Patient Satisfaction with Health Care Services; An Application of Physician’s Behavior as a Moderator
Abstract
1. Introduction
2. Review of Literature and Hypotheses
2.1. Healthcare Service and Patient Satisfaction
2.2. Laboratory and Diagnostic Care
2.3. Preventive Healthcare
2.4. Prenatal Care
2.5. Physician’s Behaviour
3. Methods
3.1. Study Setting
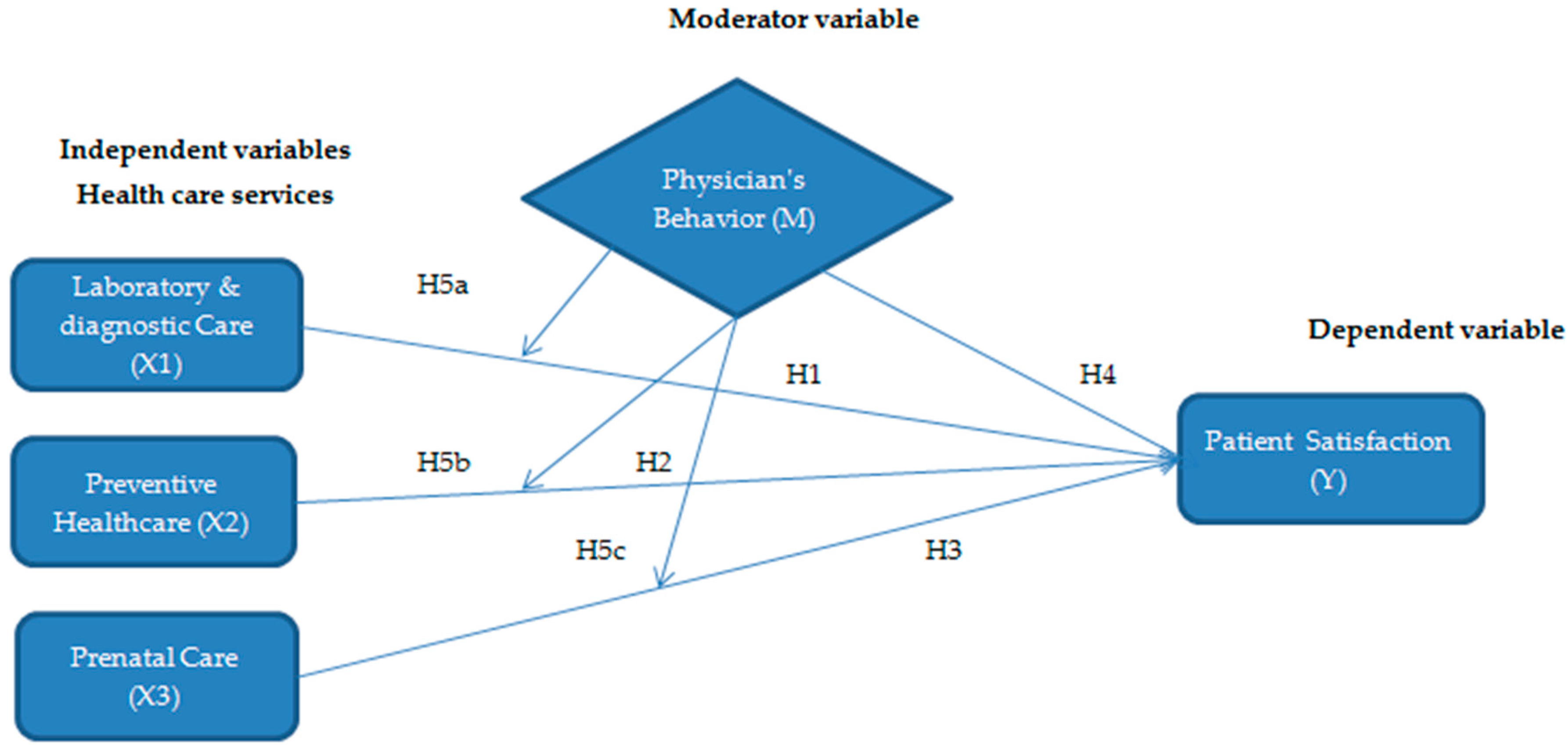
3.2. Hypothesized Model
3.3. Participants and Data Collection Procedure
3.4. Frequency Analysis
3.5. Measurement Instruments and Cronbach’s Alpha Reliability
4. Results
4.1. Descriptive Statistics
4.2. Multiple Regression Analysis and Results Interpretation
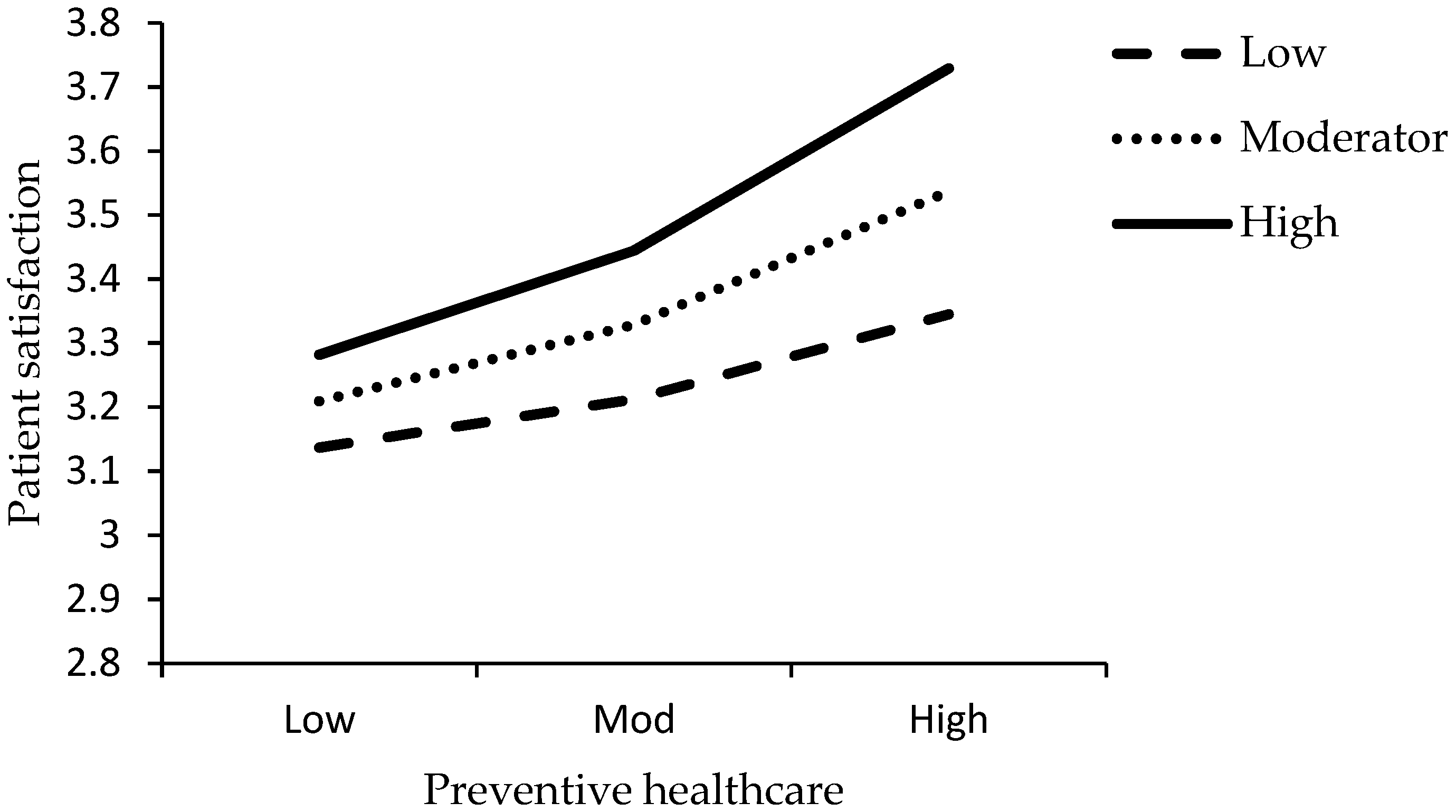
4.3. Moderation Analysis
4.4. Interpretation of Plotting
5. Discussion
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Li, M.; Lowrie, D.B.; Huang, C.-Y.; Lu, X.-C.; Zhu, Y.-C.; Wu, X.-H.; Shayiti, M.; Tan, Q.-Z.; Yang, H.-L.; Chen, S.-Y. Evaluating patients’ perception of service quality at hospitals in nine Chinese cities by use of the ServQual scale. Asian Pac. J. Trop. Biomed. 2015, 5, 497–504. [Google Scholar] [CrossRef]
- Bleustein, C.; Rothschild, D.B.; Valen, A.; Valatis, E.; Schweitzer, L.; Jones, R. Wait times, patient satisfaction scores, and the perception of care. Am. J. Manag. Care 2014, 20, 393–400. [Google Scholar] [PubMed]
- Lee, M.A.; Yom, Y.-H. A comparative study of patients’ and nurses’ perceptions of the quality of nursing services, satisfaction and intent to revisit the hospital: A questionnaire survey. Int. J. Nurs. Stud. 2007, 44, 545–555. [Google Scholar] [CrossRef] [PubMed]
- Karatepe, O.M.; Yavas, U.; Babakus, E. Measuring service quality of banks: Scale development and validation. J. Retail. Consum. Serv. 2005, 12, 373–383. [Google Scholar] [CrossRef]
- Zarei, E.; Daneshkohan, A.; Pouragha, B.; Marzban, S.; Arab, M. An empirical study of the impact of service quality on patient satisfaction in private hospitals, Iran. Glob. J. Health Sci. 2015, 7. [Google Scholar] [CrossRef] [PubMed]
- Ranaweera, C.; Prabhu, J. The influence of satisfaction, trust and switching barriers on customer retention in a continuous purchasing setting. Int. J. Serv. Ind. Manag. 2003, 14, 374–395. [Google Scholar] [CrossRef]
