Effect of Diabetes Education Through Pattern Management on Self-Care and Self-Efficacy in Patients with Type 2 Diabetes
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Consideration
2.2. Subjects
2.3. Diabetes Education Program for the PM Education and Control Groups
2.3.1. PM Education Group
2.3.2. Control Group
2.4. Study Design and Measurements
2.4.1. General Characteristics of the Subjects
2.4.2. Self-Care Behaviors
2.4.3. Self-Efficacy
2.4.4. Physiological Index
2.4.5. Statistical Analysis
3. Results
3.1. Test of Homogeneity Between the Groups
3.1.1. General Characteristics of the Study Subjects
3.1.2. Self-Care Behavior, Self-Efficacy, and HbA1c
3.2. Comparison of Changes in Self-Care Behaviors, Self-efficacy, and HbA1c Between the Groups
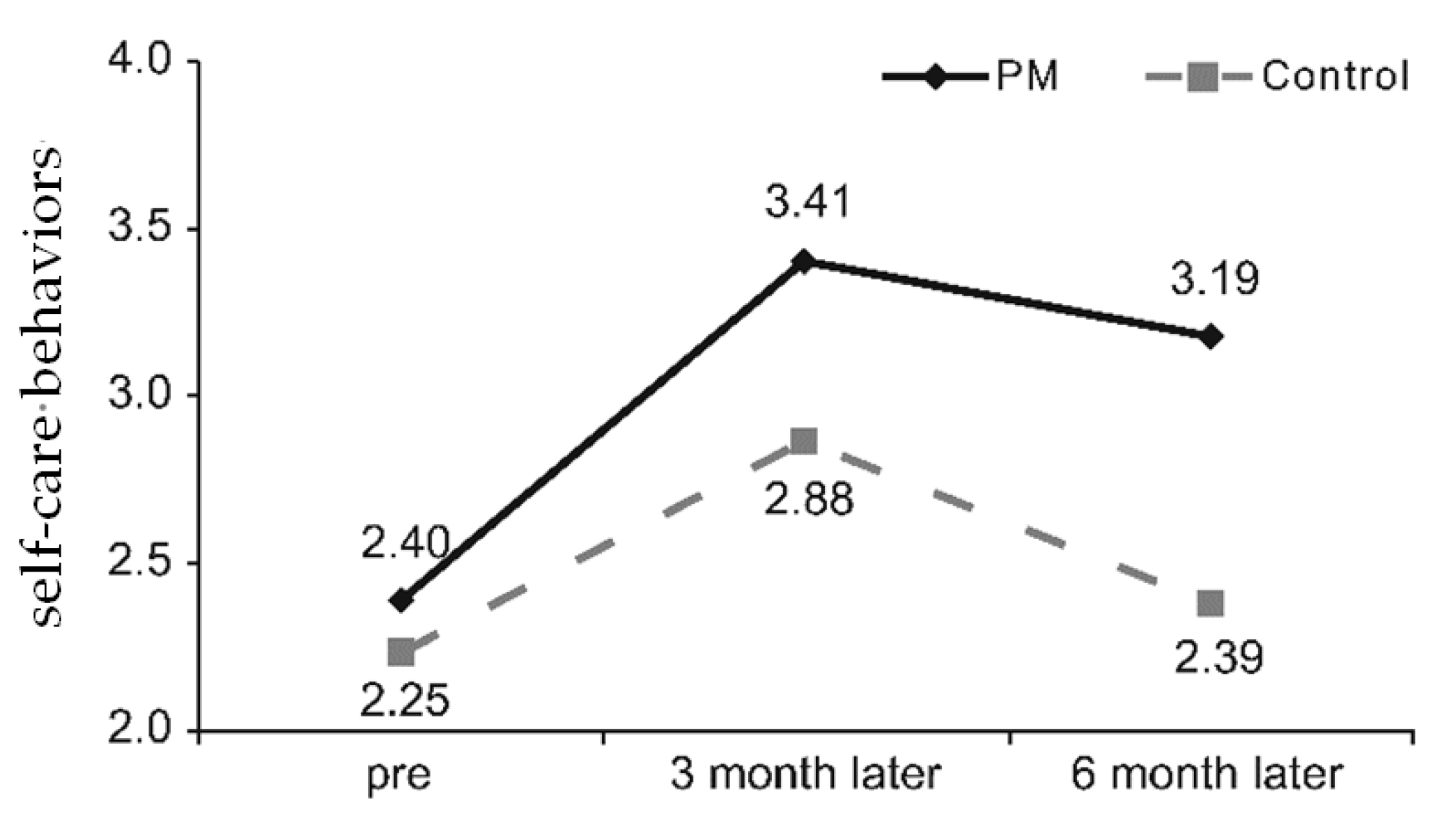
3.2.1. Self-Care Behaviors
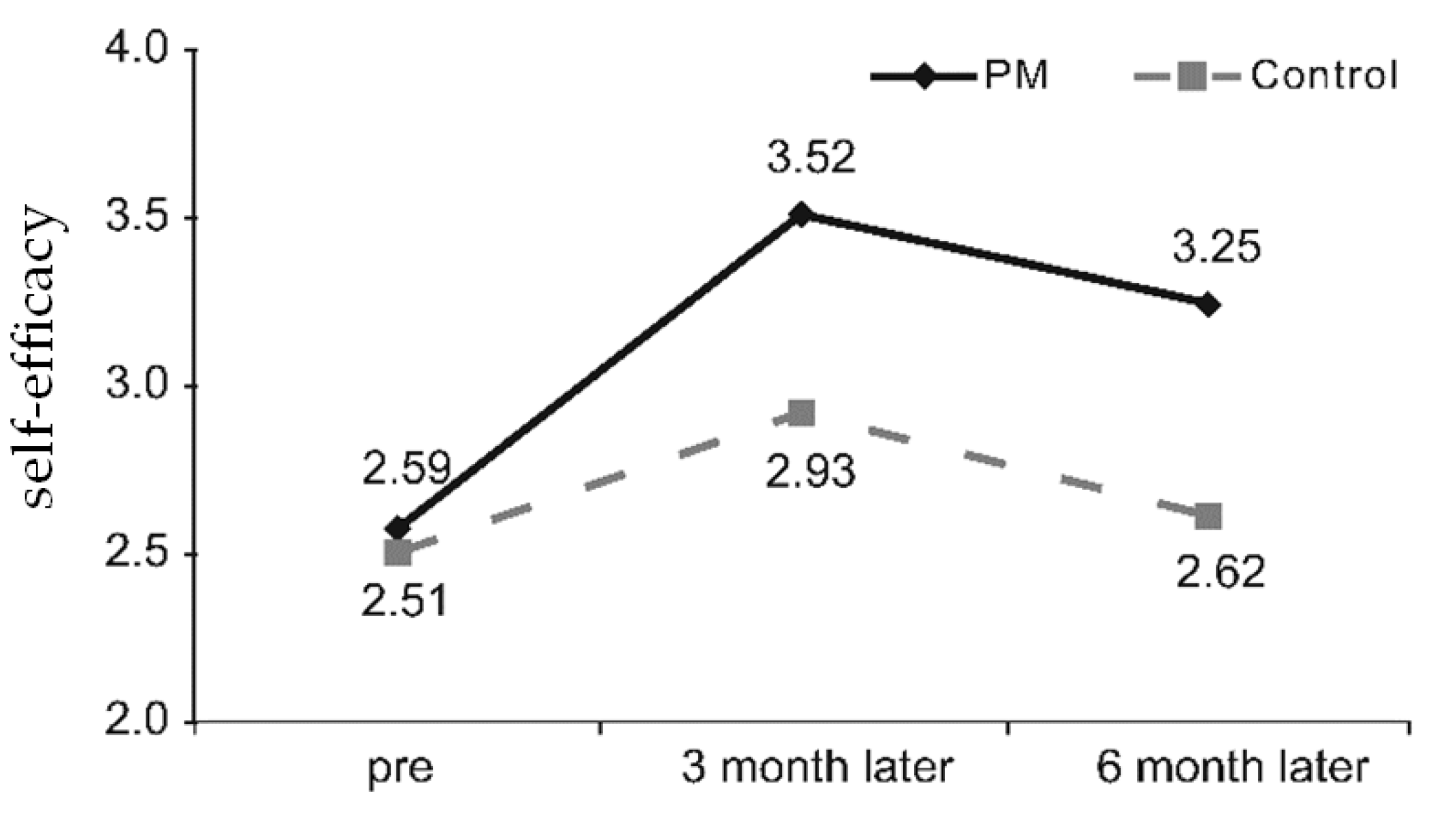
3.2.2. Self-Efficacy
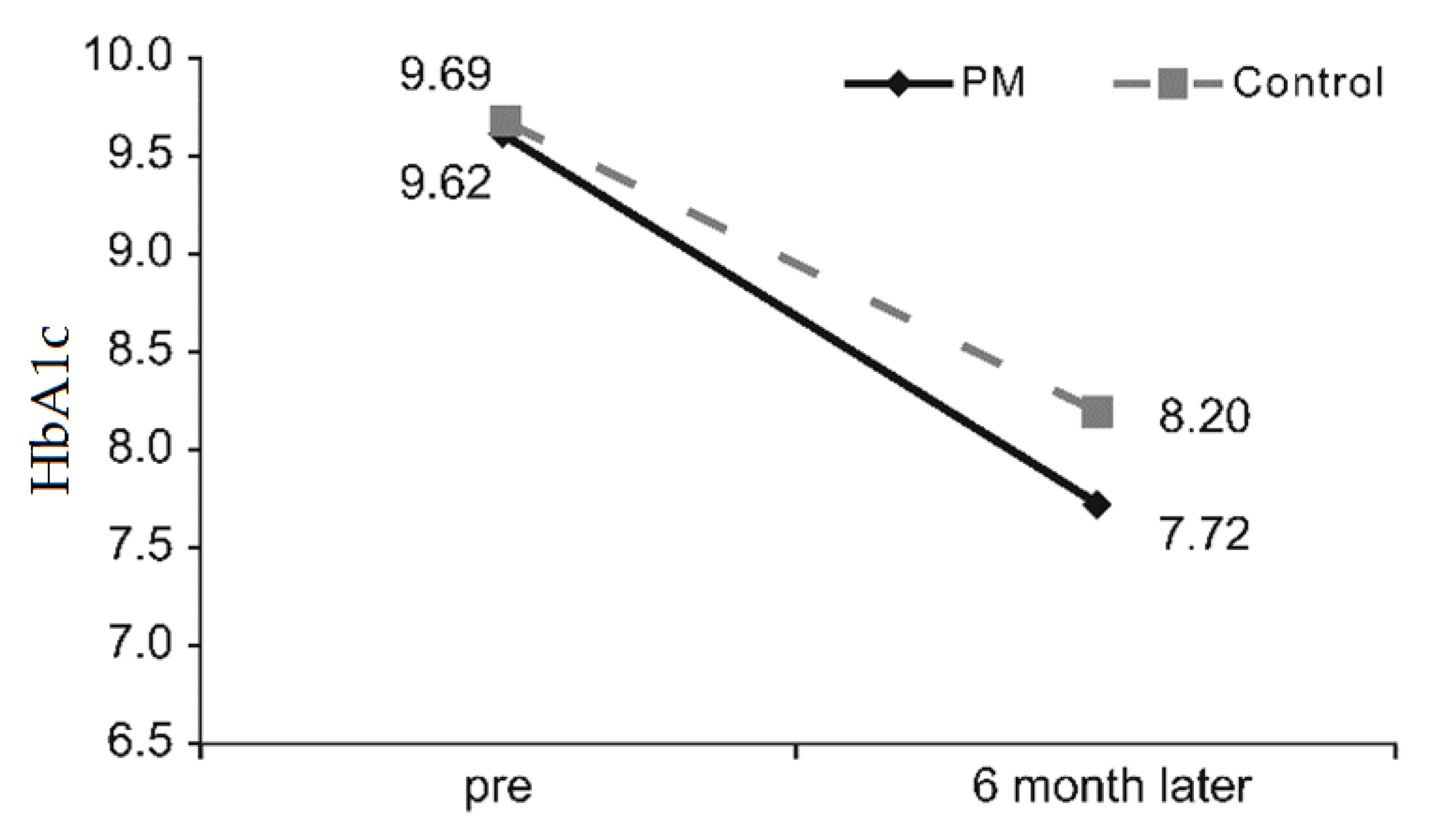
3.2.3. Physiological Index
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- World Health Organization. Global Report on Diabetes; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- Statistics Korea. Yearly statistics of causes of death. Available online: http://kostat.go.kr/portal/korea/kor_nw/2/6/2/index.board?bmode=read&bSeq=&aSeq=363268&pageNo=1&rowNum=10&navCount=10&currPg=&sTarget=title&sTxt= (accessed on 22 September 2017).
