The Persistence of Oral Health Disparities for African American Children: A Scoping Review
Abstract
1. Introduction
2. Methods
2.1. Step One: Identifying the Research Question
2.2. Step Two: Identifying Relevant Studies
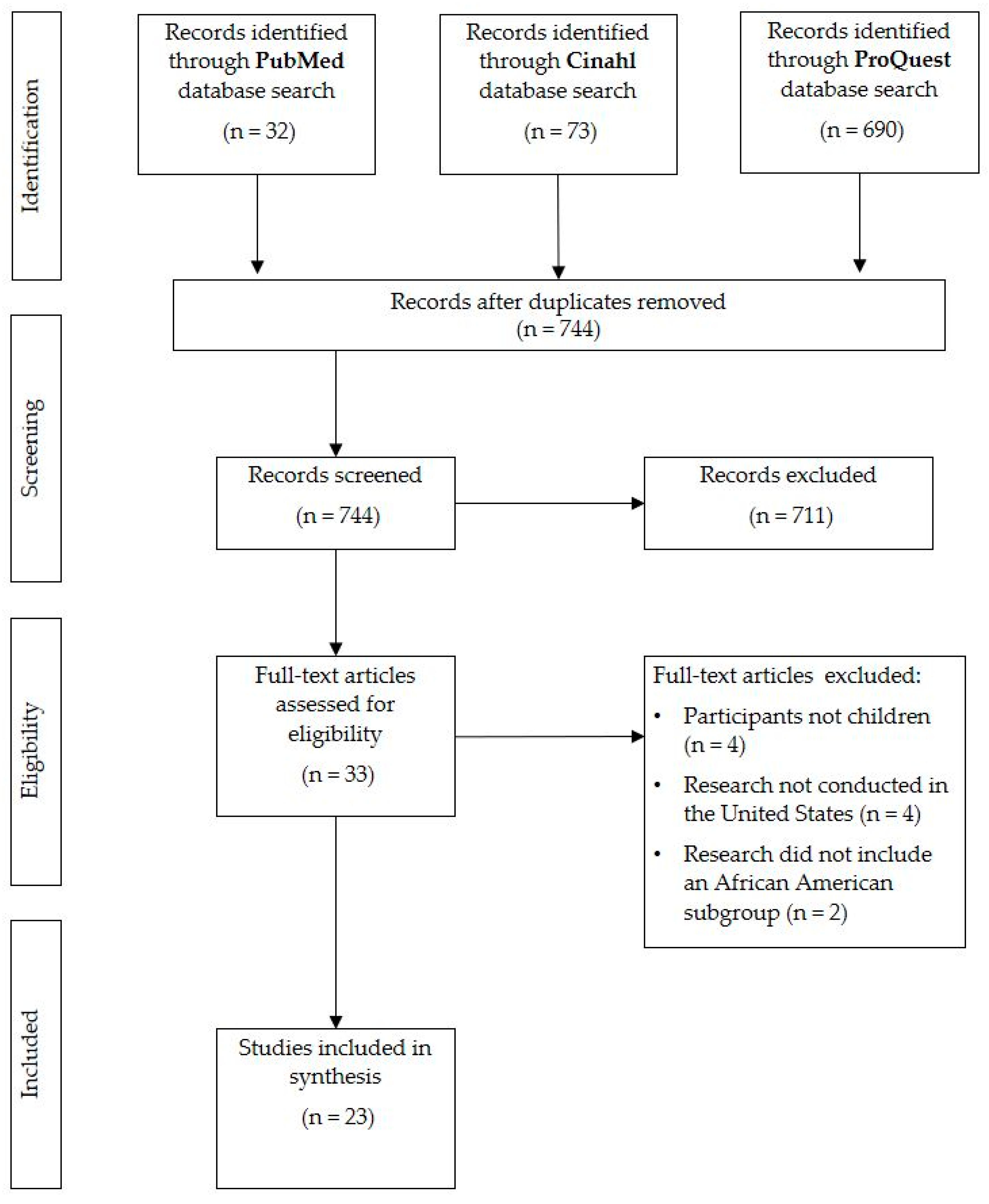
2.3. Step Three: Study Selection
2.4. Step Four: Charting the Data
2.5. Step Five: Collating, Summarizing, and Reporting the Results
3. Results
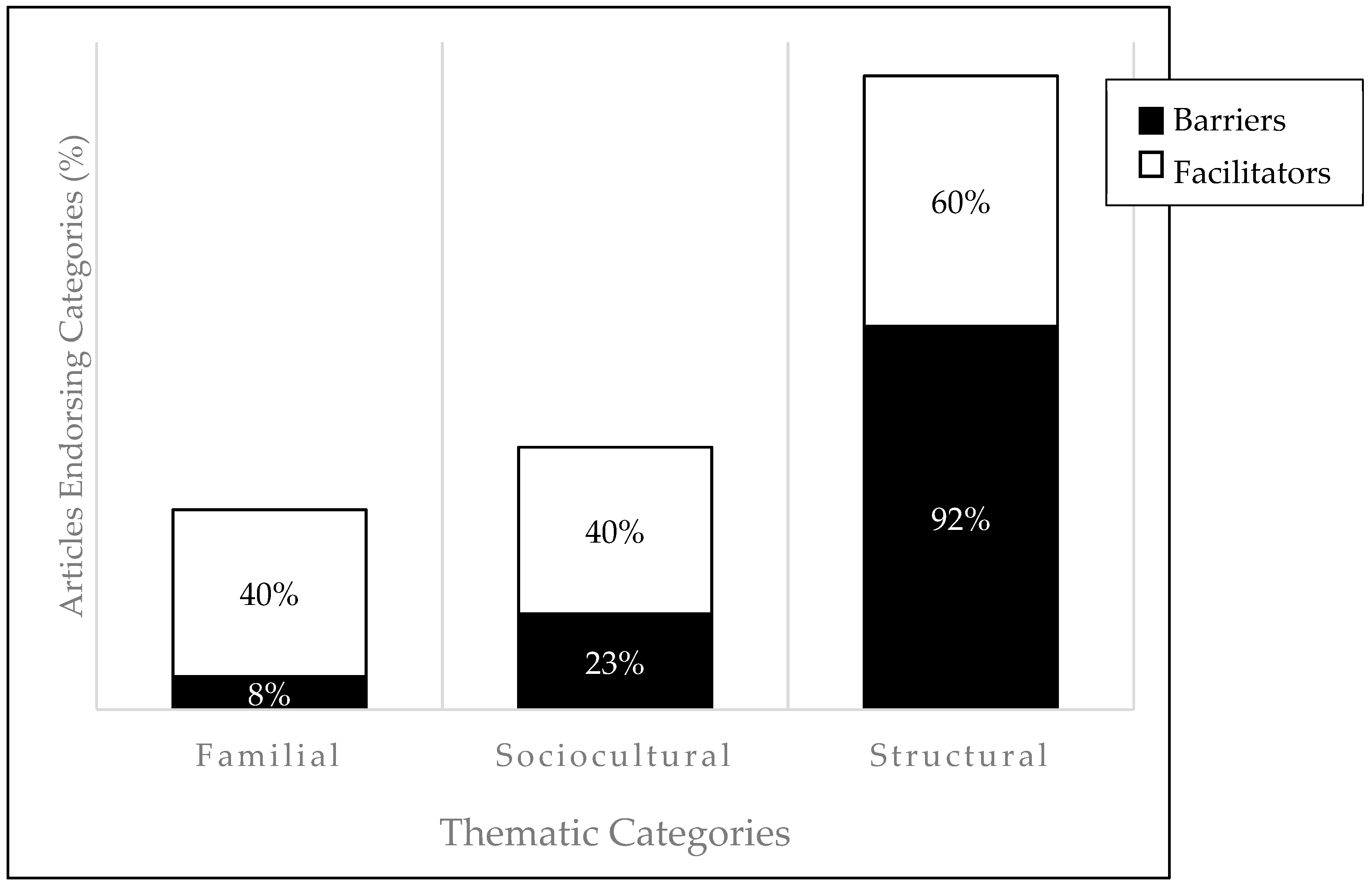
3.1. Descriptive Summary
3.1.1. Familial
3.1.2. Sociocultural
3.1.3. Structural
4. Discussion
Future Directions
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- U.S. Department of Health and Human Services. Oral Health in America: A Report of the Surgeon General; U.S. Department of Health and Human Services, National Institute of Dental and Craniofacial Research, National Institutes of Health: Rockville, MD, USA, 2000.
