Antibiotic Sales in Primary Care in Hubei Province, China: An Analysis of 2012–2017 Procurement Records
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Setting
2.2. Data Source
2.3. Data Analysis
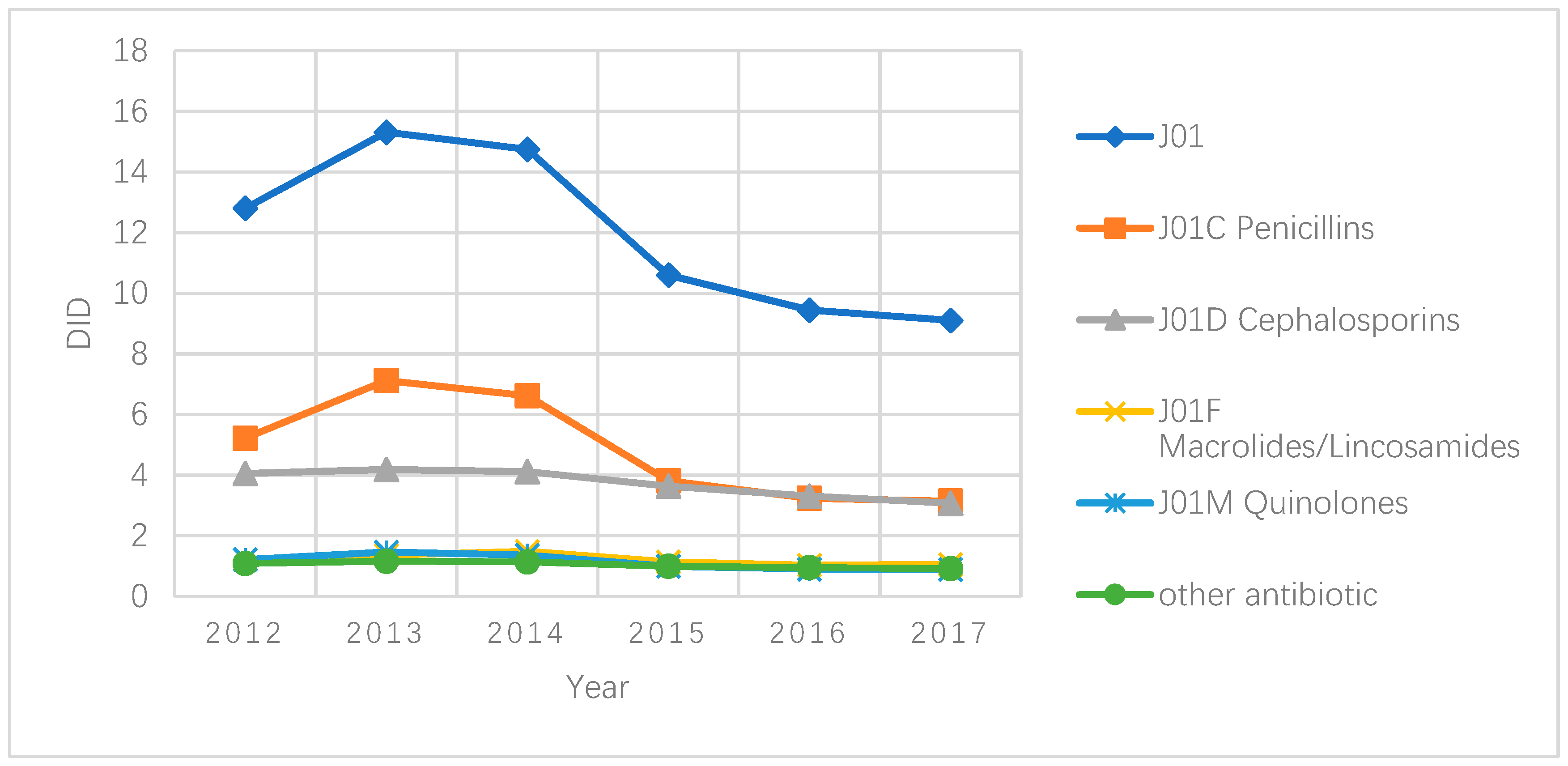
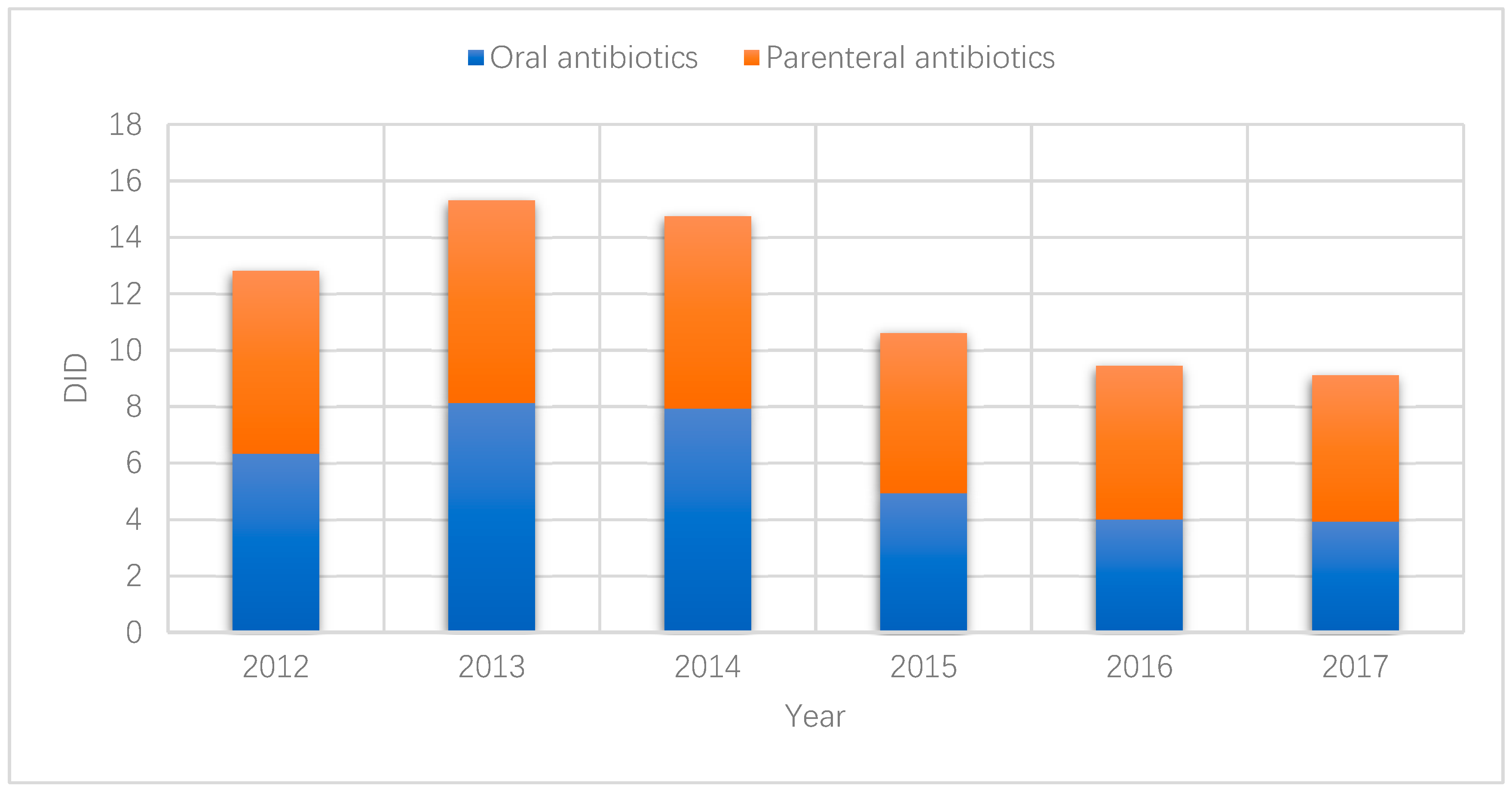
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Van Boeckel, T.P.; Gandra, S.; Ashok, A.; Caudron, Q.; Grenfell, B.T.; Levin, S.A.; Laxminarayan, R. Global antibiotic consumption 2000 to 2010: An analysis of national pharmaceutical sales data. Lancet Infect. Dis. 2014, 14, 742–750. [Google Scholar] [CrossRef]
- Ghafur, A. Overconsumption of antibiotics. Lancet Infect. Dis. 2015, 15, 377. [Google Scholar] [CrossRef]
- O’Neill, J. Antimicrobial Resistance: Tackling a Crisis for the Health and Wealth of Nations. Available online: https://amr-review.org/sites/default/files/AMR%20Review%20Paper%20-%20Tackling%20a%20crisis%20for%20the%20health%20and%20wealth%20of%20nations_1.pdf (accessed on 29 March 2019).