- Choi, K.A.; Jang, S.M.; Nam, H.W. Self-management practices, and disturbance of elderly diabetics. Korean Diabetes J. 2008, 32, 280–289. [Google Scholar] [CrossRef]
- Kuznetsov, L.; Griffin, S.J.; Davies, M.J.; Lauritzen, T.; Khunti, K.; Rutten, G.E.; Simmons, R.K. Diabetes-specific quality of life but not health status is independently associated with glycaemic control among patients with type 2 diabetes: A cross-sectional analysis of the ADDITION-Europe trial cohort. Diabetes Res. Clin. Pract. 2014, 104, 281–287. [Google Scholar] [CrossRef] [PubMed]
- Korean Diabetes Association. 2015 Practice Guideline on Diabetes; Korean Diabetes Association: Seoul, Korea, 2015. [Google Scholar]
- Norris, S.L.; Lau, J.; Smith, S.J.; Schmid, C.H.; Engelgau, M.M. Self-management education for adults with type 2 diabetes: A meta-analysis of the effect on glycemic control. Diabetes Care 2002, 25, 1159–1171. [Google Scholar] [CrossRef] [PubMed]
- Sarkadi, A.; Rosenqvist, U. Experience-based group education in Type 2 diabetes: A randomised controlled trial. Patient Educ. Couns. 2004, 53, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Hong, M.H.; Yoo, J.W.; Gu, M.O.; Kim, S.A.; Lee, J.R.; Gu, M.J.; Kang, Y.G.; Jang, S.H.; Park, B.S.; Shim, K.H.; et al. A study on effects and their continuity of the self regulation education program in patients with type 2 diabetes. Clinic. Diabetes 2009, 10, 187–195. [Google Scholar]
- Gu, M.O. A study of the relationship among self efficacy, self regulation, situational barriers and self care behavior in patients with diabetes mellitus. J. Korean Acad. Nurs. 1994, 24, 635–651. [Google Scholar] [CrossRef]
- Kim, H.S. Fasting blood sugar and adherence to diabetes control recommendation: Impact of education using short messaging service of cellular phone. J. Korean Biologic. Nurs. Sci. 2003, 5, 13–19. [Google Scholar]
- Kim, H. Role of diabetes educators and effectiveness of diabetes education. J. Korean Diabetes 2013, 14, 194–198. [Google Scholar] [CrossRef]
- Kim, C.G.; Chung, C.H. Effects of telephone consulting program on self-efficacy and self-care in NIDDM patients. Korean J. Adult Nurs. 2002, 14, 306–314. [Google Scholar]
- Shim, K.H. Information Desk: Effective diabetes self-management education: Focus on blood glucose pattern management. J. Korean Diabetes 2016, 17, 35–40. [Google Scholar] [CrossRef]
- Parkin, C.G.; Davidson, J.A. Value of self-monitoring blood glucose pattern analysis in improving diabetes outcomes. J. Diabetes Sci. Technol. 2009, 3, 500–508. [Google Scholar] [CrossRef]
- Choudhary, P.; Genovese, S.; Reach, G. Blood glucose pattern management in diabetes: Creating order from disorder. J. Diabetes Sci. Technol. 2013, 7, 1575–1584. [Google Scholar] [CrossRef] [PubMed]
- Powers, M.A.; Davidson, J.; Bergenstal, R.M. Glucose pattern management teaches glycemia-related problem-solving skills in a diabetes self-management education program. Diabetes Spectr. 2013, 6, 91–97. [Google Scholar] [CrossRef][Green Version]
