The Social Context of HIV Prevention and Care among Black Men Who Have Sex with Men in Three U.S. Cities: The Neighborhoods and Networks (N2) Cohort Study
Abstract
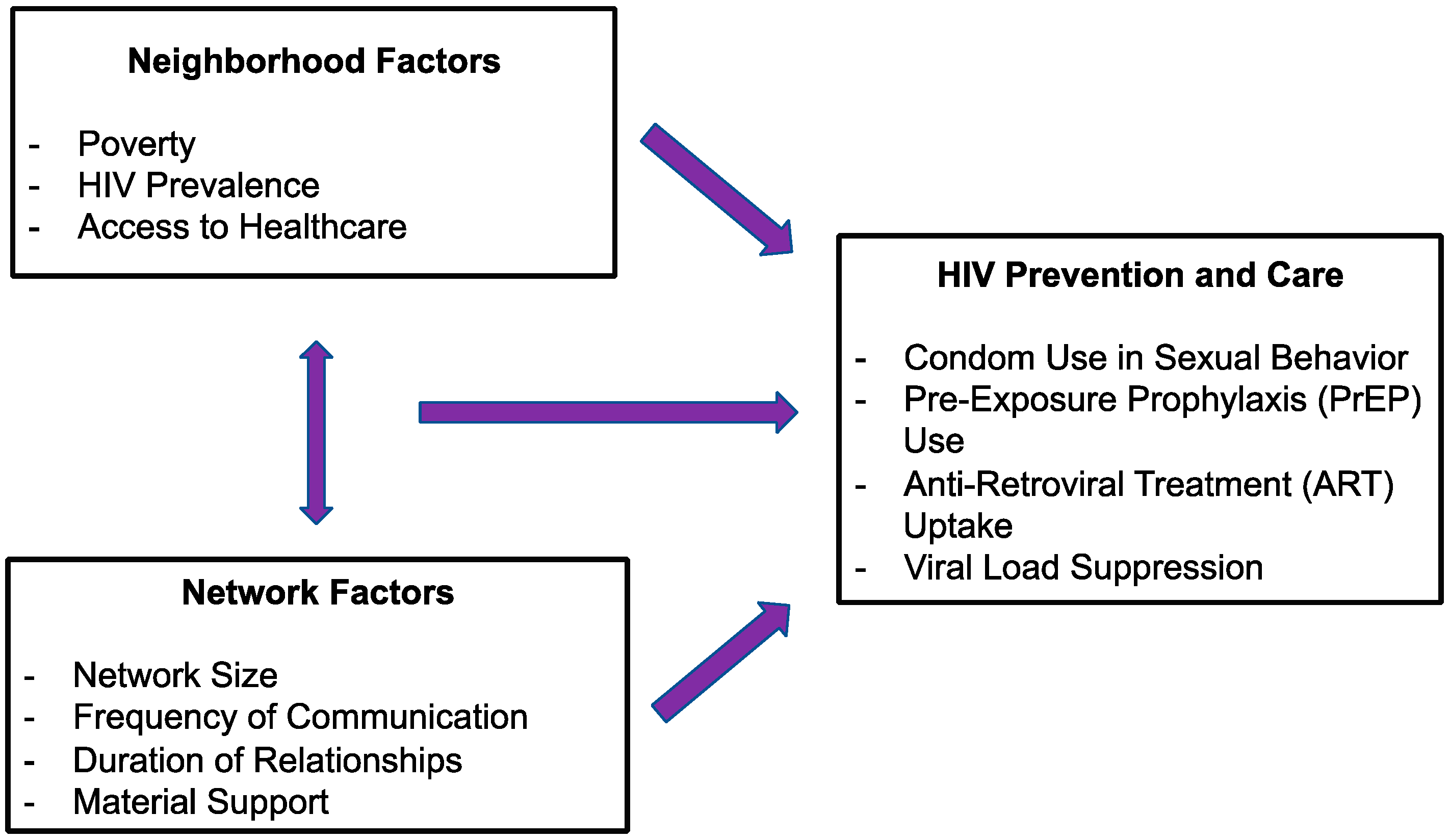
1. Background
2. Methods/Design
2.1. Overview of Study Design
2.2. Governance and Organizational Structure
2.3. Ethical Oversight
2.4. Participant Recruitment
2.5. Inclusion and Exclusion Criteria
2.5.1. Data Collection 1: Self-Report Survey Instruments
2.5.2. Data Collection 2: Neighborhoods Assessment
2.5.3. Data Collection 3: Social and Sexual Networks Assessment
2.5.4. HIV Prevention and Care Continuum Outcomes
2.5.5. Covariates
2.5.6. Retention Plans
2.6. Data Management, Quality Assurance and Control, and Statistical Analysis
3. Findings to Date
4. Discussion
Strengths and Limitations
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| ART | antiretroviral treatment |
| CSV | comma separated value |
| HIV | human immunodeficiency virus |
| ERGMs | exponential random graph models |
| GIS | geographic information systems |
| GPS | global positioning system |
| LGBT | lesbian, gay, bisexual and transgender |
| MSM | men who have sex with men |
| N2 | Neighborhoods and Networks |
| PrEP | pre-exposure prophylaxis |
| RDS | respondent-driven sampling |
| STIs | sexually transmitted infections |
Appendix A. Research and Coordination Sites
Appendix A.1. Chicago Site: Chicago Center for HIV Elimination
Appendix A.2. Jackson Site: My Brother’s Keeper, Inc.
Appendix A.3. New Orleans Site: Brotherhood, Inc.
