Screening of Forestry Workers in Guadalajara Province (Spain) for Antibodies to Lymphocytic Choriomeningitis Virus, Hantavirus, Rickettsia spp. and Borrelia burgdorferi
Abstract
1. Introduction
2. Materials and Methods
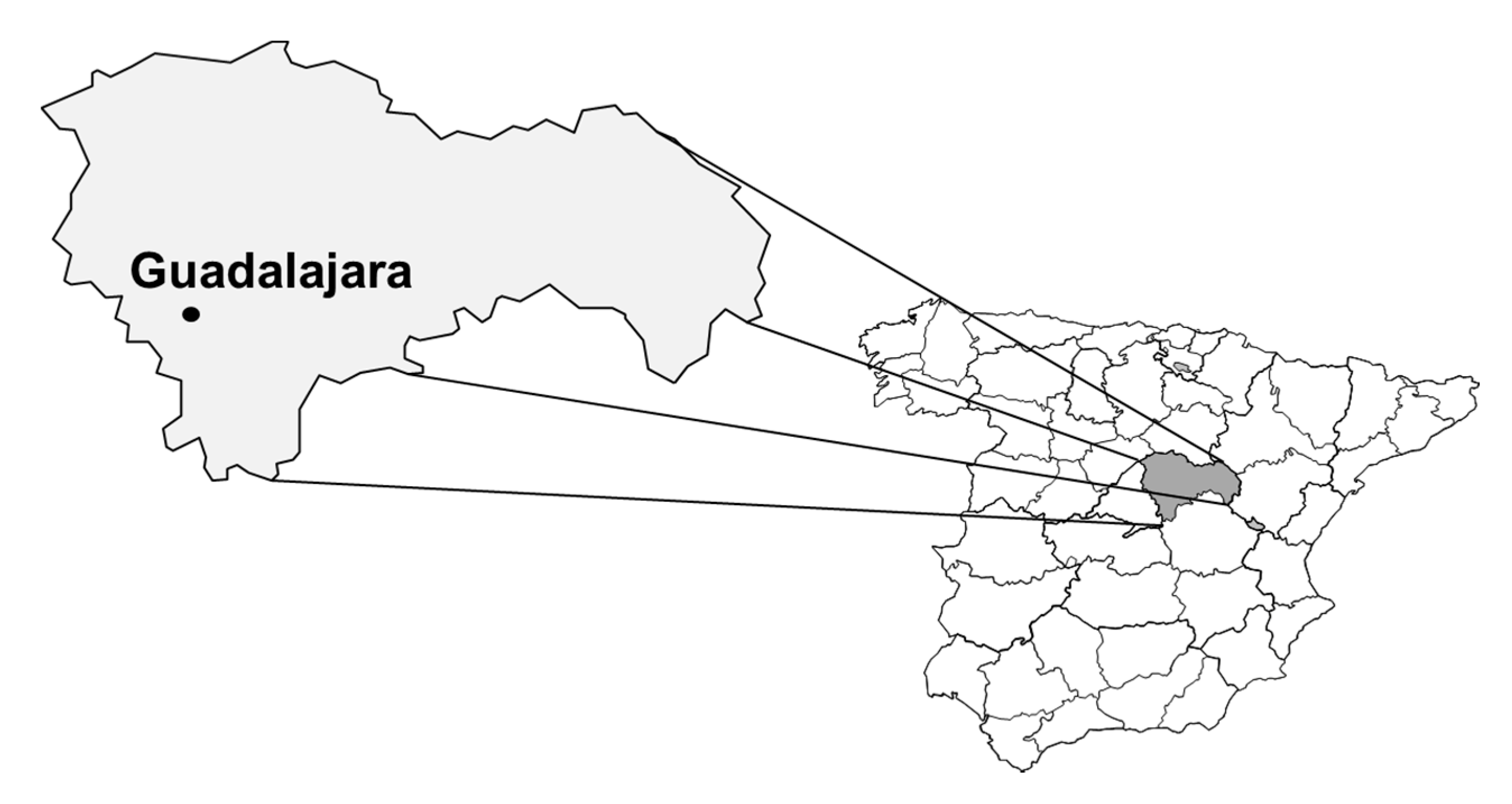
2.1. Study Area
2.2. Serum Samples
2.3. Immunofluorescence
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Chmielewska-Badora, J.; Moniuszko, A.; Żukiewicz-Sobczak, W.; Zwoliński, J.; Piątek, J.; Pancewicz, S. Serological survey in persons occupationally exposed to tick-borne pathogens in cases of co-infections with Borrelia burgdorferi, Anaplasma phagocytophilum, Bartonella spp. and Babesia microti. Ann. Agric. Environ. Med. 2012, 19, 271–274. [Google Scholar]
- Verhaegh, E.M.; Moudrous, W.; Buiting, A.G.; van der Eijk, A.A.; Tijssen, C.C. Meningitis after a mouse bite. Ned. Tijdschr. Geneeskd. 2014, 158, 7033–7037. [Google Scholar]
- Perez-Ruiz, M.; Navarro-Marí, J.-M.; Sánchez-Seco, M.-P.; Gegúndez, M.-I.; Palacios, G.; Savji, N.; Lipkin, W.I.; Fedele, G.; De Ory-Manchón, F. Lymphocytic Choriomeningitis Virus—associated meningitis, southern Spain. Emerg. Infect. Dis. 2012, 18, 855–858. [Google Scholar] [CrossRef] [PubMed]
- Gegúndez, M.I.J.; Saz, J.V.; Alves, M.J.; Merino, F.J.; Filipe, A.R.; Beltrán, M. Hantavirus infection in Spain: seroepidemiologic study in the province of Soria. Medicina Clínica 1996, 106, 131–133. [Google Scholar] [PubMed]
- Sanfeliu, I.; Nogueras, M.M.; Gegúndez, M.I.; Segura, F.; Lledó, L.; Font, B.; Saz, J.V. Seroepidemiological survey of hantavirus infection in healthy people in Vallès Occidental, Barcelona. Vector-Borne Zoonotic Dis. 2011, 11, 697–700. [Google Scholar] [CrossRef]
- Heinemann, P.; Alabi, A.; Anon, J.-C.; Auste, B.; Essbauer, S.; Gnionsahe, A.; Kigninlman, H.; Klempa, B.; Kraef, C.; Leendertz, F.H.; et al. Human infections by non–rodent-associated hantaviruses in Africa. J. Infect. Dis. 2016, 214, 1507–1511. [Google Scholar] [CrossRef]
- Lledó, L.; Saz, J.; Alves, M.; Gegúndez, M.; Beltran, M. Serological study of hantavirus in man in the Autonomous Community of Madrid, Spain. J. Med. Microbiol. 2002, 51, 861–865. [Google Scholar]
- Nogueras, M.-M.; Cardeñosa, N.; Sanfeliu, I.; Munoz, T.; Font, B.; Segura, F. Evidence of infection in humans with Rickettsia typhi and Rickettsia felis in catalonia in the northeast of Spain. Ann. N. Y. Acad. Sci. 2006, 1078, 159–161. [Google Scholar] [CrossRef]
