A Cross Sectional Study Evaluating Psychosocial Job Stress and Health Risk in Emergency Department Nurses
Abstract
1. Introduction
2. Materials and Methods
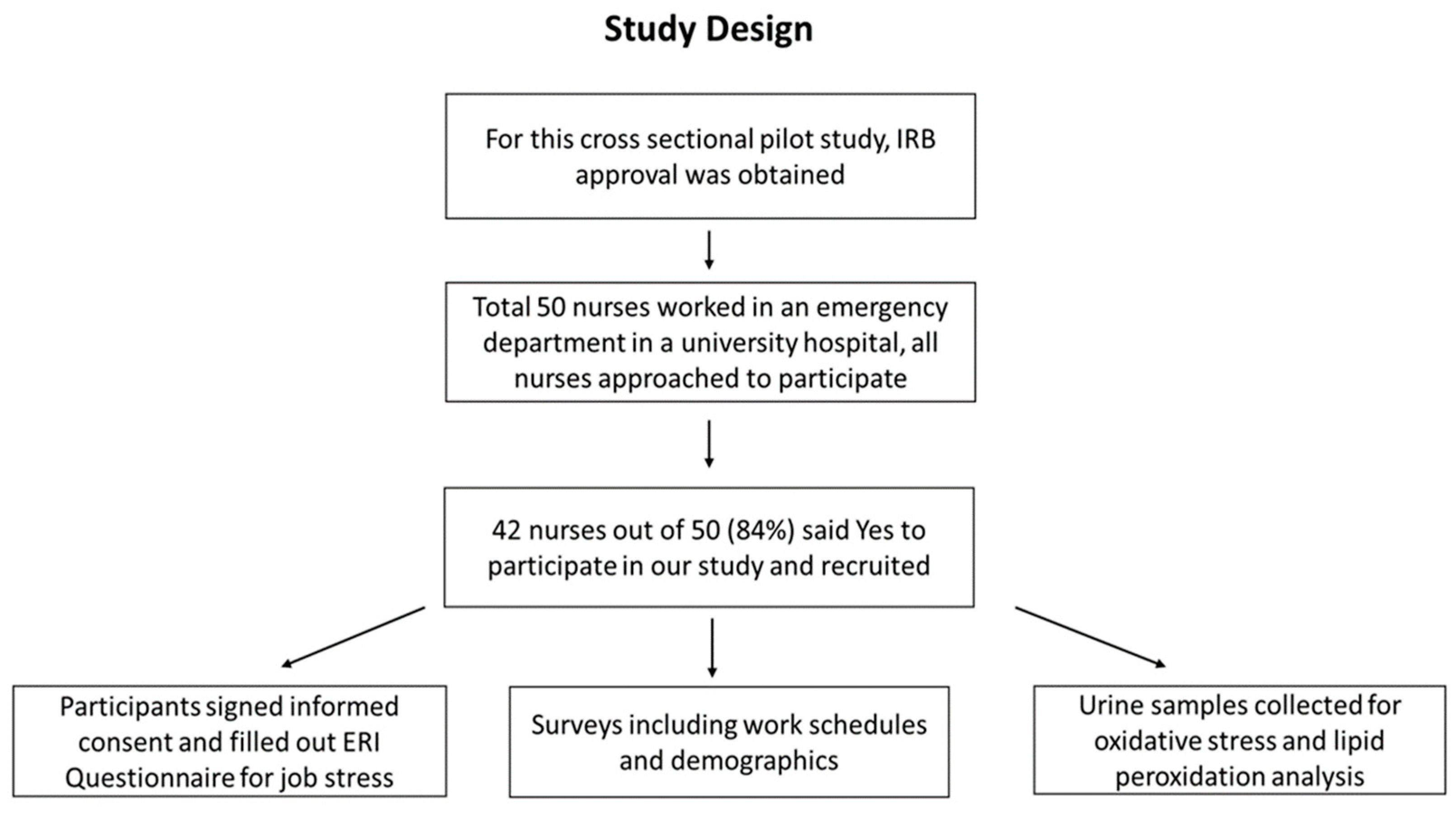
2.1. Study Design
2.2. Evaluation of Job Stress Using the Effort–Reward Imbalance Model
2.3. Evaluation of Oxidative Stress/Lipid Peroxidation from Urine
2.3.1. Urinary Malondialdehyde Assay
2.3.2. Urinary 8-Isoprostane Assay
2.3.3. Total Antioxidant Capacity Assay
2.3.4. Creatinine Assay
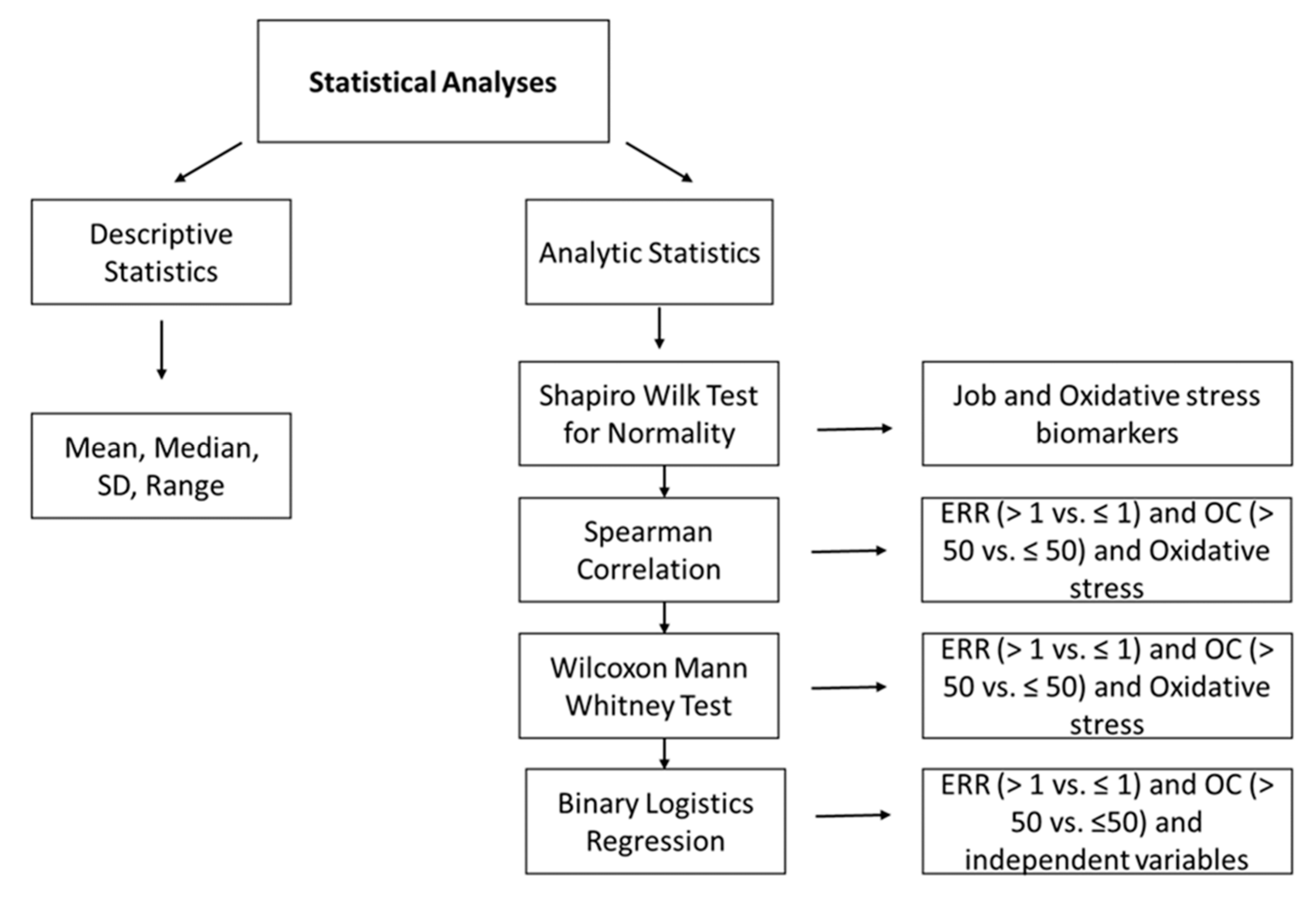
2.4. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Potential Health Risk Indicators Measured in This Study
3.3. Distribution of the Statistical Variables
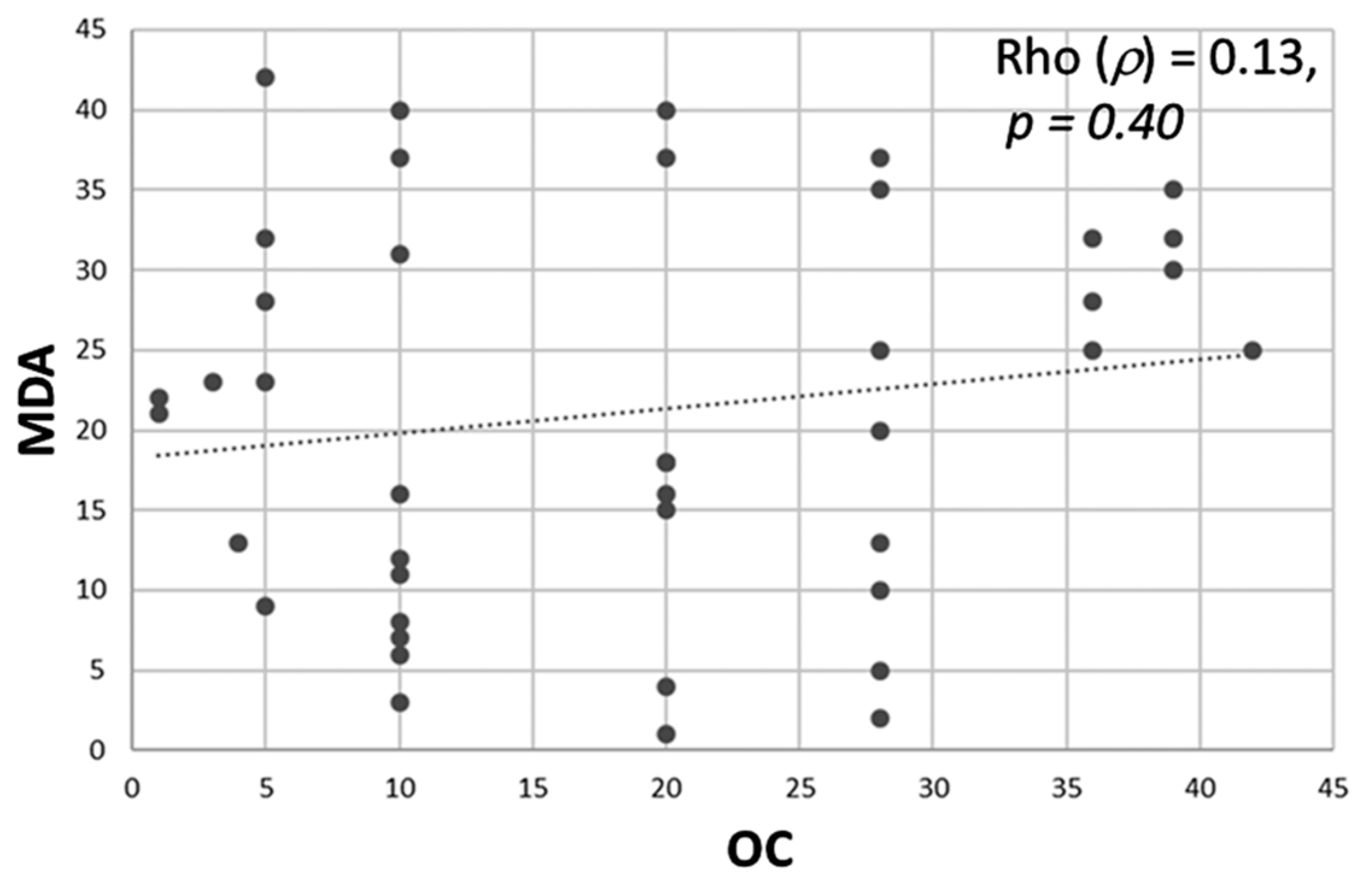
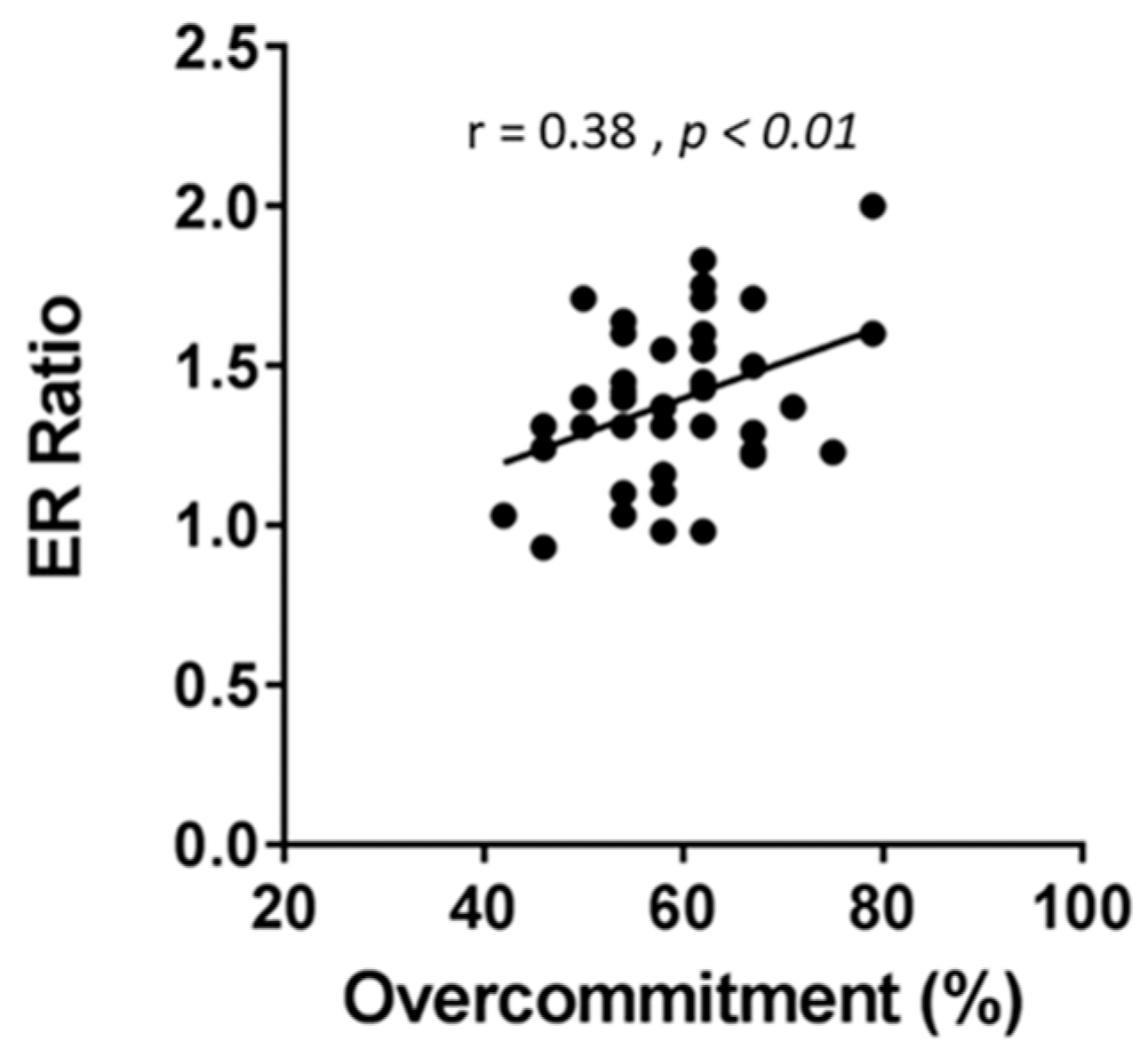
3.4. Association between Job Stress Indicators (ERR and OC) and Oxidative Stress Biomarkers
3.5. Job Stress as a Function of Age, BMI, and Work Conditions
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Siegrist, J. Effort-reward imbalance at work and depression: Current research evidence. Nervenarzt 2013, 84, 33–37. [Google Scholar] [CrossRef] [PubMed]
- Siegrist, J. Effort-reward imbalance at work and cardiovascular diseases. Int. J. Occup. Med. Environ. Health 2010, 23, 279–285. [Google Scholar] [CrossRef] [PubMed]
- Siegrist, J.; Starke, D.; Chandola, T.; Godin, I.; Marmot, M.; Niedhammer, I.; Peter, R. The measurement of effort–reward imbalance at work: European comparisons. Soc. Sci. Med. 2004, 58, 1483–1499. [Google Scholar] [CrossRef]
- Siegrist, J.; Li, J. Associations of Extrinsic and Intrinsic Components of Work Stress with Health: A Systematic Review of Evidence on the Effort-Reward Imbalance Model. Int. J. Environ. Res. Public Health 2016, 13, 432. [Google Scholar] [CrossRef] [PubMed]
- Siegrist, J.; Dragano, N. Psychosocial stress and disease risks in occupational life. Results of international studies on the demand-control and the effort-reward imbalance models. Bundesgesundheitsblatt Gesundh. Gesundh. 2008, 51, 305–312. [Google Scholar] [CrossRef] [PubMed]
