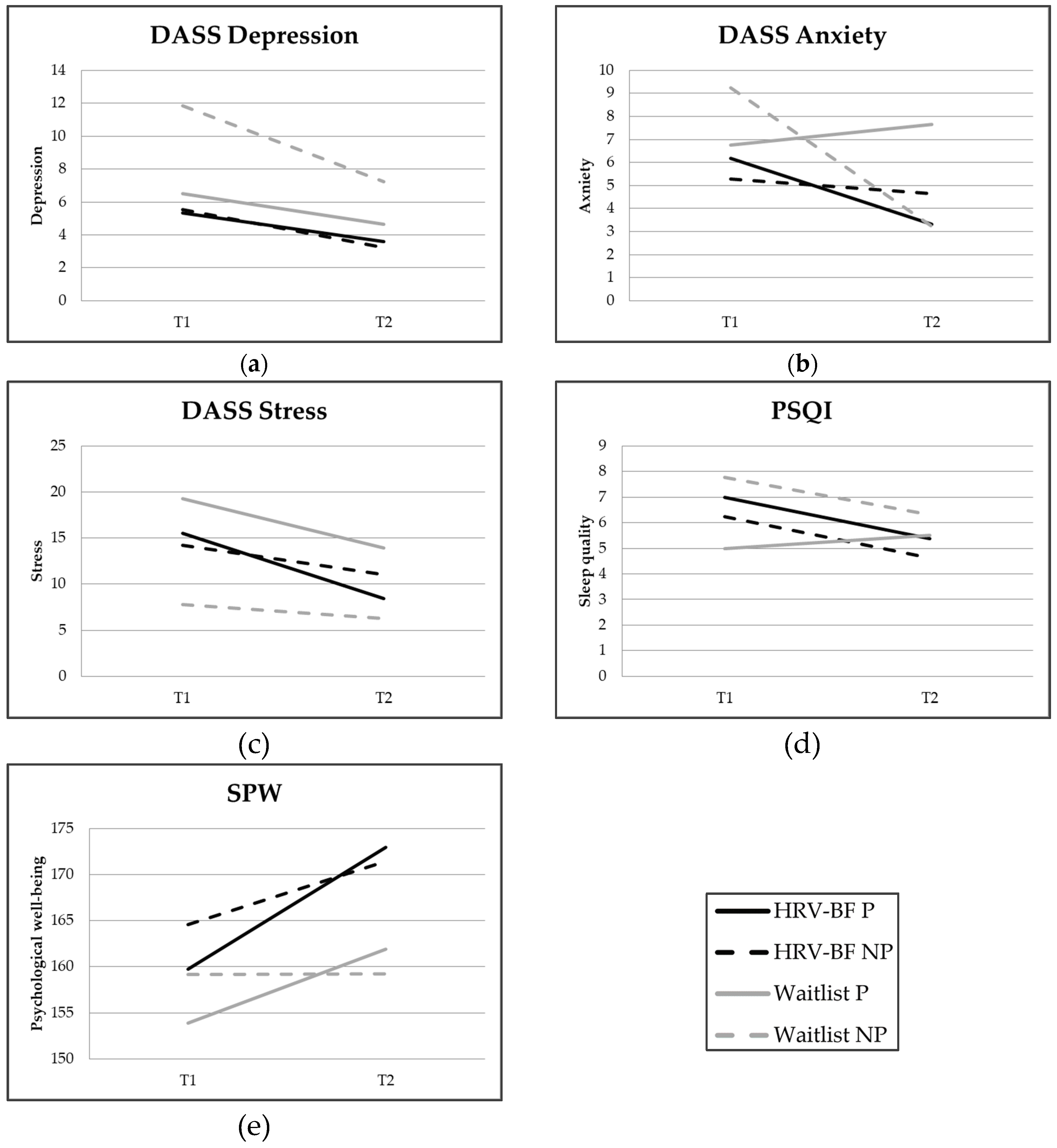
3.2. Change over Time
3.3. Pregnant and Non-Pregnant Women
3.4. Sensitivity Analyses
3.5. Adherence
4. Discussion
4.1. Limitations and Strengths
4.2. Future Research
4.3. Clinical Implications
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kessler, R.C.; Petukhova, M.; Sampson, N.A.; Zaslavsky, A.M.; Wittchen, H.U. Twelve-month and lifetime prevalence and lifetime morbid risk of anxiety and mood disorders in the United States. Int. J. Methods Psychiatr. Res. 2012, 21, 169–184. [Google Scholar] [CrossRef] [PubMed]
- Wiegner, L.; Hange, D.; Bjorkelund, C.; Ahlborg, G. Prevalence of perceived stress and associations to symptoms of exhaustion, depression and anxiety in a working age population seeking primary care—An observational study. BMC Fam. Pract. 2015, 16, 38. [Google Scholar] [CrossRef] [PubMed]
- WHO. Mental Health Action Plan 2013–2020. 2013. Available online: http://www.who.int/mental_health/publications/action_plan/en/ (accessed on 2 May 2017).