- Murthy, V. Oral health in America, 2000 to present: Progress made, but challenges remain. Public Health Rep. 2000, 131, 224–225. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Health and Human Services. Healthy People 2020. 2016. Available online: https://www.healthypeople.gov/2020/topics-objectives/topic/oral-health. (accessed on 25 January 2017).
- Calderon, S.J.; Mallory, C. A systematic review of oral health behavior research in American adolescents. J. Sch. Nurs. 2014, 30, 396–403. [Google Scholar] [CrossRef] [PubMed]
- Jackson, S.L.; Vann, W.F.; Kotch, J.B.; Pahel, B.T.; Lee, J.Y. Impact of poor oral health on children’s school attendance and performance. Am. J. Public Health 2011, 101, 1900–1906. [Google Scholar] [CrossRef] [PubMed]
- Seirawan, H.; Faust, S.; Mulligan, R. The impact of oral health on the academic performance of disadvantaged children. Am. J. Public Health 2012, 102, 1729–1734. [Google Scholar] [CrossRef] [PubMed]
- Centers for Medicare & Medicaid Services. Children’s Health Insurance Program. n.d. Available online: https://www.medicaid.gov/chip/index.html (accessed on 25 January 2017).
- Centers for Disease Control and Prevention. Oral Health: School Based Dental Sealant Programs. 2016. Available online: https://www.cdc.gov/oralhealth/dental_sealant_program/ (accessed on 25 January 2017).
- Centers for Disease Control and Prevention. Oral Health: Community Water Fluoridation. 2016. Available online: https://www.cdc.gov/fluoridation/index.html (accessed on 25 January 2017).
- World Health Organization Expert Committee. Fluorides and Oral Health: WHO Technical Report Series; World Health Organization: Geneva, Switzerland, 1994. [Google Scholar]
- Flores, G.; Tomany-Korman, S.C. Racial and ethnic disparities in medical and dental health, access to care, and use of services in U.S. children. Pediatrics 2008, 121, e286–e298. [Google Scholar] [CrossRef] [PubMed]
- Dye, B.A.; Li, X.; Thornton-Evans, G. NCHS Data Brief on Oral Health Disparities as Determined by Selected Healthy People 2020 Oral Health Objectives for the United States, 2009–2010; National Center for Health Statistics: Hyattsville, MD, USA, 2012.
- Centers for Disease Control and Prevention. Oral Health in America: Summary of the Surgeon General’s Report. 2016. Available online: http://www.cdc.gov/oralhealth/publications/sgr2000_05.htm (accessed on 25 January 2017).