- Sandle, T. The antibiotic crisis and the need for new forms of antibiotics. EC Microbiol. 2014, 1, 1–3. [Google Scholar]
- Klein, E.Y.; Van Boeckel, T.P.; Martinez, E.M.; Pant, S.; Gandra, S.; Levin, S.A.; Goossens, H.; Laxminarayan, R. Global increase and geographic convergence in antibiotic consumption between 2000 and 2015. Proc. Natl. Acad. Sci. USA 2018, 115, E3463–E3470. [Google Scholar] [CrossRef] [PubMed]
- The European Centre for Disease Prevention and Control (ECDC). Surveillance of Antimicrobial Consumption in Europe 2013–2014; The European Centre for Disease Prevention and Control (ECDC): Solna Municipality, Sweden, 2018.
- Smieszek, T.; Pouwels, K.B.; Dolk, F.C.K.; Smith, D.R.M.; Hopkins, S.; Sharland, M.; Hay, A.D.; Moore, M.V.; Robotham, J.V. Potential for reducing inappropriate antibiotic prescribing in English primary care. J. Antimicrob. Chemother. 2018, 73, ii36–ii43. [Google Scholar] [CrossRef] [PubMed]
- Fleming-Dutra, K.E.; Hersh, A.L.; Shapiro, D.J.; Bartoces, M.; Enns, E.A.; File, T.M., Jr.; Finkelstein, J.A.; Gerber, J.S.; Hyun, D.Y.; Linder, J.A.; et al. Prevalence of Inappropriate Antibiotic Prescriptions Among US Ambulatory Care Visits, 2010–2011. JAMA 2016, 315, 1864–1873. [Google Scholar] [CrossRef] [PubMed]
- Wong, C.K.M.; Kung, K.; Au-Doung, P.L.W.; Ip, M.; Lee, N.; Fung, A.; Wong, S.Y.S. Antibiotic resistance rates and physician antibiotic prescription patterns of uncomplicated urinary tract infections in southern Chinese primary care. PLoS ONE 2017, 12, e0177266. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Lu, J.; Hu, S.; Cheng, K.K.; De Maeseneer, J.; Meng, Q.; Mossialos, E.; Xu, D.R.; Yip, W.; Zhang, H.; et al. The primary health-care system in China. Lancet 2017, 390, 2584–2594. [Google Scholar] [CrossRef]
- National Health Commission of the People’s Republic of China National Health Service in China 2017. Available online: http://www.nhc.gov.cn/guihuaxxs/s10743/201806/44e3cdfe11fa4c7f928c879d435b6a18.shtml (accessed on 23 March 2019).
