Work-Related Burdens and Requirements for Health Promotion Programs for Nursing Staff in Different Care Settings: A Cross-Sectional Study
Abstract
:1. Introduction
- What are the differences of nurses in different roles regarding psychological strains (e.g., Mental Health, Chronic Stress, Mental Strains)?
- What are the differences of nurses in different roles regarding physiological strains (e.g., Physical Health, Physical Strains)?
- What are the differences of nurses in different roles regarding requests and barriers for participation in health promotion programs, especially in physical activity?
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Outcome Measures
2.3.1. Health Survey (SF 12)
2.3.2. Trier Inventory for Chronic Stress (TICS)
2.3.3. Questionnaire for Subjective Assessment of Workplace Exposure (modified Slesina Questionnaire)
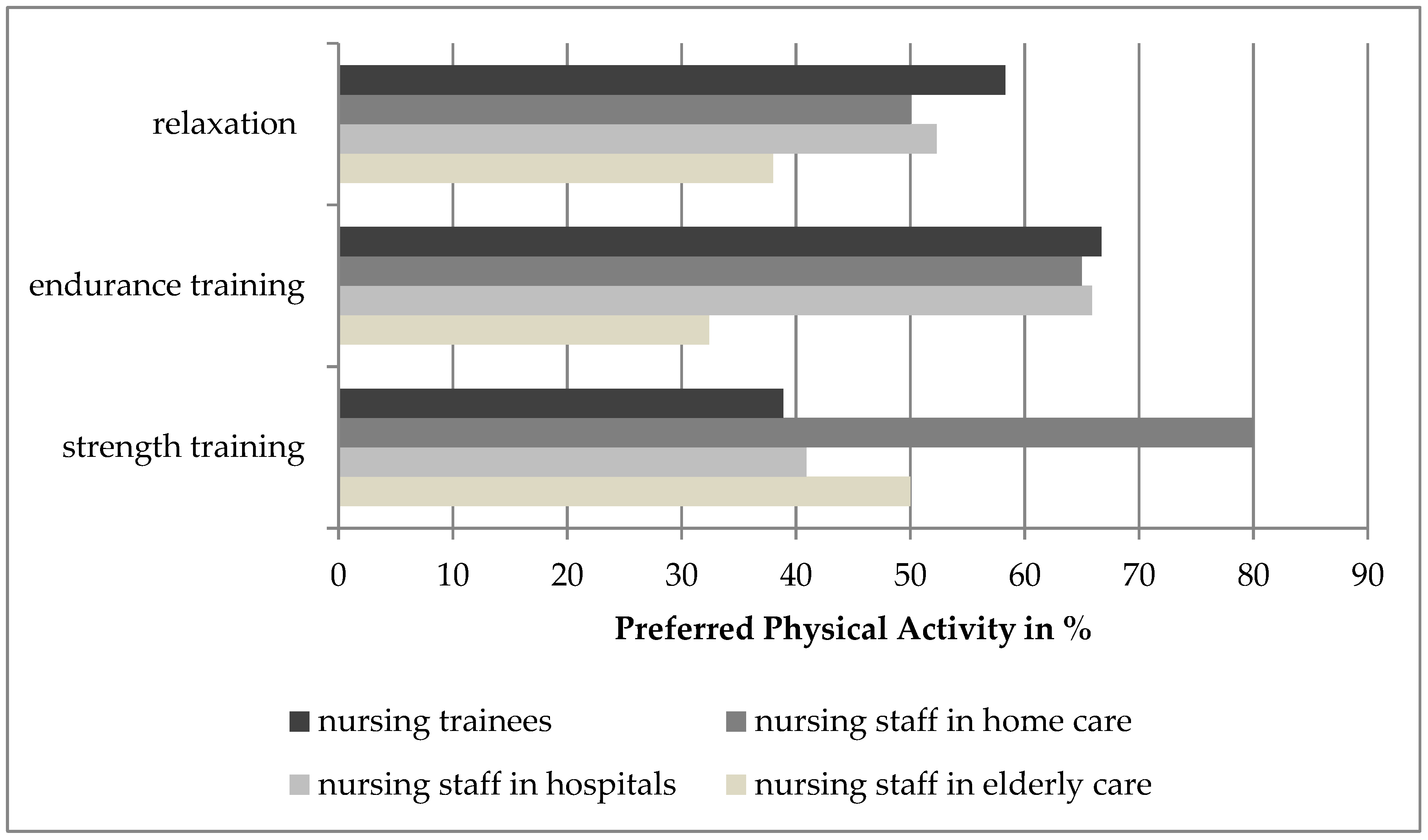
2.3.4. Requests for Participation in an Individualized Intervention
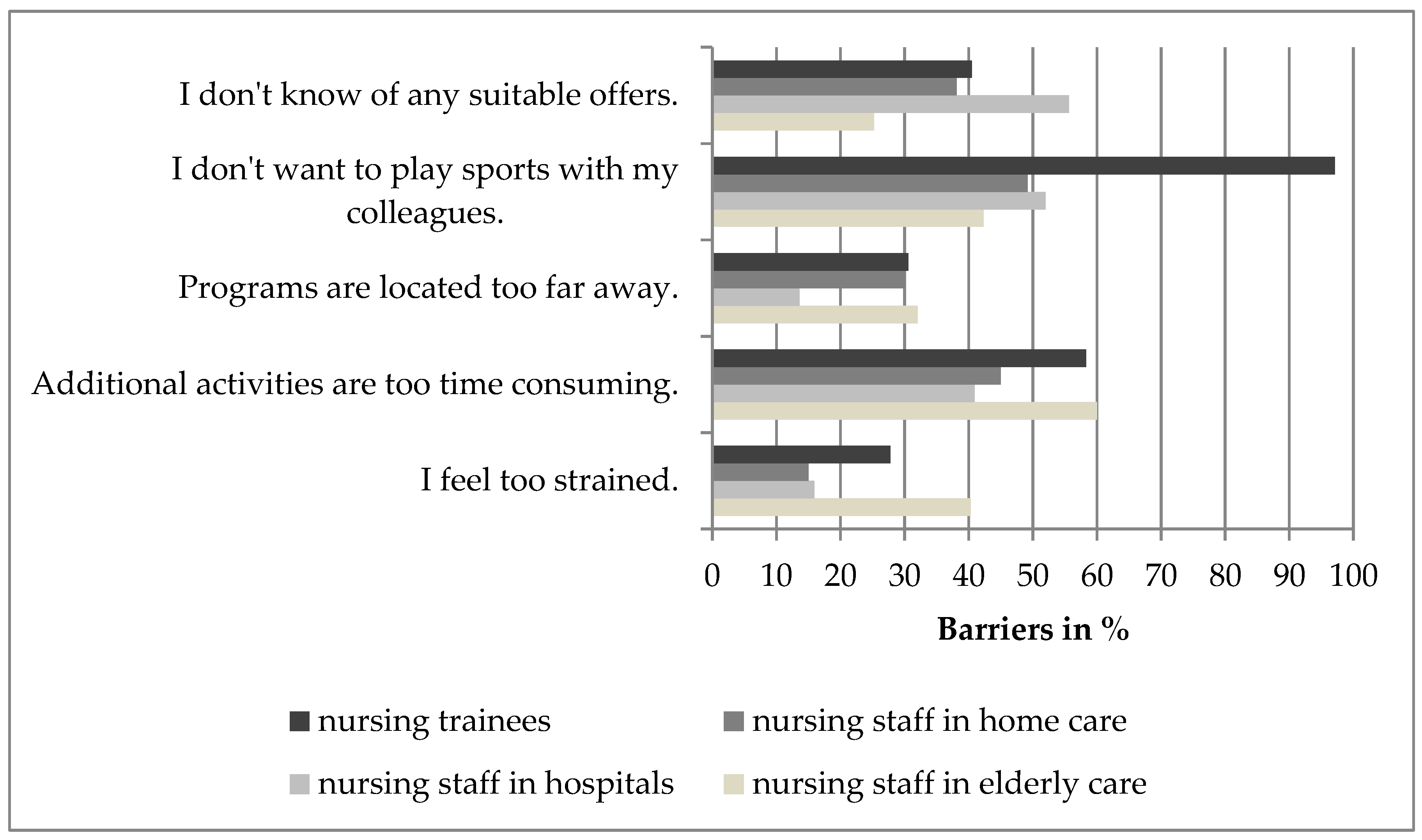
2.3.5. Barriers to Participate in Health Promotion Programs
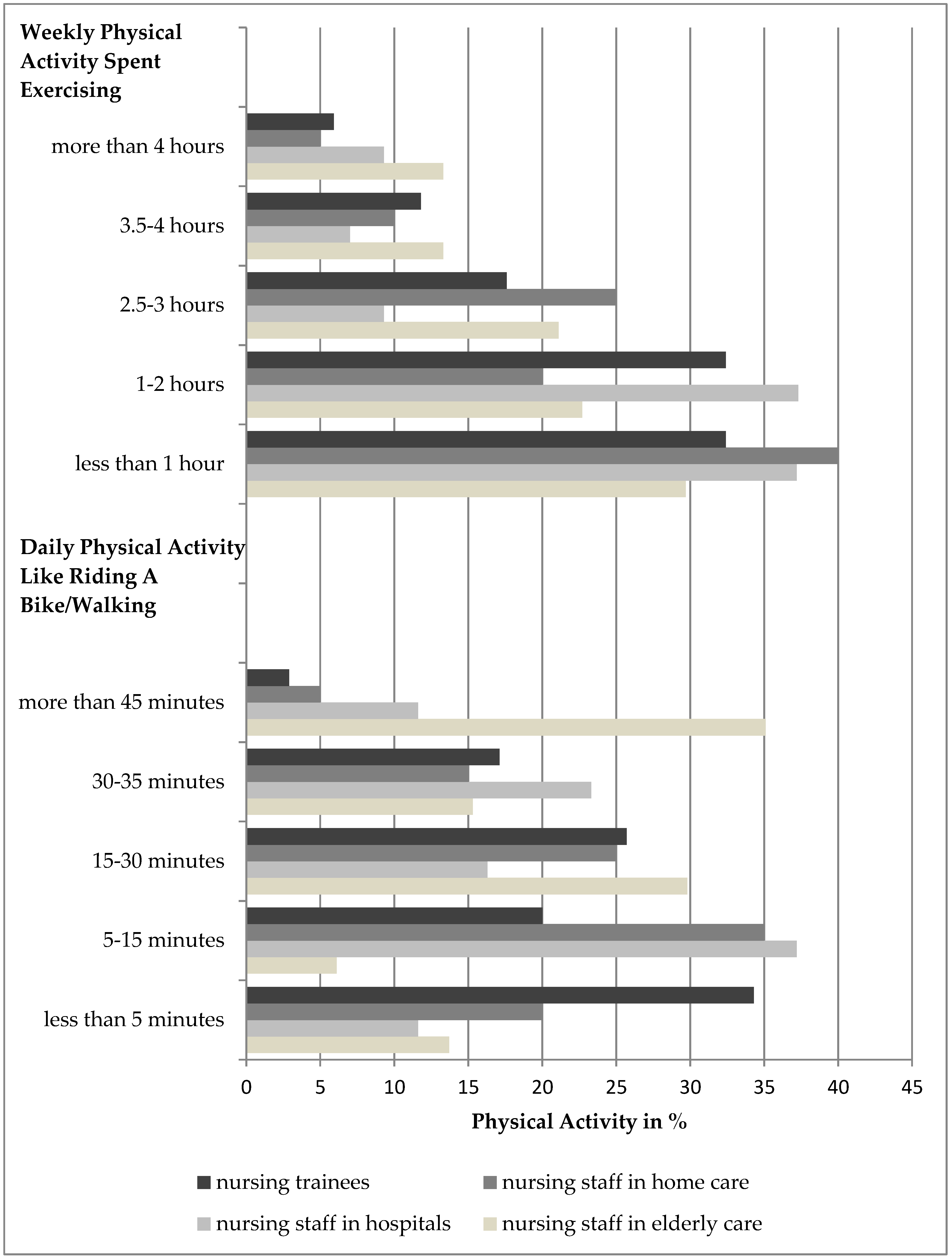
2.3.6. Physical Activity
2.4. Data Analysis
3. Results
- Heavy physical tasks (66.1% nursing staff in elderly care, 59.1% nursing staff in hospitals, 70.0% nursing staff in home care, 55.6% nursing trainees; Chi2 = 59.213, p < 0.001);
- Awkward posture (65.3% nursing staff in elderly care, 77.3% nursing staff in hospitals, 80.0% nursing staff in home care, 75.0% nursing trainees, Chi2 = 77.796, p < 0.001);
- Lifting heavy load (61.9% nursing staff in elderly care, 50.0% nursing staff in hospitals, 55.0% nursing staff in home care, 66.7% nursing trainees; Chi2 = 105.987, p < 0.001);
- Holding heavy load (51.3% nursing staff in elderly care, 52.3% nursing staff in hospitals, 60.0% nursing staff in home care, 44.4% nursing trainees; Chi2 = 89.762, p < 0.001);
- Time pressure (67.8% nursing staff in elderly care, 79.5% nursing staff in hospitals, 80.0% nursing staff in home care, 69.4% nursing trainees; Chi2 = 45.957, p < 0.001);
- Pressure to perform (55.9% nursing staff in elderly care, 70.5% nursing staff in hospitals, 60.0% nursing staff in home care, 66.7% nursing trainees; Chi2 = 62.872, p < 0.001).