- Lledó, L.; Giménez-Pardo, C.; Domínguez-Peñafiel, G.; Sousa, R.; Gegúndez, M.I.; Casado, N.; Criado, A. Molecular detection of hemoprotozoa and Rickettsia Species in arthropods collected from wild animals in the Burgos province, Spain. Vector-Borne Zoonotic Dis. 2010, 10, 735–738. [Google Scholar] [CrossRef]
- Lledó, L.; Gegúndez, M.I.; Fernandes, N.; Sousa, R.; Vicente, J.; Alamo, R.; Fernández-Soto, P.; Pérez-Sánchez, R.; Bacellar, F. The seroprevalence of human infection with Rickettsia slovaca, in an area of northern Spain. Ann. Trop. Med. Parasitol. 2006, 100, 337–343. [Google Scholar] [CrossRef]
- Bolaños-Rivero, M.; Santana-Rodríguez, E.; Angel-Moreno, A.; Hernández-Cabrera, M.; Limiñana-Canal, J.-M.; Carranza-Rodríguez, C.; Martín-Sánchez, A.-M.; Pérez-Arellano, J.-L. Seroprevalence of Rickettsia typhi and Rickettsia conorii infections in the Canary Islands (Spain). Int. J. Infect. Dis. 2011, 15, 481–485. [Google Scholar] [CrossRef] [PubMed]
- Bernabeu-Wittel, M.; Toro, M.D.; Nogueras, M.-M.; Muniáin, M.A.; Cardeñosa, N.; Márquez, F.J.; Segura, F.; Pachón, J. Seroepidemiological study of Rickettsia felis, Rickettsia typhi, and Rickettsia conorii infection among the population of southern Spain. Eur. J. Clin. Microbiol. Infect. Dis. 2006, 25, 375–381. [Google Scholar] [CrossRef] [PubMed]
- Lledó, L.; Gegúndez, M.I.; Medina, J.; González, J.; Alamo, R.; Saz, J. Epidemiological study of Rickettsia typhi infection in two provinces of the north of Spain: Analysis of sera from the general population and sheep. Vector-Borne Zoonotic Dis. 2005, 5, 157–161. [Google Scholar] [CrossRef] [PubMed]
- Nogueras, M.-M.; Pons, I.; Pla, J.; Ortuño, A.; Miret, J.; Sanfeliu, I.; Segura, F. The role of dogs in the eco-epidemiology of Rickettsia typhi, etiological agent of Murine typhus. Veter-Microbiol. 2013, 163, 97–102. [Google Scholar] [CrossRef]
- Giménez-Pardo, C.; Lledó, L.; CSerrano, J.L.; Gegúndez, M.I.; Saz, J.V. Antibodies to Rickettsia spp. and Borrelia burgdorferi in Spanish Wild Red Foxes (Vulpes vulpes). J. Wildl. Dis. 2016, 52, 122–125. [Google Scholar]
- Lindgren, E.; Tälleklint, L.; Polfeldt, T. Impact of climatic change on the northern latitude limit and population density of the disease-transmitting European tick ixodes ricinus. Environ. Heal. Perspect. 2000, 108, 119–123. [Google Scholar] [CrossRef]
