Care-Seeking Dynamics among Patients with Diabetes Mellitus and Hypertension in Selected Rural Settings in Kenya
Abstract
1. Introduction
2. Methods
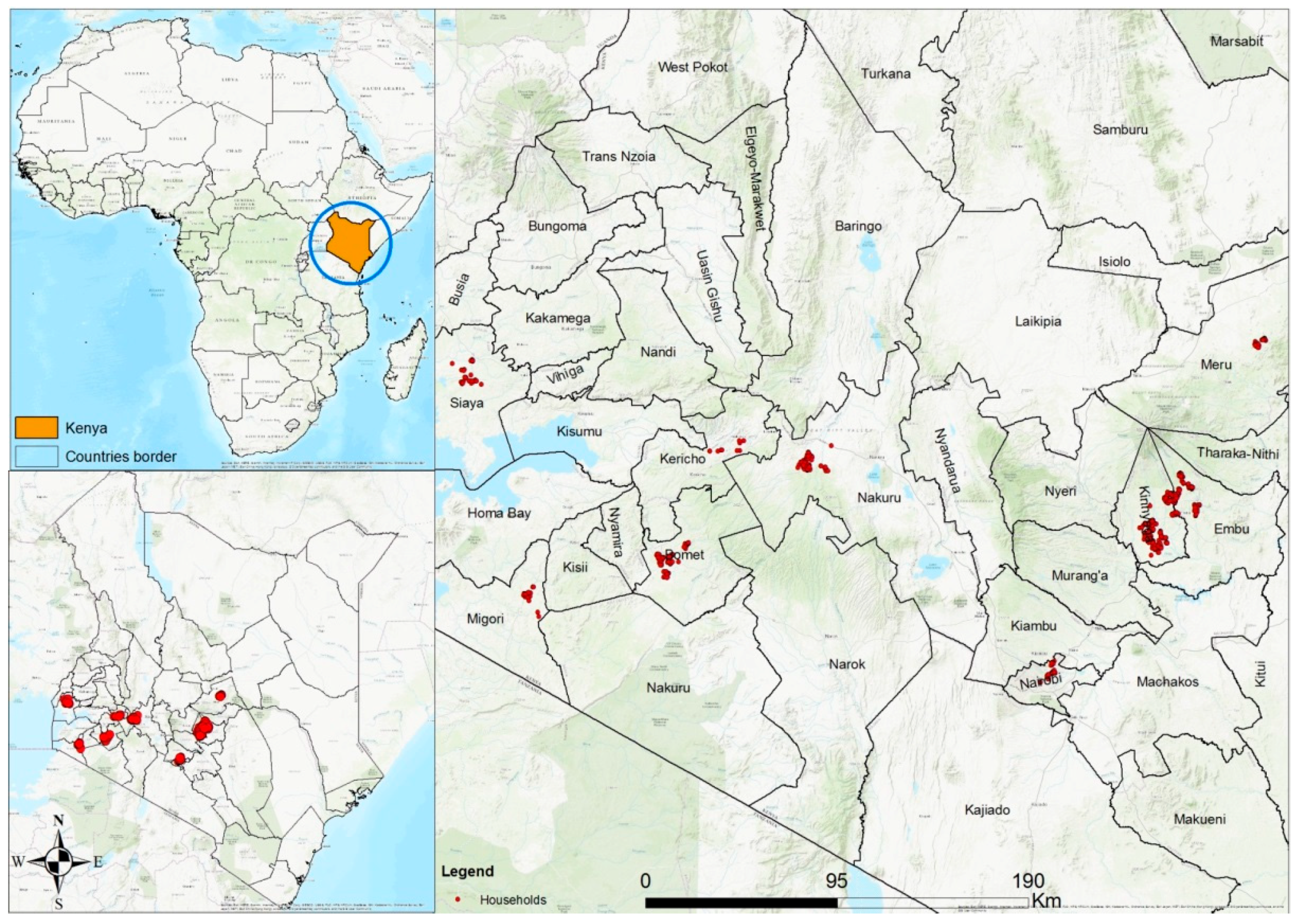
2.1. Study Design and Setting
2.2. Study Population and Sampling
2.3. Data Collection and Measurements
2.4. Statistical Analysis
2.5. Ethical Approval
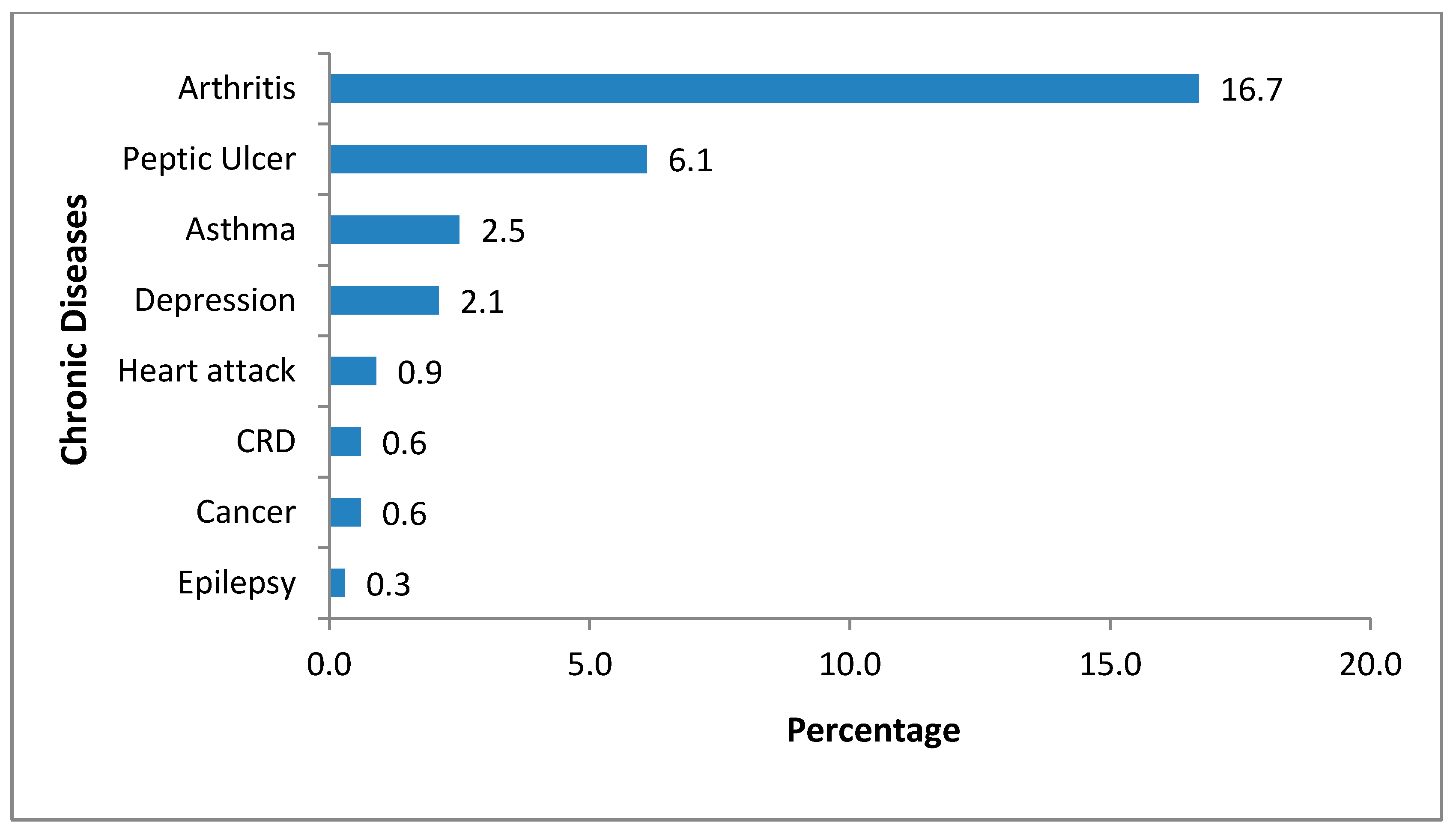
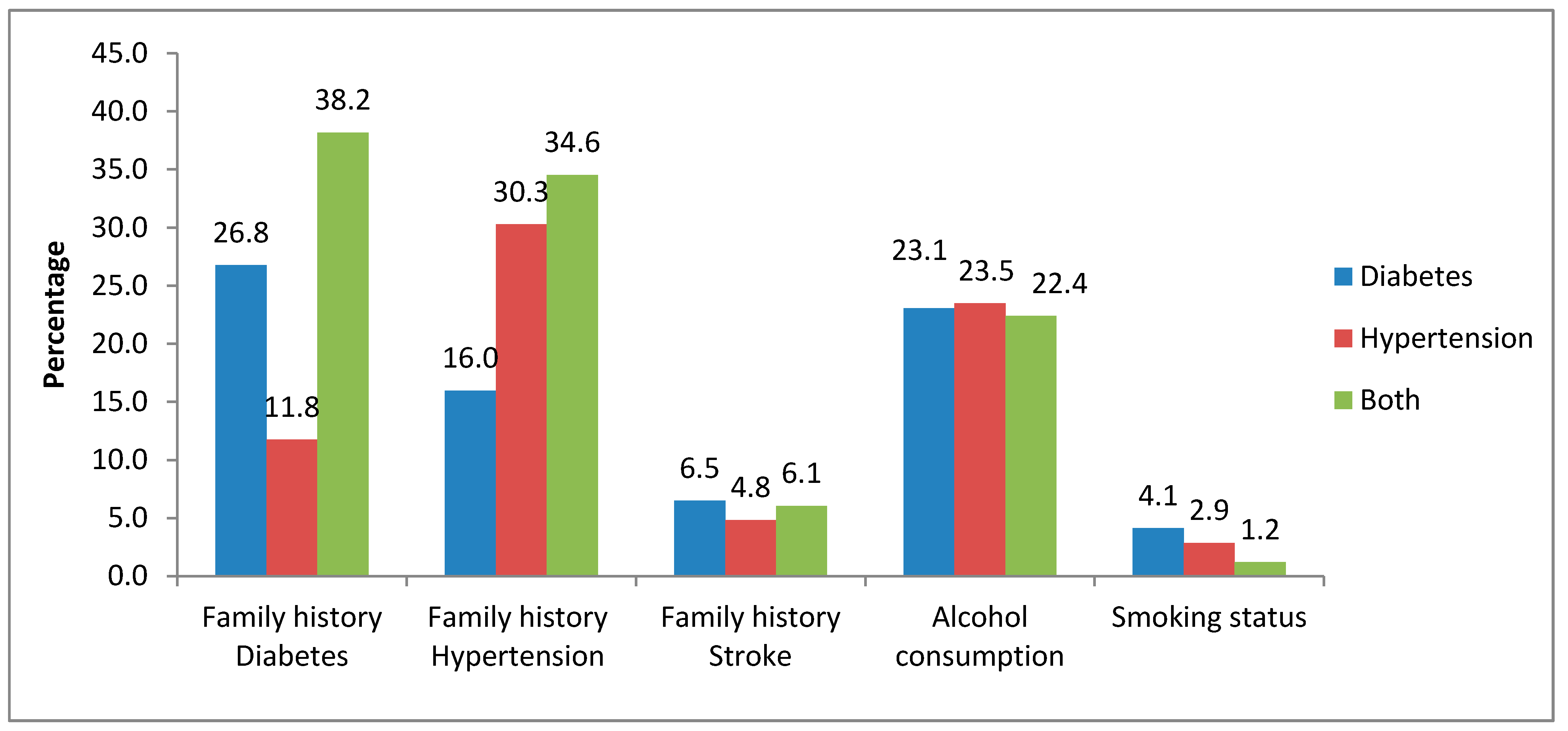
3. Results
3.1. Chronic Respiratory Disease (CRD)
3.2. More than 100% as Some Respondents Offered More Than One Reason
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Onyango, M.J.; Kombe, I.; Nyamongo, D.S.; Mwangi, M. A study to determine the prevalence and factors associated with hypertension among employees working at a call centre Nairobi Kenya. Pan Afr. Med. J. 2017, 27, 178. [Google Scholar] [CrossRef] [PubMed]
- Benziger, C.P.; Roth, G.A.; Moran, A.E. The global burden of disease study and the preventable burden of NCD. Glob. Heart 2016, 11, 393–397. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Health Estimates 2016: Deaths by Cause, Age, Sex, by Country and by Region, 2000–2016; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Olowe, O.A.; Ross, A.J. Knowledge, adherence and control among patients with hypertension attending a peri-urban primary health care clinic, KwaZulu-Natal. Afr. J. Prim. Health Care Fam. Med. 2017, 9, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Pradeepa, R. The rising burden of diabetes and hypertension in southeast asian and african regions: Need for effective strategies for prevention and control in primary health care settings. Int. J. Hypertens. 2013, 2013, 14. [Google Scholar]
- International Diabetes Federation. IDF Diabetes Atlas, 7th ed.; International Diabetes Federation: Brussels, Belgium, 2015. [Google Scholar]