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Bundesagentur für Arbeit. Arbeitsmarktsituation im Pflegebereich Labour Market Situation in the Nursing Sector; Bundesagentur für Arbeit: Nürnberg, Germany, 2019. [Google Scholar]
- Hasselhorn, H.-M.; Tackenberg, P.; Müller, B.H. Vorzeitiger Berufsausstieg aus der Pflege in Deutschland als zunehmendes Problem für den Gesundheitsdienst—Eine Ubersichtsarbeit Premature Departure from Nursing in Germany as a Growing Problem for the Health Care System—A Review. Gesundheitswesen 2003, 65, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Heinen, M.M.; van Achterberg, T.; Schwendimann, R.; Zander, B.; Matthews, A.; Kózka, M.; Ensio, A.; Sjetne, I.S.; Moreno Casbas, T.; Ball, J.; et al. Nurses’ intention to leave their profession: A cross sectional observational study in 10 European countries. Int. J. Nurs. Stud. 2013, 50, 174–184. [Google Scholar] [CrossRef]
- Büssing, A.; Glaser, J.; Höge, T. Psychische und physische Belastungen in der ambulanten Pflege: Ein Screening zum Arbeits- und Gesundheitsschutz Psychological and physical work load in home care: A screening instrument for occupational health and safety. Zeitschrift für Arbeits-und Organisationspsychologie A-O 2004, 48, 165–180. [Google Scholar] [CrossRef]
- Fiabane, E.; Giorgi, I.; Sguazzin, C.; Argentero, P. Work engagement and occupational stress in nurses and other healthcare workers: The role of organisational and personal factors. J. Clin. Nurs. 2013, 22, 2614–2624. [Google Scholar] [CrossRef] [PubMed]
- Magnavita, N. Workplace violence and occupational stress in healthcare workers: A chicken-and-egg situation-results of a 6-year follow-up study. J. Nurs. Sch. 2014, 46, 366–376. [Google Scholar] [CrossRef]
- Weinberg, A.; Creed, F. Stress and psychiatric disorder in healthcare professionals and hospital staff. Lancet 2000, 355, 533–537. [Google Scholar] [CrossRef]
- Owen, B.D.; Keene, K.; Olson, S. Patient-handling tasks perceived to be most stressful by hospital nursing personnel. J. Healthc. Saf. Compliance Infect. Control 2000, 5, 19–25. [Google Scholar]
- McVicar, A. Workplace stress in nursing: A literature review. J. Adv. Nurs. 2003, 44, 633–642. [Google Scholar] [CrossRef] [PubMed]
- Michie, S. Reducing work related psychological ill health and sickness absence: A systematic literature review. Occup. Environ. Med. 2003, 60, 3–9. [Google Scholar] [CrossRef] [PubMed]
- İlhan, M.N.; Durukan, E.; Taner, E.; Maral, I.; Bumin, M.A. Burnout and its correlates among nursing staff: Questionnaire survey. J. Adv. Nurs. 2008, 61, 100–106. [Google Scholar] [CrossRef] [PubMed]
- Hasson, H.; Arnetz, J.E. Nursing staff competence, work strain, stress and satisfaction in elderly care: A comparison of home-based care and nursing homes. J. Clin. Nurs. 2008, 17, 468–481. [Google Scholar] [CrossRef] [PubMed]
- Nübling, M.; Vomstein, M.; Schmidt, S.G.; Gregersen, S.; Dulon, M.; Nienhaus, A. Psychosocial work load and stress in the geriatric care. BMC Public Health 2010, 10, 428. [Google Scholar] [CrossRef]
- Wenderlein, F.U. Arbeitszufriedenheit und Fehlzeiten in der Krankenpflege—Untersuchung an 1021 Examinierten und Schülern Work Satisfaction and Absenteeism of Nursing Staff—Comparative Study of 1021 Nursing Trainees and Nurses. Gesundheitswesen 2003, 65, 620–628. [Google Scholar] [CrossRef] [PubMed]