- Yin, X.; Song, F.; Gong, Y.; Tu, X.; Wang, Y.; Cao, S.; Liu, J.; Lu, Z. A systematic review of antibiotic utilization in China. J. Antimicrob. Chemother. 2013, 68, 2445–2452. [Google Scholar] [CrossRef]
- Hay, A.D.; Thomas, M.; Montgomery, A.; Wetherell, M.; Lovering, A.; McNulty, C.; Lewis, D.; Carron, B.; Henderson, E.; MacGowan, A. The relationship between primary care antibiotic prescribing and bacterial resistance in adults in the community: A controlled observational study using individual patient data. J. Antimicrob. Chemother. 2005, 56, 146–153. [Google Scholar] [CrossRef]
- Hillier, S.; Roberts, Z.; Dunstan, F.; Butler, C.; Howard, A.; Palmer, S. Prior antibiotics and risk of antibiotic-resistant community-acquired urinary tract infection: A case-control study. J. Antimicrob. Chemother. 2007, 60, 92–99. [Google Scholar] [CrossRef]
- Samore, M.H.; Tonnerre, C.; Hannah, E.L.; Stoddard, G.J.; Borotkanics, R.J.; Haddadin, B.; Harbarth, S. Impact of Outpatient Antibiotic Use on Carriage of Ampicillin-Resistant Escherichia coli. Antimicrob. Agents Chemother. 2011, 55, 1135–1141. [Google Scholar] [CrossRef] [PubMed]
- Costelloe, C.; Metcalfe, C.; Lovering, A.; Mant, D.; Hay, A.D. Effect of antibiotic prescribing in primary care on antimicrobial resistance in individual patients: Systematic review and meta-analysis. BMJ 2010, 340, c2096. [Google Scholar] [CrossRef] [PubMed]
- Bryce, A.; Hay, A.D.; Lane, I.F.; Thornton, H.V.; Wootton, M.; Costelloe, C. Global prevalence of antibiotic resistance in paediatric urinary tract infections caused by Escherichia coli and association with routine use of antibiotics in primary care: Systematic review and meta-analysis. BMJ 2016, 352, i939. [Google Scholar] [CrossRef] [PubMed]
- Yip, W.C.; Hsiao, W.C.; Chen, W.; Hu, S.; Ma, J.; Maynard, A. Early appraisal of China’s huge and complex health-care reforms. Lancet 2012, 379, 833–842. [Google Scholar] [CrossRef]
- Hu, S.; Tang, S.; Liu, Y.; Zhao, Y.; Escobar, M.L.; de Ferranti, D. Reform of how health care is paid for in China: Challenges and opportunities. Lancet 2008, 372, 1846–1853. [Google Scholar] [CrossRef]
- Meng, Q.; Cheng, G.; Silver, L.; Sun, X.; Rehnberg, C.; Tomson, G. The impact of China’s retail drug price control policy on hospital expenditures: A case study in two Shandong hospitals. Health Policy Plan. 2005, 20, 185–196. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Han, S.; Liang, H.; Su, W.; Xue, Y.; Shi, L. Can price controls reduce pharmaceutical expenses? A case study of antibacterial expenditures in 12 Chinese hospitals from 1996 to 2005. Int. J. Health Serv. Plan. Adm. Eval. 2013, 43, 91–103. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Liu, X.; Wang, Y.; Chen, Y.; Huang, M.; Fan, M.; Lu, M.; Huang, Y.; Wang, L.; Yao, K.; et al. Antibiotic use in pulmonology wards of Chinese children’s hospitals: 2002–2006. J. Clin. Pharm. Ther. 2009, 34, 61–65. [Google Scholar] [CrossRef]
- People’s Medical Publishing House. Year Book of Health in the People’s Republic of China; People’s Medical Publishing House: Beijing, China, 2013. [Google Scholar]
- Guan, X.; Liang, H.; Xue, Y.; Shi, L. An analysis of China’s national essential medicines policy. J. Public Health Policy 2011, 32, 305–319. [Google Scholar] [CrossRef]
- Chen, M.; Wang, L.; Chen, W.; Zhang, L.; Jiang, H.; Mao, W. Does economic incentive matter for rational use of medicine? China’s experience from the essential medicines program. PharmacoEconomics 2014, 32, 245–255. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.; Liu, C.; Ferrier, J.A.; Zhou, W.; Zhang, X. The impact of the National Essential Medicines Policy on prescribing behaviours in primary care facilities in Hubei province of China. Health Policy Plan. 2013, 28, 750–760. [Google Scholar] [CrossRef] [PubMed]
- Yi, H.; Miller, G.; Zhang, L.; Li, S.; Rozelle, S. Intended and unintended consequences of China’s zero markup drug policy. Health Aff. 2015, 34, 1391–1398. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Y.; Li, L. Legislation of clinical antibiotic use in China. Lancet Infect. Dis. 2013, 13, 189–191. [Google Scholar] [CrossRef]
- Tang, Y.; Liu, C.; Zhang, Z.; Zhang, X. Effects of prescription restrictive interventions on antibiotic procurement in primary care settings: A controlled interrupted time series study in China. Cost Eff. Resour. Alloc. 2018, 16, 1. [Google Scholar] [CrossRef] [PubMed]
- The Measures for the Management of the Clinical Application of Antibacterial Drugs. Available online: http://www.moh.gov.cn/mohyzs/s3584/201205/54645.shtml (accessed on 12 July 2018).