- EU-OSHA. Calculating the Costs of Work-Related Stress and Psychosocial Risks—A Literature Review. The Business Case for Managing Stress and Psychosocial Risks. 2014. Available online: https://osha.europa.eu/en (accessed on 2 May 2017).
- McManus, I.C.; Winder, B.C.; Gordon, D. The causal links between stress and burnout in a longitudinal study of UK doctors. Lancet 2002, 359, 2089–2090. [Google Scholar] [CrossRef]
- Hammen, C. Stress and depression. Annu. Rev. Clin. Psychol. 2004, 1, 293–319. [Google Scholar] [CrossRef] [PubMed]
- Kendler, K.S.; Hettema, J.M.; Butera, F.; Gardner, C.O.; Prescott, C.A. Life event dimensions of loss, humiliation, entrapment, and danger in the prediction of onsets of major depression and generalized anxiety. Arch. Gen. Psychiatry 2003, 60, 789–796. [Google Scholar] [PubMed]
- Schneiderman, N.; Ironson, G.; Siegel, S.D. Stress and health: Psychological, behavioral, and biological determinants. Annu. Rev. Clin. Psychol. 2005, 1, 607–628. [Google Scholar] [CrossRef] [PubMed]
- Backe, E.M.; Seidler, A.; Latza, U.; Rossnagel, K.; Schumann, B. The role of psychosocial stress at work for the development of cardiovascular diseases: A systematic review. Int. Arch. Occup. Environ. Health 2012, 85, 67–79. [Google Scholar] [CrossRef]
- Lehrer, P.M.; Gevirtz, R. Heart rate variability biofeedback: How and why does it work? Front. Psychol. 2014, 5, 756. [Google Scholar]
- Holzman, J.B.; Bridgett, D.J. Heart rate variability indices as bio-markers of top-down self-regulatory mechanisms: A meta-analytic review. Neurosci. Biobehav. Rev. 2017, 74, 233–255. [Google Scholar] [CrossRef] [PubMed]
- Porges, S.; Doussard-Roosevelt, J.A.; Maiti, A.K. Vagal tone and the physiological regulation of emotion. Monogr. Soc. Res. Child Dev. 1994, 59, 167–186. [Google Scholar] [CrossRef]
- Goessl, V.C.; Curtiss, J.E.; Hofmann, S.G. The effect of heart rate variability biofeedback training on stress and anxiety: A meta-analysis. Psychol. Med. 2017, 47, 2578–2586. [Google Scholar] [CrossRef] [PubMed]
- Henriques, G.; Keffer, S.; Abrahamson, C.; Horst, S.J. Exploring the effectiveness of a computer-based heart rate variability biofeedback program in reducing anxiety in college students. Appl. Psychophysiol. Biofeedback 2011, 36, 101–112. [Google Scholar] [CrossRef] [PubMed]
- Van der Zwan, J.E.; De Vente, W.; Huizink, A.C.; Bögels, S.M.; De Bruin, E.I. Physical activity, mindfulness meditation, or heart rate variability biofeedback for stress reduction: A randomized controlled trial. Appl. Psychophysiol. Biofeedback 2015, 40, 257–268. [Google Scholar] [CrossRef] [PubMed]
- Kramer, M.S.; Lydon, J.; Seguin, L.; Goulet, L.; Kahn, S.R.; McNamara, H.; Genest, J.; Dassa, C.; Chen, M.F.; Sharma, S.; et al. Stress pathways to spontaneous preterm birth: The role of stressors, psychological distress, and stress hormones. Am. J. Epidemiol. 2009, 169, 1319–1326. [Google Scholar] [CrossRef] [PubMed]
- Gutteling, B.M.D. The effects of prenatal stress on temperament and problem behavior of 27-month-old toddlers. Eur. Child Adolesc. Psychiatry 2005, 14, 41–51. [Google Scholar] [CrossRef] [PubMed]
- Huizink, A.C.; de Medina, P.G.R.; Mulder, E.J.H.; Visser, G.H.A.; Buitelaar, J.K. Psychological measures of prenatal stress as predictors of infant temperament. J. Am. Acad. Child Adolesc. Psychiatry 2002, 41, 1078–1085. [Google Scholar] [CrossRef] [PubMed]