- Wagner, B.D.; Accurso, F.J.; Laguna, T.A. The applicability of urinary creatinine as a method of specimen normalization in the cystic fibrosis population. J. Cyst. Fibros. 2010, 9, 212–216. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Wang, J.; Yang, C.; Fan, J. Nurse practitioner job content and stress effects on anxiety and depressive symptoms, and self-perceived health status. J. Nurs. Manag. 2016, 24, 695–704. [Google Scholar] [CrossRef]
- Cheung, T.; Yip, P.S. Lifestyle and Depression among Hong Kong Nurses. Int. J. Environ. Res. Public Health 2016, 13, 135. [Google Scholar] [CrossRef]
- Li, J.; Zhang, M.; Loerbroks, A.; Angerer, P.; Siegrist, J. Work stress and the risk of recurrent coronary heart disease events: A systematic review and meta-analysis. Int. J. Occup. Med. Environ. Health 2015, 28, 8–19. [Google Scholar] [CrossRef]
- Cao, L.; Tian, H.; Zhang, Q.; Zhu, X.; Zhan, Y.; Su, J.; Xu, T.; Zhu, H.; Liu, L. Effect of occupational stress on oxidation/antioxidant capacity in nurses. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi 2014, 32, 100–103. [Google Scholar]
- Lu, J.; Chen, B.; Chen, T.; Guo, S.; Xue, X.; Chen, Q.; Zhao, M.; Xia, L.; Zhu, Z.; Zheng, L.; et al. Comprehensive metabolomics identified lipid peroxidation as a prominent feature in human plasma of patients with coronary heart diseases. Redox Biol. 2017, 12, 899–907. [Google Scholar] [CrossRef] [PubMed]
- Suridjan, I.; Herrmann, N.; Adibfar, A.; Saleem, M.; Andreazza, A.; Oh, P.I.; Lanctot, K.L. Lipid Peroxidation Markers in Coronary Artery Disease Patients with Possible Vascular Mild Cognitive Impairment. J. Alzheimers Dis. 2017, 58, 885–896. [Google Scholar] [CrossRef] [PubMed]
- Gönenç, A.; Özkan, Y.; Torun, M.; Şimşek, B. Plasma malondialdehyde (MDA) levels in breast and lung cancer patients. J. Clin. Pharm. Ther. 2001, 26, 141–144. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.A.; Baseer, A. Increased malondialdehyde levels in coronary heart disease. J. Pak. Med. Assoc. 2000, 50, 261–264. [Google Scholar] [PubMed]