- Irving, J.A.; Dobkin, P.L.; Park, J. Cultivating mindfulness in health care professionals: A review of empirical studies of mindfulness-based stress reduction (MBSR). Complement. Ther. Clin. Pract. 2009, 15, 61–66. [Google Scholar] [CrossRef]
- Dawson, A.P.; McLennan, S.N.; Schiller, S.D.; Jull, G.A.; Hodges, P.W.; Stewart, S. Interventions to prevent back pain and back injury in nurses: A systematic review. Occup. Environ. Med. 2007, 64, 642–650. [Google Scholar] [CrossRef]
- Seidler, A.; Euler, U.; Bolm-Audorff, U.; Ellegast, R.; Grifka, J.; Haerting, J.; Jäger, M.; Michaelis, M.; Kuss, O. Physical workload and accelerated occurrence of lumbar spine diseases: Risk and rate advancement periods in a German multicenter case-control study. Scand. J. Work Environ. Health 2011, 37, 30–36. [Google Scholar]
- Eriksen, W. Work factors as predictors of intense or disabling low back pain; a prospective study of nurses’ aides. Occup. Environ. Med. 2004, 61, 398–404. [Google Scholar] [CrossRef]
- Lorusso, A.; Bruno, S.; L’Abbate, N. A Review of Low Back Pain and Musculoskeletal Disorders among Italian Nursing Personnel. Ind. Health 2007, 45, 637–644. [Google Scholar] [CrossRef] [Green Version]
- Simon, M.; Tackenberg, P.; Nienhaus, A.; Estryn-Behar, M.; Conway, P.M.; Hasselhorn, H.-M. Back or neck-pain-related disability of nursing staff in hospitals, nursing homes and home care in seven countries--results from the European NEXT-Study. Int. J. Nurs. Stud. 2008, 45, 24–34. [Google Scholar] [CrossRef]
- Von Korff, M.; Ormel, J.; Keefe, F.J.; Dworkin, S.F. Grading the severity of chronic pain. Pain 1992, 50, 133–149. [Google Scholar] [CrossRef]
- Unternehmenskultur und Gesundheit—Herausforderungen und Chancen. Zahlen, Daten, Analysen Aus Allen Branchen der Wirtschaft Corporate Culture and Health-Challenges and Opportunities. Figures, Data, Analyses from All Sectors of the Economy; Badura, B., Ed.; Springer: Berlin/Heidelberg, Germany, 2016. [Google Scholar]
- BARMER GEK. BARMER GEK Pflegereport 2016. Schriftenreihe zur Gesundheitsanalyse; BARMER GEK Care Report 2016; Series on Health Analysis; Rothgang, H., Kalwitzkli, T., Müller, R., Runte, R., Unger, R., Eds.; Springer: Berlin/Heidelberg, Germany, 2016. [Google Scholar]
- Kromark, K.; Dulon, M.; Beck, B.-B.; Nienhaus, A. Back disorders and lumbar load in nursing staff in geriatric care: A comparison of home-based care and nursing homes. J. Occup. Med. Toxicol. 2009, 4, 33. [Google Scholar] [CrossRef] [PubMed]
- Gesundheit und Arbeit—Blickpunkt Gesundheitswesen. BKK Gesundheitsatlas 2017 Health and Work-Focus on Healthcare. BKK Health Atlas 2017; Kliner, K., Rennert, D., Richter, M., Eds.; 1. Auflage; MWV Medizinisch Wissenschaftliche Verlagsgesellschaft: Berlin, Germany, 2017. [Google Scholar]
- Miranda, H.; Punnett, L.; Gore, R.; Boyer, J. Violence at the workplace increases the risk of musculoskeletal pain among nursing home workers. Occup. Environ. Med. 2011, 68, 52–57. [Google Scholar] [CrossRef] [PubMed]
- Evers, W.; Tomic, W.; Brouwers, A. Aggressive behaviour and burnout among staff of homes for the elderly. Int. J. Ment. Health Nurs. 2002, 11, 2–9. [Google Scholar] [CrossRef] [PubMed]
- Jenull, B.; Brunner, E. Death and Dying in Nursing Homes: A Burden for the Staff? J. Appl. Gerontol. 2008, 27, 166–180. [Google Scholar] [CrossRef]
- Mitchell, T.; O’Sullivan, P.B.; Burnett, A.F.; Straker, L.; Rudd, C. Low back pain characteristics from undergraduate student to working nurse in Australia: A cross-sectional survey. Int. J. Nurs. Stud. 2008, 45, 1636–1644. [Google Scholar] [CrossRef] [PubMed]