- Dunkel Schetter, C.; Tanner, L. Anxiety, depression and stress in pregnancy: Implications for mothers, children, research, and practice. Curr. Opin. Psychiatry 2012, 25, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Huizink, A.; Dick, D.; Sihvola, E.; Pulkkinen, L.; Rose, R.; Kaprio, J. Chernobyl exposure as stressor during pregnancy and behaviour in adolescent offspring. Acta Psychiatr. Scand. 2007, 116, 438–446. [Google Scholar] [CrossRef]
- O’Donnell, K.J.; Glover, V.; Barker, E.D.; O’Connor, T.G. The persisting effect of maternal mood in pregnancy on childhood psychopathology. Dev. Psychopathol. 2014, 26, 393–403. [Google Scholar] [CrossRef] [PubMed]
- Huizink, A.; Menting, B.; Moor, M.; Verhage, M.; Kunseler, F.; Schuengel, C.; Oosterman, M. From prenatal anxiety to parenting stress: A longitudinal study. Arch. Women’s Ment. Health 2017, 20, 663–672. [Google Scholar] [CrossRef] [PubMed]
- Glover, V. Maternal depression, anxiety and stress during pregnancy and child outcome; what needs to be done. Best Pract. Res. 2014, 28, 25–35. [Google Scholar] [CrossRef] [PubMed]
- Zijlmans, M.A.; Riksen-Walraven, J.; de Weerth, C. Associations between maternal prenatal cortisol concentrations and child outcomes: A systematic review. Neurosci. Biobehav. Rev. 2015, 53, 1–24. [Google Scholar] [CrossRef] [PubMed]
- Loomans, E.M.; van Dijk, A.E.; Vrijkotte, T.G.; van, E.M.; Stronks, K.; Gemke, R.J.; Van den Bergh, B.R. Psychosocial stress during pregnancy is related to adverse birth outcomes: Results from a large multi-ethnic community-based birth cohort. Eur. J. Public Health 2013, 23, 485–491. [Google Scholar] [CrossRef] [PubMed]
- Fontein-Kuipers, Y.J.; Nieuwenhuijze, M.J.; Ausems, M.; Bude, L.; De Vries, R. Antenatal interventions to reduce maternal distress: A systematic review and meta-analysis of randomised trials. BJOG 2014, 121, 389–397. [Google Scholar] [CrossRef]
- Cullins, S.; Gevirtz, R.; Poeltler, D.; Cousins, L.; Edward Harpin, R.; Muench, F. An exploratory analysis of the utility of adding cardiorespiratory biofeedback in the standard care of pregnancy-induced hypertension. Appl. Psychophysiol. Biofeedback 2013, 38, 161–170. [Google Scholar] [CrossRef] [PubMed]
- Siepmann, M.; Hennig, U.D.; Siepmann, T.; Nitzsche, K.; Muck-Weymann, M.; Petrowski, K.; Weidner, K. The effects of heart rate variability biofeedback in patients with preterm labour. Appl. Psychophysiol. Biofeedback 2014, 39, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Soma-Pillay, P.; Nelson-Piercy, C.; Tolppanen, H.; Mebazaa, A. Physiological changes in pregnancy. Cardiovasc. J. Afr. 2016, 27, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Balajewicz-Nowak, M.; Furgala, A.; Pitynski, K.; Thor, P.; Huras, H.; Rytlewski, K. The dynamics of autonomic nervous system activity and hemodynamic changes in pregnant women. Neuroendocrinol. Lett. 2016, 37, 70–77. [Google Scholar] [PubMed]
- Reiner, R. Integrating a portable biofeedback device into clinical practice for patients with anxiety disorders: Results of a pilot study. Appl. Psychophysiol. Biofeedback 2008, 33, 55–61. [Google Scholar] [CrossRef]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef]