- Grunberger, G.; Bailey, T.; Camacho, P.M.; Einhorn, D.; Garber, A.J.; Handelsman, Y.; Harrell, R.M.; Lando, H.M.; Law, B., Jr.; Leffert, J.D.; et al. Glucose Monitoring Consensus Conference Writing Committee. Proceedings from the American Association of Clinical Endocrinologists and American College of Endocrinology consensus conference on glucose monitoring. Endocr. Pract. 2015, 21, 522–533. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, S.; Scheiner, G. The role of continuous glucose monitoring in the management of type-1 and type-2 diabetes. In Evidence-Based Management of Diabetes; TFM: Shrewsbury, UK, 2012; pp. 91–110. [Google Scholar]
- Kang, Y.G. Application of Continuous Glucose Monitoring System (CGMS) and patient education. J. Korean Diabetes 2011, 12, 159–162. [Google Scholar] [CrossRef][Green Version]
- de Oliveira, A.O.T.; Bartholomew, K.; Lavin-Tompkins, J.; Sperl-Hillen, J. Use of continuous glucose monitoring as an educational tool in the primary care setting. Diabetes Spectr. 2013, 26, 120–123. [Google Scholar] [CrossRef][Green Version]
- Gehlaut, R.R.; Dogbey, G.Y.; Schwartz, F.L.; Marling, C.R.; Shubrook, J.H. Hypoglycemia in type 2 diabetes-more common than you think: A continuous glucose monitoring study. J. Diabetes Sci. Technol. 2015, 9, 999–1005. [Google Scholar] [CrossRef]
- Yoo, H.J.; An, H.G.; Park, S.Y.; Ryu, O.H.; Kim, H.Y.; Seo, J.A.; Hong, E.G.; Shin, D.H.; Kim, Y.H.; Kim, S.G.; et al. Use of a real time continuous glucose monitoring system as a motivational device for poorly controlled type 2 diabetes. Diabetes Res. Clin. Pract. 2008, 82, 73–79. [Google Scholar] [CrossRef]
- Tamborlane, W.V.; Beck, R.W.; Bode, B.W.; Buckingham, B.; Chase, H.P.; Clemons, R.; Fiallo-Scharer, R.; Fox, L.A.; Gilliam, L.K.; Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group. Continuous glucose monitoring and intensive treatment of type 1 diabetes. N. Engl. J. Med. 2008, 359, 1464–1476. [Google Scholar]
- Chetty, V.T.; Almulla, A.; Odueyungbo, A.; Thabane, L. The effect of continuous subcutaneous glucose monitoring (CGMS) versus intermittent whole blood finger-stick glucose monitoring (SBGM) on hemoglobin A1c (HBA1c) levels in Type I diabetic patients: A systematic review. Diabetes Res. Clin Pract. 2008, 81, 79–87. [Google Scholar] [CrossRef]
- Moon, S.H.; Lee, Y.W.; Ham, O.-K.; Kim, S.-H. The effect of the experience of diabetes education on knowledge, self-care behavior and glycosylated hemoglobin in type 2 diabetic patients. J. Korean Acad. Soc. Nurs. Educ. 2014, 20, 81–92. [Google Scholar] [CrossRef]
- Song, M.S.; Choi, S.Y.; Kim, S.A.; Seo, K.S.; Lee, S.J.; Kim, E.H. Development and validation of the Diabetes Management Self-efficacy Scale for Older Adults (DMSES-O). J. Muscle Joint. Health 2014, 1, 184–194. [Google Scholar] [CrossRef]