- Oteo, J.A.; De Artola, V.M.; Casas, J.; Lozano, A.; Calvo, J.L.F.; Grandival, R. Epidemiology and prevalence of seropositivity against Borrelia burgdorferi antigen in La Rioja, Spain. Revue d’Épidémiologie et de Santé Publique 1992, 40, 85–92. [Google Scholar]
- Asensi, J.M.; Martínez, A.M.; Guerrero, A.; Asensi, V.; Escudero, R.; De La Iglesia, P.; Arribas, J.M. Epidemiologic study of Lyme disease in Asturias. Enfermedades Infecciosas y Microbiología Clínica 1993, 11, 420–423. [Google Scholar]
- Lledó, L.; Gegúndez, M.I.; Saz, J.V.; Beltrán, M. Screening of the prevalence of antibodies to Borrelia burgdorferi in Madrid province, Spain. Eur. J. Epidemiol. 2004, 19, 471–472. [Google Scholar] [CrossRef]
- Gutierrez, J.; Maroto, M.C.; Higuera, A.; Guerrero, M.; Padilla, E.; Piédrola, G. Three-year study of antibody to Borrelia burgdorferi in southern Spain. Eur. J. Clin. Microbiol. Infect. Dis. 1995, 14, 542–546. [Google Scholar] [CrossRef]
- Merino, F.; Serrano, J.; Saz, J.; Nebreda, T.; Gegundez, M.; Beltran, M. Epidemiological characteristics of dogs with Lyme borreliosis in the province of Soria (Spain). Eur. J. Epidemiol. 2000, 16, 97–100. [Google Scholar] [CrossRef] [PubMed]
- Treviño, C.M.; Navarro, D.L.C.D.; Trastoy, P.R. Borrelia burgdorferi serology and diagnosis of Lyme disease in the healthcare area of Santiago de Compostela (Galicia, Spain): 2006–2016. Med. Clin. 2017, 151, 162–163. [Google Scholar] [CrossRef] [PubMed]
- Lledó, L.; Gegúndez, M.I.; Giménez-Pardo, C.; Alamo, R.; Fernández-Soto, P.; Núncio, M.S.; Saz, J.V. A Seventeen-year epidemiological surveillance study of Borrelia burgdorferi infections in two provinces of northern Spain. Int. J. Environ. Res. Public Health 2014, 11, 1661–1672. [Google Scholar] [CrossRef] [PubMed]
- Lledó, L.; Gegúndez, M.I.; Saz, J.V.; Bahamontes, N.; Beltrán, M. Lymphocytic Choriomeningitis virus infection in a province of Spain: Analysis of sera from the general population and wild rodents. J. Med. Virol. 2003, 70, 273–275. [Google Scholar]
- Lee, H.W.; Lee, P.W. Korean hemorrhagic fever. Demonstration of causative antigen and antibodies. Korean J. Intern. Med. 1976, 19, 371–383. [Google Scholar]
- Philip, R.N.; Casper, E.A.; Ormsbee, R.A.; Peacock, M.G.; Burgdorfer, W. Microimmunofluorescence test for the serological study of rocky mountain spotted fever and typhus. J. Clin. Microbiol. 1976, 3, 51–61. [Google Scholar]