- Coenen, S.; Ferech, M.; Haaijer-Ruskamp, F.M.; Butler, C.C.; Vander Stichele, R.H.; Verheij, T.J.; Monnet, D.L.; Little, P.; Goossens, H. European Surveillance of Antimicrobial Consumption (ESAC): Quality indicators for outpatient antibiotic use in Europe. Qual. Saf. Health Care 2007, 16, 440–445. [Google Scholar] [CrossRef] [PubMed]
- Hubei Statistics Year Book 2016; China Statistics Press: Beijinng, China, 2016.
- Department of Population and Employment Statistics National Burean of Statistics; Department of Planning and Finance Ministry of Human Resources ans Social Statistics. China Labour Statistical Yearbook 2017. Available online: http://data.cnki.net/yearbook/Single/N2018070151 (accessed on 29 March 2019).
- National Health Commission of People’s Republic of China. 2018 Year Book of Health Statistic in the People’s Republic of China; China Union Medical University Press: Beijing, China, 2018. [Google Scholar]
- Management Measures On Use of Essential Medicines in Medical Institutions in Hubei Province. Available online: http://www.chinaemed.com/Province/hubei/Docs/BaseMedFile/BaseMedFile/10674 (accessed on 1 April 2019).
- ATC/DDD Index and Guidelines. Available online: http://www.whocc.no/atc_ddd_index/ (accessed on 14 April 2019).
- The European Centre for Disease Prevention and Control (ECDC) Quality Indicators for Antibiotic Consumption in the Community. Available online: https://ecdc.europa.eu/en/antimicrobial-consumption/database/quality-indicators (accessed on 31 March 2019).
- England, P.H. English Surveillance Programme for Antimicrobial Utilisation and Resistance (ESPAUR) Report 2018. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/759975/ESPAUR_2018_report.pdf?_ga=2.34148065.152362810.1566804694-1442484965.1566116176 (accessed on 22 August 2019).
- Wu, D.; Lam, T.P.; Lam, K.F.; Zhou, X.D.; Sun, K.S. Public views towards community health and hospital-based outpatient services and their utilisation in Zhejiang, China: A mixed methods study. BMJ Open 2017, 7, e017611. [Google Scholar] [CrossRef]
- Wu, D.; Lam, T.P.; Lam, K.F.; Zhou, X.D.; Sun, K.S. Health reforms in china: The public’s choices for first-contact care in urban areas. Fam. Pract. 2017, 34, 194–200. [Google Scholar] [CrossRef][Green Version]
- Wushouer, H.; Tian, Y.; Guan, X.-D.; Han, S.; Shi, L.-W. Trends and patterns of antibiotic consumption in China’s tertiary hospitals: Based on a 5 year surveillance with sales records, 2011–2015. PLoS ONE 2017, 12, e0190314. [Google Scholar] [CrossRef]
- Zhang, Z.; Hu, Y.; Zou, G.; Lin, M.; Zeng, J.; Deng, S.; Zachariah, R.; Walley, J.; Tucker, J.D.; Wei, X. Antibiotic prescribing for upper respiratory infections among children in rural China: A cross-sectional study of outpatient prescriptions. Glob. Health Action 2017, 10, 1287334. [Google Scholar] [CrossRef]
- Chang, J.; Ye, D.; Lv, B.; Jiang, M.; Zhu, S.; Yan, K.; Tian, Y.; Fang, Y. Sale of antibiotics without a prescription at community pharmacies in urban China: A multicentre cross-sectional survey. J. Antimicrob. Chemother. 2017, 72, 1235–1242. [Google Scholar] [CrossRef] [PubMed]
