The Effect of the Full Coverage of Essential Medicines Policy on Utilization and Accessibility of Primary Healthcare Service for Rural Seniors: A Time Series Study in Qidong, China
Abstract
1. Introduction
2. Materials
2.1. Settings
2.2. FCEMs Policy for Rural Seniors in Qidong County
2.3. Study Outcomes
2.4. Data Collection
2.5. Statistical Analysis
3. Results
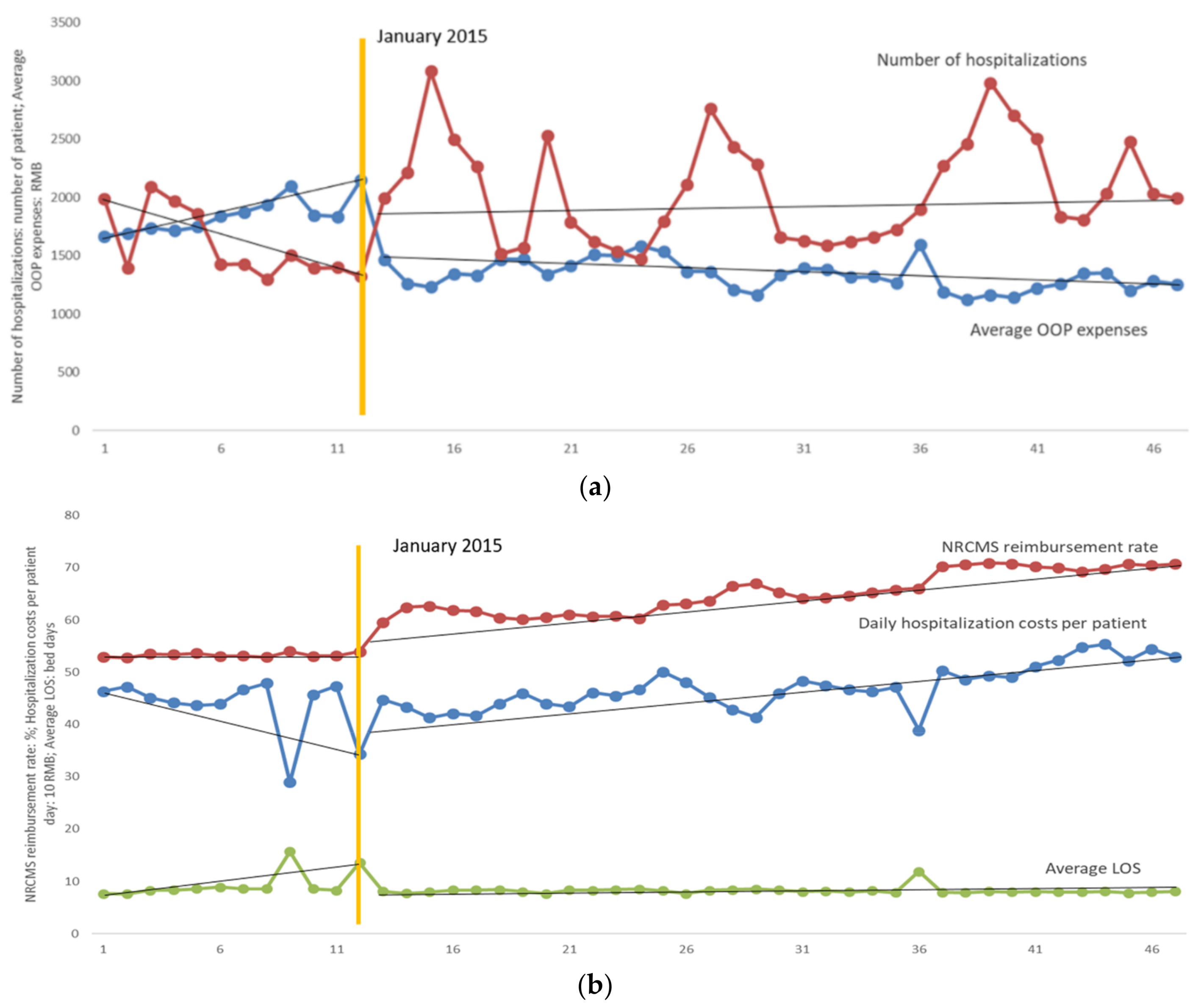
3.1. Primary Health Service Utilization
3.2. Daily Hospitalization Costs of the Elderly Inpatients
3.3. OOP Expenses and NRCMS Reimbursement Rate
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- National Bureau of Statistics of China. China Statistical Yearbook 2018; Statistics Press: Beijing, China, 2018.