- Davies, S.S.; Roberts, L.J. F2-isoprostanes as an indicator and risk factor for coronary heart disease. Free Radic. Biol. Med. 2011, 50, 559–566. [Google Scholar] [CrossRef]
- Milne, G.L.; Dai, Q.; Roberts, L.J. The isoprostanes—25 years later. Biochim. Biophys. Acta 2015, 1851, 433–445. [Google Scholar] [CrossRef]
- Msaouel, P.; Keramaris, N.C.; Apostolopoulos, A.P.; Syrmos, N.; Kappos, T.; Tasoulis, A.; Tripodaki, E.-S.; Kagiampaki, E.; Lekkas, I.; Siegrist, J. The Effort-reward Imbalance Questionnaire in Greek: Translation, Validation and Psychometric Properties in Health Professionals. J. Occup. Health 2012, 54, 119–130. [Google Scholar] [CrossRef] [PubMed]
- de Araujo, T.M.; Siegrist, J.; Moreno, A.B.; de Jesus Mendes da Fonseca, M.; Barreto, S.M.; Chor, D.; Griep, R.H. Effort-Reward Imbalance, Over-Commitment and Depressive Episodes at Work: Evidence from the ELSA-Brasil Cohort Study. Int. J. Environ. Res. Public Health 2019, 16, 3025. [Google Scholar] [CrossRef]
- Li, J.; Herr, R.M.; Allen, J.; Stephens, C.; Alpass, F. Validating the short measure of the Effort-Reward Imbalance Questionnaire in older workers in the context of New Zealand. J. Occup. Health 2017, 59, 495–505. [Google Scholar] [CrossRef]
- Padilla Fortunatti, C.; Palmeiro-Silva, Y.K. Effort-Reward Imbalance and Burnout Among ICU Nursing Staff: A Cross-Sectional Study. Nurs. Res. 2017, 66, 410–416. [Google Scholar] [CrossRef]
- de Cassia Fogaca, M.; de Carvalho, W.B.; de Albuquerque Citero, V.; Nogueira-Martins, L.A. Preliminary study about occupational stress of physicians and nurses in pediatric and neonatal intensive care units: The balance between effort and reward. Rev. Lat. Am. Enferm. 2010, 18, 67–72. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Finger, V.; Baumstarck, K.; Boufercha, R.; Lehucher-Michel, M.P.; Loundou, A.; Auquier, P.; Sari-Minodier, I. Psychosocial risks assessment at hospital: Development of a French questionnaire. Med. Lav. 2016, 107, 378–391. [Google Scholar]