- Morgan, D.J.; Okeke, I.N.; Laxminarayan, R.; Perencevich, E.N.; Weisenberg, S. Non-prescription antimicrobial use worldwide: A systematic review. Lancet Infect. Dis. 2011, 11, 692–701. [Google Scholar] [CrossRef]
- Meng, Q.; Xu, L.; Zhang, Y.; Qian, J.; Cai, M.; Xin, Y.; Gao, J.; Xu, K.; Boerma, J.T.; Barber, S.L. Trends in access to health services and financial protection in China between 2003 and 2011: A cross-sectional study. Lancet 2012, 379, 805–814. [Google Scholar] [CrossRef]
- Laxminarayan, R.; Duse, A.; Wattal, C.; Zaidi, A.K.; Wertheim, H.F.; Sumpradit, N.; Vlieghe, E.; Hara, G.L.; Gould, I.M.; Goossens, H.; et al. Antibiotic resistance-the need for global solutions. Lancet Infect. Dis. 2013, 13, 1057–1098. [Google Scholar] [CrossRef]
- Zhang, W.; Shen, X.; Wang, Y.; Chen, Y.; Huang, M.; Zeng, Q.; Fan, M.; Bergman, U.; Yang, Y. Outpatient antibiotic use and assessment of antibiotic guidelines in Chinese children’s hospitals. Eur. J. Clin. Pharmacol. 2008, 64, 821–828. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Y. Antimicrobial Stewardship in China: Systems, Actions and Future Strategies. Clin. Infect. Dis. 2018, 67, S135–S141. [Google Scholar] [CrossRef] [PubMed]
- Robertson, J.; Iwamoto, K.; Hoxha, I.; Ghazaryan, L.; Abilova, V.; Cvijanovic, A.; Pyshnik, H.; Darakhvelidze, M.; Makalkina, L.; Jakupi, A.; et al. Antimicrobial Medicines Consumption in Eastern Europeand Central Asia—An Updated Cross-National Study and Assessment of QuantitativeMetrics for Policy Action. Front. Pharmacol. 2018, 9, 1156. [Google Scholar] [CrossRef] [PubMed]
- Paterson, D.L. “Collateral damage” from cephalosporin or quinolone antibiotic therapy. Clin. Infect. Dis. 2004, 38, S341–S345. [Google Scholar] [CrossRef] [PubMed]
- Du, B.; Chen, D.C.; Liu, D.W.; Long, Y.; Shi, Y.; Wang, H.; Rui, X.; Cui, N. Restriction of third-generation cephalosporin use decreases infection-related mortality. Crit. Care Med. 2003, 31, 1088–1093. [Google Scholar] [CrossRef]
- Coenen, S.; Muller, A.; Adriaenssens, N.; Vankerckhoven, V.; Hendrickx, E.; Goossens, H. European Surveillance of Antimicrobial Consumption (ESAC): Outpatient parenteral antibiotic treatment in Europe. J. Antimicrob. Chemother. 2014, 64, 200–205. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tang, Y.; Liu, C.; Zhang, X. Public reporting as a prescriptions quality improvement measure in primary care settings in China: Variations in effects associated with diagnoses. Sci. Rep. 2016, 6, 39361. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, L.; McKee, M. Serve the people or close the sale? Profit-driven overuse of injections and infusions in China’s market-based healthcare system. Int. J. Health Plan. Manag. 2011, 26, 449–470. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Sun, X.; Birch, S.; Gong, F.; Valentijn, P.; Chen, L.; Zhang, Y.; Huang, Y.; Yang, H. People-centred integrated care in urban China. Bull. World Health Organ. 2018, 96, 843–852. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Wang, W.; Li, Y.; Zhang, J.; Pavlova, M.; Liu, H.; Yin, P.; Lu, Z. Analysis of factors influencing the outpatient workload at Chinese health centres. BMC Health Serv. Res. 2010, 10, 151. [Google Scholar] [CrossRef]