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- McLeroy, K.R.; Bibeau, D.; Steckler, A.; Glanz, K. An ecological perspective on health promotion programs. Health Educ. Q. 1988, 15, 351–377. [Google Scholar] [CrossRef] [PubMed]
- Behrens, D.; Lear, J. Strengthening children’s oral health: Views from the field. Health Aff. (Millwood) 2013, 30, 2208–2213. [Google Scholar] [CrossRef] [PubMed]
- Bhagavatula, P.; Xiang, Q.; Eichmiller, F.; Szabo, A.; Okunseri, C. Racial/Ethnic disparities in receipt of dental procedures amongst children enrolled in Delta Dental insurance in Milwaukee, Wisconsin. J. Public Health Dent. 2014, 74, 50–56. [Google Scholar] [CrossRef] [PubMed]
- Collins, C.; Villa-Torres, L.; Sams, L.; Zeldin, L.; Divaris, K. Framing young children’s oral health: A participatory action research project. PLoS ONE 2016, 11, E0161728. [Google Scholar] [CrossRef] [PubMed]
- Dawkins, E.; Michimi, A.; Ellis-Griffith, G.; Peterson, T.; Carter, D.; English, G. Dental caries among children visiting a mobile dental clinic in South Central Kentucky: A pooled cross-sectional study. BMC Oral Health 2013, 13, 19. [Google Scholar] [CrossRef] [PubMed]
- Dodd, V.J.; Logan, H.; Brown, C.D.; Calderon, A.; Catalanotto, F. Perceptions of oral health, preventive care, and care-seeking behaviors among rural adolescents. J. Sch. Health 2014, 84, 802–809. [Google Scholar] [CrossRef] [PubMed]
- Eisen, C.H.; Bowie, J.V.; Gaskin, D.J.; LaVeist, T.A.; Thorpe, R.J. The contribution of social and environmental factors to race differences in dental services use. J. Urban Health 2015, 92, 415–421. [Google Scholar] [CrossRef] [PubMed]
- Fisher-Owens, S.; Isong, I.A.; Soobader, M.; Gansky, S.A.; Weintraub, J.A.; Platt, L.J.; Newacheck, P.W. An examination of racial/ethnic disparities in children’s oral health in the United States. J. Public Health Dent. 2013, 73, 166–174. [Google Scholar] [CrossRef] [PubMed]
- Flores, G.; Lin, H. Trends in racial/ethnic disparities in medical and oral health, access to care, and use of services in US children: Has anything changed over the years? Int. J. Equity Health 2013, 12, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Flores, G.; Lin, H.; Walker, C.; Lee, M.; Portillo, A.; Henry, M.; Massey, K. A cross-sectional study of parental awareness of and reasons for lack of health insurance among minority children, and the impact on health, access to care, and unmet needs. Int. J. Equity Health 2016, 15, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Guarnizo-Herreño, C.; Wehby, G.L. Explaining Racial/Ethnic disparities in children’s dental health: A decomposition analysis. Am. J. Public Health 2012, 102, 859–866. [Google Scholar] [CrossRef] [PubMed]
- Isong, I.A.; Soobader, M.; Fisher-Owens, S.A.; Weintraub, J.A.; Gansky, S.A.; Platt, L.J.; Newacheck, P.W. Racial disparity trends in children’s dental visits: US national health interview survey, 1964–2010. Pediatrics 2012, 130, 306–314. [Google Scholar] [CrossRef] [PubMed]
- Lau, M.; Lin, H.; Flores, G. Racial/Ethnic disparities in health and health care among U.S. adolescents. Health Serv. Res. 2012, 47, 2031–2059. [Google Scholar] [CrossRef] [PubMed]
- Pourat, N.; Finocchio, L. Racial and ethnic disparities in dental care for publicly insured children. Health Aff. (Millwood) 2010, 29, 1356–1363. [Google Scholar] [CrossRef] [PubMed]
- Adams, S.H.; Rowe, C.R.; Gansky, S.A.; Cheng, N.F.; Barker, J.C.; Hyde, S. Caregiver acceptability and preferences for preventive dental treatments for young African American children. J. Public Health Dent. 2012, 72, 252–260. [Google Scholar] [CrossRef] [PubMed]
- Baker, A.D.; Gilley, J.; James, J.; Kimani, M. “High five to healthy living”: A health intervention program for youth at an inner-city community center. J. Community Health 2012, 37, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Devlin, D.; Henshaw, M. Improving access to preventive dental services through a school-based dental sealant program. J. Dent. Hyg. 2011, 85, 211–219. [Google Scholar] [PubMed]