- Matheka, D.M.; Nderitu, J.; Vedanthan, R.; Demaio, A.R.; Murgor, M.; Kajana, K.; Loyal, P.; Alkizim, F.O.; Kishore, S.P. Young professionals for health development: The Kenyan experience in combating non-communicable diseases. Glob. Health Action 2013, 6, 22461. [Google Scholar] [CrossRef][Green Version]
- Kenya National Bureau of Statistics. Kenya Stepwise Survey for Non-Communicable Diseases Risk Factors; 2015 Report; Kenya National Bureau of Statistics: Nairobi, Kenya, 2015.
- Christensen, D.L.; Friis, H.; Mwaniki, D.; Kilonzo, B.; Tetens, I.; Boit, M.; Omondi, B.; Kaduka, L.; Borch-Johnsen, K. Prevalence of glucose intolerance and associated risk factors in rural and urban populations of different ethnic groups in Kenya. Diabetes Res. Clin. Pr. 2009, 84, 303–310. [Google Scholar] [CrossRef] [PubMed]
- Joshi, M.D.; Ayah, R.; Njau, E.K.; Wanjiru, R.; Kayima, J.K.; Njeru, E.K.; Mutai, K.K. Prevalence of hypertension and associated cardiovascular risk factors in an urban slum in Nairobi, Kenya: A population-based survey. BMC Public Health 2014, 14, 1177. [Google Scholar] [CrossRef]
- Hendriks, M.E.; Wit, F.W.; Roos, M.T.; Brewster, L.M.; Akande, T.M.; De Beer, I.H.; Mfinanga, S.G.; Kahwa, A.M.; Gatongi, P.; Van Rooy, G. Hypertension in sub-Saharan Africa: Cross-sectional surveys in four rural and urban communities. PloS ONE 2012, 7, 32638. [Google Scholar] [CrossRef]
- Pastakia, S.D.; Ali, S.M.; Kamano, J.H.; Akwanalo, C.O.; Ndege, S.K.; Buckwalter, V.L.; Vedanthan, R.; Bloomfield, G.S. Screening for diabetes and hypertension in a rural low income setting in western Kenya utilizing home-based and community-based strategies. Glob. Health 2013, 9, 21. [Google Scholar] [CrossRef][Green Version]
- Kengne, A.P.; Mayosi, B.M. Readiness of the primary care system for non-communicable diseases in sub-Saharan Africa. Lancet Glob. Health 2014, 2, 247–248. [Google Scholar] [CrossRef]