- United Nations Department of Economic and Social Affairs. World Population Prospects: The 2010 Revision; United Nations: New York, NY, USA, 2011. [Google Scholar]
- Pearson, W.S.; Bhat-Schelbert, K.; Probst, J.C. Multiple chronic conditions and the aging of America: Challenge for primary care physicians. J. Prim. Care Community Health 2012, 3, 51–56. [Google Scholar] [CrossRef] [PubMed]
- Qiu, Y.; Xu, W.; Cao, S.; Gao, Q.; Wang, Y. Study on disease burden of elderly residents in rural areas. Chin. J. PHM 2014, 30, 143–146. (In Chinese) [Google Scholar]
- Qian, J.; Chen, Y.; Meng, Q. Trends analysis and strategic measures for diseases economic burden of the aging population in China. Chin. J. Health Policy 2012, 5, 12–16. (In Chinese) [Google Scholar]
- Wang, H.; Wang, Z.; Ma, P. Analysis and reflection on poverty caused by illness in rural areas based on the survey of 1214 poor households caused by illness in 9 western provinces and cities. Economist 2016, 10, 71–81. (In Chinese) [Google Scholar]
- Chinese Ministry of Health. 2010 Chinese Health Statistical Digest; Chinese Ministry of Health: Beijing, China, 2011.
- National Health Development Research Center (NHDRC). China National Health Accounts Report; National Health Development Research Center (NHDRC): Beijing, China, 2013. [Google Scholar]
- Guo, Z.; Guan, X.; Shi, L. The impacts of implementation of National Essential Medicines Policies on primary healthcare institutions: A cross-sectional study in China. BMC Health Serv. Res. 2017, 17, 723. [Google Scholar] [CrossRef]
- Guan, X.; Liang, H.; Xue, Y.; Shi, L. An analysis of China’s national essential medicines policy. J. Public Health Policy 2011, 32, 305–319. [Google Scholar] [CrossRef]
- Fang, Y.; Wagner, A.K.; Yang, S.; Jiang, M.; Zhang, F.; Ross-Degnan, D. Access to affordable medicines after health reform: Evidence from two cross-sectional surveys in Shaanxi Province, western China. Lancet Glob. Health 2013, 1, e227–e237. [Google Scholar] [CrossRef]
- Shang, J.; Guo, Z.; Lin, Q.; Li, L.; Chen, C.; Feng, L.; Song, R.; Guan, X.; Shi, L. Analysis of accessibility of essential medicine in Beijing. Chin. J. Health Policy 2016, 2, 52–58. (In Chinese) [Google Scholar]
- Guan, X.; Wang, B.; Xin, X.; Guo, Z.; Han, S. Free pharmaceutical policy to promote equity and access: Its implications for China. Chin. J. Health Policy 2015, 2, 54–59. (In Chinese) [Google Scholar]
- Mudur, G. India’s health assurance plan will offer free medicines, diagnostics, insurance, and traditional medicine. BMJ 2014, 349, g6023. [Google Scholar] [CrossRef]
- Honda, A.; Hanson, K. Do equity funds protect the poor? Case studies from north-western Madagascar. Health Policy Plan. 2013, 28, 75–89. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Puig-Junoy, J.; García-Gómez, P.; Casado-Marín, D. Free medicines thanks to retirement: Impact of coinsurance exemption on pharmaceutical expenditures and hospitalization offsets in a national health service. Health Econ. 2016, 25, 750–767. [Google Scholar] [CrossRef] [PubMed]