- Lee, Y.-R.; Kang, M.; Kim, P.-G. The effects of an admission-education program on knowledge, self-efficacy, self-care and glucose control in type 2 diabetes patients. J. Korean Acad. Soc. Nurs. Educ. 2008, 14, 12–19. [Google Scholar] [CrossRef]
- Allen, N.A.; Fain, J.A.; Braun, B.; Chipkin, S.R. Continuous glucose monitoring counseling improves physical activity behaviors of individuals with type 2 diabetes: A randomized clinical trial. Diabetes Res. Clin. Pract. 2008, 80, 371–379. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.A.; Park, K.M.; Sunwoo, S.; Yang, Y.J.; Seo, Y.S.; Song, S.W.; Kim, B.S.; Kim, Y.S. Factors associated with compliance using diamicron in patients with type 2 diabetes. Korean J. Health Promot. 2012, 12, 75–82. [Google Scholar]
- Osterberg, L.; Blaschke, T. Adherence to medication. N. Engl. J. Med. 2005, 353, 487–497. [Google Scholar] [CrossRef]
- Rubin, R.R. Adherence to pharmacologic therapy in patients with type 2 diabetes mellitus. Am. J. Med. 2005, 118, 27S–34S. [Google Scholar] [CrossRef]
- Park, H.S.; Lee, Y.M.; Choi, Y.; Bae, E.S.; Na, J.H.; Kim, M.S. Effect of diabetes education program on glucose metabolism and lipid metabolism, self-efficacy in NIDDM patients. Korean Rehabil. Nurs. 2001, 4, 165–178. [Google Scholar]
- Jung, J.G.; Chung, E.Y.; Kim, A.R.; Park, H.J.; Kim, Y.J.; Ban, Y.H.; Kim, J.S.; Yoon, S.J.; Kim, S.Y.; Ahn, S.K.; et al. Improvement of knowledge, self-efficacy and self-care behaviors among diabetic patients participated in the education program of Sejong Center for Hypertension and Diabetes Management. J. Agric. Med. Community Health 2017, 42, 234–243. [Google Scholar]
- Xiao-yun, Y.; Du, G.Z.; Xue, Y.Z. Effect of step-by-step self-management education on the self-efficacy of diabetic patients treated with CGMS and CSII. J. Qilu. Nurs. 2009, 2, 20–26. [Google Scholar]
- Krichbaum, K.; Aarestad, V.; Buethe, M. Exploring the connection between self-efficacy and effective diabetes self-f management. Diabetes Educator 2003, 29, 653–662. [Google Scholar] [CrossRef]
- Williams, K.E.; Bond, M.J. The roles of self-efficacy, outcome expectancies and social support in the self-care behaviours of diabetics. Psychol. Health Med. 2002, 7, 127–141. [Google Scholar] [CrossRef]
- Lee, S.H. Effect of self-efficacy promoting program on self-efficacy, metabolic control and self-care behaviors in patients with NIDDM. Korean. J. Rehabil. Nurs. 2005, 8, 59–67. [Google Scholar]
- Lee, H.Y. The effect of a diabetic group teaching program. J. Korean Acad. Nurs. 1993, 23, 170–186. [Google Scholar] [CrossRef]
- Goudswaard, A.N.; Stolk, R.P.; Zuithoff, N.P.; de Valk, H.W.; Rutten, G.E. Long-term effects of self-management education for patients with Type 2 diabetes taking maximal oral hypoglycaemic therapy: A randomized trial in primary care. Diabetes Med. 2004, 21, 491–496. [Google Scholar] [CrossRef]