- Wege, N.; Li, J.; Siegrist, J. Are there gender differences in associations of effort-reward imbalance at work with self-reported doctor-diagnosed depression? Prospective evidence from the German Socio-Economic Panel. Int. Arch. Occup. Environ. Health 2018, 91, 435–443. [Google Scholar] [CrossRef] [PubMed]
- Fujishiro, K.; Lawson, C.C.; Hibert, E.L.; Chavarro, J.E.; Rich-Edwards, J.W. Job strain and changes in the body mass index among working women: A prospective study. Int. J. Obes. 2015, 39, 1395–1400. [Google Scholar] [CrossRef]
- Nyberg, S.T.; Heikkila, K.; Fransson, E.I.; Alfredsson, L.; De Bacquer, D.; Bjorner, J.B.; Bonenfant, S.; Borritz, M.; Burr, H.; Casini, A.; et al. Job strain in relation to body mass index: Pooled analysis of 160,000 adults from 13 cohort studies. J. Intern. Med. 2012, 272, 65–73. [Google Scholar] [CrossRef]
- Gotz, S.; Hoven, H.; Muller, A.; Dragano, N.; Wahrendorf, M. Age differences in the association between stressful work and sickness absence among full-time employed workers: Evidence from the German socio-economic panel. Int. Arch. Occup. Environ. Health 2018, 91, 479–496. [Google Scholar] [CrossRef]
- Balakrishnamurthy, C.; Shankar, S. Impact of age and level of experience on occupational stress experienced by non-gazetted officers of the central reserve police force. Ind. Psychiatry J. 2009, 18, 81–83. [Google Scholar] [CrossRef] [PubMed]
- Han, K.; Kim, Y.-H.; Lee, H.Y.; Cho, H.; Jung, Y.S. Changes in health behaviours and health status of novice nurses during the first 2 years of work. J. Adv. Nurs. 2019, 75, 1648–1656. [Google Scholar] [CrossRef] [PubMed]
- Hatch, D.J.; Freude, G.; Martus, P.; Rose, U.; Muller, G.; Potter, G.G. Age, burnout and physical and psychological work ability among nurses. Occup. Med. 2018, 68, 246–254. [Google Scholar] [CrossRef]
- Dai, Q.; Zhu, X. F2-isoprostanes and Metabolite, and Breast Cancer Risk. Am. Chin. J. Med. Sci. 2009, 2, 106–108. [Google Scholar] [CrossRef]
- Gaweł, S.; Wardas, M.; Niedworok, E.; Wardas, P. Malondialdehyde (MDA) as a lipid peroxidation marker. Wiad. Lek. 2004, 57, 453–455. [Google Scholar]