- Paniz, V.M.; Fassa, A.G.; Facchini, L.A.; Picchini, L.A.; Tomasi, E.; Thume, E.; da Silverira, D.S.; Rodrigues, M.A.; Domingues, M.R.; Bertoldi, A.D. Free access to hypertension and diabetes medicines among the elderly: A reality yet to be constructed. Cadernos de Saúde Pública 2010, 26, 1163–1174. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.; Qin, X.; Xu, Q.; Ma, J. Comparison of effect of treating essential hypertension between free of charge and self-paying in rural communities. Chin. J. School Dr. 2014, 28, 122–123. (In Chinese) [Google Scholar]
- Li, K.; Wang, Q.; Du, G.; Ma, T. The management effect of free medication for elderly hypertension patients in rural areas. Chin. J. Prev. Contr. Chron Dis. 2015, 23, 532–533. (In Chinese) [Google Scholar]
- Xu, A.; Bu, X.; Dong, L.; Ge, M.; Liu, P.; Liu, W. Effect evaluation of the free medication for poor people with serious mental illness in Weifang. J. Psychiatry. 2013, 26, 178–180. (In Chinses) [Google Scholar]
- National Bureau of Statistics. China Statistical Yearbook; China Statistics Publishing House: Beijing, China, 2014.
- Lin, C.; Ma, T.; Lin, C.; Kao, C. The impact of global budgeting on health service utilization, health care expenditures, and quality of care among patients with pneumonia in Taiwan. Eur. J. Clin. Microbiol. Infect. Dis. 2016, 35, 219–225. [Google Scholar] [CrossRef]
- Liu, C.; Zhao, J. The new rural cooperative medical service system and evaluation and its influencing factors: An empirical analysis based on data CHARLS. Econ. Probl. 2016, 2, 86–91. (In Chinese) [Google Scholar]
- Campbell, S.M.; Reeves, D.; Kontopantelis, E.; Sibbald, B.; Roland, M. Effects of pay for performance on the quality of primary care in England. N. Engl. J. Med. 2009, 361, 368–378. [Google Scholar] [CrossRef]
- Serumaga, B.; Ross-Degnan, D.; Avery, A.J.; Elliott, R.; Majumdar, S.R.; Zhang, F.; Soumerai, S.B. Effect of pay for performance on the management and outcomes of hypertension in the United Kingdom: Interrupted time series study. BMJ 2011, 342, d108. [Google Scholar] [CrossRef]
- Wager, A.K.; Ross-Degnan, D.; Gurwitz, J.; Zhang, F.; Gilden, D.; Soumerai, S.B. Effect of medicaid of New York state regulatory action on benzodiazepine prescribing and hip fracture rates. Ann. Intern. Med. 2007, 146, 96–103. [Google Scholar] [CrossRef] [PubMed]
- Singer, J.D.; Willett, J.B. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence; Oxford University Press: New York, NY, USA, 2003. [Google Scholar]
- Wagner, A.K.; Soumerai, S.B.; Zhang, F.; Ross-Degnan, D. Segmented regression analysis of interrupted time series studies in medication use research. J. Clin. Pharm. Ther. 2002, 27, 299–309. [Google Scholar] [CrossRef] [PubMed]
- Emmerick, I.C.M.; Campos, M.R.; Luiza, V.L.; Chaves, L.A.; Bertoldi, A.D.; Ross-Degan, D. Retrospective interrupted time series examining hypertension and diabetes medicines usage following changes in patient cost sharing in the ‘Farmácia Popular’ programme in Brazil. BMJ Open 2017, 7, e017308. [Google Scholar] [CrossRef] [PubMed]
- Crosbie, J. Interrupted time series analysis with brief single-subject data. J. Consult. Clin. Psychol. 1993, 61, 966–974. [Google Scholar] [CrossRef]