- Russell, H.; Sampson, J.S.; Schmid, G.P.; Wilkinson, H.W.; Plikaytis, B. Enzyme-Linked Immunosorbent assay and indirect immunofluorescence assay for Lyme disease. J. Infect. Dis. 1984, 149, 465–470. [Google Scholar] [CrossRef]
- Barton, L.L.; Peters, C.J.; Ksiazek, T.G. Lymphocytic Choriomeningitis virus: An unrecognized teratogenic pathogen. Emerg. Infect. Dis. 1995, 1, 152–153. [Google Scholar] [CrossRef]
- Ambrosio, A.M.; Feuillade, M.R.; Gamboa, G.S.; Maiztegui, J.I. Prevalence of Lymphocytic Choriomeningitis Virus infection in a human population of Argentina. Am. J. Trop. Med. Hyg. 1994, 50, 381–386. [Google Scholar] [CrossRef]
- Stephensen, C.B.; Blount, S.R.; Lanford, R.E.; Holmes, K.V.; Montali, R.J.; Fleenor, M.E.; Shaw, J.F. Prevalence of serum antibodies against lymphocytic Choriomeningitis virus in selected populations from two U.S. cities. J. Med. Virol. 1992, 38, 27–31. [Google Scholar] [CrossRef]
- Park, J.Y.; Rollin, P.E.; Maetz, H.M.; Stephensen, C.B.; Waites, K.B.; Gray, B.; Ksiazek, T.G.; Katholi, C.R.; Peters, C.J. Age distribution of lymphocytic Choriomeningitis virus serum antibody in Birmingham, Alabama: evidence of a decreased risk of infection. Am. J. Trop. Med. Hyg. 1997, 57, 37–41. [Google Scholar] [CrossRef] [PubMed]
- Fulhorst, C.F.; Milazzo, M.L.; Armstrong, L.R.; Childs, J.E.; Rollin, P.E.; Khabbaz, R.; Peters, C.; Ksiazek, T.G. Hantavirus and arenavirus antibodies in persons with occupational rodent exposure, north America. Emerg. Infect. Dis. 2007, 13, 532–538. [Google Scholar] [CrossRef] [PubMed]
- Ledesma, J.; Fedele, C.G.; Carro, F.; Lledo, L.; Sánchez-Seco, M.P.; Tenorio, A.; Soriguer, R.C.; Saz, J.V.; Dominguez, G.; Rosas, M.F.; et al. Independent lineage of lymphocytic Choriomeningitis virus in wood mice (Apodemus sylvaticus), Spain. Emerg. Infect. Dis. 2009, 15, 1677–1680. [Google Scholar] [CrossRef] [PubMed]
- Tagliapietra, V.; Rosa, R.; Rossi, C.; Rosso, F.; Hauffe, H.C.; Tommasini, M.; Versini, W.; Cristallo, A.F.; Rizzoli, A. Emerging rodent-borne viral zoonoses in Trento, Italy. EcoHealth 2018, 15, 695–704. [Google Scholar] [CrossRef]
- Lledó, L.; Gegúndez, M.I.; Saz, J.V.; Beltrán, M. Seroprevalence of antibodies to Seoul virus in occupational risk groups. Enfermedades Infecciosas y Microbiología Clínica 2004, 22, 217–219. [Google Scholar] [CrossRef]