- Olukoya, O. The war against non-communicable disease: How ready is Nigeria? Ann. Ib. Postgrad. Med. 2017, 15, 1–2. [Google Scholar]
- Crampin, A.C.; Kayuni, N.; Amberbir, A.; Musicha, C.; Koole, O.; Tafatatha, T.; Branson, K.; Saul, J.; Mwaiyeghele, E.; Nkhwazi, L. Hypertension and diabetes in Africa: Design and implementation of a large population-based study of burden and risk factors in rural and urban Malawi. Emerg. Themes Epidemiol. 2016, 13, 3. [Google Scholar] [CrossRef] [PubMed]
- Bigdeli, M.J.B.; Men, C.R.; Nilsen, K.; Van Damme, W.; Dujardin, B. Access to Treatment for Diabetes and Hypertension in Rural Cambodia: Performance of Existing Social Health Protection Schemes. PloS ONE 2016, 11, 0146147. [Google Scholar] [CrossRef] [PubMed]
- Samb, B.; Desai, N.; Nishtar, S.; Mendis, S.; Bekedam, H.; Wright, A.; Hsu, J.; Martiniuk, A.; Celletti, F.; Patel, K. Prevention and management of chronic disease: A litmus test for health-systems strengthening in low-income and middle-income countries. Lancet 2010, 376, 1785–1797. [Google Scholar] [CrossRef]
- JO, F.; Olowokere, A.; Ayamolowo, S.; Faronbi, G.; Adebiyi, M. Health Seeking Behaviour and Perception of Quality of Care among Patients with Chronic Diseases in a Nigerian Teaching Hospital. Joj Nurse Health Care 2017, 5, 6. [Google Scholar]
- Wang, Q.; Brenner, S.; Leppert, G.; Banda, T.H.; Kalmus, O.; De Allegri, M. Health seeking behaviour and the related household out-of-pocket expenditure for chronic non-communicable diseases in rural Malawi. Health Policy Plan. 2014, 30, 242–252. [Google Scholar] [CrossRef] [PubMed]
- Beaglehole, R.; Epping-Jordan, J.; Patel, V.; Chopra, M.; Ebrahim, S.; Kidd, M.; Haines, A. Improving the prevention and management of chronic disease in low-income and middle-income countries: A priority for primary health care. Lancet 2008, 372, 940–949. [Google Scholar] [CrossRef]