- Sun, J.; Hu, G.; Ma, J.; Chen, Y.; Wu, L.; Liu, Q.; Hu, J.; Livoti, C.; Jiang, Y.; Liu, Y. Consumer satisfaction with tertiary healthcare in China: Findings from the 2015 China National Patient Survey. Int. J. Qual. Health Care 2017, 29, 213–221. [Google Scholar] [CrossRef]
- Shabbir, A.; Malik, S.A.; Malik, S.A. Measuring patients’ healthcare service quality perceptions, satisfaction, and loyalty in public and private sector hospitals in Pakistan. Int. J. Qual. Reliab. Manag. 2016, 33, 538–557. [Google Scholar] [CrossRef]
- Li, Z.; Hou, J.; Lu, L.; Tang, S.; Ma, J. On residents’ satisfaction with community health services after health care system reform in Shanghai, China, 2011. BMC Public Health 2012, S9. [Google Scholar] [CrossRef]
- Nie, Y.; Mao, X.; Cui, H.; He, S.; Li, J.; Zhang, M. Hospital survey on patient safety culture in China. BMC Health Serv. Res. 2013, 13, 228. [Google Scholar] [CrossRef]
- Ganasegeran, K.; Perianayagam, W.; Abdul Manaf, R.; Jadoo, A.; Ahmed, S.; Al-Dubai, S.A.R. Patient satisfaction in Malaysia’s busiest outpatient medical care. Sci. World J. 2015, 2015, 714754. [Google Scholar] [CrossRef] [PubMed]
- Joosten, E.A.; DeFuentes-Merillas, L.; De Weert, G.; Sensky, T.; Van Der Staak, C.; de Jong, C.A. Systematic review of the effects of shared decision-making on patient satisfaction, treatment adherence and health status. Psychother. Psychosom. 2008, 77, 219–226. [Google Scholar] [CrossRef] [PubMed]
- Mohd, A.; Chakravarty, A. Patient satisfaction with services of the outpatient department. Med. J. Armed Forces India 2014, 70, 237–242. [Google Scholar] [CrossRef] [PubMed]
- Dong, W.; Zhang, Q.; Yan, C.; Fu, W.; Xu, L. Residents’ satisfaction with primary medical and health services in Western China. BMC Health Serv. Res. 2017, 17, 298. [Google Scholar] [CrossRef]
- Jakobsson, L.; Holmberg, L. Quality from the patient’s perspective: A one-year trial. Int. J. Health Care Qual. Assur. 2012, 25, 177–188. [Google Scholar] [CrossRef] [PubMed]
- Manimay, G. Measuring patient satisfaction. Leadersh. Health Serv. 2014, 27, 240–254. [Google Scholar]
- Zeithaml, V.A. Service quality, profitability, and the economic worth of customers: What we know and what we need to learn. J. Acad. Mark. Sci. 2000, 28, 67–85. [Google Scholar] [CrossRef]