- Ghazal, T.; Levy, S.; Childers, N.; Broffitt, B.; Cutter, G.; Wiener, H.; Cavanaugh, J. Factors associated with early childhood caries incidence among high caries-risk children. Community Dent. Oral Epidemiol. 2015, 43, 366–374. [Google Scholar] [CrossRef] [PubMed]
- Heima, M.; Lee, W.; Milgrom, P.; Nelson, S. Caregiver’s education level and child’s dental caries in African Americans: A path analytic study. Caries Res. 2015, 49, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Ismail, A.I.; Ondersma, S.; Willem Jedele, J.M.; Little, R.J.; Lepkowski, J.M. Evaluation of a brief tailored motivational intervention to prevent early childhood caries. Community Dent. Oral Epidemiol. 2011, 39, 433–448. [Google Scholar] [CrossRef] [PubMed]
- Johansson, I.; Lif Holgerson, P.; Kressin, N.R.; Nunn, M.E.; Tanner, A.C. Snacking habits and caries in young children. Caries Res. 2010, 44, 421–430. [Google Scholar] [CrossRef] [PubMed]
- Nelson, S.; Mandelaris, J.; Ferretti, G.; Heima, M.; Spiekerman, C.; Milgrom, P. School screening and parental reminders in increasing dental care for children in need: A retrospective cohort study. J Public Health Dent. 2012, 72, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Weatherwax, J.; Bray, K.; Williams, K.; Gadbury-Amyot, C. Exploration of the relationship between parent/guardian sociodemographic, intention, and knowledge and the oral health status of their children/wards enrolled in a central Florida Head Start program. Int. J. Dent. Hyg. 2015, 13, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Yuen, H.K.; Wiegand, R.E.; Hill, E.G.; Magruder, K.M.; Slate, E.H.; Salinas, C.F.; London, S.D. Factors associated with toothache among African American adolescents living in rural South Carolina. Soc. Work Public Health 2011, 26, 695–707. [Google Scholar] [CrossRef] [PubMed]
- Edelstein, B.L. Disparities in oral health and access to care: Findings of national surveys. Ambul. Pediatr. 2002, 2, 141–147. [Google Scholar] [CrossRef]
- Waldman, H.B.; Ackerman, M.B.; Perlman, S.P. Increasing use of dental services by children, but many are unable to secure needed care. J. Clin. Pediatr. Dent. 2014, 39, 9–11. [Google Scholar] [CrossRef] [PubMed]
- Kelesidis, N. A racial comparison of sociocultural factors and oral health perceptions. J. Dent. Hyg. 2014, 88, 173–182. [Google Scholar] [PubMed]
- Gamble, V.N. Under the shadow of Tuskegee: African Americans and health care. Am. J. Public Health 1997, 87, 1773–1778. [Google Scholar] [CrossRef] [PubMed]
- Tajeu, G.S.; Cherrington, A.L.; Andreae, L.; Prince, C.; Holt, C.L.; Halanych, J.H. “We’ll get to you when we get to you”: Exploring potential contributions of health care staff behaviors to patient perceptions of discrimination and satisfaction. Am. J. Public Health 2015, 105, 2076–2082. [Google Scholar] [CrossRef] [PubMed]
- Siegel, K.; Schrimshaw, E.; Kunzel, C.; Wolfson, N.; Moon-Howard, J.; Moats, H.; Mitchell, D. Types of dental fear as barriers to dental care among African American adults with oral health symptoms in Harlem. J. Health Care Poor Underserved 2012, 23, 1294–1309. [Google Scholar] [CrossRef] [PubMed]
- Habibian, M.; Seirawan, H.; Mulligan, R. Dental students’ attitudes toward underserved populations across four years of dental school. J. Dent. Educ. 2011, 75, 1020–1029. [Google Scholar] [PubMed]
- Muskat, B.; Burnham Riosa, P.; Nicholas, D.B.; Roberts, W.; Stoddart, K.P.; Zwaigenbaum, L. Autism comes to the hospital: The experiences of patients with autism spectrum disorder, their parents and health-care providers at two Canadian paediatric hospitals. Autism 2015, 19, 482–490. [Google Scholar] [CrossRef] [PubMed]
- Tregnago, M.K.; Cheak-Zamora, N.C. Systematic review of disparities in health care for individuals with autism spectrum disorders in the united states. Res. Autism Spectr. Disord. 2012, 6, 1023–1031. [Google Scholar] [CrossRef]
- American Dental Association Health Policy Institute. The Dentist Workforce: Key Facts. 2015. Available online: https://www.ada.org/~/media/ADA/Science%20and%20Research/HPI/Files/HPIgraphic_0716_1.pdf?la=en (accessed on 25 March 2018).