- Jaspers, L.; Colpani, V.; Chaker, L.; van der Lee, S.J.; Muka, T.; Imo, D.; Mendis, S.; Chowdhury, R.; Bramer, W.M.; Falla, A. The global impact of non-communicable diseases on households and impoverishment: A systematic review. Eur. J. Epidemiol. 2015, 30, 163–188. [Google Scholar] [CrossRef] [PubMed]
- Epping-Jordan, J.; Pruitt, S.; Bengoa, R.; Wagner, E.H. Improving the quality of health care for chronic conditions. BMJ Qual. Saf. 2004, 13, 299–305. [Google Scholar] [CrossRef]
- Higuchi, M. Lifestyle Diseases: Access to Chronic Disease Care in Low-and Middle-Income Countries. Un Chron. 2010, 47, 2. [Google Scholar]
- O’Hara, E.G.; Nuche-Berenguer, B.; Kirui, N.K.; Cheng, S.Y.; Chege, P.M.; Buckwalter, V.; Laktabai, J.; Pastakia, S.D. Diabetes in rural Africa: What can Kenya show us? Lancet Diabetes Endocrinol. 2016, 4, 807–809. [Google Scholar] [CrossRef]
- Bovet, P.; Gervasoni, J.-P.; Mkamba, M.; Balampama, M.; Lengeler, C.; Paccaud, F. Low utilization of health care services following screening for hypertension in Dar es Salaam (Tanzania): A prospective population-based study. BMC Public Health 2008, 8, 407. [Google Scholar] [CrossRef] [PubMed]
- Bigdeli, M.; Peters, D.H.; Wagner, A.K. Organization WHO: Medicines in Health Systems: Advancing Access, Affordability and Appropriate Use; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Hartung, C.; Lerer, A.; Anokwa, Y.; Tseng, C.; Brunette, W.; Borriello, G. Open Data Kit: Tools to Build Information Services for Developing Regions. In Proceedings of the 4th ACM/IEEE International Conference on Information and Communication Technologies and Development (ACM 2010), London, UK, 13–16 December 2010; p. 18. [Google Scholar]
- National Health Insurance Fund. Available online: http://www.nhif.or.ke/healthinsurance/Objectives (accessed on 5 June 2019).