- Il’Yasova, D.; Scarbrough, P.; Spasojevic, I. Urinary Biomarkers of Oxidative Status. Clin. Chim. Acta 2012, 413, 1446–1453. [Google Scholar] [CrossRef]
- Spirlandeli, A.L.; Deminice, R.; Jordao, A.A. Plasma malondialdehyde as biomarker of lipid peroxidation: Effects of acute exercise. Int. J. Sports Med. 2014, 35, 14–18. [Google Scholar] [CrossRef]
- Salem, E.A.; Ebrahem, S.M. Psychosocial work environment and oxidative stress among nurses’. J. Occup. Health 2018, 60, 182–191. [Google Scholar] [CrossRef]
- Buyukhatipoglu, H.; Kirhan, I.; Vural, M.; Taskin, A.; Sezen, Y.; Dag, O.F.; Turan, M.N.; Aksoy, N. Oxidative stress increased in healthcare workers working 24-h on-call shifts. Am. J. Med. Sci. 2010, 340, 462–467. [Google Scholar] [CrossRef] [PubMed]
- Ulas, T.; Buyukhatipoglu, H.; Kirhan, I.; Dal, M.S.; Eren, M.A.; Hazar, A.; Demir, M.E.; Aydogan, T.; Karababa, F.; Uyanikoglu, A.; et al. The effect of day and night shifts on oxidative stress and anxiety symptoms of the nurses. Eur. Rev. Med Pharmacol. Sci. 2012, 16, 594-9. [Google Scholar] [PubMed]
- Gromadzinska, J.; Peplonska, B.; Sobala, W.; Reszka, E.; Wasowicz, W.; Bukowska, A.; Lie, J.A. Relationship between intensity of night shift work and antioxidant status in blood of nurses. Int. Arch. Occup. Environ. Health 2013, 86, 923–930. [Google Scholar] [CrossRef] [PubMed]
- Spiers, J.G.; Chen, H.J.; Sernia, C.; Lavidis, N.A. Activation of the hypothalamic-pituitary-adrenal stress axis induces cellular oxidative stress. Front. Neurosci. 2014, 8, 456. [Google Scholar] [CrossRef]
- Fadaee, S.B.; Beetham, K.S.; Howden, E.J.; Stanton, T.; Isbel, N.M.; Coombes, J.S. Oxidative stress is associated with decreased heart rate variability in patients with chronic kidney disease. Redox Rep. 2017, 22, 197–204. [Google Scholar] [CrossRef]
- Caruso, C.C. Negative impacts of shiftwork and long work hours. Rehabil. Nurs. 2014, 39, 16–25. [Google Scholar] [CrossRef]
- Puttonen, S.; Harma, M.; Hublin, C. Shift work and cardiovascular disease—Pathways from circadian stress to morbidity. Scand. J. Work Environ. Health 2010, 36, 96–108. [Google Scholar] [CrossRef] [PubMed]