- Cohen, S.; Janicki-Deverts, D. Who’s stressed? Distributions of psychological stress in the united states in probability samples from 1983, 2006, and 2009. J. Appl. Soc. Psychol. 2012, 42, 1320–1334. [Google Scholar] [CrossRef]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [PubMed]
- De Beurs, E.; Van Dyck, R.; Marquenie, L.A.; Lange, A.; Blonk, R.W.B. De DASS: Een vragenlijst voor het meten van depressie, angst en stress [The DASS: A questionnaire for measuring depression, anxiety and stress]. Gedragstherapie 2001, 34, 35–53. [Google Scholar]
- Buysse, D.J.; Reynolds, C.F.; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh sleep quality index—A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Ryff, C.D.; Keyes, C.L.M. The structure of psychological well-being revisited. J. Personal. Soc. Psychol. 1995, 69, 719–727. [Google Scholar] [CrossRef]
- Van Dierendonck, D. The construct validity of Ryff’s Scales of Psychological Well-being and its extension with spiritual well-being. Personal. Indiv. Diff. 2004, 36, 629–643. [Google Scholar] [CrossRef]
- De Vente, W.; Van der Zwan, J.E. Protocol for HRV Biofeedback Course A’dem (manual); Vrije Universiteit Amsterdam: Amsterdam, The Netherlands, 2014. [Google Scholar]
- Lehrer, P.M.V.; Vaschillo, E.; Vaschillo, B. Resonant frequency biofeedback training to increase cardiac variability: Rationale and manual for training. Appl. Psychophysiol. Biofeedback 2000, 25, 177–191. [Google Scholar] [CrossRef] [PubMed]
- Vaschillo, E.G.V.; Vaschillo, B.; Lehrer, P.M. Characteristics of resonance in heart rate variability stimulated by biofeedback. Appl. Psychophysiol. Biofeedback 2006, 31, 129–142. [Google Scholar] [CrossRef] [PubMed]
- Shaffer, F.; Combatalade, D.C. Don’t Add or miss a beat: A guide to cleaner heart rate variability recordings. Biofeedback 2013, 41, 121–130. [Google Scholar] [CrossRef]
- Committee for Medicinal Products for Human Use. Guidline on Missing Data in Confirmatory Clinical Trials. Revision 1—Adopted Guideline. 2010. Available online: https://www.ema.europa.eu/en/missing-data-confirmatory-clinical-trials (accessed on 5 January 2019).
- Barnard, J.; Rubin, D.B. Small-sample degrees of freedom with multiple imputation. Biometrika 1999, 86, 948–955. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Erlbaum: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Sutarto, A.; Wahab, N.; Mat Zin, N. Resonant Breathing Biofeedback Training for Stress Reduction among Manufacturing Operators. Int. J. Occup. Saf. Ergon. 2012, 18, 549–561. [Google Scholar] [CrossRef] [PubMed]
- Ratanasiripong, P.; Ratanasiripong, N.; Kathalae, D. Biofeedback intervention for stress and anxiety among nursing students: A randomized controlled trial. ISRN Nurs. 2012, 2012, 827972. [Google Scholar] [CrossRef] [PubMed]
- Lovibond, S.H.; Lovibond, P.F. Manual for the Depression Anxiety Stress Scale; The Psychology Foundation of Australia: Sydney, Australia, 1995. [Google Scholar]
- Meier, N.F.; Welch, A.S. Walking versus biofeedback: A comparison of acute interventions for stressed students. Anxiety Stress Coping 2016, 29, 463–478. [Google Scholar] [CrossRef] [PubMed]
- Prinsloo, G.E.; Rauch, H.G.L.; Lambert, M.I.; Muench, F.; Noakes, T.D.; Derman, W.E. The effect of short duration heart rate variability (HRV) biofeedback on cognitive performance during laboratory induced cognitive stress. Appl. Cognit. Psychol. 2011, 25, 792–801. [Google Scholar] [CrossRef]