- Syed, N.; Rockers, P.C.; Vian, T.; Onyango, M.; Laing, R.O.; Wirtz, V.J. Access to Antihypertensive Medicines at the Household Level. A Study From 8 Counties of Kenya. Glob. Heart 2018, 13, 247–253. [Google Scholar] [CrossRef] [PubMed]
- Wirtz, V.J.; Turpin, K.; Laing, R.O.; Mukiira, C.K.; Rockers, P.C. Access to medicines for asthma, diabetes and hypertension in eight counties of Kenya. Trop. Med. Int. Health 2018, 23, 879–885. [Google Scholar] [CrossRef] [PubMed]
- Mutua, E.M.; Gitonga, M.M.; Mbuthia, B.; Muiruri, N.; Cheptum, J.J.; Maingi, T. Level of blood pressure control among hypertensive patients on follow-up in a Regional Referral Hospital in Central Kenya. Pan Afr. Med J. 2014, 18. [Google Scholar] [CrossRef] [PubMed]
- Yunus, S.Z.S.A.; Binti Musa, N.S.E.; Sapian, R.A.; Azahar, A.; Binti Zainuddin, N.A. Anti-diabetic drugs utilization pattern and its cost in managing Type 2 Diabetes patients in hospitals in Selangor, Malaysia. Inf. Med. Unlocked 2018, 13, 21–25. [Google Scholar] [CrossRef]
- Makinga, P.; Beke, A. A cross-sectional survey on the lifestyle and healthseeking behaviour of Basotho patients with diabetes. South Afr. Fam. Pr. 2013, 55, 190–195. [Google Scholar]
- Bersusa, A.A.S.; Pascalicchio, Á.E.; Pessoto, U.C.; Escuder, M.M.L. Access of hypertension and/or diabetes patients to healthcare services in Baixada Santista. Rev. Bras. De Epidemiol. 2010, 13, 513–522. [Google Scholar] [CrossRef]
- Feng, D.; Serrano, R.; Ye, T.; Tang, S.; Duan, L.; Xu, Y.; Yang, J.; Liang, Y.; Chen, S.; Feng, Z. What contributes to the regularity of patients with hypertension or diabetes seeking health services? A pilot follow-up, observational study in two sites in Hubei province, China. Int. J. Env. Res. Public Health 2016, 13, 1268. [Google Scholar] [CrossRef]
- Inche Zainal Abidin, S.; Sutan, R.; Shamsuddin, K. Prevalence and determinants of appropriate health seeking behaviour among known diabetics: Results from a community-based survey. Adv. Epidemiol. 2014, 2014, 7. [Google Scholar] [CrossRef]
- Nguma, L.K. Health Seeking and Health Related Behaviour for Type 2 Diabetes Mellitus Among Adults in an Urban Community in Tanzania. Ph.D. Thesis, University of Otago, Otago, New Zealand, 2010. [Google Scholar]
- Meme, N.; Amwayi, S.; Nganga, Z.; Buregyeya, E. Prevalence of undiagnosed diabetes and pre-diabetes among hypertensive patients attending Kiambu district Hospital, Kenya: A cross-sectional study. Pan Afr. Med J. 2015, 22, 286. [Google Scholar] [CrossRef] [PubMed]
- Chuma, J.; Gilson, L.; Molyneux, C. Treatment-seeking behaviour, cost burdens and coping strategies among rural and urban households in Coastal Kenya: An equity analysis. Trop. Med. Int. Health 2007, 12, 673–686. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Diabetes N = 170 n (%) | Hypertension N = 768 n (%) | Both N = 162 n (%) | Total N = 1100 n (%) | p-Value |
|---|---|---|---|---|---|
| Age group | 0.009 | ||||
| Less than 40 | 18 (10.6) | 56 (7.3) | 2 (1.2) | 76 (6.9) | |
| 40 to 59 | 60 (35.3) | 232 (30.2) | 45 (27.8) | 337 (30.6) | |
| 60 to 79 | 73 (42.9) | 381 (49.6) | 95 (58.6) | 549 (49.9) | |
| Above 80 | 19 (11.2) | 99 (12.9) | 20 (12.4) | 138 (12.6) | |
| Mean age (SD), years | 61 (16) | 63 (15) | 67 (12) | 64 (15) | |
| Gender | <0.001 | ||||
| Male | 72 (42.4) | 185 (24.0) | 42 (25.9) | 299 (27.2) | |
| Female | 98 (57.6) | 581 (75.7) | 120 (74.1) | 799 (72.6) | |
| Missing | 0 (0) | 2 (0.3) | 0 (0) | 2 (0.2) | |
| Marital Status | |||||
| Single | 25 (14.7) | 69 (9.0) | 15 (9.3) | 109 (9.9) | 0.276 |
| Married | 82 (48.2) | 376(49.0) | 87 (53.7) | 545 (49.5) | |
| Widow/Widower/Divorced | 63 (37.1) | 321 (41.8) | 60 (37.0) | 444 (40.4) | |
| Missing | 0 (0) | 2 (0.2) | 0 (0) | 2 (0.2) | |