- National Dental Association. About Us. 2018. Available online: http://www.ndaonline.org (accessed on 25 March 2018).
- Chi, D.; Masterson, E.; Carle, A.C.; Mancl, L.A.; Coldwell, S.E. Socioeconomic status, food security, and dental caries in US children: Mediation analyses of data from the National Health and Nutrition Examination Survey, 2007–2008. Am. J. Public Health 2014, 104, 860–864. [Google Scholar] [CrossRef] [PubMed]
- U.S. Department of Agriculture. Economic Research Center. Definitions of Food Security. 2017. Available online: https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/definitions-of-food-security/#ranges (accessed on 17 November 2017).
- Liburd, L.C. Food, identity, and African-American women with type 2 diabetes: An anthropological perspective. Diabetes Spectr. 2003, 16, 160–165. [Google Scholar] [CrossRef]
- U.S. Department of Health and Human Services. Healthy People 2020. 2019. Available online: https://www.healthypeople.gov/2020/data/disparities/summary/Chart/5028/4. (accessed on 18 February 2019).
- World Health Organization. Health Topics: Adolescent Health. 2018. Available online: https://www.who.int/topics/adolescent_health/en/ (accessed on 21 March 2018).
- Pederson, S.; Gronhoj, A.; Thogersen, J. Following family or friends. Social norms in adolescent healthy eating. Appetite 2015, 86, 54–60. [Google Scholar] [CrossRef] [PubMed]
- Loth, K.A.; MacLehose, R.F.; Larson, N.; Berge, J.M.; Neumark-Sztainer, D. Food availability, modeling and restriction: How are these different aspects of the family eating environment related to adolescent dietary intake? Appetite 2016, 96, 80–86. [Google Scholar] [CrossRef] [PubMed]
- Vann, W.F.; Lee, J.Y.; Baker, D.; Divaris, K. Oral health literacy among female caregivers: Impact on oral health outcomes in early childhood. J. Dent. Res. 2010, 89, 1395–1400. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Introduction to Public Health. 2016. Available online: http://www.cdc.gov/publichealth101/public-health.html (accessed on 25 January 2017).
- Dickie, V.; Cutchin, M.; Humphry, R. Occupation as transactional experience: A critique of individualism in occupational science. J. Occup. Sci. 2006, 13, 83–93. [Google Scholar] [CrossRef]
- Institute for Healthcare Improvement. IHI Triple Aim Initiative. 2017. Available online: http://www.ihi.org/Engage/Initiatives/TripleAim/Pages/default.aspx (accessed on 25 January 2017).