References
- Singh, S.; Song, R.; Johnson, A.S.; McCray, E.; Hall, H.I. HIV Incidence, Prevalence, and Undiagnosed Infections in U.S. Men Who Have Sex with Men. Ann. Intern. Med. 2018, 168, 685–694. [Google Scholar] [CrossRef]
- CDC. Diagnoses of HIV Infection in the United States and Dependent Areas 2015; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2016. [Google Scholar]
- CDC. Kaposi’s Sarcoma and Pneumocystis Pneumonia among Homosexual Men—New York City and California; Report No.: 30(25); Centers for Disease Control and Prevention: Atlanta, GA, USA, 1981. [Google Scholar]
- Anna; Johnson, S.; Hall, R.S.I. (Eds.) State-level estimates of HIV prevalence, incidence, and undiagnosed infections. In Proceedings of the Conference on Retroviruses and Opportunistic Infections, Seattle, WA, USA, 13–16 February 2017. [Google Scholar]
- Hess, K.L.; Hu, X.; Lansky, A.; Mermin, J.; Hall, H.I. (Eds.) Estimating the lifetime risk of a diagnosis of HIV infection in the United States. In Proceedings of the Conference on Retroviruses and Opportunistic Infections, Boston, MA, USA, 22–25 February 2016. [Google Scholar]
- Chicago Department of Public Health. HIV/STI Surveillance Report, 2014; Chicago: City of Chicago, IL, USA, 2014. [Google Scholar]
- Lieb, S.; Prejean, J.; Thompson, D.R.; Fallon, S.J.; Cooper, H.; Gates, G.J.; Liberti, T.M.; Friedman, S.R.; Malow, R.M. HIV prevalence rates among men who have sex with men in the southern United States: Population-based estimates by race/ethnicity. AIDS Behav. 2011, 15, 596–606. [Google Scholar] [CrossRef][Green Version]
- Oster, A.M.; Dorell, C.G.; Mena, L.A.; Thomas, P.E.; Toledo, C.A.; Heffelfinger, J.D. HIV risk among young African American men who have sex with men: A case-control study in Mississippi. Am. J. Public Health 2011, 101, 137–143. [Google Scholar] [CrossRef]
- Mississippi State Department of Health. State of Mississippi 2010 STD/HIV Epidemiologic Profile; Mississippi State Department of Health: Jackson, MS, USA, 2010. [Google Scholar]
- Mississippi State Department of Health. Mississippians Living with HIV Disease in 2013; Mississippi State Department of Health: Jackson, MS, USA, 2014. [Google Scholar]
- Millett, G.A.; Peterson, J.L.; Flores, S.A.; Hart, T.A.; Jeffries, W.L., 4th; Wilson, P.A.; Rourke, S.B.; Heilig, C.M.; Elford, J.; Fenton, K.A.; et al. Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: A meta-analysis. Lancet 2012, 380, 341–348. [Google Scholar] [CrossRef]
- Adeyemi, O.M.; Livak, B.; McLoyd, P.; Smith, K.Y.; French, A.L. Racial/ethnic disparities in engagement in care and viral suppression in a large urban HIV clinic. Clin. Infect. Dis. 2013, 56, 1512–1514. [Google Scholar] [CrossRef]
- Hoots, B.E.; Finlayson, T.; Nerlander, L.; Paz-Bailey, G.; National HIV Behavioral Surveillance Study Group. Willingness to Take, Use of, and Indications for Pre-exposure Prophylaxis Among Men Who Have Sex with Men-20 US Cities, 2014. Clin. Infect. Dis. 2016, 63, 672–677. [Google Scholar] [CrossRef] [PubMed]
- Baral, S.; Logie, C.H.; Grosso, A.; Wirtz, A.L.; Beyrer, C. Modified social ecological model: A tool to guide the assessment of the risks and risk contexts of HIV epidemics. BMC Public Health 2013, 13, 482. [Google Scholar] [CrossRef] [PubMed]
- Bouris, A.; Voisin, D.; Pilloton, M.; Flatt, N.; Eavou, R.; Hampton, K.; Kuhns, L.M.; Eder, M.; Schneider, J.A. Project nGage: Network supported HIV care engagement for younger black men who have sex with men and transgender persons. J. AIDS Clin. Res. 2013, 4. [Google Scholar] [CrossRef]
- Díaz, R.M.; Ayala, G. Social Discrimination and Health: The Case of Latino Gay Men and HIV Risk; The Policy Institute of the National Gay and Lesbian Task Force: Washington, DC, USA, 2001. [Google Scholar]
- Bauermeister, J.A.; Connochie, D.; Eaton, L.; Demers, M.; Stephenson, R. Geospatial Indicators of Space and Place: A Review of Multilevel Studies of HIV Prevention and Care Outcomes Among Young Men Who Have Sex with Men in the United States. J. Sex Res. 2017, 54, 446–464. [Google Scholar] [CrossRef] [PubMed]
- Frye, V.; Nandi, V.; Egan, J.E.; Cerda, M.; Rundle, A.; Quinn, J.W.; Sheehan, D.; Ompad, D.C.; Van Tieu, H.; Greene, E.; et al. Associations Among Neighborhood Characteristics and Sexual Risk Behavior Among Black and White MSM Living in a Major Urban Area. AIDS Behav. 2017, 21, 870–890. [Google Scholar] [CrossRef]
- Chen, Y.T.; Kolak, M.; Duncan, D.T.; Schumm, P.; Michaels, S.; Fujimoto, K.; Schneider, J.A. Neighbourhoods, networks and pre-exposure prophylaxis awareness: A multilevel analysis of a sample of young black men who have sex with men. Sex. Transm. Infect. 2018, 95, 228–235. [Google Scholar] [CrossRef]
- Fujimoto, K.; Flash, C.A.; Kuhns, L.M.; Kim, J.Y.; Schneider, J.A. Social networks as drivers of syphilis and HIV infection among young men who have sex with men. Sex. Transm. Infect. 2018, 94, 365–371. [Google Scholar] [CrossRef] [PubMed]
- Dasgupta, S.; Kramer, M.R.; Rosenberg, E.S.; Sanchez, T.H.; Reed, L.; Sullivan, P.S. The Effect of Commuting Patterns on HIV Care Attendance Among Men Who Have Sex with Men (MSM) in Atlanta, Georgia. JMIR Public Health Surveill. 2015, 1, e10. [Google Scholar] [CrossRef] [PubMed]
- Goswami, N.D.; Schmitz, M.M.; Sanchez, T.; Dasgupta, S.; Sullivan, P.; Cooper, H.; Rane, D.; Kelly, J.; Del Rio, C.; Waller, L.A. Understanding Local Spatial Variation Along the Care Continuum: The Potential Impact of Transportation Vulnerability on HIV Linkage to Care and Viral Suppression in High-Poverty Areas, Atlanta, Georgia. J. Acquir. Immune Defic. Syndr. 2016, 72, 65–72. [Google Scholar] [CrossRef]