- Lledó, L.; González, R.; Beltrán, M.; Ledesma, J.; Domingo, C.; Gegúndez, M.I.; Saz, J.V.; Romanyk, J. Prevalence of anti-hantavirus antibodies in patients with hypertransaminemia in Madrid (Spain). Am. J. Trop. Med. Hyg. 2007, 77, 371–375. [Google Scholar] [CrossRef]
- Chai, C.-L.; Lu, Q.-Y.; Sun, J.-M.; Jiang, L.-P.; Ling, F.; Zhang, L.-J.; Zheng, S.-G.; Zhang, H.; Ge, J.-H. Sero-epidemiologic investigation on tick-borne diseases of humans and domestic animals in Zhejiang province. Zhonghua Liu Xing Bing Xue Za Zhi 2010, 31, 1144–1147. [Google Scholar]
- Silveira, I.; Martins, T.F.; Olegário, M.M.; Peterka, C.; Guedes, E.; Ferreira, F.; Labruna, M.B. Rickettsial infection in animals, humans and ticks in Paulicéia, Brazil. Zoonoses Public Health 2015, 62, 525–533. [Google Scholar] [CrossRef]
- Podsiadły, E.; Chmielewski, T.; Karbowiak, G.; Kędra, E.; Tylewska-Wierzbanowska, S. The occurrence of spotted fever rickettsioses and other tick-borne infections in forest workers in Poland. Vector-Borne Zoonotic Dis. 2011, 11, 985–989. [Google Scholar] [CrossRef]
- Anton, E.; Nogueras, M.M.; Pons, I.; Font, B.; Munoz, T.; Sanfeliu, I.; Segura, F. Rickettsia slovaca Infection in Humans in the Northeast of Spain: seroprevalence study. Vector-Borne Zoonotic Dis. 2008, 8, 689–694. [Google Scholar] [CrossRef]
- Lledó, L.; Gegúndez, M.; Saz, J.; Beltrán, M. Prevalence of antibodies to Rickettsia typhi in an area of the center of Spain. Eur. J. Epidemiol. 2001, 17, 927–928. [Google Scholar] [CrossRef] [PubMed]
- Ortuño, A.; Pons, I.; Quesada, M.; Lario, S.; Anton, E.; Gil, A.; Castellà, J.; Segura, F. Evaluation of the presence of Rickettsia slovaca infection in domestic ruminants in Catalonia, Northeastern Spain. Vector Borne Zoonotic Dis. 2012, 12, 1019–1022. [Google Scholar] [CrossRef] [PubMed]
- Kubiak, K.; Dzika, E.; Równiak, J.; Dziedziech, M.; Dzisko, J. Seroprevalence of Lyme disease and genospecies of Borrelia burgdorferi sensu lato in patients diagnosed with borreliosis in the Province of Warmia-Masuria in north-eastern Poland. Ann. Agric. Environ. Med. 2012, 19, 203–207. [Google Scholar] [PubMed]
- Oteiza-Olaso, J.; Tiberio-López, G.; Martínez de Artola, V.; Belzunegui-Otano, T. Seroprevalence of Lyme disease in Navarra, Spain. Med. Clin. 2011, 136, 336–339. [Google Scholar] [CrossRef]
| Microorganisms | Men (n) | Women (n) | p Value * | OR (CL 95%) | Age (Mean) | p Value ** |
|---|---|---|---|---|---|---|
| Lymphocytic choriomeningitis viruses (LCMV) + | 2 | 0 | 1 | NA | 50 | 0.037 |