- Figueiredo, B.; Conde, A. Anxiety and depression symptoms in women and men from early pregnancy to 3-months postpartum: Parity differences and effects. J. Affect. Disord. 2011, 132, 146–157. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.M.; Lam, S.K.; Mun Lau, S.M.S.; Chong, C.S.Y.; Chui, H.W.; Fong, D.Y.T. Prevalence, course, and risk factors for antenatal anxiety and depression. Obstet. Gynecol. 2007, 110, 1102–1112. [Google Scholar] [CrossRef] [PubMed]
- Rallis, S.; Skouteris, H.; McCabe, M.; Milgrom, J. A prospective examination of depression, anxiety and stress throughout pregnancy. Women Birth 2014, 27, E36–E42. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Total | Waitlist | HRV-BF | T or χ2 | p Value | Effect Size |
|---|---|---|---|---|---|---|
| N = 50 | n = 21 | n = 29 | ||||
| Age (years) (mean, SD) | 31.6 (5.9) | 31.3 (6.1) | 31.8 (5.9) | T(48) = −0.31 | 0.760 | 0.09 3 |
| Level of education (n, %) | χ2(3) = 3.29 | 0.349 | 0.15 2 | |||
| High school | 6 (12.0) | 2 (9.5) | 4 (13.8) | |||
| Lower vocational school | 3 (6.0) | - | 3 (10.3) | |||
| Higher vocational school | 11 (22.0) | 4 (19.0) | 7 (24.1) | |||
| University | 30 (60.0) | 15 (71.4) | 15 (51.7) | |||
| Work (n, %) | χ2(3) = 5.43 | 0.143 | 0.19 2 | |||
| College | 9 (18.0) | 5 (23.8) | 4 (13.8) | |||
| Full-time | 14 (28.0) | 7 (33.3) | 7 (24.1) | |||
| Part-time | 17 (34.0) | 8 (38.1) | 9 (31.0) | |||
| Unemployed/On leave | 10 (20.0) | 1 (4.8) | 9 (31.0) | |||
| Pregnancy (n, %) | χ2(1) = 0.06 | 0.815 | 0.03 2 | |||
| Non-pregnant | 30 (60.0) | 13 (61.9) | 17 (58.6) | |||
| Pregnant | 20 (40.0) | 8 (38.1) | 12 (41.4) | |||
| Parity (n, % of pregnant) | χ2(1) = 2.06 | 0.152 | 0.17 2 | |||
| Nulliparous | 13 (65.0) | 6 (75.0) | 7 (58.3) | |||
| Primiparous or multiparous | 7 (35.0) | 2 (25.0) | 5 (41.7) | |||
| GA 1 at T1 (mean, SD) | 19.33 (5.2) | 21.0 (4.9) | 18.2 (5.3) | T(18) = 1.2 | 0.243 | 0.56 3 |
| Measure | Condition | T1 | T2 | T3 1 | T1–T2 | T1–T3 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | T(df) | p | d | T(df) | p | d | ||
| DASS Depr. | Waitlist | 9.81 | 8.55 | 6.40 | 4.97 | 6.12 | 8.20 | −2.45 (19.21) | 0.024 | −0.46 | |||
| HRV-BF | 5.45 | 4.24 | 2.80 | 3.40 | 4.22 | 3.56 | −2.21 (19.20) | 0.039 | −0.47 | −1.00 (25.05) | 0.327 | −0.23 | |
| DASS Anx. | Waitlist | 8.29 | 8.30 | 4.90 | 4.66 | 6.12 | 6.50 | −2.07 (19.08) | 0.053 | −0.46 | |||
| HRV-BF | 5.66 | 4.28 | 4.10 | 4.08 | 3.89 | 4.57 | −1.71 (24.75) | 0.101 | −0.39 | −1.26 (22.74) | 0.220 | −0.30 | |
| DASS Stress | Waitlist | 17.71 | 9.26 | 13.00 | 6.76 | 12.82 | 9.06 | −3.06 (18.81) | 0.007 | −0.55 | |||
| HRV-BF | 14.76 | 5.33 | 9.60 | 6.24 | 9.56 | 7.18 | −4.52 (24.45) | <0.001 | −0.85 | −3.13 (20.99) | 0.005 | −0.64 | |
| PSQI | Waitlist | 6.71 | 3.21 | 6.05 | 2.63 | 5.50 | 2.71 | −1.48 (18.23) | 0.156 | −0.23 | |||
| HRV-BF | 6.55 | 4.15 | 4.70 | 2.66 | 4.20 | 1.93 | −1.98 (18.17) | 0.063 | −0.38 | −1.87 (9.98) | 0.091 | −0.37 | |
| SPW | Waitlist | 157.14 | 26.04 | 160.10 | 22.39 | 164.59 | 20.92 | 1.11 (18.53) | 0.283 | 0.12 | |||
| HRV-BF | 162.59 | 20.98 | 174.25 | 17.12 | 171.28 | 15.72 | 2.52 (12.60) | 0.026 | 0.38 | 2.65 (24.70) | 0.014 | 0.40 | |
| Predictors | Condition | Condition and Pregnancy | ||||||
|---|---|---|---|---|---|---|---|---|