- Drager, L.F.; McEvoy, R.D.; Barbe, F.; Lorenzi-Filho, G.; Redline, S.; Initiative, I. Sleep Apnea and Cardiovascular Disease: Lessons from Recent Trials and Need for Team Science. Circulation 2017, 136, 1840–1850. [Google Scholar] [CrossRef] [PubMed]
- Cocchiara, R.A.; Peruzzo, M.; Mannocci, A.; Ottolenghi, L.; Villari, P.; Polimeni, A.; Guerra, F.; La Torre, G. The Use of Yoga to Manage Stress and Burnout in Healthcare Workers: A Systematic Review. J. Clin. Med. 2019, 8, 284. [Google Scholar] [CrossRef] [PubMed]
- Morrison Wylde, C.; Mahrer, N.E.; Meyer, R.M.L.; Gold, J.I. Mindfulness for Novice Pediatric Nurses: Smartphone Application Versus Traditional Intervention. J. Pediatr. Nurs. 2017, 36, 205–212. [Google Scholar] [CrossRef] [PubMed]
- Fallatah, F.; Laschinger, H.K.; Read, E.A. The effects of authentic leadership, organizational identification, and occupational coping self-efficacy on new graduate nurses’ job turnover intentions in Canada. Nurs. Outlook 2017, 65, 172–183. [Google Scholar] [CrossRef] [PubMed]


| Characteristics | Total (−n = 42) −n (%) or Mean (SD) * | Median (Range) |
|---|---|---|
| Age (years) * | 33.04 (9.79) | 30 (22–60) |
| Sex | ||
| Female | 29 (69) | |
| Male | 13 (31) | |
| BMI * | 28.2 (6.36) | 27.3 (19.1–44.6) |
| Marital status | ||
| Married | 21 (50) | |
| Single | 21 (50) | |
| Years of experience | ||
| ≤10 | 33 (79) | |
| >10 | 9 (21) | |
| Shift work | ||
| Day shift | 16 (38) | |
| Rotating shift | 26 (62) | |
| Weekend work | ||
| Yes | 259 (71.2) | |
| No | 9 (2.5) | |
| Work hours/week | ||
| ≤40 | 21 (50) | |
| >40 | 21 (50) |
| Characteristics | Total (−n = 42) −n (%) or Mean (SD) * | Median (Range) |
|---|---|---|
| ERR | ||
| Low ≤ 1 | 3 (7) | |
| High > 1 | 39 (93) | |
| OC | ||
| Low ≤ 50 | 7 (17) | |
| High > 50 | 35 (83) | |
| MDA * (µm) | 19.34 (0.249) | 19.35 (19–20) |
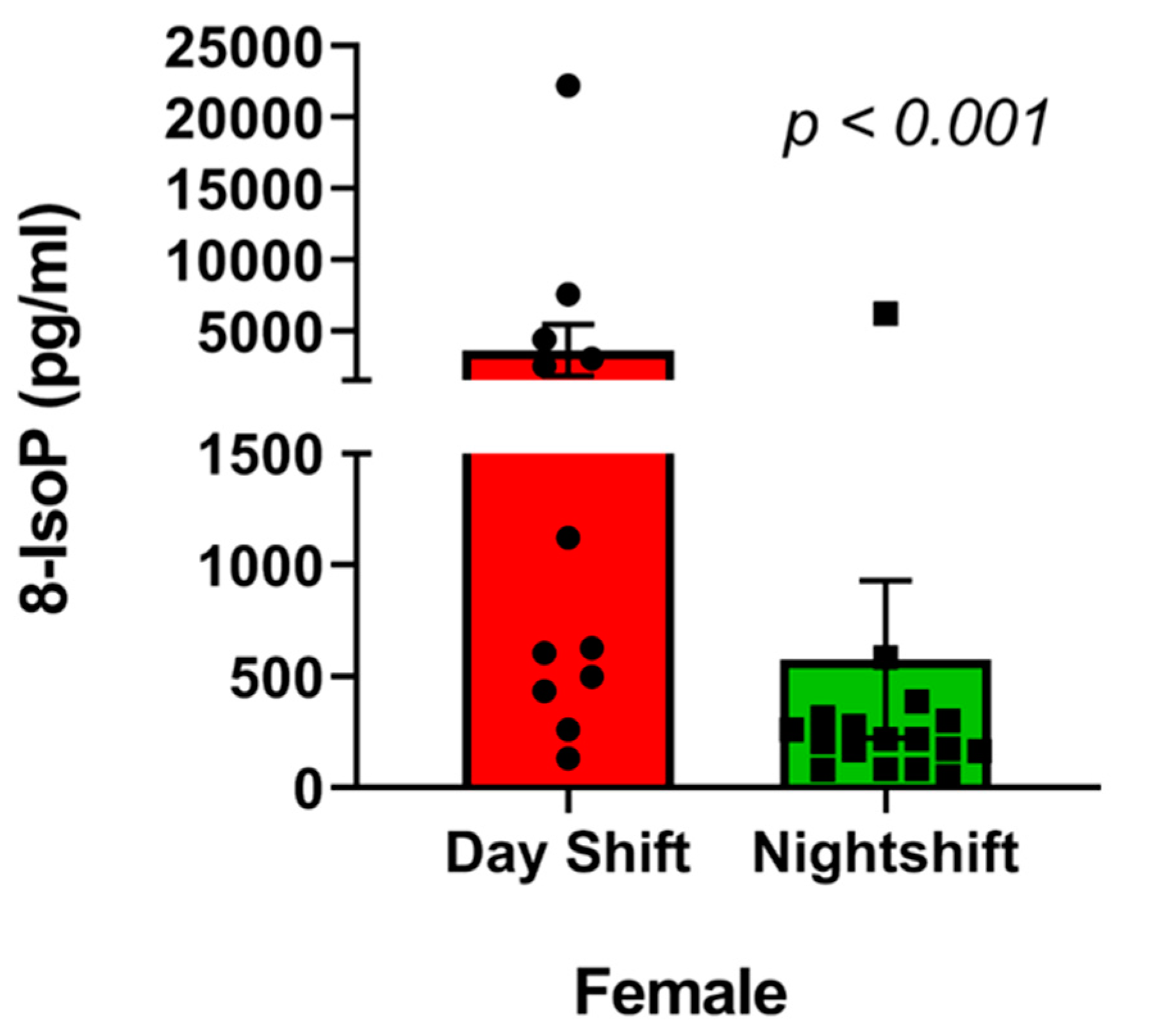
| 8-IsoP * (pg/mL) | 1452.9 (3682.7) | 349.68 (51–22248) |