| Head of household | 0.003 | ||||
| No | 48 (28.2) | 325 (42.3) | 67 (41.4) | 440 (40.0) | |
| Yes | 122 (71.8) | 442 (57.6) | 95 (58.6) | 659 (59.9) | |
| Missing | 0 (0) | 1 (0.1) | 0 (0) | 1 (0.1) | |
| Educational Level | <0.001 | ||||
| No education | 38 (22.4) | 252 (32.8) | 52 (32.1) | 342 (31.1) | |
| Primary | 74 (43.5) | 335 (43.6) | 75 (46.3) | 484 (44.0) | |
| Sec/Post primary | 38 (22.4) | 123 (16.0) | 23 (14.2) | 184 (16.7) | |
| College and University | 20 (11.8) | 30 (3.9) | 7 (4.3) | 57 (5.2) | |
| Others | 0 (0.0) | 28 (3.7) | 5 (3.1) | 33 (3.0) | |
| Ethnicity | <0.001 | ||||
| Kikuyu | 89 (52.4) | 312 (40.6) | 89 (54.9) | 490 (44.6) | |
| Luo | 37 (21.8) | 130 (16.9) | 23 (14.2) | 190 (17.3) | |
| Meru | 1 (0.6) | 64 (8.3) | 0 (0.0) | 65 (5.9) | |
| Embu | 16 (9.4) | 139 (18.1) | 28 (17.3) | 183 (16.7) | |
| Kalenjin | 21 (12.3) | 87 (11.3) | 19 (11.7) | 127 (11.6) | |
| Others | 6 (3.5) | 34 (4.4) | 3 (1.9) | 43 (3.9) | |
| Missing | 0 (0) | 2 (0.3) | 0 (0) | 2 (0.2) | |
| Occupation | 0.147 | ||||
| Family farm/business | 50 (29.6) | 292 (38.1) | 56 (33.9) | 398 (36.2) | |
| Skilled/unskilled worker | 28 (16.6) | 106 (13.8) | 23 (13.9) | 157 (14.3) | |
| Unemployed | 67 (39.6) | 301 (39.3) | 73 (44.2) | 441 (40.1) | |
| Missing | 1 (0.6) | 3 (0.4) | 0 (0) | 4 (0.4) | |
| Health status | 0.489 | ||||
| Good | 63 (37.1) | 258 (33.6) | 47 (29) | 368 (33.5) | |
| Average | 86 (50.6) | 399 (52.0) | 85 (52.5) | 570 (51.8) | |
| Poor | 21 (12.3) | 108 (14.0) | 30 (18.5) | 159 (14.4) | |
| Don’t know | 0 (0) | 3 (0.4) | 0 (0) | 3 (0.3) | |
| Social support with illness | 0.687 | ||||
| No | 49 (28.8) | 197 (25.6) | 41 (25.3) | 287 (26.1) | |
| Yes | 121 (71.2) | 568 (74) | 121 (74.7) | 810 (73.6) | |
| Missing | 0 (0) | 3 (0.4) | 0 (0) | 3 (0.3) | |
| Comorbidity | 0.006 | ||||
| No | 128 (75.3) | 538 (70.1) | 98 (60.5) | 764 (69.5) | |
| Yes | 39 (22.9) | 222 (28.9) | 63 (38.9) | 324 (29.5) | |
| Missing | 3 (1.8) | 8 (1) | 1 (0.6) | 12 (1.1) | |
| Debt due to illness | 0.036 | ||||
| No | 135 (85.4) | 597 (89.1) | 139 (87.4) | 871 (88.3) | |
| Yes | 16 (10.1) | 65 (9.7) | 19 (12) | 100 (10.1) | |
| Decline to answer | 7 (4.4) | 8 (1.2) | 1 (0.6) | 16 (1.6) |
| Characteristics | Diabetes N = 170 n (%) | Hypertension N = 768 n (%) | Both N = 162 n (%) | Total N = 1100 n (%) | p-Value |
|---|---|---|---|---|---|
| Place of diagnosis | 0.004 | ||||
| Mobile clinic/screening | 5 (2.9) | 56 (7.3) | 4 (2.5) | 65 (5.9) | |
| Private clinic/lab | 55 (32.4) | 169 (22) | 52 (32.1) | 276 (25.1) | |
| Public facility | 107 (62.9) | 533 (69.4) | 104 (64.2) | 744 (67.6) | |
| Others | 3 (1.8) | 10 (1.3) | 2 (1.2) | 15 (1.4) | |
| Treatment type | 0.001 | ||||
| Allopathic treatment | 158 (92.9) | 670 (87.2) | 159 (98.2) | 987 (89.7) | |
| Traditional treatment | 1 (0.6) | 10 (1.3) | 1 (0.6) | 12 (1.1) | |
| Not on treatment | 11 (6.5) | 88 (11.5) | 2 (1.2) | 101 (9.2) | |
| Current source of treatment | |||||
| Public hospital | 75 (47.5) | 309 (46.1) | 67 (42.1) | 451 (45.7) | 0.429 |
| Mission hospital | 8 (5.1) | 35 (5.2) | 11 (6.9) | 54 (5.5) | |
| Private hospital/clinic | 14 (8.9) | 78 (11.7) | 18 (11.3) | 110 (11.1) | |
| Pharmacy/chemist/shop | 14 (8.9) | 95 (14.2) | 25 (15.7) | 134 (13.6) | |
| others | 47 (29.6) | 153 (22.8) | 38 (23.9) | 238 (24.1) | |
| Regular/scheduled clinic visits | |||||
| No | 63 (39.9) | 307 (45.8) | 48 (30.2) | 418 (42.4) | 0.001 |
| Yes | 95 (60.1) | 363 (54.2) | 111 (69.8) | 569 (57.6) | |
| Last blood pressure check | <0.001 | ||||
| Less than a week | 33 (19.4) | 187 (24.4) | 43 (26.5) | 263 (24.0) | |
| 1 month | 85 (50.0) | 418 (54.6) | 99 (61.1) | 602 (54.9) | |
| 6 months | 27 (15.9) | 96 (12.6) | 11 (6.8) | 134 (12.2) | |