| B | SE | t | p | B | SE | t | p | |
| DASS Depression | −1.40 | 1.08 | −1.30 | 0.193 | ||||
| Condition | −1.96 | 1.39 | −1.40 | 0.160 | ||||
| Pregnancy | −0.86 | 1.63 | −0.52 | 0.600 | ||||
| Condition × Pregnancy | 1.28 | 2.14 | 0.60 | 0.548 | ||||
| DASS Anxiety | −0.16 | 1.10 | −0.15 | 0.881 | ||||
| Condition | 2.55 | 1.28 | 1.99 | 0.046 | ||||
| Pregnancy | 5.13 | 1.55 | 3.31 | 0.001 | ||||
| Condition × Pregnancy | −6.73 | 1.97 | −3.42 | 0.001 | ||||
| DASS Stress | −1.57 | 1.47 | −1.07 | 0.286 | ||||
| Condition | −0.03 | 1.81 | −0.01 | 0.989 | ||||
| Pregnancy | 0.46 | 2.20 | 0.21 | 0.836 | ||||
| Condition × Pregnancy | −3.70 | 2.87 | −1.29 | 0.197 | ||||
| SPW | 8.48 | 3.26 | 2.60 | 0.009 | ||||
| Condition | 8.81 | 4.17 | 2.11 | 0.035 | ||||
| Pregnancy | 5.98 | 5.04 | 1.19 | 0.235 | ||||
| Condition × Pregnancy | −1.44 | 6.78 | −0.21 | 0.832 | ||||
| PSQI | −1.00 | 0.60 | −1.69 | 0.092 | ||||
| Condition | −1.10 | 0.81 | −1.36 | 0.173 | ||||
| Pregnancy | 0.23 | 1.06 | 0.21 | 0.831 | ||||
| Condition × Pregnancy | 0.22 | 1.33 | 0.17 | 0.866 | ||||
| Measure | Last Observation Carried Forward | High Training Subsample (Training Duration >400 min) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T1–T2 | T1–T3 | T1–T2 | T1–T3 | |||||||||
| T(df) | p | d | T(df) | p | d | T(df) | p | d | T(df) | p | d | |
| DASS Depression | −1.82 (28) | 0.080 | −0.21 | −1.10 (28) | 0.279 | −0.15 | −1.73 (9.61) | 0.116 | −0.49 | −0.49 (12) | 0.632 | −0.15 |
| DASS Anxiety | −1.71 (28) | 0.098 | −0.27 | −1.57 (28) | 0.127 | −0.31 | −0.26 (10.20) | 0.802 | −0.07 | −0.27 (12) | 0.788 | −0.11 |
| DASS Stress | −3.83 (28) | 0.001 | −0.46 | −3.19 (28) | 0.004 | −0.46 | −2.15 (10.07) | 0.057 | −0.62 | −1.05 (12) | 0.315 | −0.26 |
| PSQI | −1.35 (28) | 0.188 | −0.14 | −1.05 (28) | 0.301 | −0.11 | −0.54 (10.17) | 0.598 | −0.16 | −0.50 (11) | 0.626 | −0.15 |
| SPW | 1.98 (28) | 0.058 | 0.14 | 2.42 (28) | 0.022 | 0.23 | 1.02 (9.86) | 0.334 | 0.18 | 0.63 (12) | 0.543 | −0.11 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
van der Zwan, J.E.; Huizink, A.C.; Lehrer, P.M.; Koot, H.M.; de Vente, W. The Effect of Heart Rate Variability Biofeedback Training on Mental Health of Pregnant and Non-Pregnant Women: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2019, 16, 1051. https://doi.org/10.3390/ijerph16061051
van der Zwan JE, Huizink AC, Lehrer PM, Koot HM, de Vente W. The Effect of Heart Rate Variability Biofeedback Training on Mental Health of Pregnant and Non-Pregnant Women: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2019; 16(6):1051. https://doi.org/10.3390/ijerph16061051
Chicago/Turabian Stylevan der Zwan, Judith Esi, Anja C. Huizink, Paul M. Lehrer, Hans M. Koot, and Wieke de Vente. 2019. "The Effect of Heart Rate Variability Biofeedback Training on Mental Health of Pregnant and Non-Pregnant Women: A Randomized Controlled Trial" International Journal of Environmental Research and Public Health 16, no. 6: 1051. https://doi.org/10.3390/ijerph16061051
APA Stylevan der Zwan, J. E., Huizink, A. C., Lehrer, P. M., Koot, H. M., & de Vente, W. (2019). The Effect of Heart Rate Variability Biofeedback Training on Mental Health of Pregnant and Non-Pregnant Women: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 16(6), 1051. https://doi.org/10.3390/ijerph16061051