| LCMV − | 68 | 30 | 35.1 | |||
| Hantavirus + | 3 | 1 | 1 | 1.3 (0.13–13.01) | 33.5 | 0.438 |
| Hantavirus − | 67 | 29 | 35.5 | |||
| Rickettsia + | 7 | 1 | 0.429 | 3.2 (0.38–27.41) | 42.6 | 0.011 |
| Rickettsia − | 63 | 29 | 34.8 | |||
| B. burgdorferi + | 5 | 2 | 1 | 1.1 (0.20–5.89) | 39.6 | 0.157 |
| B. burgdorferi − | 65 | 28 | 35.1 |
| Positives | Lymphocytic choriomeningitis Viruses (LCMV) | Hantaviruses | Rickettsia | B. burgdorferi | ||
|---|---|---|---|---|---|---|
| SAA | Seoul | R. typhi | R. slovaca | |||
| 1 | 1/64 | 1/64 | ||||
| 2 | 1/64 | 1/32 | ||||
| 3 | 1/2048 | |||||
| 4 | 1/256 | |||||
| 5 | 1/512 | |||||
| 6 | 1/256 | |||||
| 7 | 1/32 | |||||
| 8 | 1/512 | |||||
| 9 | 1/64 | |||||
| 10 | 1/128 | |||||
| 11 | 1/512 | |||||
| 12 | 1/32 | |||||
| 13 | 1/64 | 1/512 | ||||
| 14 | 1/256 | |||||
| 15 | 1/32 | |||||
| 16 | 1/512 | |||||
| 17 | 1/32 | |||||
| 18 | 1/256 | |||||
| 19 | 1/64 | |||||
| 20 | 1/64 | 1/32 | ||||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lledó, L.; Giménez-Pardo, C.; Gegúndez, M.I. Screening of Forestry Workers in Guadalajara Province (Spain) for Antibodies to Lymphocytic Choriomeningitis Virus, Hantavirus, Rickettsia spp. and Borrelia burgdorferi. Int. J. Environ. Res. Public Health 2019, 16, 4500. https://doi.org/10.3390/ijerph16224500
Lledó L, Giménez-Pardo C, Gegúndez MI. Screening of Forestry Workers in Guadalajara Province (Spain) for Antibodies to Lymphocytic Choriomeningitis Virus, Hantavirus, Rickettsia spp. and Borrelia burgdorferi. International Journal of Environmental Research and Public Health. 2019; 16(22):4500. https://doi.org/10.3390/ijerph16224500
Chicago/Turabian StyleLledó, Lourdes, Consuelo Giménez-Pardo, and María Isabel Gegúndez. 2019. "Screening of Forestry Workers in Guadalajara Province (Spain) for Antibodies to Lymphocytic Choriomeningitis Virus, Hantavirus, Rickettsia spp. and Borrelia burgdorferi" International Journal of Environmental Research and Public Health 16, no. 22: 4500. https://doi.org/10.3390/ijerph16224500
APA StyleLledó, L., Giménez-Pardo, C., & Gegúndez, M. I. (2019). Screening of Forestry Workers in Guadalajara Province (Spain) for Antibodies to Lymphocytic Choriomeningitis Virus, Hantavirus, Rickettsia spp. and Borrelia burgdorferi. International Journal of Environmental Research and Public Health, 16(22), 4500. https://doi.org/10.3390/ijerph16224500