- Niba, M.B. Communication between Healthcare Workers and Isizulu Speaking Female Patients at the Scottsville Clinic. Master’s Thesis, University of Natal, Pietermaritzburg, South Africa, 2000. [Google Scholar]
- Ryu, S.; Ho, S.H.; Han, I. Knowledge sharing behavior of physicians in hospitals. Expert Syst. Appl. 2003, 25, 113–122. [Google Scholar] [CrossRef]
- Fisher, A.W. Patients’ evaluation of outpatient medical care. Acad. Med. 1971, 46, 238–244. [Google Scholar] [CrossRef]
- Wolf, M.H.; Putnam, S.M.; James, S.A.; Stiles, W.B. The Medical Interview Satisfaction Scale: Development of a scale to measure patient perceptions of physician behavior. J. Behav. Med. 1978, 1, 391–401. [Google Scholar] [CrossRef]
- Hussain, A.; Asif, M.; Jameel, A.; Hwang, J. Measuring OPD Patient Satisfaction with Different Service Delivery Aspects at Public Hospitals in Pakistan. Int. J. Environ. Res. Public Health 2019, 16, 2340. [Google Scholar] [CrossRef] [PubMed]
- Elleuch, A. Patient satisfaction in Japan. Int. J. Health Care Qual. Assur. 2008, 21, 692–705. [Google Scholar] [CrossRef] [PubMed]
- Grönroos, C. A service quality model and its marketing implications. Eur. J. Mark. 1984, 18, 36–44. [Google Scholar] [CrossRef]
- Arasli, H.; Haktan Ekiz, E.; Turan Katircioglu, S. Gearing service quality into public and private hospitals in small islands: Empirical evidence from Cyprus. Int. J. Health Care Qual. Assur. 2008, 21, 8–23. [Google Scholar] [CrossRef] [PubMed]
- Andaleeb, S.S. Service quality perceptions and patient satisfaction: A study of hospitals in a developing country. Soc. Sci. Med. 2001, 52, 1359–1370. [Google Scholar] [CrossRef]
- Bakan, I.; Buyukbese, T.; Ersahan, B. The impact of total quality service (TQS) on healthcare and patient satisfaction: An empirical study of Turkish private and public hospitals. Int. J. Health Plan. Manag. 2014, 29, 292–315. [Google Scholar] [CrossRef] [PubMed]
- Leisen Pollack, B. The nature of the service quality and satisfaction relationship: Empirical evidence for the existence of satisfiers and dissatisfiers. Manag. Serv. Qual. Int. J. 2008, 18, 537–558. [Google Scholar] [CrossRef]
- Cronin, J.J., Jr.; Taylor, S.A. Measuring service quality: A reexamination and extension. J. Mark. 1992, 56, 55–68. [Google Scholar] [CrossRef]