- Smith, D.R.; Sato, M.; Miyajima, T.; Mizutani, T.; Yamagata, Z. Musculoskeletal disorders self-reported by female nursing students in central Japan: A complete cross-sectional survey. Int. J. Nurs. Stud. 2003, 40, 725–729. [Google Scholar] [CrossRef] [PubMed]
- Alexandre, N.M.C.; Moraes, M.A.A.D.; Corrêa Filho, H.R.; Jorge, S.A. Evaluation of a program to reduce back pain in nursing personnel. Revista de Saúde Pública 2001, 35, 356–361. [Google Scholar] [CrossRef]
- Dahl, J.C.; Nilsson, A. Evaluation of a randomized preventive behavioural medicine work site intervention for public health workers at risk for developing chronic pain. Eur. J. Pain 2001, 5, 421–432. [Google Scholar] [CrossRef]
- Edwards, D.; Burnard, P. A systematic review of stress and stress management interventions for mental health nurses. J. Adv. Nurs. 2003, 42, 169–200. [Google Scholar] [CrossRef]
- Bischoff, L.L.; Otto, A.-K.; Hold, C.; Wollesen, B. The effect of physical activity interventions on occupational stress for health personnel: A systematic review. Int. J. Nurs. Stud. 2019, 97, 94–104. [Google Scholar] [CrossRef]
- Freitas, A.R.; Carneseca, E.C.; Paiva, C.E.; Paiva, B.S.R. Impact of a physical activity program on the anxiety, depression, occupational stress and burnout syndrome of nursing professionals. Rev. Lat. Am. Enferm. 2014, 22, 332–336. [Google Scholar] [CrossRef] [Green Version]
- Hawker, C.L. Physical activity and mental well-being in student nurses. Nurse Educ. Today 2012, 32, 325–331. [Google Scholar] [CrossRef] [PubMed]
- Michael, Y.L.; Colditz, G.A.; Coakley, E.; Kawachi, I. Health behaviors, social networks, and healthy aging: Cross-sectional evidence from the Nurses’ Health Study. Qual. Life Res. 1999, 8, 711–722. [Google Scholar] [CrossRef] [PubMed]
- Hamzehgardeshi, Z.; Shahhosseini, Z. A cross-sectional study of facilitators and barriers of Iranian nurses’ participation in continuing education programs. Glob. J. Health Sci. 2013, 6, 183–188. [Google Scholar] [CrossRef] [PubMed]
- Jerdén, L.; Hillervik, C.; Hansson, A.-C.; Flacking, R.; Weinehall, L. Experiences of Swedish community health nurses working with health promotion and a patient-held health record. Scand. J. Caring Sci. 2006, 20, 448–454. [Google Scholar] [CrossRef] [PubMed]
- Naidoo, J.; Wills, J. Developing Practice for Public Health and Health Promotion E-Book, 3rd ed.; Bailliere Tindall: Kent, UK, 2010. [Google Scholar]
- Bullinger, M.; Kirchberger, I.; Ware, J. Der deutsche SF-36 Health Survey Übersetzung und psychometrische Testung eines krankheitsübergreifenden Instruments zur Erfassung der gesundheitsbezogenen Lebensqualität the German SF-36 health survey translation and psychometric testing of a generic instrument for the assessment of health-related quality of life. J. Public Health 1995, 3, 21–36. [Google Scholar] [CrossRef]
- Stieglitz, R.-D.; Bullinger, M.; Kirchberger, I. SF-36. Fragebogen zum Gesundheitszustand (SF-36. Health Survey). Göttingen: Hogrefe. Zeitschrift für Klinische Psychologie und Psychotherapie 1999, 28, 143–145. [Google Scholar] [CrossRef]
- Ware, J.E.; Kosinski, M.; Keller, S.D. SF-12. How to Score the SF-12 Physical and Mental Health Summary Scales, 4th ed.; QualityMetric Inc.: Lincoln, RI, USA; Health Assessment Lab.: Boston, MA, USA, 2002. [Google Scholar]