- Lee, M.R.; Song, M.S. Long term effects of a self-care education program promoting self-efficacy for elderly people with diabetes. J. Korean Gerontol. Nurs. 2003, 5, 91–101. [Google Scholar]
- Sim, K.H.; Hwang, M.S. Effect of self-monitoring of blood glucose based diabetes self-management education on glycemic control in type 2 diabetes. J. Korean Acad. Soc. Nurs. Educ. 2013, 19, 127–136. [Google Scholar] [CrossRef][Green Version]

| Variables | PM Group (n = 30) | Control Group (n = 30) | χ2 or t | p-Value |
| Sex | ||||
| Male | 16 (53.3) | 21 (70.0) | 1.763 | 0.184 |
| Female | 14 (46.7) | 9 (30.0) | ||
| Age | 53.77 ± 9.22 | 53.60 ± 9.04 | 0.071 | 0.944 |
| Marriage | ||||
| Married | 26 (86.7) | 27 (90.0) | 0.162 | 0.688 |
| Single | 4 (13.3) | 3 (10.0) | ||
| Education | ||||
| ≤High school | 19 (63.3) | 19(63.3) | 2.232 | 0.526 |
| ≥College | 11 (36.7) | 11 (36.7) | ||
| Income (10,000 won) | ||||
| Low | 7 (23.3) | 4 (13.3) | 5.762 | 0.218 |
| Moderate | 6 (20.0) | 10 (33.3) | ||
| High | 17 (56.7) | 16 (53.3) | ||
| Weight | 69.36 ± 13.13 | 66.87 ± 9.85 | 0.832 | 0.409 |
| Height | 165.73 ± 10.21 | 165.77 ± 6.56 | –0.015 | 0.988 |
| Duration(y) | 8.73 ± 5.74 | 9.53 ± 7.25 | –0.474 | 0.637 |
| Treatment | ||||
| OHA | 4 (13.3) | 10 (33.3) | 4.591 | 0.101 |
| Insulin | 4 (13.3) | 1 (3.3) | ||
| OHA +Insulin | 22 (73.3) | 19 (63.3) | ||
| Complication | ||||
| No | 23 (76.7) | 21 (70.0) | 4.202 | 0.521 |
| Yes | 7 (23.3) | 9 (30.0) | ||
| Admission | ||||
| Yes | 8 (26.7) | 7 (23.3) | 0.089 | 0.766 |
| No | 22 (73.3) | 23 (76.7) | ||
| Homogeneity of self-care, self- efficacy, and HbA1c according to education groups (mean ± SD) | ||||
| Self-care behavior | 2.40 ± 0.33 | 2.25 ± 0.35 | 1.798 | 0.077 |
| Self-efficacy | 2.59 ± 0.36 | 2.51 ± 0.40 | 0.736 | 0.465 |
| HbA1c | 9.56 ± 1.22 | 9.94 ± 1.80 | –0.976 | 0.334 |
| Variables | Self-Care Behavior | Self-Efficacy | HbA1c |
|---|---|---|---|
| Self-care behavior | 1 | ||
| Self-efficacy | 0.833 *** | 1 | |
| HbA1c | –0.258 * | –0.300 * | 1 |
| Variables | Group | M ± SD | F | p | |||
|---|---|---|---|---|---|---|---|
| Pre | 3 Month Later | 6 Month Later | |||||
| Dietry related | CGMS | 2.20 ± 0.37 | 3.26 ± 0.42 | 2.97 ± 0.47 | Time | 118.591 *** | <0.001 |
| Control | 2.13 ± 0.42 | 2.77 ± 0.48 | 2.28 ± 0.42 | Group | 20.427 *** | <0.001 | |
| Time × group | 16.600 *** | <0.001 | |||||
| Medication related | CGMS | 3.03 ± 0.51 | 3.83 ± 0.34 | 3.64 ± 0.49 | Time | 35.584 *** | <0.001 |
| Control | 2.62 ± 0.91 | 3.24 ± 0.57 | 2.88 ± 0.65 | Group | 23.525 *** | <0.001 | |
| Time × group | 2.189 | 0.128 | |||||
| Exercise related | CGMS | 2.12 ± 0.81 | 3.37 ± 0.56 | 3.12 ± 0.78 | Time | 42.969 *** | <0.001 |
| Control | 2.40 ± 0.84 | 2.89 ± 0.84 | 2.26 ± 0.69 | Group | 4.716 * | 0.034 | |
| Time × group | 19.372 *** | <0.001 | |||||
| Self-management related | CGMS | 2.55 ± 0.46 | 3.47 ± 0.38 | 3.34 ± 0.42 | Time | 53.951 *** | <0.001 |
| Control | 2.13 ± 0.61 | 2.85 ± 0.57 | 2.38 ± 0.53 | Group | 54.773 *** | <0.001 | |