- Bauermeister, J.A.; Eaton, L.; Andrzejewski, J.; Loveluck, J.; VanHemert, W.; Pingel, E.S. Where You Live Matters: Structural Correlates of HIV Risk Behavior Among Young Men Who Have Sex with Men in Metro Detroit. AIDS Behav. 2015, 19, 2358–2369. [Google Scholar] [CrossRef]
- Meyer, I.H. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychol. Bull. 2003, 129, 674–697. [Google Scholar] [CrossRef]
- Frye, V.; Nandi, V.; Egan, J.; Cerda, M.; Greene, E.; Van Tieu, H.; Ompad, D.C.; Hoover, D.R.; Lucy, D.; Baez, E.; Koblin, B.A. Sexual orientation- and race-based discrimination and sexual HIV risk behavior among urban MSM. AIDS Behav. 2015, 19, 257–269. [Google Scholar] [CrossRef]
- Holtgrave, D.R.; Kim, J.J.; Adkins, C.; Maulsby, C.; Lindsey, K.D.; Johnson, K.M.; Montoya, D.C.; Kelley, R.T. Unmet HIV service needs among Black men who have sex with men in the United States. AIDS Behav 2014, 18, 36–40. [Google Scholar] [CrossRef]
- Sampson, R.J.; Groves, W.B. Community Structure and Crime: Testing Social-Disorganization Theory. Am. J. Sociol. 1989, 94, 774–802. [Google Scholar] [CrossRef]
- Gallo, L.C.; Bogart, L.M.; Vranceanu, A.M.; Matthews, K.A. Socioeconomic status, resources, psychological experiences, and emotional responses: A test of the reserve capacity model. J. Personal. Soc. Psychol. 2005, 88, 386–399. [Google Scholar] [CrossRef]
- Bauermeister, J.; Eaton, L.; Stephenson, R. A Multilevel Analysis of Neighborhood Socioeconomic Disadvantage and Transactional Sex with Casual Partners Among Young Men Who Have Sex with Men Living in Metro Detroit. Behav. Med. 2016, 42, 197–204. [Google Scholar] [CrossRef]
- Frye, V.; Latka, M.H.; Koblin, B.; Halkitis, P.N.; Putnam, S.; Galea, S. The urban environment and sexual risk behavior among men who have sex with men. J. Urban Health 2006, 83, 308–324. [Google Scholar] [CrossRef]
- Bohl, D.; Raymond, H.; Arnold, M.; McFarland, W. Concurrent sexual partnerships and racial disparities in HIV infection among men who have sex with men. Sex. Transm. Infect. 2009, 85, 367–369. [Google Scholar] [CrossRef]
- Hurt, C.B.; Matthews, D.D.; Calabria, M.S.; Green, K.A.; Adimora, A.A.; Golin, C.E.; Hightow-Weidman, L.B. Sex with older partners is associated with primary HIV infection among men who have sex with men in North Carolina. JAIDS J. Acquir. Immune Defic. Syndr. 2010, 54, 185–190. [Google Scholar] [CrossRef]
- Skaathun, B.; Khanna, A.S.; Morgan, E.; Friedman, S.R.; Schneider, J.A. Network Viral Load: A Critical Metric for HIV Elimination. J. Acquir. Immune Defic. Syndr. 2018, 77, 167–174. [Google Scholar] [CrossRef]
- Birkett, M.; Kuhns, L.M.; Latkin, C.; Muth, S.; Mustanski, B. The sexual networks of racially diverse young men who have sex with men. Arch. Sex. Behav. 2015, 44, 1787–1797. [Google Scholar] [CrossRef]
- Schneider, J.A.; Cornwell, B.; Ostrow, D.; Michaels, S.; Schumm, P.; Laumann, E.O.; Friedman, S. Network mixing and network influences most linked to HIV infection and risk behavior in the HIV epidemic among black men who have sex with men. Am. J. Public Health 2013, 103, e28–e36. [Google Scholar] [CrossRef]
- Schneider, J.; Michaels, S.; Bouris, A. Family network proportion and HIV risk among black men who have sex with men. J. Acquir. Immune Defic. Syndr. 2012, 61, 627–635. [Google Scholar] [CrossRef]
- Shah, N.S.; Iveniuk, J.; Muth, S.Q.; Michaels, S.; Jose, J.A.; Laumann, E.O.; Schneider, J.A. Structural bridging network position is associated with HIV status in a younger Black men who have sex with men epidemic. AIDS Behav. 2014, 18, 335–345. [Google Scholar] [CrossRef]
- Khanna, A.S.; Schumm, P.; Schneider, J.A. Facebook network structure and awareness of preexposure prophylaxis among young men who have sex with men. Ann. Epidemiol. 2017, 27, 176–180. [Google Scholar] [CrossRef]
- Newcomb, M.E.; Mustanski, B. Racial differences in same-race partnering and the effects of sexual partnership characteristics on HIV Risk in MSM: A prospective sexual diary study. J. Acquir. Immune Defic. Syndr. 2013, 62, 329–333. [Google Scholar] [CrossRef]
- Schneider, J.; Cornwell, B.; Jonas, A.; Lancki, N. Network dynamics of HIV risk and prevention in a population-based cohort of young Black men who have sex with men. Netw. Sci. 2017, 5, 381–409. [Google Scholar] [CrossRef]
- Schneider, J.A.; Lancki, N.; Schumm, P. At the intersection of criminal justice involvement and sexual orientation: Dynamic networks and health among a population-based sample of young Black men who have sex with men. Soc. Netw. 2017, 51, 73–87. [Google Scholar] [CrossRef] [PubMed]
- Young, L.E.; Jonas, A.B.; Michaels, S.; Jackson, J.D.; Pierce, M.L.; Schneider, J.A.; uConnect Study Team. Social-structural properties and HIV prevention among young men who have sex with men in the ballroom house and independent gay family communities. Soc. Sci. Med. 2017, 174, 26–34. [Google Scholar] [CrossRef] [PubMed]
- Kubicek, K.; McNeeley, M.; Holloway, I.W.; Weiss, G.; Kipke, M.D. “It’s Like Our Own Little World”: Resilience as a Factor in Participating in the Ballroom Community Subculture. AIDS Behav. 2013, 17, 1524–1539. [Google Scholar] [CrossRef] [PubMed]
- Khanna, A.S.; Michaels, S.; Skaathun, B.; Morgan, E.; Green, K.; Young, L.; Schneider, J.A.; for the uConnect Study Team. Preexposure Prophylaxis Awareness and Use in a Population-Based Sample of Young Black Men Who Have Sex with Men. JAMA Intern. Med. 2016, 176, 136–138. [Google Scholar] [CrossRef]