| Reference | Purpose | Population | Study Design | Key Findings | Category |
|---|---|---|---|---|---|
| Behrens et al. [16] | To explore factors and identify strategies that could improve the oral health of low income and minority children | 25 state and federal policy makers, workforce experts, foundation officials, educators, researchers with interest in children’s oral health | Qualitative Study; interviews with stakeholder and policy makers | Policy stakeholders believe that improving oral health for children requires addressing: both consumer demand and provider supply, lack of outcry for accessible oral health, undervaluing oral health, health literacy and outreach campaigns | Structural |
| Bhagavatula et al. [17] | To document the rates of prevention, restoration, and surgical dental procedures provided to children enrolled in private insurance, Delta Dental | 266,380 children (age 0–18) (12% African American), that received care from 2002–2008 in Milwaukee | Descriptive study; registry summary design | 44% of AA had one dental visit during study period; rates of preventative procedures increased to age 9 and then decreased | Structural |
| Collins et al. [18] | To understand what parents consider to be important factors and resources that influence their child’s oral care | Utilized Photovoice with 10 parents of infants and toddlers; five group sessions were conducted | Qualitative Study; participatory research approach | Poor oral health was associated with avoidance of problems; financial constraints, time constraints, and occasional parental frustration completing child’s oral hygiene routines | Familial, Sociocultural, Structural |
| Dawkins et al. [19] | To compare sociodemographic differences between caries and no caries groups and investigate factors associated with untreated dental caries | 2453 participants (5.8% African American), children (age 6–15), school-based dental sealant program in KY | Observational Study; pooled cross-sectional design | Older children living in rural areas were more likely to have untreated dental caries and lack insurance | Structural |
| Dodd et al. [20] | To explore oral health perceptions and dental care behaviors among rural adolescents | 100 rural youth (age 12–18), (80% Black), low SES | Qualitative study; emergent thematic approach | Perceived threat from oral disease was low, esthetics main reason for seeking care; access, finances, transportation, and fear were also noted | Sociocultural |
| Eisen et al. [21] | Examine relationship between race and dental services | 1408 participants (59.3% African American) | Observational Study; cross-sectional analysis of data from The Exploring Health Disparities in Integrated Communities (Baltimore, MD) | More AA used dental services in previous 2 years; place of living an important factor to consider when seeking to understand race difference in dental service use | Structural |
| Fisher-Owens et al. [22] | To assess the extent that factors other than race explain disparities in children’s oral health | Data from National Survey of Children’s Health Children (n = 82,020) (age 2–17) | Observational Study; model based survey data analysis | AA more likely to report poor oral health, lack preventative care, and experience unmet need. However, these are attenuated, to varying degrees, when researchers adjust for socioeconomic status | Structural |
| Flores et al. [23] | To identify racial/ethnic disparities in medical and oral health, access to care, and uses of services in U.S. children | Sample from National Surveys of Children’s Health, parents of 90,117 children (age 0–17), (9.84% African American) | Descriptive study; secondary analysis | Disparities continue to exist, with increased use of services disparities decreased; however, several new disparities for African American children including uninsurance rates and difficulty getting specialty care | Structural |
| Flores et al. [24] | To examine parental awareness of and the reasons for lack of insurance coverage in eligible communities | 97 recruitment sites; 267 participants (age 0–18) (35% African American) | Observational Study; cross-sectional design | Half the participants were unaware that their children were eligible for federally funded insurance | Structural |
| Guarnizo-Herreño et al. [25] | To measure inequalities in children’s dental health based on racial/ethnic identity | Representative sample of children and adolescents (age 2–11); White, Black, Hispanic | Observational Study; decomposition model for analysis | SES accounted for 71% of the gap in preventive dental care between AA and White | Structural |
| Isong et al. [26] | To examine the impact of national health policies on AA children’s receipt of dental care | Children 2–17 years old; from 1964 to 2010 | Observational study | Percent of AA children without a dental visit declined significantly over time | Sociocultural, Structural |
| Lau et al. [27] | To examine racial/ethnic disparities in medical and oral health status, access to care and use of services in U.S. adolescents | 47,728 parent responses from National Surveys of Children’s Health for adolescents (age 10–17), (9.84% African American) | Descriptive study; secondary analysis | Suboptimal health and lack of personal doctor were found to be one of the most profound disparities to exist | Structural |