- Orcutt, H. Application of least squares regression to relationships containing autocorrelated error terms. J. Am. Stat. Assoc. 1949, 44, 32–61. [Google Scholar]
- Choi, C.Y.; Hu, L.; Ogaki, M. Robust estimation for structural spurious regressions and a hausman-type cointegration Test. J. Econom. 2008, 142, 327–351. [Google Scholar] [CrossRef]
- Ali, S.; Liu, Y.; Ishaq, M.; Shah, T.; Ilyas, A.; Din, I. Climate change and its impact on the yield of major food crops: Evidence from Pakistan. Foods 2017, 6, 39. [Google Scholar] [CrossRef]
- Healy, W.L.; Rana, A.J.; Iorio, R. Hospital economics of primary total knee arthroplasty at a teaching hospital. Clin. Orthop. Relat. Res. 2011, 469, 87–94. [Google Scholar] [CrossRef][Green Version]
- Ito, K.; Avorn, J.; Shrank, W.H.; Toscano, M.; Brennan, T.; Choudhry, N.K. Long-Term cost-effectiveness of providing full coverage for preventive medications after myocardial infarction. Circ. Cardiovasc. Qual. Outcomes 2015, 8, 252–259. [Google Scholar] [CrossRef]
- Curtis, S.E.; Boye, K.S.; Lage, M.J.; Garcia-Perze, L.E. Medication adherence and improved outcomes among patients with type 2 diabetes. Am. J. Manag. Care 2017, 23, e208–e214. [Google Scholar]
- Hood, S.R.; Giazzon, A.J.; Seamon, G.; Lane, K.A.; Wang, J.; Eckert, G.J.; Tu, W.; Murray, M.D. Association between medication adherence and the outcomes of heart failure. Pharmacotherapy 2018, 38, 539–545. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Bu, W.; Zhang, X.; Xu, F.; Wang, D. Analysis of influence factors of average length of stay in the general third class comprehensive hospital. Chin. Hosp. Manag. 2014, 34, 41–43. (In Chinese) [Google Scholar]
- Mo, C.; Yang, T.; Shi, Y. Research on average length of stay as an efficient index for comparing inter-hospital evaluation. Chin. Hosp. 2009, 13, 16–18. (In Chinese) [Google Scholar]
- Yu, B.; Zhang, X.; Wang, G. Full coverage for hypertension drugs in rural communities in China. Am. J. Manag. Care 2013, 19, e22–e29. [Google Scholar]
- Felix, K.; Lutz, H.; Maarten, P. Availability and affordability of antimalarial and antibiotic medicines in Malawi. PLoS ONE 2017, 12, e0175399. [Google Scholar]
- Choudhry, N.K.; Patrick, A.R.; Antman, E.M.; Avorn, J.; Shrank, W.H. Cost-Effectiveness of providing full drug coverage to increase medication adherence in post-myocardial infarction medicare beneficiaries. Circulation 2008, 117, 1261–1268. [Google Scholar] [CrossRef]
- Xu, Y.; Yang, H.; Bo, Y.; Chen, H.; Cai, Y. A pilot research on operational mode of free hypertensive drug administration in community. Chin. J. Soc. Med. 2013, 30, 48–50. (In Chinese) [Google Scholar]
- Tavares, N.U.; Luiza, V.L.; Oliveira, M.A.; Costa, K.S.; Mengue, S.S.; Arrais, P.S.; Ramos, L.R.; Farias, M.R.; Pizzol, T.D.; Bertoldi, A.D. Free access to medicines for the treatment of chronic diseases in Brazil. Rev. Saude Publica 2016, 50 (Suppl. 2), 7s. [Google Scholar] [CrossRef]
- Chalmers, N.I.; Compton, R.D. Children’s access to dental care affected by reimbursement rates, dentist density, and dentist participation in medicaid. Am. J. Public Health 2017, 107, e1–e3. [Google Scholar] [CrossRef]