- Duncan, D.T.; Kapadia, F.; Halkitis, P.N. Examination of spatial polygamy among young gay, bisexual, and other men who have sex with men in New York City: The P18 cohort study. Int. J. Environ. Res. Public Health 2014, 11, 8962–8983. [Google Scholar] [CrossRef] [PubMed]
- Duncan, D.T.; Kawachi, I.; Subramanian, S.V.; Aldstadt, J.; Melly, S.J.; Williams, D.R. Examination of how neighborhood definition influences measurements of youths’ access to tobacco retailers: A methodological note on spatial misclassification. Am. J. Epidemiol. 2014, 179, 373–381. [Google Scholar] [CrossRef]
- Duncan, D.T.; Tamura, K.; Regan, S.D.; Athens, J.; Elbel, B.; Meline, J.; Al-Ajlouni, Y.A.; Chaix, B. Quantifying spatial misclassification in exposure to noise complaints among low-income housing residents across New York City neighborhoods: A Global Positioning System (GPS) study. Ann. Epidemiol. 2017, 27, 67–75. [Google Scholar] [CrossRef]
- Duncan, D.T.; Regan, S.; Chaix, B. Operational Neighborhood Definitions in Health Research: Spatial Misclassification and Other Issues. In Neighborhoods and Health, 2nd ed.; Duncan, D.T., Kawachi, I, Eds.; Oxford University Press: Oxford, UK, 2018. [Google Scholar]
- Chaix, B.; Merlo, J.; Evans, D.; Leal, C.; Havard, S. Neighbourhoods in eco-epidemiologic research: Delimiting personal exposure areas. A response to Riva, Gauvin, Apparicio and Brodeur. Soc. Sci. Med. 2009, 69, 1306–1310. [Google Scholar] [CrossRef] [PubMed]
- Chum, A.; O’Campo, P. Contextual determinants of cardiovascular diseases: Overcoming the residential trap by accounting for non-residential context and duration of exposure. Health Place 2013, 24, 73–79. [Google Scholar] [CrossRef]
- Matthews, S.A. Spatial Polygamy and the Heterogeneity of Place: Studying People and Place via Egocentric Methods; Springer: New York, NY, USA, 2011. [Google Scholar]
- Zenk, S.N.; Schulz, A.J.; Matthews, S.A.; Odoms-Young, A.; Wilbur, J.; Wegrzyn, L.; Gibbs, K.; Braunschweig, C.; Stokes, C. Activity space environment and dietary and physical activity behaviors: A pilot study. Health Place 2011, 17, 1150–1161. [Google Scholar] [CrossRef]
- Kwan, M.-P. The Uncertain Geographic Context Problem. Ann. Assoc. Am. Geogr. 2012, 102, 958–968. [Google Scholar] [CrossRef]
- Kwan, M.-P. How GIS can help address the uncertain geographic context problem in social science research. Ann. GIS 2012, 18, 245–255. [Google Scholar] [CrossRef]
- Koblin, B.A.; Egan, J.E.; Nandi, V.; Sang, J.M.; Cerda, M.; Tieu, H.V.; Ompad, D.C.; Hoover, D.R.; Frye, V. Congruence of Home, Social and Sex Neighborhoods among Men Who Have Sex with Men, NYCM2M Study. J. Urban Health 2017, 94, 364–374. [Google Scholar] [CrossRef]
- Chaix, B.; Meline, J.; Duncan, S.; Merrien, C.; Karusisi, N.; Perchoux, C.; Lewin, A.; Labadi, K.; Kestens, Y. GPS tracking in neighborhood and health studies: A step forward for environmental exposure assessment, a step backward for causal inference? Health Place 2013, 21, 46–51. [Google Scholar] [CrossRef]
- Duncan, D.T.; Kapadia, F.; Regan, S.D.; Goedel, W.C.; Levy, M.D.; Barton, S.C.; Friedman, S.R.; Halkitis, P.N. Feasibility and Acceptability of Global Positioning System (GPS) Methods to Study the Spatial Contexts of Substance Use and Sexual Risk Behaviors among Young Men Who Have Sex with Men in New York City: A P18 Cohort Sub-Study. PLoS ONE 2016, 11, e0147520. [Google Scholar] [CrossRef]
- Duncan, D.T.; Chaix, B.; Regan, S.D.; Park, S.H.; Draper, C.; Goedel, W.C.; Gipson, J.A.; Guilamo-Ramos, V.; Halkitis, P.N.; Brewer, R.; et al. Collecting Mobility Data with GPS Methods to Understand the HIV Environmental Riskscape Among Young Black Men Who Have Sex with Men: A Multi-city Feasibility Study in the Deep South. AIDS Behav. 2018, 22, 3057–3070. [Google Scholar] [CrossRef]
- Tieu, H.V.; Liu, T.Y.; Hussen, S.; Connor, M.; Wang, L.; Buchbinder, S.; Wilton, L.; Gorbach, P.; Mayer, K.; Griffith, S.; et al. Sexual Networks and HIV Risk among Black Men Who Have Sex with Men in 6 U.S. Cities. PLoS ONE 2015, 10, e0134085. [Google Scholar] [CrossRef]
- Heckathorn, D.D. Respondent-driven sampling: A new approach to the study of hidden populations. Soc. Probl. 1997, 44, 174–199. [Google Scholar] [CrossRef]
- Fujimoto, K.; Turner, R.; Kuhns, L.M.; Kim, J.Y.; Zhao, J.; Schneider, J.A. Network Centrality and Geographical Concentration of Social and Service Venues that Serve Young Men Who Have Sex with Men. AIDS Behav. 2017, 21, 3578–3589. [Google Scholar] [CrossRef] [PubMed]
- Morgan, E.; Khanna, A.S.; Skaathun, B.; Michaels, S.; Young, L.; Duvoisin, R.; Chang, M.; Voisin, D.; Cornwell, B.; Coombs, R.W.; et al. Marijuana Use Among Young Black Men Who Have Sex with Men and the HIV Care Continuum: Findings From the uConnect Cohort. Subst. Use Misuse 2016, 51, 1751–1759. [Google Scholar] [CrossRef] [PubMed]
- Young, L.E.; Schumm, P.; Alon, L.; Bouris, A.; Ferreira, M.; Hill, B.; Khanna, A.S.; Valente, T.W.; Schneider, J.A. PrEP Chicago: A randomized controlled peer change agent intervention to promote the adoption of pre-exposure prophylaxis for HIV prevention among young Black men who have sex with men. Clin. Trials 2018, 15, 44–52. [Google Scholar] [CrossRef] [PubMed]
- Encyclopedia of Survey Research Methods. 2008. Available online: https://us.sagepub.com/en-us/nam/encyclopedia-of-survey-research-methods/book227714 (accessed on 11 January 11 2019).