| Antioxidant * (µm) | 480.2 (0.0007) | 480.4 (479–481) |
| Variables | Test Statistic | p Value |
|---|---|---|
| ERR | 0.98 | 0.78 (Normal) |
| OC | 0.95 | 0.14 (Normal) |
| MDA | 0.45 | <0.0001 |
| 8-IsoP | 0.38 | <0.0001 |
| Antioxidant | 0.92 | <0.01 |
| Variables | ERR < 1 −n (3) Mean, Median, SD | ERR > 1 −n (39) Mean, Median, SD | Test Statistic | p Value |
|---|---|---|---|---|
| MDA | 19.42, 19.27, 0.27 | 19.34, 19.25, 0.25 | 78.5 | 0.50 |
| 8-IsoP | 183.71, 83.62, 176 | 1550.58, 352.024, 3807 | 32 | 0.11 |
| Antioxidant | 480.1, 480.49, 0.75 | 480.21, 480.44, 0.73 | 55 | 0.66 |
| Variables | OC < 50 | OC > 50 | ||
|---|---|---|---|---|
| −n (7) Mean, Median, SD | −n (35) Mean, Median, SD | Test Statistic | p Value | |
| MDA | 19.25, 19.25, 0.002 | 19.36, 19.26, 0.26 | 89 | 0.03 * |
| 8-IsoP | 1113.13, 376.82, 1393 | 1520.91, 316.89, 3998 | 168 | 0.56 |
| Antioxidant | 480.36, 480.65, 0.82 | 480.17, 480.41, 0.71 | 177 | 0.38 |
| Characteristics | OR (95% CI) | p Value |
|---|---|---|
| Age (years) | ||
| 20–30 | 1.00 (Reference) | |
| >30–40 | 1.084 (0.051–23.208) | 0.70 |
| >40 | 0.423 (0.005–33.97) | 0.63 |
| Sex | ||
| Female | 0.640 (0.051–7.95) | |
| Male | 1.00 (Reference) | 0.72 |
| Years of experience | ||
| ≤10 | 1.976 (0.05–69.20) | |
| >10 | 1.00 (Reference) | 0.70 |
| Shift work | ||
| Day shift | 1.00 (Reference) | |
| Rotating shift | 0.309 (0.031–3.09) | 0.31 |
| Weekend work | ||
| Yes | 2.913 (0.033–254.75) | |
| No | 1.00 (Reference) | 0.63 |
| Work hours/week | ||
| ≤40 | 1.00 (Reference) | |
| >40 | 0.818 (113-5.922) | 0.84 |
| BMI | ||
| Obese (≥30) | 2.653 (0.206–34.15) | 0.56 |
| Overweight (25.0–29.9) | 1.731 (0.208–14.39) | 0.95 |
| Normal (<25) | 1.00 (Reference) |
| Characteristics | OR (95% CI) | p Value |
|---|---|---|
| Age (years) | ||
| 20–30 | 1.00 (Reference) | |
| 31–40 | 1.903 (0.111–32.70) | 0.95 |
| >40 | 4.143 (0.107–160.47) | 0.48 |
| Sex | ||
| Female | 2.967 (0.397–22.18) | 0.28 |
| Male | 1.00 (Reference) | |
| Years of experience | ||
| <10 | 1.00 (Reference) | |
| >10 | 0.177 (0.009–3.57) | 0.26 |