| 1 year or more | 13 (7.65) | 50 (6.5) | 8 (4.9) | 71 (6.5) | |
| Don’t know | 12 (7.1) | 14 (1.8) | 1 (0.6) | 27 (2.5) | |
| Missing | 0 (0) | 3 (0) | 0 (0) | 3 (0) | |
| Last blood sugar check | <0.001 | ||||
| Less than a week | 39 (22.9) | 84 (11.0) | 40 (24.7) | 163 (14.8) | |
| 1 month | 97 (57.1) | 219 (28.6) | 98 (60.5) | 414 (37.7) | |
| 6 months | 15 (8.8) | 113 (14.7) | 14 (8.6) | 142 (12.9) | |
| 1 year or more | 10 (5.9) | 147 (19.7) | 9 (5.6) | 166 (15.1) | |
| Don’t know | 9 (5.3) | 204 (26.6) | 1 (0.6) | 214 (19.5) | |
| Missing | 0 (0) | 1 (0) | 0 (0) | 1 (0) | |
| Last eye check-up | <0.001 | ||||
| Less than a week | 6 (3.5) | 33 (4.3) | 8 (4.9) | 47 (4.3) | |
| 1 month | 11 (6.5) | 61 (8.0) | 23 (14.2) | 95 (8.7) | |
| 6 months | 12 (7.1) | 59 (7.7) | 13 (8.0) | 84 (7.7) | |
| 1 year or more | 28 (16.5) | 118 (15.4) | 46 (28.4) | 192 (17.5) | |
| Don’t know | 113 (66.5) | 495 (64.6) | 72 (44.4) | 680 (61.9) | |
| Missing | 0 (0) | 2 (0) | 0 (0) | 2 (0) | |
| Admission last one year | 0.001 | ||||
| No | 151 (88.8) | 713 (92.8) | 135 (83.3) | 999 (90.8) | |
| Yes | 19 (11.2) | 55 (7.2) | 26 (16.1) | 100 (9.1) | |
| Missing | 0 (0) | 0 (0) | 1 (0.6) | 1 (0.1) | |
| Health insurance | 0.007 | ||||
| No | 123 (72.3) | 598 (77.9) | 108 (66.7) | 829 (75.4) | |
| Yes | 47 (27.7) | 168 (22.1) | 54 (33.3.7) | 271 (24.6) |
| Reasons for Non-Treatment | Number | Percentage |
|---|---|---|
| No money for medication | 38 | 37.6 |
| Feeling better, don’t think I need treatment anymore | 30 | 29.7 |
| Thinks that the disease is not serious | 13 | 12.9 |
| Treatment place too far | 11 | 10.9 |
| Disease got worse/no improvement/no hope of cure | 8 | 7.9 |
| Moved to other place | 6 | 5.9 |
| Not satisfied with treatment program | 4 | 3.9 |
| Medicines make me sick | 4 | 3.9 |
| Don’t believe that I have the disease—feel alright | 3 | 2.9 |
| Advised by health provider | 3 | 2.9 |
| Too busy with daily business | 2 | 1.9 |
| Name of Drug | Number | Percentage ** |
|---|---|---|
| Metformin | 196 | 66.0 |
| Glibenclamide | 126 | 42.4 |
| Insulin | 44 | 14.8 |
| Saxagliptin | 3 | 1.0 |
| Pioglitazone | 3 | 1.0 |
| Gliclazide, Sitagliptin, Glimepiride | Less than 1% on each of these drugs | |
| Number of antidiabetic drugs per patient | ||
| 1 | 142 | 47.8 |
| 2 | 115 | 38.7 |
| 3 | 2 | 0.7 |
| Missing | 38 | 12.8 |
| Name of Drug | Number | Percentage ** |
|---|---|---|
| Nifedipine | 359 | 49.5 |
| Hydrchlorothiazide | 325 | 44.8 |
| Enalapril | 132 | 18.2 |
| Lorsatan | 90 | 12.4 |
| Atenolol | 64 | 8.8 |
| Furosemide | 61 | 8.4 |
| Amlodipine | 39 | 5.4 |
| Methyldopa | 23 | 3.2 |
| Spironolactone | 11 | 1.5 |
| Telmisartan, Lisinopril, Irbesartan, Propranolol, Carvedilol, Hydralazine, Vastarel, Nebivolol, Olmesartan, Candesartan Atacand, Indapamide, Felodipine | Less than 1% on each of these drugs | |
| Number of antihypertensive drugs per patient | ||
| 1 | 269 | 37.1 |
| 2 | 328 | 45.2 |
| 3 | 62 | 8.6 |
| 4 or more | 11 | 1.5 |
| Characteristics | Inappropriate N = 418 n (%) | Appropriate N = 569 n (%) | Crude OR (95% CI) | p Value | Adjusted OR (95% CI) | p Value |
|---|---|---|---|---|---|---|
| Social support with illness * | ||||||
| No | 143 (34.3) | 97 (17.1) | Reference | |||
| Yes | 274 (65.7) | 471 (82.9) | 2.53 (1.88–3.41) | <0.001 | 2.46 (1.81–3.35) | <0.001 |
| Health status * | ||||||
| Poor | 73 (17.5) | 67 (11.8) | Reference | |||
| Average | 217 (51.9) | 296 (52.1) | 1.75 (1.17–2.60) | 0.006 | 1.54 (1.02–2.26) | 0.038 |
| Good | 128 (30.6) | 205 (36.1) | 1.49 (1.02–2.16) | 0.038 | 1.77 (1.16–2.70) | 0.008 |
| Current source of treatment * | ||||||
| Public hospital | 178 (42.6) | 273 (47.9) | Reference | |||