- Mavoa, S.; Oliver, M.; Witten, K.; Badland, H.M. Linking GPS and travel diary data using sequence alignment in a study of children’s independent mobility. Int. J. Health Geogr. 2011, 10, 64. [Google Scholar] [CrossRef] [PubMed]
- Schipperijn, J.; Kerr, J.; Duncan, S.; Madsen, T.; Klinker, C.D.; Troelsen, J. Dynamic Accuracy of GPS Receivers for Use in Health Research: A Novel Method to Assess GPS Accuracy in Real-World Settings. Front. Public Health 2014, 2, 21. [Google Scholar] [CrossRef]
- Oreskovic, N.M.; Perrin, J.M.; Robinson, A.I.; Locascio, J.J.; Blossom, J.; Chen, M.L.; Winickoff, J.P.; Field, A.E.; Green, C.; Goodman, E. Adolescents’ use of the built environment for physical activity. BMC Public Health 2015, 15, 251. [Google Scholar] [CrossRef]
- Theall, K.P.; Felker-Kantor, E.; Wallace, M.; Zhang, X.; Morrison, C.N.; Wiebe, D.J. Considering high alcohol and violence neighborhood context using daily diaries and GPS: A pilot study among people living with HIV. Drug Alcohol Depend. 2018, 187, 236–241. [Google Scholar] [CrossRef]
- Harrison, F.; Burgoine, T.; Corder, K.; van Sluijs, E.M.; Jones, A. How well do modelled routes to school record the environments children are exposed to? A cross-sectional comparison of GIS-modelled and GPS-measured routes to school. Int. J. Health Geogr. 2014, 13, 5. [Google Scholar] [CrossRef]
- Oliver, M.; Mavoa, S.; Badland, H.M.; Carroll, P.A.; Asiasiga, L.; Tavae, N.; Kearns, R.A.; Witten, K. What constitutes a ‘trip’? Examining child journey attributes using GPS and self-report. Children’s Geogr. 2014, 12, 249–256. [Google Scholar] [CrossRef]
- Oliver, M.; Witten, K.; Kearns, R.A.; Mavoa, S.; Badland, H.M.; Carroll, P.; Drumheller, C.; Tavae, N.; Asiasiga, L.; Jelley, S.; et al. Kids in the city study: Research design and methodology. BMC Public Health 2011, 11, 587. [Google Scholar] [CrossRef]
- Goedel, W.C.; Reisner, S.L.; Janssen, A.C.; Poteat, T.C.; Regan, S.D.; Kreski, N.T.; Confident, G.; Duncan, D.T. Acceptability and Feasibility of Using a Novel Geospatial Method to Measure Neighborhood Contexts and Mobility Among Transgender Women in New York City. Transgender Health 2017, 2, 96–106. [Google Scholar] [CrossRef] [PubMed]
- Georgiadou, P.Y.; Kleusberg, A. On carrier signal multipath effects in relative GPS positioning. Manuscr. Geod. 1988, 13, 172–179. [Google Scholar]
- U.S. Census Bureau. American Census Survey (ACS). Available online: https://www.census.gov/programs-surveys/acs/ (accessed on 11 January 2019).
- U.S. Census Bureau. Decennial Census of Population and Housing. Available online: https://www.census.gov/programs-surveys/decennial-census.html (accessed on 11 January 2019).
- Duncan, D.T.; Goedel, W.; Chunara, R. Quantitative Methods for Measuring Neighborhood Characteristics in Health Research. In Neighborhoods and Health, 2nd ed.; Duncan, D.T., Kawachi, I., Eds.; Oxford University Press: Oxford, UK, 2018. [Google Scholar]
- Burt, R.S. Network items and the general social survey. Soc. Netw. 1984, 6, 293–339. [Google Scholar] [CrossRef]
- Suzman, R. The National Social Life, Health, and Aging Project: An introduction. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2009, 64, i5–i11. [Google Scholar] [CrossRef]
- Latkin, C.; Yang, C.; Tobin, K.; Roebuck, G.; Spikes, P.; Patterson, J. Social network predictors of disclosure of MSM behavior and HIV-positive serostatus among African American MSM in Baltimore, Maryland. AIDS Behav. 2012, 16, 535–542. [Google Scholar] [CrossRef]
- Young, A.M.; Rudolph, A.E.; Su, A.E.; King, L.; Jents, S.; Havens, J.R. Accuracy of name and age data provided about network members in a social network study of people who use drugs: Implications for constructing sociometric networks. Ann. Epidemiol. 2016, 26, 802–809. [Google Scholar] [CrossRef] [PubMed]
- Schneider, J.A.; Zhou, A.N.; Laumann, E.O. A new HIV prevention network approach: Sociometric peer change agent selection. Soc. Sci. Med. (1982) 2015, 125, 192–202. [Google Scholar] [CrossRef]
- (CDC) CfDCaP. HIV Testing and Risk Behaviors among Gay, Bisexual, and Other Men Who Have Sex with Men-United States; Contract No.: 958; CDC: Atlanta, GA, USA, 2013. [Google Scholar]
- Anselin, L. Spatial Econometrics: Methods and Models; Springer Science & Business Media: Berlin, Germany, 2013. [Google Scholar]
- Anselin, L.B.; Bera, A.K. Spatial dependence in linear regression models with an introduction to spatial econometrics. Stat. Textb. Monogr. 1998, 155, 237–290. [Google Scholar]
- LeSage, J.P. An introduction to spatial econometrics. Revue D’économie Industrielle 2008, 3, 19–44. [Google Scholar] [CrossRef]
- Altman, M.G.; Gill, J.; McDonald, M.P. Numerical Issues in Statistical Computing for the Social Scientist; John Wiley & Sons: Hoboken, NJ, USA, 2004. [Google Scholar]
- Robins, G.; Pattison, P.; Woolcock, J. Missing data in networks: Exponential random graph (p∗) models for networks with non-respondents. Soc. Netw. 2004, 26, 257–283. [Google Scholar] [CrossRef]
- Handcock, M.S.; Gile, K.J. Modeling social networks from sampled data. Ann. Appl. Stat. 2010, 4, 5–25. [Google Scholar] [CrossRef] [PubMed]
- White House Office of National AIDS Policy. National HIV/AIDS Strategy for the United States: Updated to 2020. 2015. Available online: https://www.aids.gov/federal-resources/national-hiv-aids-strategy/nhas-update.pdf (accessed on 11 January 2019).