- Xu, J.; Wang, J.; King, M.; Liu, R.; Yu, F.; Xing, J.; Su, L.; Lu, M. Rural–Urban disparities in the utilization of mental health inpatient services in China: The role of health insurance. Int. J. Health Econ. Manag. 2018, 18, 377–393. [Google Scholar] [CrossRef]
- Su, S.; Bao, H.; Wang, X.; Wang, Z.; Li, X.; Zhang, M.; Wang, J.; Jiang, H.; Wang, W.; Qu, S.; et al. The quality of invasive breast cancer care for low reimbursement rate patients: A retrospective study. In Proceedings of the China Health Statistics Annual Conference, Wuhan, China, 22–25 August 2017. [Google Scholar]
- Cai, C.; Li, L. Medical insurance and medical care demand for the elderly in China. Econ. Res. J. 2011, 46, 95–107. [Google Scholar]
- Yu, D. Does basic medical insurance for urban residents raise medical service utilization? An empirical evaluation of system running effect. Financ. Econ. Res. 2015, 30, 117–128. [Google Scholar]
- Li, J.; Feng, X.L. Health care-seeking behaviors and health expenditures in adults aged 45 years and older in China, 2011–2013. Trop. Med. Int. Health 2017, 22, 638–654. [Google Scholar] [CrossRef] [PubMed]
- Hu, H.; Luan, W.; Li, J. Medical insurance health services utilization and excessive demands for medical services—The impact of medical insurance on utilization of health service of the elderly. J. Shanxi Univ. Financ. Econ. 2015, 37, 14–24. (In Chinese) [Google Scholar]
- Yao, Y.; Liu, B.; Liu, G.; Zang, W. Medical insurance, household registration system and healthcare utilization: Evidences from CHARLS data Analysis. Insur. Stud. 2014, 6, 105–116. (In Chinese) [Google Scholar]
- Miao, Y.; Gu, J.; Zhang, L.; He, R.; Sandeep, S.; Wu, J. Improving the performance of social health insurance system through increasing outpatient expenditure reimbursement ratio: A quasi-experimental evaluation study from rural China. Int. J. Equity Health 2018, 17, 89. [Google Scholar] [CrossRef]
- Rashidian, A.; Joudaki, H.; Khodayari-Moez, E.; Omranikhoo, H.; Geraili, B.; Arab, M. The impact of rural health system reform on hospitalization rates in the Islamic Republic of Iran: An interrupted time series. Bull. World Health Organ. 2013, 91, 942–949. [Google Scholar] [CrossRef]
- Hyman, R. Quasi-Experimentation: Design and analysis issues for field settings (Book). J. Person. Assess. 1982, 46, 96–97. [Google Scholar] [CrossRef]

| Outcomes | Indicators | Units of Measurement |
|---|---|---|
| Utilization of primary healthcare services | Number of hospitalizations | Number of patients |
| Average LOS a | Hospital inpatient bed-days | |
| Accessibility of Primary Healthcare Services | Daily hospitalization costs per patient b | RMB |
| Average OOP expenses c | RMB | |
| NRCMS reimbursement rate d | Percentages |
| Indicators | 2014 | 2015 | 2016 | 2017 |
|---|---|---|---|---|
| Number of hospitalizations | 19,076 | 24,092 | 23,169 | 25,109 |
| Average LOS (bed-days) | 9.28 | 8.16 | 8.49 | 7.99 |
| Daily hospitalization costs per patient, monthly average (RMB) | 434.10 | 440.36 | 456.74 | 518.29 |
| Average OOP expenses, monthly average (RMB) | 1829.86 | 1387.62 | 1353.75 | 1221.73 |