- Schulz, P.; Schlotz, W. Trierer Inventar zur Erfassung von chronischem Streß (TICS): Skalenkonstruktion, teststatistische Überprüfung und Validierung der Skala Arbeitsüberlastung (The Trier Inventory for the Assessment of Chronic Stress (TICS). Scale construction, statistical testing, and validation of the scale work overload). Diagnostica 1999, 45, 8–19. [Google Scholar] [CrossRef]
- Petrowski, K.; Paul, S.; Albani, C.; Brähler, E. Factor structure and psychometric properties of the trier inventory for chronic stress (TICS) in a representative German sample. BMC Med. Res. Methodol. 2012, 12, 42. [Google Scholar] [CrossRef]
- Slesina, W. FEBA: Fragebogen zur Subjektiven Einschätzung der Belastung am Arbeitsplatz (Questionnaire for Subjective Assessment of Workplace Exposure). Available online: http://www.rueckenkompass.de/download_files/doc/Fragen-Slesina.pdf (accessed on 8 July 2019).
- Finger, J.D.; Mensink, G.; Lange, C.; Manz, K. Gesundheitsfördernde Körperliche Aktivität in der Freizeit Bei Erwachsenen in Deutschland; Health-promoting physical activity in the leisure time of adults in Germany; Robert Koch Institute: Berlin, Germany, 2017. [Google Scholar]
- Sallis, J.F.; Saelens, B.E. Assessment of physical activity by self-report: Status, limitations, and future directions. Res. Q. Exerc. Sport 2000, 71 (Suppl. 2), 1–14. [Google Scholar] [CrossRef]
- Shephard, R.J. Limits to the measurement of habitual physical activity by questionnaires. Br. J. Sports Med. 2003, 37, 197–206. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Recommendations on Physical Activity for Health; WHO: Genève, Switzerland, 2010. [Google Scholar]
- Van Hoof, W.; O’Sullivan, K.; O’Keeffe, M.; Verschueren, S.; O’Sullivan, P.; Dankaerts, W. The efficacy of interventions for low back pain in nurses: A systematic review. Int. J. Nurs. Stud. 2018, 77, 222–231. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Scores | Nursing Staff in Elderly Care (n = 142) | Nursing Staff in Hospitals (n = 44) | Nursing Staff in Home Care (n = 20) | Nursing Trainees (n = 36) |
|---|---|---|---|---|
| SF12-Health Survey | ||||
| Physical Score | 48.23 ± 9.80 | 53.31 ± 7.07 | 54.77 ± 5.76 | 54.20 ± 7.50 |
| Mental Score | 46.36 ± 10.33 | 43.72 ± 9.84 | 44.40 ± 12.21 | 41.85 ± 11.62 |
| Trier Inventory for Chronic Stress | ||||
| Screening Scale Chronic Stress (SSCS) | 17.82 ± 10.64 | 22.61 ± 10.08 | 26.10 ± 12.86 | 22.86 ± 10.65 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Otto, A.-K.; Bischoff, L.L.; Wollesen, B. Work-Related Burdens and Requirements for Health Promotion Programs for Nursing Staff in Different Care Settings: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2019, 16, 3586. https://doi.org/10.3390/ijerph16193586
Otto A-K, Bischoff LL, Wollesen B. Work-Related Burdens and Requirements for Health Promotion Programs for Nursing Staff in Different Care Settings: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2019; 16(19):3586. https://doi.org/10.3390/ijerph16193586
Chicago/Turabian StyleOtto, Ann-Kathrin, Laura L. Bischoff, and Bettina Wollesen. 2019. "Work-Related Burdens and Requirements for Health Promotion Programs for Nursing Staff in Different Care Settings: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 16, no. 19: 3586. https://doi.org/10.3390/ijerph16193586
APA StyleOtto, A.-K., Bischoff, L. L., & Wollesen, B. (2019). Work-Related Burdens and Requirements for Health Promotion Programs for Nursing Staff in Different Care Settings: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 16(19), 3586. https://doi.org/10.3390/ijerph16193586