- Fauci, A.S.; Redfield, R.R.; Sigounas, G.; Weahkee, M.D.; Giroir, B.P. Ending the HIV Epidemic: A Plan for the United States. JAMA 2019, 321, 844–845. [Google Scholar] [CrossRef] [PubMed]
- McNairy, M.L.; El-Sadr, W.M. The HIV care continuum: No partial credit given. AIDS 2012, 26, 1735–1738. [Google Scholar] [CrossRef]
- Halkitis, P.N.; Kapadia, F.; Siconolfi, D.E.; Moeller, R.W.; Figueroa, R.P.; Barton, S.C.; Blachman-Forshay, J. Individual, psychosocial, and social correlates of unprotected anal intercourse in a new generation of young men who have sex with men in New York City. Am. J. Public Health 2013, 103, 889–895. [Google Scholar] [CrossRef] [PubMed]
- Okafor, N.; Rosenberg, E.S.; Luisi, N.; Sanchez, T.; del Rio, C.; Sullivan, P.S.; Kelley, C.F. Disparities in herpes simplex virus type 2 infection between black and white men who have sex with men in Atlanta, GA. Int. J. STD AIDS 2015, 26, 740–745. [Google Scholar] [CrossRef]
- Sullivan, P.S.; Peterson, J.; Rosenberg, E.S.; Kelley, C.F.; Cooper, H.; Vaughan, A.; Salazar, L.F.; Frew, P.; Wingood, G.; Diclemente, R.; et al. Understanding racial HIV/STI disparities in black and white men who have sex with men: A multilevel approach. PLoS ONE 2014, 9, e90514. [Google Scholar] [CrossRef]
- Goodkin, K.; Miller, E.N.; Cox, C.; Reynolds, S.; Becker, J.T.; Martin, E.; Selnes, O.A.; Ostrow, D.G.; Sacktor, N.C.; Multicenter AIDS Cohort Study. Effect of ageing on neurocognitive function by stage of HIV infection: Evidence from the Multicenter AIDS Cohort Study. Lancet HIV 2017, 4, e411–e422. [Google Scholar] [CrossRef]
- McNulty, M.C.; Schneider, J.A. Care continuum entry interventions: Seek and test strategies to engage persons most impacted by HIV within the United States. AIDS 2018, 32, 407–417. [Google Scholar] [CrossRef] [PubMed]
- New York City Department of Health and Mental Hygiene. The New York City HIV Status Neutral Prevention and Treatment Cycle 2016. Available online: https://www1.nyc.gov/site/doh/health/health-topics/hiv-status-neutral-prevention-and-treatment-cycle.page (accessed on 11 January 2019).
- Halkitis, P.N.; Kapadia, F.; Bub, K.L.; Barton, S.; Moreira, A.D.; Stults, C.B. A Longitudinal Investigation of Syndemic Conditions Among Young Gay, Bisexual, and Other MSM: The P18 Cohort Study. AIDS Behav. 2015, 19, 970–980. [Google Scholar] [CrossRef]
- Sullivan, P.S.; Rosenberg, E.S.; Sanchez, T.H.; Kelley, C.F.; Luisi, N.; Cooper, H.L.; Diclemente, R.J.; Wingood, G.M.; Frew, P.M.; Salazar, L.F.; et al. Explaining racial disparities in HIV incidence in black and white men who have sex with men in Atlanta, GA: A prospective observational cohort study. Ann. Epidemiol. 2015, 25, 445–454. [Google Scholar] [CrossRef]
- Koblin, B.A.; Mayer, K.H.; Eshleman, S.H.; Wang, L.; Mannheimer, S.; del Rio, C.; Shoptaw, S.; Magnus, M.; Buchbinder, S.; Wilton, L.; et al. Correlates of HIV acquisition in a cohort of Black men who have sex with men in the United States: HIV prevention trials network (HPTN) 061. PLoS ONE 2013, 8, e70413. [Google Scholar] [CrossRef]
- Magnus, M.; Franks, J.; Griffith, S.; Arnold, M.P.; Goodman, K.; Wheeler, D.P.; HPTN 061 Study Group. Engaging, recruiting, and retaining black men who have sex with men in research studies: Don’t underestimate the importance of staffing--lessons learned from HPTN 061, the BROTHERS study. J. Public Health Manag. Pract JPHMP 2014, 20, E1–E9. [Google Scholar] [CrossRef]
- Garcia, J.; Parker, R.G.; Parker, C.; Wilson, P.A.; Philbin, M.; Hirsch, J.S. The limitations of ‘Black MSM’ as a category: Why gender, sexuality, and desire still matter for social and biomedical HIV prevention methods. Glob. Public Health 2016, 11, 1026–1048. [Google Scholar] [CrossRef] [PubMed]
- Bowleg, L.; Del Rio-Gonzalez, A.M.; Holt, S.L.; Pérez, C.; Massie, J.S.; Mandell, J.E.; Boone, C.A. Intersectional Epistemologies of Ignorance: How Behavioral and Social Science Research Shapes What We Know, Think We Know, and Don’t Know About U.S. Black Men’s Sexualities. J. Sex Res. 2017, 54, 577–603. [Google Scholar] [CrossRef]
- Livak, B.; Michaels, S.; Green, K.; Nelson, C.; Westbrook, M.; Simpson, Y.; Prachand, N.G.; Benbow, N.; Schneider, J.A. Estimating the number of young Black men who have sex with men (YBMSM) on the south side of Chicago: Towards HIV elimination within US urban communities. J. Urban Health Bull. N. Y. Acad. Med. 2013, 90, 1205–1213. [Google Scholar] [CrossRef] [PubMed]
| Domain | Topics |
|---|---|
| Early Life Experiences | Adverse Childhood Experiences, Childhood Peer Victimization |
| Identity | Internalized Racism, Internalized Homophobia, Identity Congruence |
| Housing | Current Living Arrangement, Housing Affordability |