| NRCMS reimbursement rate (%) | 53.29 | 61.09 | 64.89 | 70.35 |
| Indicators | Intercept and Trend | ADF Statistic | P Value | 5% Critical Value | Stationarity |
|---|---|---|---|---|---|
| Number of hospitalizations | intercept | −3.409 | 0.011 | −2.944 | stationarity |
| Average LOS | trend | −6.839 | <0.001 | −2.941 | stationarity |
| Daily hospitalization costs per patient | trend | −6.038 | <0.001 | −3.516 | stationarity |
| Average OOP expenses | trend | −3.415 | 0.049 | −2.941 | stationarity |
| NRCMS reimbursement rate | intercept and trend | −3.536 | 0.048 | −3.513 | stationarity |
| Indicators | Slope: Jan 2014 to Dec 2014 (SE) | p | Change in Level: Predicted Value of Jan 2015 Based on Post-FCEMs Trend Minus Predicted Value Based on Pre-FCEMs Trend (SE) | p | Change in Slope from Jan 2014-Dec 2014 to Jan 2015-Nov 2017 (SE) | p | Parameters of Model Fit | ||
|---|---|---|---|---|---|---|---|---|---|
| DW | Root MSE | R2 | |||||||
| Number of hospitalizations | −55.953 (45.602) | 0.227 | 720.440 (329.545) | 0.034 | 58.328 (48.691) | 0.238 | 1.790 | 351.420 | 0.209 |
| Average LOS | 0.372 (0.082) | <0.001 | −3.257 (0.625) | <0.001 | −0.369 (0.083) | <0.001 | 2.267 | 1.190 | 0.508 |
| Daily hospitalization costs per patient | −6.263 (2.793) | 0.030 | 13.844 (21.478) | 0.523 | 9.382 (2.841) | 0.002 | 2.028 | 35.765 | 0.534 |
| Average OOP expenses | 38.035 (11.555) | 0.012 | −626.905 (90.261) | <0.001 | −43.215 (14.950) | 0.006 | 1.891 | 106.130 | 0.741 |
| NRCMS reimbursement rate | 0.066 (0.165) | 0.692 | 5.301 (1.033) | <0.001 | 0.283 (0.185) | 0.135 | 1.636 | 1.012 | 0.915 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, Y.; Zhu, Y.; Shi, H.; Sun, X.; Chen, N.; Li, X. The Effect of the Full Coverage of Essential Medicines Policy on Utilization and Accessibility of Primary Healthcare Service for Rural Seniors: A Time Series Study in Qidong, China. Int. J. Environ. Res. Public Health 2019, 16, 4316. https://doi.org/10.3390/ijerph16224316
Wang Y, Zhu Y, Shi H, Sun X, Chen N, Li X. The Effect of the Full Coverage of Essential Medicines Policy on Utilization and Accessibility of Primary Healthcare Service for Rural Seniors: A Time Series Study in Qidong, China. International Journal of Environmental Research and Public Health. 2019; 16(22):4316. https://doi.org/10.3390/ijerph16224316
Chicago/Turabian StyleWang, Ying, Yulei Zhu, Hang Shi, Xiaoluan Sun, Na Chen, and Xin Li. 2019. "The Effect of the Full Coverage of Essential Medicines Policy on Utilization and Accessibility of Primary Healthcare Service for Rural Seniors: A Time Series Study in Qidong, China" International Journal of Environmental Research and Public Health 16, no. 22: 4316. https://doi.org/10.3390/ijerph16224316
APA StyleWang, Y., Zhu, Y., Shi, H., Sun, X., Chen, N., & Li, X. (2019). The Effect of the Full Coverage of Essential Medicines Policy on Utilization and Accessibility of Primary Healthcare Service for Rural Seniors: A Time Series Study in Qidong, China. International Journal of Environmental Research and Public Health, 16(22), 4316. https://doi.org/10.3390/ijerph16224316