| Pourat et al. [28] | To look at racial and ethnic differences between children with private insurance and those in Medicaid or CHIP | Sample from the California Survey of Health, 10,805 children (age 0–11) (7% African American) | Descriptive study | AA with Medicare more likely to have longer intervals between visits than Caucasian children with Medicare | Structural |
| Reference | Purpose | Population | Study Design | Key Findings | Category |
|---|---|---|---|---|---|
| Adams et al. [29] | To determine AA parents’ treatment acceptability and treatment preferences to prevent early childhood caries | 48 parents/caregivers with an African American child (age 1–5) | Mixed method study; concurrent triangulation design | All treatments were acceptable; parents strongly preferred tooth brushing rather than fluoride varnish and the use of xylitol in gum or food | Familial |
| Baker et al. [30] | Provide developmental program focused on promoting healthy lifestyles to inner-city youth including one module focused on oral hygiene | 46 African American youth (age 11–14) | Experimental study; non-randomized controlled trial; 5-week module intervention | Surveys indicated that 42% of the participants exhibited positive behavioral change following completion of the oral hygiene module | Sociocultural |
| Devlin et al. [31] | To evaluate school-based dental sealant programs | Framingham school district 2nd graders (≈6% African American) with dental sealants | Experimental; non-randomized controlled trial | School based dental sealant programs can help decrease barriers for access to dental services | Structural |
| Ghazal et al. [32] | To assess the relationship between behavioral factors and caries in AA preschoolers | 96 African American children (age 3–22 months) | Observational study; longitudinal cohort study | Living in a non-fluoridated community, more frequent consumption of sweetened food, less frequent consumption of 100% juice, less frequent tooth brushing, significantly associated with greater ECC incidence. | Sociocultural, Structural |
| Heima et al. [33] | To investigate the influence of caregiver education level on dental caries | 423 children (age 5–6) and caregiver dyads (94% African American), low income, urban | Cross-sectional design; secondary analysis of longitudinal study data | Caregiver education level was associated with 34% less untreated decayed teeth | Familial |
| Ismail et al. [34] | To evaluate the effectiveness of a tailored intervention on oral health behaviors and new untreated caries | 1021 randomly selected African American children (age 0–5) and their caregivers | Experimental study; randomized controlled trial | Caregivers receiving motivational interviewing and watching DVD more likely to report checking for “pre-cavities” | Familial |
| Johansson et al. [35] | To investigate the association between snacking and caries | 1206 preschool children (age 1–4) (61% African American) | Observational study; cross-sectional design | Presence of plaque, sugar intake and SES were associated; consumption of chips was associated with caries | Sociocultural, Structural |
| Nelson et al. [36] | To assess follow-up dental care received by children given baseline screening and referrals as part of an ongoing clinical trial | 303 participants (age 5–6), (96% African American), who had at least one dental visit | Observational study; retrospective cohort design | Utilization of dental services was low for poor minority inner city kindergarten children despite school screening referrals and parental reminders | Structural |
| Weatherwax et al. [37] | To identify possible relationships between parent/guardian sociodemographic, intention, knowledge, and oral health status of their child | 181 child (age 3–5) and parent/ caregiver dyad (31% African American), Head Start program | Observational study; cross-sectional design | Caregiver race/ethnicity and years of education were inversely significantly associated with decayed, missing or filled teeth | Familial, Structural |
| Yuen et al. [38] | To explore behavioral factors associated with toothaches among African American adolescents | Convenience sample of 156 African American adolescents (age 10–18) | Observational study; cross-sectional design | Age and consumption of cariogenic snacks and soda are related to toothache pain | Sociocultural, Structural |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Como, D.H.; Stein Duker, L.I.; Polido, J.C.; Cermak, S.A. The Persistence of Oral Health Disparities for African American Children: A Scoping Review. Int. J. Environ. Res. Public Health 2019, 16, 710. https://doi.org/10.3390/ijerph16050710
Como DH, Stein Duker LI, Polido JC, Cermak SA. The Persistence of Oral Health Disparities for African American Children: A Scoping Review. International Journal of Environmental Research and Public Health. 2019; 16(5):710. https://doi.org/10.3390/ijerph16050710
Chicago/Turabian StyleComo, Dominique H., Leah I. Stein Duker, José C. Polido, and Sharon A. Cermak. 2019. "The Persistence of Oral Health Disparities for African American Children: A Scoping Review" International Journal of Environmental Research and Public Health 16, no. 5: 710. https://doi.org/10.3390/ijerph16050710
APA StyleComo, D. H., Stein Duker, L. I., Polido, J. C., & Cermak, S. A. (2019). The Persistence of Oral Health Disparities for African American Children: A Scoping Review. International Journal of Environmental Research and Public Health, 16(5), 710. https://doi.org/10.3390/ijerph16050710