| Neighborhood Perceptions | Spatial Stigma, Social and Physical Disorder, Collective Efficacy |
| Mental Health | Depression, Anxiety, Post-Traumatic Stress Disorder |
| Substance Use | Tobacco Use, Alcohol Use, Illicit Drug Use |
| Sexual Behavior | Female Partners, Male Partners, Transgender Female Partners |
| HIV Care | Linkage to Care, Retention in Care, Viral Load |
| HIV Prevention | Perceived Risk for HIV Infection, Exposure to Prevention Activities |
| Healthcare | Health Literacy, Health Insurance Coverage, Medical Mistrust |
| Social Media and Technology | Smartphone Ownership, Social Media Use |
| Socioeconomic Circumstances | Financial Hardship, Relationship Status, Nativity |
| Total | Chicago | Deep South | |||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | p-diff a | |
| Total participants | 361 | 259 | 102 | ||||
| Age range in years (M; SD) | 17–65 (34.3; 5.1) | 17–36 (26.0; 4.1) | 21–65 (37.5; 10.8) | 0.04 | |||
| Highest education received | |||||||
| Some high school | 54 | 15.0% | 33 | 12.7% | 21 | 20.6% | 0.02 |
| High school | 128 | 35.5% | 102 | 39.4% | 26 | 25.5% | |
| Some secondary education | 179 | 49.6% | 124 | 47.9% | 55 | 53.9% | |
| Employment status | |||||||
| Employed or studying | 185 | 51.2% | 135 | 52.1% | 50 | 49% | 0.60 |
| Not employed, not studying | 176 | 48.8% | 124 | 47.9% | 52 | 51% | |
| Annual income | |||||||
| <$25,000 | 240 | 66.5% | 185 | 71.4% | 55 | 53.9% | <0.001 |
| ≥$25,000 | 102 | 28.3% | 73 | 28.2% | 29 | 28.4% | |
| Not reported | 19 | 5.3% | 1 | 0.4% | 18 | 17.6% | |
| Housingb | |||||||
| Homeless | 105 | 29.1% | 80 | 30.9% | 25 | 24.5% | 0.74 |
| Live alone | 77 | 21.3% | 53 | 20.5% | 24 | 23.5% | |
| Live with partner | 22 | 6.1% | 15 | 5.8% | 7 | 6.9% | |
| Roommates | 43 | 11.9% | 32 | 12.4% | 11 | 10.8% | |
| Others | 114 | 31.6% | 79 | 30.5% | 35 | 34.3% | |
| Sexual orientation | |||||||
| Gay | 202 | 56.0% | 147 | 56.8% | 55 | 53.9% | 0.46 |
| Bisexual | 106 | 29.4% | 72 | 27.8% | 34 | 33.3% | |
| Straight | 24 | 6.6% | 20 | 7.7% | 4 | 3.9% | |
| Other or not reported | 29 | 8% | 20 | 7.7% | 9 | 8.8% | |
| Previous sexual partnersc | |||||||
| Cisgender men | 337 | 93.4% | 250 | 96.5% | 87 | 85.3% | <0.001 |
| Cisgender women | 169 | 46.8% | 132 | 51.0% | 37 | 36.3% | 0.01 |
| Transgender women | 72 | 19.9% | 54 | 20.8% | 18 | 17.6% | 0.49 |
| Current relationship status | |||||||
| Not in a relationship | 231 | 64.0% | 163 | 62.9% | 68 | 66.7% | 0.41 |
| Relationship with a man | 106 | 29.4% | 77 | 29.7% | 29 | 28.4% | |
| Relationship with a woman d | 20 | 5.5% | 17 | 6.6% | 3 | 2.9% | |
| Relationship with multiple partners | 4 | 1.1% | 2 | 0.8% | 2 | 2.0% | |
| Total | Chicago | Deep South | |||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | p-diff a | |
| Total participants | 361 | 259 | 102 | ||||
| HIV status | |||||||
| Unknown | 9 | 2.5% | 7 | 2.7% | 2 | 2.0% | 0.82 |
| HIV negative | 229 | 63.4% | 162 | 62.5% | 67 | 65.7% | |
| HIV positive | 123 | 34.1% | 90 | 34.7% | 33 | 32.4% | |
| HIV testingb,c | |||||||
| No test | 52 | 21.8% | 39 | 23.1% | 13 | 18.8% | 0.70 |
| One or two times | 54 | 22.7% | 39 | 23.1% | 15 | 21.7% | |
| Three or more times | 132 | 55.5% | 91 | 53.8% | 41 | 59.4% | |
| HIV pre-exposure prophylaxisc | |||||||
| Never taken | 150 | 63.0% | 105 | 62.1% | 45 | 65.2% | 0.37 |
| Previously taken | 32 | 13.4% | 26 | 15.4% | 6 | 8.7% | |
| Currently taking | 56 | 23.5% | 38 | 22.5% | 18 | 26.1% | |
| HIV treatmentd | |||||||
| Never taken | 5 | 4.1% | 2 | 2.2% | 3 | 9.1% | 0.07 |
| Previously taken | 7 | 5.7% | 7 | 7.8% | 0 | 0.0% | |
| Currently taking | 111 | 90.2% | 81 | 90.0% | 30 | 90.9% | |
| HIV treatment adherencee | |||||||
| Always/almost always take medication | 59 | 48.0% | 40 | 49.4% | 19 | 63.3% | 0.03 |
| Sometimes forget to take medication | 35 | 28.5% | 31 | 38.3% | 4 | 13.3% | |
| Often forget to take medication | 17 | 13.8% | 10 | 12.3% | 7 | 23.3% | |
| Recent condom usef,g | |||||||
| Consistent condom use | 81 | 24.5% | 55 | 22.9% | 26 | 28.9% | 0.26 |
| Inconsistent condom use | 249 | 75.5% | 185 | 77.1% | 64 | 71.1% | |
| Sex work or transactional sexf | |||||||
| Paid someone for sex (client) | 29 | 8.0% | 10 | 3.9% | 19 | 18.6% | <0.001 |
| Recently paid for sex (worker) | 61 | 16.9% | 40 | 15.4% | 21 | 20.6% | 0.37 |
| Previously paid for sex (worker) | 33 | 9.1% | 26 | 10.0% | 7 | 6.9% | |
| Never paid for sex (worker) | 267 | 74.0% | 193 | 74.5% | 74 | 72.5% | |
| Group sex participationf | |||||||
| No previous group sex | 197 | 54.6% | 140 | 54.1% | 57 | 55.9% | 0.68 |
| Recent group sex | 96 | 26.6% | 72 | 27.8% | 24 | 23.5% | |