| Shift work | ||
| Day shift | 1.00 (Reference) | |
| Rotating shift | 2.683 (0.45–15.94) | 0.28 |
| Weekend work | ||
| Yes | 1.502 (0.020–115.13) | 0.85 |
| No | 1.00 (Reference) | |
| Work hours/week | ||
| ≤40 | 1.00 (Reference) | 0.34 |
| >40 | 2.429 (0.37–15.56) | |
| BMI | ||
| Obese (≥30) | 2.006 (0.226–17.77) | 0.68 |
| Overweight (25.0–29.9) | 1.684 (0.223–12.727) | 0.86 |
| Normal (<25) | 1.00 (Reference) |
| Oxidative Stress Biomarkers | vs. ERR | |
|---|---|---|
| Rho (ρ) | p Value | |
| MDA | 0.087 | 0.58 |
| 8-IsoP | −0.11 | 0.46 |
| Antioxidant | 0.106 | 0.50 |
| Oxidative Stress Biomarkers | vs. OC | |
|---|---|---|
| Rho (ρ) | p Value | |
| MDA | 0.13 | 0.40 |
| 8-IsoP | −0.19 | 0.20 |
| Antioxidant | 0.10 | 0.49 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bardhan, R.; Heaton, K.; Davis, M.; Chen, P.; Dickinson, D.A.; Lungu, C.T. A Cross Sectional Study Evaluating Psychosocial Job Stress and Health Risk in Emergency Department Nurses. Int. J. Environ. Res. Public Health 2019, 16, 3243. https://doi.org/10.3390/ijerph16183243
Bardhan R, Heaton K, Davis M, Chen P, Dickinson DA, Lungu CT. A Cross Sectional Study Evaluating Psychosocial Job Stress and Health Risk in Emergency Department Nurses. International Journal of Environmental Research and Public Health. 2019; 16(18):3243. https://doi.org/10.3390/ijerph16183243
Chicago/Turabian StyleBardhan, Rupkatha, Karen Heaton, Melissa Davis, Peter Chen, Dale A. Dickinson, and Claudiu T. Lungu. 2019. "A Cross Sectional Study Evaluating Psychosocial Job Stress and Health Risk in Emergency Department Nurses" International Journal of Environmental Research and Public Health 16, no. 18: 3243. https://doi.org/10.3390/ijerph16183243
APA StyleBardhan, R., Heaton, K., Davis, M., Chen, P., Dickinson, D. A., & Lungu, C. T. (2019). A Cross Sectional Study Evaluating Psychosocial Job Stress and Health Risk in Emergency Department Nurses. International Journal of Environmental Research and Public Health, 16(18), 3243. https://doi.org/10.3390/ijerph16183243