- Badri, M.A.; Attia, S.; Ustadi, A.M. Healthcare quality and moderators of patient satisfaction: Testing for causality. Int. J. Health Care Qual. Assur. 2009, 22, 382–410. [Google Scholar] [CrossRef]
- Asif, M.; Jameel, A.; Sahito, N.; Hwang, J.; Hussain, A.; Manzoor, F. Can leadership enhance patient satisfaction? Assessing the role of administrative and medical quality. Int. J. Environ. Res. Public Health 2019, 16, 3212. [Google Scholar] [CrossRef]
- Brennan, P.F. Patient satisfaction and normative decision theory. J. Am. Med. Inform. Assoc. 1995, 2, 250–259. [Google Scholar] [CrossRef] [PubMed]
- Chahal, H.; Mehta, S. Modeling patient satisfaction construct in the Indian health care context. Int. J. Pharm. Healthc. Mark. 2013, 7, 75–92. [Google Scholar] [CrossRef]
- Naidu, A. Factors affecting patient satisfaction and healthcare quality. Int. J. Health Care Qual. Assur. 2009, 22, 366–381. [Google Scholar] [CrossRef] [PubMed]
- Thimbleby, H. Technology and the future of healthcare. J. Public Health Res. 2013, 2, e28. [Google Scholar] [CrossRef] [PubMed]
- Desalegn, D.M.; Abay, S.; Taye, B. The availability and functional status of focused antenatal care laboratory services at public health facilities in Addis Ababa, Ethiopia. BMC Res. Notes 2016, 9, 403. [Google Scholar] [CrossRef] [PubMed]
- George, M. The role of basic laboratory services in strengthening primary health centres. Indian J. Med. Ethics 2011, 8, 161–163. [Google Scholar] [CrossRef] [PubMed]
- Mindaye, T.; Taye, B. Patients satisfaction with laboratory services at antiretroviral therapy clinics in public hospitals, Addis Ababa, Ethiopia. BMC Res. Notes 2012, 5, 184. [Google Scholar] [CrossRef] [PubMed]
- Abera, R.G.; Abota, B.A.; Legese, M.H.; Negesso, A.E. Patient satisfaction with clinical laboratory services at Tikur Anbessa specialized hospital, Addis Ababa, ethiopia. Patient Prefer. Adherence 2017, 11, 1181–1188. [Google Scholar] [CrossRef] [PubMed]
- Kamra, V.; Singh, H.; Kumar De, K. Factors affecting patient satisfaction: An exploratory study for quality management in the health-care sector. Total Qual. Manag. Bus. Excell. 2016, 27, 1013–1027. [Google Scholar] [CrossRef]
- Wankar, A.D. Study of determination of laboratory turnaround time in tertiary care hospital in India. Int. J. Res. Med. Sci. 2017, 2, 1396–1401. [Google Scholar] [CrossRef]