| Year | Year-End Population (10,000) | Primary Care Visit | Hospital Sector Visit | Share (%) of Primary Care |
|---|---|---|---|---|
| 2012 | 5799 | 194,226,467 | 92,367,048 | 67.77 |
| 2013 | 5799 | 221,885,235 | 98,597,112 | 69.23 |
| 2014 | 5816 | 239,407,480 | 109,767,232 | 68.56 |
| 2015 | 5851.5 | 205,444,029 | 117,219,783 | 63.67 |
| 2016 | 5885 | 212,090,000 | 126,660,279 | 62.61 |
| 2017 | 5902 | 205,080,000 | 135,382,043 | 60.24 |
| ATC Classification | Sales Measured in DID (%) | Overall % | |||||
|---|---|---|---|---|---|---|---|
| 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | ||
| J01A TETRACYCLINES | |||||||
| J01AA Tetracyclines | - | - | - | 0.024 (0.22) | 0.029 (0.31) | 0.025 (0.27) | 0.1 |
| J01C BETA-LACTAM ANTIBACTERIALS, PENICILLINS | |||||||
| J01CA Penicillins with extended spectrum | 4.076 (31.82) | 5.388 (35.19) | 4.919 (33.37) | 2.773 (26.17) | 2.197 (23.27) | 2.095 (23.00) | 29.8 |
| J01CE Beta-lactamase sensitive penicillins | 0.725 (5.66) | 1.227 (8.01) | 1.152 (7.81) | 0.452 (4.27) | 0.359 (3.80) | 0.346 (3.79) | 5.9 |
| J01CF Beta-lactamase resistant penicillins | 0.062 (0.49) | 0.055 (0.36) | 0.051 (0.35) | 0.042 (0.40) | 0.034 (0.37) | 0.030 (0.34) | 0.4 |
| J01CR Combinations of penicillins, including beta-lactamase inhibitors | 0.358 (2.80) | 0.450 (2.94) | 0.500 (3.39) | 0.550 (5.20) | 0.653 (6.92) | 0.676 (7.42) | 4.5 |
| J01D OTHER BETA-LACTAM ANTIBACTERIALS | |||||||
| J01DB First-generation cephalosporins | 0.776 (6.06) | 0.828 (5.41) | 0.761 (5.16) | 0.522 (4.93) | 0.368 (3.90) | 0.333 (3.66) | 5.0 |
| J01DC Second-generation cephalosporins | 0.952 (7.43) | 1.184 (7.73) | 1.326 (9.00) | 1.247 (11.76) | 1.109 (11.73) | 1.113 (12.23) | 9.7 |
| J01DD Third-generation cephalosporins | 2.329 (18.18) | 2.176 (14.21) | 2.034 (13.79) | 1.870 (17.65) | 1.835 (19.43) | 1.630 (17.89) | 16.5 |
| J01E SULFONAMIDES AND TRIMETHOPRIM | |||||||
| J01EC Intermediate-acting sulfonamides | - | - | 0.001 (0.01) | 0.002 (0.013) | 0.001 (0.014) | 0.001 (0.015) | 0.0 |
| J01EE Combinations of sulfonamides and trimethoprim, including derivatives | 0.016 (0.12) | 0.015 (0.10) | 0.018 (0.12) | 0.008 (0.075) | 0.003 (0.028) | 0.003 (0.029) | 0.1 |
| J01F MACROLIDES, LINCOSAMIDES AND STREPTOGRAMINS | |||||||
| J01FA Macrolides | 0.725 (5.66) | 0.809 (5.27) | 0.894 (6.06) | 0.776 (7.32) | 0.698 (7.40) | 0.729 (7.97) | 6.4 |
| J01FF Lincosamides | 0.494 (3.86) | 0.559 (3.65) | 0.597 (4.05) | 0.365 (3.45) | 0.332 (3.52) | 0.336 (3.69) | 3.7 |
| J01G AMINOGLYCOSIDE ANTIBACTERIALS | |||||||
| J01GA Streptomycins | 0.014 (0.011) | 0.013 (0.078) | 0.009 (0.06) | 0.006 (0.050) | 0.002 (0.028) | 0.002 (0.029) | 0.1 |
| J01GB Other aminoglycosides | 0.186 (1.44) | 0.150 (0.98) | 0.118 (0.80) | 0.103 (0.97) | 0.093 (0.99) | 0.078 (0.85) | 1.0 |