| Time × group | 5.671 ** | 0.009 | |||||
| Variables | Group | M ± SD | F | p | |||
|---|---|---|---|---|---|---|---|
| pre | 3 Month Later | 6 Month Later | |||||
| Proper exercise | CGMS | 2.58 ± 0.63 | 3.38 ± 0.57 | 3.13 ± 0.67 | Time | 20.526 *** | <0.001 |
| Control | 2.83 ± 0.62 | 3.00 ± 0.60 | 2.75 ± 0.47 | Group | 1.840 | 0.180 | |
| Time × group | 11.743 *** | <0.001 | |||||
| A healthy diet | CGMS | 2.62 ± 0.50 | 3.48 ± 0.58 | 3.22 ± 0.49 | Time | 32.511 *** | <0.001 |
| Control | 2.57 ± 0.60 | 3.02 ± 0.53 | 2.73 ± 0.41 | Group | 12.086 ** | 0.001 | |
| Time × group | 4.481 * | 0.019 | |||||
| Monitoring of blood sugar and resolving problems with hypoglycemia | CGMS | 2.64 ± 0.54 | 3.63 ± 0.40 | 3.36 ± 0.57 | Time | 50.277 *** | <0.001 |
| Control | 2.39 ± 0.63 | 2.93 ± 0.47 | 2.57 ± 0.50 | Group | 32.510 *** | <0.001 | |
| Time × group | 7.126 ** | 0.003 | |||||
| Hyperglycemia problem solving | CGMS | 2.05 ± 0.81 | 3.38 ± 0.57 | 3.22 ± 0.55 | Time | 66.011 *** | <0.001 |
| Control | 1.98 ± 0.72 | 2.83 ± 0.77 | 2.30 ± 0.52 | Group | 15.217 *** | <0.001 | |
| Time × group | 9.654 *** | <0.001 | |||||
| Understanding treatment for prevention of complications | CGMS | 2.81 ± 0.52 | 3.65 ± 0.42 | 3.36 ± 0.52 | Time | 45.116 *** | <0.001 |
| Control | 2.66 ± 0.49 | 3.06 ± 0.40 | 2.78 ± 0.35 | Group | 23.849 *** | <0.001 | |
| Time × group | 7.316 ** | 0.002 | |||||
| Coping with medication and psychological difficulties | CGMS | 2.56 ± 0.53 | 3.40 ± 0.40 | 3.10 ± 0.51 | Time | 21.420 *** | <0.001 |
| Control | 2.59 ± 0.56 | 2.71 ± 0.35 | 2.50 ± 0.47 | Group | 22.716 *** | <0.001 | |
| Time × group | 14.206 *** | <0.001 | |||||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, S.-K.; Shin, D.-H.; Kim, Y.-H.; Lee, K.-S. Effect of Diabetes Education Through Pattern Management on Self-Care and Self-Efficacy in Patients with Type 2 Diabetes. Int. J. Environ. Res. Public Health 2019, 16, 3323. https://doi.org/10.3390/ijerph16183323
Lee S-K, Shin D-H, Kim Y-H, Lee K-S. Effect of Diabetes Education Through Pattern Management on Self-Care and Self-Efficacy in Patients with Type 2 Diabetes. International Journal of Environmental Research and Public Health. 2019; 16(18):3323. https://doi.org/10.3390/ijerph16183323
Chicago/Turabian StyleLee, Sung-Kyoung, Dong-Hyun Shin, Yong-Hyun Kim, and Kang-Sook Lee. 2019. "Effect of Diabetes Education Through Pattern Management on Self-Care and Self-Efficacy in Patients with Type 2 Diabetes" International Journal of Environmental Research and Public Health 16, no. 18: 3323. https://doi.org/10.3390/ijerph16183323
APA StyleLee, S.-K., Shin, D.-H., Kim, Y.-H., & Lee, K.-S. (2019). Effect of Diabetes Education Through Pattern Management on Self-Care and Self-Efficacy in Patients with Type 2 Diabetes. International Journal of Environmental Research and Public Health, 16(18), 3323. https://doi.org/10.3390/ijerph16183323