- Mustafa-Alsheikh, G.Y.; Murtadha, N.; Al-Taweel, A.S. The Role of Laboratory Diagnosis in Primary Health Care Delivery: Community Based versus Hospital–Based Approach. Med. J. Tikrit Univ. 1999, 5, 21–25. [Google Scholar]
- Cueto, M. The origins of primary health care and selective primary health care. Am. J. Public Health 2004, 94, 1864–1874. [Google Scholar] [CrossRef] [PubMed]
- Beaglehole, R.; Epping-Jordan, J.; Patel, V.; Chopra, M.; Ebrahim, S.; Kidd, M.; Haines, A. Improving the prevention and management of chronic disease in low-income and middle-income countries: A priority for primary health care. Lancet 2008, 372, 940–949. [Google Scholar] [CrossRef]
- Balas, E.A.; Weingarten, S.; Garb, C.T.; Blumenthal, D.; Boren, S.A.; Brown, G.D. Improving preventive care by prompting physicians. Arch. Intern. Med. 2000, 160, 301–308. [Google Scholar] [CrossRef]
- Mazza, D.; Shand, L.K.; Warren, N.; Keleher, H.; Browning, C.J.; Bruce, E.J. General practice and preventive health care: A view through the eyes of community members. Med. J. Aust. 2011, 195, 180–183. [Google Scholar]
- Elley, C.R.; Kerse, N.; Arroll, B.; Robinson, E. Effectiveness of counselling patients on physical activity in general practice: Cluster randomised controlled trial. BMJ 2003, 326, 793. [Google Scholar] [CrossRef] [PubMed]
- Budhwani, H.; Hearld, K.R.; Harbison, H. Individual and area level factors associated with prenatal, delivery, and postnatal care in Pakistan. Matern. Child Health J. 2015, 19, 2138–2146. [Google Scholar] [CrossRef]
- Fekede, B. Antenatal care services utilization and factors associated in Jimma Town (south west Ethiopia). Ethiop. Med. J. 2007, 45, 123–133. [Google Scholar]
- Gu, E.; Page-Jarrett, I. The top-level design of social health insurance reforms in China: Towards universal coverage, improved benefit design, and smart payment methods. J. Chin. Gov. 2018, 3, 331–350. [Google Scholar] [CrossRef]
- Ajaegbu, O.O. Perceived Challenges of Using Maternal Healthcare Services in Nigeria. Available online: https://go.galegroup.com/ps/anonymous?id=GALE%7CA365455677&sid=googleScholar&v=2.1&it=r&linkaccess=abs&issn=21516200&p=AONE&sw=w (accessed on 9 September 2019).