| Mission hospital | 14 (3.4) | 40 (7.0) | 1.86 (0.99–3.52) | 0.056 | 1.51 (0.78–2.89) | 0.219 |
| Private hospital/clinic | 44 (10.5) | 66 (11.6) | 0.98 (0.64–1.50) | 0.918 | 0.90 (0.58–1.40) | 0.637 |
| Pharmacy/chemist/shop | 83 (19.9) | 51 (8.9) | 0.40 (0.27–0.60) | <0.001 | 0.42 (0.28–0.63) | <0.001 |
| others | 99 (23.7) | 139 (24.4) | 0.92 (0.67–1.26) | 0.588 | 0.91 (0.65–1.27) | 0.569 |
| Admission last one year * | ||||||
| No | 392 (93.8) | 498 (87.5) | Reference | |||
| Yes | 26 (6.2) | 70 (12.3) | 2.12 (1.32–3.39) | 0.002 | 2.06 (1.27–3.36) | 0.004 |
| Alcohol status * | ||||||
| No | 308 (73.7) | 451 (79.3) | Reference | |||
| Yes | 110 (26.3) | 118 (20.7) | 0.73 (0.54–0.98) | 0.040 | 0.71 (0.52–0.98) | 0.002 |
| Age group | ||||||
| Less than 40 | 21 (5) | 40 (7) | Reference | |||
| 40 to 59 | 125 (29.9) | 178 (31.3) | 0.75 (0.42–1.33) | 0.322 | ||
| 60 to 79 | 204 (48.8) | 291 (51.1) | 0.75 (0.43–1.31) | 0.310 | ||
| Above 80 | 68 (16.3) | 60 (10.5) | 0.46 (0.25–0.87) | 0.017 | ||
| Gender | ||||||
| Female | Reference | |||||
| Male | 101 (24.2) | 162 (28.5) | 1.25 (0.94–1.67) | 0.132 | ||
| Marital Status | ||||||
| Single | 37 (8.9) | 55 (9.7) | Reference | |||
| Married | 186 (44.6) | 304 (53.5) | 1.00 (0.7–1.73) | 0.683 | ||
| Widow/Widower/Divorced | 194 (46.5) | 209 (36.8) | 0.72 (0.46–1.15) | 0.170 | ||
| Ethnicity | ||||||
| Kikuyu | 189 (45.3) | 261 (46) | Reference | |||
| Luo | 69 (16.6) | 96 (16.9) | 1.01 (0.70–1.45) | 0.968 | ||
| Meru | 11 (2.6) | 36 (6.3) | 2.37 (1.17–4.78) | 0.016 | ||
| Embu | 86 (20.6) | 93 (16.4) | 0.78 (0.55–1.11) | 0.168 | ||
| Kalenjin | 42 (10.1) | 66 (11.6) | 1.14 (0.74–1.75) | 0.556 | ||
| Others | 20 (4.8) | 16 (2.8) | 0.58 (0.29–1.15) | 0.117 | ||
| Smoking status | ||||||
| No | 405 (96.9) | 558 (98.1) | Reference | |||
| Yes | 13 (3.1) | 11 (1.9) | 0.61 (0.27–1.38) | 0.240 | ||
| Family history of hypertension | 274 (65.6) | 351 (61.7) | ||||
| No | 112 (26.8) | 177 (31.1) | ||||
| Yes | 274 (65.6) | 351 (61.7) | 1.23 (0.92–1.64) | 0.148 | ||
| Health insurance | ||||||
| No | 316 (75.6) | 410 (72.1) | Reference | |||
| Yes | 102 (24.4) | 159 (27.9) | 1.20 (0.90–1.60) | 0.213 | ||
| Education Topics | Number | Percentage |
|---|---|---|
| Education on diabetes disease | 78 | 26.5 |
| Education on hypertension | 158 | 53.7 |
| Education on lifestyle change | 63 | 21.4 |
| Education on nutrition | 78 | 26.5 |
| Education on adherence to medication | 63 | 21.4 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Karinja, M.; Pillai, G.; Schlienger, R.; Tanner, M.; Ogutu, B. Care-Seeking Dynamics among Patients with Diabetes Mellitus and Hypertension in Selected Rural Settings in Kenya. Int. J. Environ. Res. Public Health 2019, 16, 2016. https://doi.org/10.3390/ijerph16112016
Karinja M, Pillai G, Schlienger R, Tanner M, Ogutu B. Care-Seeking Dynamics among Patients with Diabetes Mellitus and Hypertension in Selected Rural Settings in Kenya. International Journal of Environmental Research and Public Health. 2019; 16(11):2016. https://doi.org/10.3390/ijerph16112016
Chicago/Turabian StyleKarinja, Miriam, Goonaseelan Pillai, Raymond Schlienger, Marcel Tanner, and Bernhards Ogutu. 2019. "Care-Seeking Dynamics among Patients with Diabetes Mellitus and Hypertension in Selected Rural Settings in Kenya" International Journal of Environmental Research and Public Health 16, no. 11: 2016. https://doi.org/10.3390/ijerph16112016
APA StyleKarinja, M., Pillai, G., Schlienger, R., Tanner, M., & Ogutu, B. (2019). Care-Seeking Dynamics among Patients with Diabetes Mellitus and Hypertension in Selected Rural Settings in Kenya. International Journal of Environmental Research and Public Health, 16(11), 2016. https://doi.org/10.3390/ijerph16112016