| J01M QUINOLONE ANTIBACTERIALS | |||||||
| J01MA Fluoroquinolones | 1.219 (9.51) | 1.466 (9.58) | 1.366 (9.26) | 1.001 (9.44) | 0.907 (9.60) | 0.901 (9.88) | 9.5 |
| J01X OTHER ANTIBACTERIALS | |||||||
| J01XD Imidazole derivatives | 0.761 (5.94) | 0.846 (5.53) | 0.770 (5.22) | 0.683 (6.44) | 0.673 (7.12) | 0.658 (7.23) | 6.1 |
| J01XX Other antibacterials | 0.113 (0.88) | 0.143 (0.93) | 0.227 (1.54) | 0.173 (1.64) | 0.151 (1.60) | 0.153 (1.68) | 1.3 |
| Year | Absolute Sales * | Relative Sales | Broad/Narrow | Seasonal Variations | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| J01_DID | J01C_DID | J01D_DID | J01F_DID | J01M_DID | J01CE_% | J01CR_% | J01DD+DE_% | J01MA_% | J01_B/N | J01_SV | J01M_SV | |
| 2012 | 21.34 | 8.70 | 6.76 | 2.03 | 2.03 | 5.66 | 2.8 | 18.19 | 9.52 | 2.98 | 6.01 | 1.15 |
| 2013 | 25.51 | 11.87 | 6.98 | 2.28 | 2.44 | 8.02 | 2.94 | 14.21 | 9.58 | 2.37 | 12.27 | 10.78 |
| 2014 | 24.57 | 11.04 | 6.87 | 2.48 | 2.28 | 7.82 | 3.39 | 13.8 | 9.26 | 2.63 | 14.39 | 17.24 |
| 2015 | 17.67 | 6.36 | 6.07 | 1.90 | 1.67 | 4.27 | 5.19 | 17.65 | 9.44 | 4.52 | 11.97 | −15.22 |
| 2016 | 15.74 | 5.41 | 5.52 | 1.72 | 1.51 | 3.8 | 6.91 | 19.43 | 9.6 | 5.78 | 7.45 | −0.88 |
| 2017 | 15.18 | 5.24 | 5.13 | 1.77 | 1.50 | 3.8 | 7.42 | 17.9 | 9.89 | 5.99 | N/A | N/A |
 Higher than all of the compared countries;
Higher than all of the compared countries;  Ranked in top 25% of compared countries;
Ranked in top 25% of compared countries;  Ranked in the middle 25% of countries above median;
Ranked in the middle 25% of countries above median;  Ranked in the middle 25% of countries below median;
Ranked in the middle 25% of countries below median;  Ranked in bottom 25% of compared countries;
Ranked in bottom 25% of compared countries;  Lower than all of the compared countries.
Lower than all of the compared countries.© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, X.; Cui, Y.; Liu, C.; Zuo, K.; Tang, Y. Antibiotic Sales in Primary Care in Hubei Province, China: An Analysis of 2012–2017 Procurement Records. Int. J. Environ. Res. Public Health 2019, 16, 3376. https://doi.org/10.3390/ijerph16183376
Zhang X, Cui Y, Liu C, Zuo K, Tang Y. Antibiotic Sales in Primary Care in Hubei Province, China: An Analysis of 2012–2017 Procurement Records. International Journal of Environmental Research and Public Health. 2019; 16(18):3376. https://doi.org/10.3390/ijerph16183376
Chicago/Turabian StyleZhang, Xinping, Youwen Cui, Chaojie Liu, Keyuan Zuo, and Yuqing Tang. 2019. "Antibiotic Sales in Primary Care in Hubei Province, China: An Analysis of 2012–2017 Procurement Records" International Journal of Environmental Research and Public Health 16, no. 18: 3376. https://doi.org/10.3390/ijerph16183376
APA StyleZhang, X., Cui, Y., Liu, C., Zuo, K., & Tang, Y. (2019). Antibiotic Sales in Primary Care in Hubei Province, China: An Analysis of 2012–2017 Procurement Records. International Journal of Environmental Research and Public Health, 16(18), 3376. https://doi.org/10.3390/ijerph16183376