- Asim, M.; Malik, N.; Siddiqui, S.; Nawaz, W.; Ali, F. Antenatal Health Care; A Literature Review of Antenatal and Postnatal Health Care Utilization in Pakistan. Prof. Med. J. 2017, 24. [Google Scholar] [CrossRef]
- Falah, M.A. Females’ satisfaction and perception about prenatal care services at primary health care centres. Int. J. Sci. Res. 2015, 5, 620–627. [Google Scholar]
- Ajaegbu, O.O. Access and Utilization of Prenatal Health Care Services in Rural Communities: A Study of Isiekenesi in Imo State. Int. J. Health Serv. 2017, 47, 795–806. [Google Scholar] [CrossRef] [PubMed]
- Galle, A.; Van Parys, A.-S.; Roelens, K.; Keygnaert, I. Expectations and satisfaction with antenatal care among pregnant women with a focus on vulnerable groups: A descriptive study in Ghent. BMC Womens Health 2015, 15, 112. [Google Scholar] [CrossRef] [PubMed]
- Prudêncio, P.S.; Mamede, F.V.; Dantas, R.A.S.; Souza, L.D.; Mamede, M.V. Adaptation and validation of the Patient Expectations and Satisfaction with Prenatal Care instrument among Brazilian pregnant women. Rev. Lat. Am. Enferm. 2013, 21, 704–710. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Swaiman, K.F.; Ashwal, S.; Ferriero, D.M.; Schor, N.F. Swaiman’s Pediatric Neurology—E-Book: Principles and Practice; Elsevier Health Sciences: New York, NY, USA, 2011. [Google Scholar]
- Robin DiMatteo, M.; Prince, L.M.; Taranta, A. Patients’ percentions of physicians’ behavior. J. Community Health 1979, 4, 280–290. [Google Scholar] [CrossRef]
- Becker, M.H.; Maiman, L.A. Sociobehavioral determinants of compliance with health and medical care recommendations. Med. Care 1975, 13, 10–24. [Google Scholar] [CrossRef] [PubMed]
- Hayes-Bautista, D.E. Modifying the treatment: Patient compliance, patient control and medical care. Soc. Sci. Med. (1967) 1976, 10, 233–238. [Google Scholar] [CrossRef]
- Korsch, B.M.; Gozzi, E.K.; Francis, V. Gaps in doctor-patient communication: I. Doctor-patient interaction and patient satisfaction. Pediatrics 1968, 42, 855–871. [Google Scholar] [PubMed]
- Fremon, B.; Negrete, V.F.; Davis, M.; Korsch, B.M. Gaps in doctor-patient communication: Doctor-patient interaction analysis. Pediatr. Res. 1971, 5, 298–311. [Google Scholar] [CrossRef][Green Version]
- Linn, L.S. Factors associated with patient evaluation of health care. Milbank Meml. Fund Q. Health Soc. 1975, 53, 531–548. [Google Scholar] [CrossRef]
- Claus, P.J.; Diamond, S.; Mills, M.A. South Asian Folklore: An Encyclopedia: Afghanistan, Bangladesh, India, Nepal, Pakistan, Sri Lanka; Taylor & Francis: Abingdon, UK, 2003. [Google Scholar]
- Bowling, A. Research Methods in Health: Investigating Health and Health Services; McGraw-Hill Education: New York, NY, USA, 2014. [Google Scholar]
- Asif, M.; Qing, M.; Hwang, J.; Shi, H. Ethical leadership, affective commitment, work engagement, and creativity: Testing a multiple mediation approach. Sustainability 2019, 11, 4489. [Google Scholar] [CrossRef]
- Almatrafi, D.; Altaweel, N.; Abdelfattah, M.; Alomari, A.; Yaseen, W.; Alsulami, M.; Abonaji, F.; Alqazlan, M.; Darrar, H. Assessment of Customer Satisfaction with the Clinical Laboratory Services Provided in King Abdullah Medical City, Makkah. Egypt. J. Hosp. Med. 2018, 70, 2029–2037. [Google Scholar] [CrossRef]
- Parchman, M.L.; Burge, S.K. The patient-physician relationship, primary care attributes, and preventive services. Fam. Med. Kans. City 2004, 36, 22–27. [Google Scholar]
- Sword, W.; Heaman, M.; Biro, M.A.; Homer, C.; Yelland, J.; Akhtar-Danesh, N.; Bradford-Janke, A. Quality of prenatal care questionnaire: Psychometric testing in an Australia population. BMC Pregnancy Childbirth 2015, 15, 214. [Google Scholar] [CrossRef]
- Soomro, M.H.; Magsi, M.; Lahmar, O. Patient Satisfaction with Health Care Services in Outpatient Department of A Dental College Hospital In Pakistan. Update Dent. Coll. J. 2018, 8, 55–60. [Google Scholar] [CrossRef][Green Version]
- Nunnally, J.C.; Bernstein, I.H. Psychometric Theory; Tata McGraw-Hill: New Delhi, India, 2010. [Google Scholar]
- Qing, M.; Asif, M.; Hussain, A.; Jameel, A. Exploring the impact of ethical leadership on job satisfaction and organizational commitment in public sector organizations: The mediating role of psychological empowerment. Rev. Manag. Sci. 2019, 1–28. [Google Scholar] [CrossRef]
- Jameel, A.; Asif, M.; Hussain, A. Good Governance and Public Trust: Assessing the Mediating Effect of E-Government in Pakistan. Lex Localis-J. Local Self-Gov. 2019, 17, 299–320. [Google Scholar] [CrossRef]
- Manzoor, F.; Wei, L.; Nurunnabi, M.; Subhan, Q.A.; Shah, S.I.A.; Fallatah, S. The impact of transformational leadership on job performance and CSR as mediator in SMEs. Sustainability 2019, 11, 436. [Google Scholar] [CrossRef]
- Aiken, L.S.; West, S.G.; Reno, R.R. Multiple Regression: Testing and Interpreting Interactions; Sage: Berlin, Germany, 1991. [Google Scholar]
- Han, H.; Sahito, N.; Thi Nguyen, T.V.; Hwang, J.; Asif, M. Exploring the features of sustainable urban form and the factors that provoke shoppers towards shopping malls. Sustainability 2019, 11, 4798. [Google Scholar] [CrossRef]
- Manzoor, F.; Wei, L.; Bányai, T.; Nurunnabi, M.; Subhan, Q.A. An examination of sustainable HRM practices on job performance: An application of training as a moderator. Sustainability 2019, 11, 2263. [Google Scholar] [CrossRef]
- Preacher, K.J.; Rucker, D.D.; Hayes, A.F. Addressing moderated mediation hypotheses: Theory, methods, and prescriptions. Multivar. Behav. Res. 2007, 42, 185–227. [Google Scholar] [CrossRef] [PubMed]
- Wu, A.D.; Zumbo, B.D. Understanding and using mediators and moderators. Soc. Indic. Res. 2008, 87, 367. [Google Scholar] [CrossRef]
- Hayes, A.F. Model Templates for PROCESS for SPSS and SAS. Available online: http://afhayes.com/spss-sas-and-mplus-macros-and-code.html (accessed on 9 September 2019).
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; Guilford Publications: New York, NY, USA, 2017. [Google Scholar]
- Zhang, J.; Oldenburg, B.; Turrell, G. Measuring factors that influence the utilisation of preventive care services provided by general practitioners in Australia. BMC Health Serv. Res. 2009, 9, 218. [Google Scholar] [CrossRef] [PubMed]
- Singh Gaur, S.; Xu, Y.; Quazi, A.; Nandi, S. Relational impact of service providers’ interaction behavior in healthcare. Manag. Serv. Qual. Int. J. 2011, 21, 67–87. [Google Scholar] [CrossRef]
- Srivastava, A.; Avan, B.I.; Rajbangshi, P.; Bhattacharyya, S. Determinants of women’s satisfaction with maternal health care: A review of literature from developing countries. BMC Pregnancy Childbirth 2015, 15, 97. [Google Scholar] [CrossRef] [PubMed]
- Asif, M.; Jameel, A.; Hussain, A.; Hwang, J.; Sahito, N. Linking Transformational Leadership with Nurse-Assessed Adverse Patient Outcomes and the Quality of Care: Assessing the Role of Job Satisfaction and Structural Empowerment. Int. J. Environ. Res. Public Health 2019, 16, 2381. [Google Scholar] [CrossRef]
- Williams, B.; Wilkinson, G. Patient satisfaction in mental health care: Evaluating an evaluative method. Br. J. Psychiatry 1995, 166, 559–562. [Google Scholar] [CrossRef]
- Wiggers, J.H.; Donovan, K.O.; Redman, S.; Sanson-Fisher, R.W. Cancer patient satisfaction with care. Cancer 1990, 66, 610–616. [Google Scholar] [CrossRef]
- Jayanti, R.K.; Burns, A.C. The antecedents of preventive health care behavior: An empirical study. J. Acad. Mark. Sci. 1998, 26, 6–15. [Google Scholar] [CrossRef]
- Oladapo, O.T.; Iyaniwura, C.A.; Sule-Odu, A.O. Quality of antenatal services at the primary care level in southwest Nigeria. Afr. J. Reprod. Health 2008, 12, 71–92. [Google Scholar]
- Taenzer, P.; Bultz, B.D.; Carlson, L.E.; Speca, M.; DeGagne, T.; Olson, K.; Doll, R.; Rosberger, Z. Impact of computerized quality of life screening on physician behaviour and patient satisfaction in lung cancer outpatients. Psycho-Oncol. J. Psychol. Soc. Behav. Dimens. Cancer 2000, 9, 203–213. [Google Scholar] [CrossRef]


| Gender | Frequency | Percent | Age | Frequency | Percent | Education | Frequency | Percent |
| Male | 130 | 44.8 | 20–25 | 35 | 12.1 | No education | 70 | 24.1 |
| Female | 160 | 55.2 | 26–29 | 80 | 27.6 | Elementary school | 60 | 20.7 |
| Total | 290 | 100 | 30–39 | 60 | 20.7 | High school | 60 | 20.7 |
| 40–49 | 50 | 17.2 | Bachelor/College | 45 | 15.5 | |||
| 50 above | 65 | 22.4 | Master degree | 55 | 19 | |||
| Total | 290 | 100 | Total | 290 | 100 | |||
| Occupation | Frequency | Percent | Marital Status | Frequency | Percent | Backg-round | Frequency | Percent |
| Govt. servant | 130 | 44.8 | Married | 180 | 62.1 | Rural | 195 | 67.2 |
| House wives | 70 | 24.1 | Single | 45 | 15.5 | Urban | 95 | 32.8 |
| Retired | 30 | 10.3 | Divorced | 5 | 1.7 | Total | 290 | 100 |
| Farmers | 40 | 13.8 | Widow | 60 | 20.7 | |||
| Students | 20 | 6.9 | Total | 290 | 100 | |||
| Total | 290 | 100 |
| Variable | Mean | SD | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|---|---|
| 1. Laboratory and diagnostic care | 3.680 | 0.671 | 0.79 | ||||
| 2. Preventive healthcare | 2.491 | 0.971 | 0.047 | 0.94 | |||
| 3. Prenatal care | 3.324 | 0.851 | 0.202 ** | −0.007 | 0.82 | ||
| 4. Physician’s behavior | 3.991 | 0.601 | 0.268 ** | 0.018 | 0.252 ** | 0.81 | |
| 5. Patient Satisfaction | 3.352 | 0.576 | 0.260 ** | 0.347 ** | 0.438 ** | 0.251 ** | 0.71 |
| Variables | β | T | Significance | 95% Confidence Interval | |
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||
| Constant | 1.130 *** | 4.969 | 0.000 | 0.682 | 1.578 |
| Laboratory and diagnostic care | 0.117 ** | 2.728 | 0.007 | 0.033 | 0.202 |
| Preventive healthcare | 0.202 *** | 7.131 | 0.000 | 0.146 | 0.258 |
| Prenatal care | 0.260 *** | 7.716 | 0.000 | 0.194 | 0.327 |
| Physician’s behavior | 0.107 * | 2.201 | 0.029 | 0.011 | 0.202 |
| Interactional Effect | β | SE | T | Sig. | 95% Bootstrapping Confidence Interval | |
|---|---|---|---|---|---|---|
| LLCI | ULCI | |||||
| Interaction1 (LDC *PB) | 0.226 | 0.086 | 2.617 | 0.009 | 0.056 | 0.397 |
| Interaction2 (PHC *PB) | 0.117 | 0.056 | 2.063 | 0.031 | 0.0054 | 0.229 |
| Interaction3 (PC *PB) | 0.256 | 0.050 | 4.836 | 0.000 | 0.1518 | 0.360 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Manzoor, F.; Wei, L.; Hussain, A.; Asif, M.; Shah, S.I.A. Patient Satisfaction with Health Care Services; An Application of Physician’s Behavior as a Moderator. Int. J. Environ. Res. Public Health 2019, 16, 3318. https://doi.org/10.3390/ijerph16183318
Manzoor F, Wei L, Hussain A, Asif M, Shah SIA. Patient Satisfaction with Health Care Services; An Application of Physician’s Behavior as a Moderator. International Journal of Environmental Research and Public Health. 2019; 16(18):3318. https://doi.org/10.3390/ijerph16183318
Chicago/Turabian StyleManzoor, Faiza, Longbao Wei, Abid Hussain, Muhammad Asif, and Syed Irshad Ali Shah. 2019. "Patient Satisfaction with Health Care Services; An Application of Physician’s Behavior as a Moderator" International Journal of Environmental Research and Public Health 16, no. 18: 3318. https://doi.org/10.3390/ijerph16183318
APA StyleManzoor, F., Wei, L., Hussain, A., Asif, M., & Shah, S. I. A. (2019). Patient Satisfaction with Health Care Services; An Application of Physician’s Behavior as a Moderator. International Journal of Environmental Research and Public Health, 16(18), 3318. https://doi.org/10.3390/ijerph16183318