| Previous groups sex | 68 | 18.8% | 47 | 18.1% | 21 | 20.6% | |
| Age of first sexual experience (M; SD) | 3–31 (14.9; 4.0) | 3–26 (14.6; 3.6) | 4–31 (15.6; 4.7) | 0.02 | |||
| Total | Chicago | Deep South | |||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | p-diff a | |
| Total participants | 361 | 259 | 102 | ||||
| Connections in home neighborhood | |||||||
| No family, no friends | 79 | 21.9% | 55 | 21.2% | 24 | 23.5% | 0.21 |
| Some family, no friends | 33 | 9.1% | 23 | 8.9% | 10 | 9.8% | |
| No family, some friends | 109 | 30.2% | 72 | 27.8% | 37 | 36.3% | |
| Some friends, some family | 140 | 38.8% | 109 | 42.1% | 31 | 30.4% | |
| Important neighborhood featuresb | |||||||
| Reasonable cost | 281 | 77.8% | 202 | 78.0% | 79 | 77.5% | 0.91 |
| Quiet | 184 | 51.0% | 130 | 50.2% | 54 | 52.9% | 0.64 |
| Access to downtown area | 146 | 40.4% | 108 | 41.7% | 38 | 37.3% | 0.44 |
| Near family and friends | 109 | 30.2% | 76 | 29.3% | 33 | 32.4% | 0.58 |
| Mostly Black | 52 | 14.4% | 34 | 13.1% | 18 | 17.6% | 0.27 |
| Mostly White | 34 | 9.4% | 24 | 9.3% | 10 | 9.8% | 0.88 |
| Mostly gay | 47 | 13.0% | 32 | 12.4% | 15 | 14.7% | 0.55 |
| Current neighborhood problemsc | |||||||
| Litter, trash | 263 | 72.9% | 200 | 77.2% | 63 | 61.8% | 0.003 |
| Drug dealing | 252 | 69.8% | 189 | 73.0% | 63 | 61.8% | 0.04 |
| Adults and teenagers on the street | 220 | 60.9% | 173 | 66.8% | 47 | 46.1% | 0.001 |
| Empty/abandoned houses | 237 | 65.7% | 177 | 68.3% | 60 | 58.8% | 0.09 |
| Police harassment/abuse | 241 | 66.8% | 185 | 71.4% | 56 | 54.9% | 0.003 |
| Lack of police presence/response | 235 | 65.1% | 176 | 68.0% | 59 | 57.8% | 0.07 |
| Social group disagreements | 218 | 60.4% | 164 | 63.3% | 54 | 52.9% | 0.07 |
| Graffiti | 186 | 51.5% | 143 | 55.2% | 43 | 42.2% | 0.02 |
| Neighborhood perceptionsd | |||||||
| Neighborhood has good reputation | 108 | 29.9% | 64 | 24.7% | 44 | 43.1% | <0.001 |
| Residents viewed negatively by others | 151 | 41.8% | 117 | 45.2% | 34 | 33.3% | 0.04 |
| Neighborhood is safe | 93 | 25.8% | 55 | 21.2% | 38 | 37.3% | 0.00 |
| Recent negative eventse | |||||||
| Fight with a weapon | 210 | 58.2% | 166 | 64.1% | 44 | 43.1% | <0.001 |
| Someone was jumped or robbed | 189 | 52.4% | 162 | 62.5% | 27 | 26.5% | 0.007 |
| Robbed, or property damaged | 95 | 26.3% | 69 | 26.6% | 26 | 25.5% | 0.82 |
| Networks | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Confidants (Social Network) | Sex Partners (Sexual Network) | |||||||||
| Chicago | Deep South | Chicago | Deep South | |||||||
| n | % | n | % | p-diff a | n | % | n | % | p-diff a | |
| 608 | 328 | 587 | 123 | |||||||
| Age | ||||||||||
| <20 years old | 20 | 3.3% | 5 | 1.5% | <0.001 | 25 | 4.3% | 1 | 0.8% | <0.001 |
| 20–29 years old | 340 | 56% | 141 | 42.9% | 379 | 62% | 53 | 40.1% | ||
| ≥30 years old | 247 | 40.1% | 180 | 54.9% | 176 | 28.9% | 69 | 56.1% | ||
| Not known/refused/missing | 1 | 0.2% | 2 | 0.6% | 7 | 12.4% | 0 | 0.0% | ||
| Education | ||||||||||
| High school or less | 273 | 44.9% | 112 | 27.8% | 0.19 | 273 | 46.5% | 35 | 28.5% | 0.006 |
| Above high school | 238 | 39.1% | 120 | 29.8% | 148 | 25.2% | 38 | 30.9% | ||
| Not known/refused/missing | 97 | 16.0% | 96 | 29.3% | 166 | 28.3% | 50 | 40.7% | ||
| Employment status | ||||||||||
| Employed full-time or part-time | 428 | 71.3% | 214 | 65.2% | 0.027 | 375 | 63.9% | 65 | 52.9% | 0.002 |
| Unemployed | 166 | 27.7% | 73 | 23.2% | 149 | 25.4% | 21 | 17.1% | ||
| Retired | 8 | 1.32% | 12 | 3.7% | 0 | 0.0% | 2 | 1.6% | ||
| Not known/refused/missing | 6 | 1.0% | 26 | 7.9% | 63 | 10.7% | 35 | 28.5% | ||
| Gender | ||||||||||
| Cisgender man | 331 | 54.4% | 200 | 61.0% | 0.022 | 523 | 89.1% | 93 | 75.6% | 0.001 |
| Cisgender woman | 225 | 37.0% | 106 | 32.3% | 45 | 7.7% | 20 | 16.3% | ||
| Transgender man/woman | 52 | 8.6% | 15 | 4.6% | 19 | 3.2% | 8 | 6.5% | ||
| Not known/refused/missing | 0 | 0.0% | 7 | 2.1% | 0 | 0.0% | 2 | 1.6% | ||
| Sexual partner typeb | ||||||||||
| Main partners | 68 | 11.2% | 26 | 52.0% | 154 | 26.2% | 26 | 21.1% | 0.92 | |
| Causal partners | 11 | 1.8% | 20 | 40.0% | 399 | 68.0% | 62 | 50.4% | ||
| Sex work/exchange partners | 1 | 0.2% | 4 | 8.0% | 28 | 4.8% | 5 | 4.1% | ||
| Not known/refused/missing | -- c | -- c | -- c | -- c | 6 | 1.0% | 30 | 24.4% | ||
| HIV status | ||||||||||
| HIV positive | 107 | 17.6% | 16 | 4.9% | <0.001 | 72 | 15.3% | 4 | 3.3% | 0.002 |
| HIV negative | 453 | 74.5% | 173 | 52.7% | 318 | 54.6% | 79 | 64.2% | ||
| Not known/refused/missing | 48 | 7.9% | 139 | 42.4% | 197 | 33.5% | 40 | 32.5% | ||
| Criminal justice involvement | ||||||||||
| Ever incarcerated | 149 | 24.5% | 71 | 21.7% | 0.87 | 137 | 27.6% | 22 | 17.9% | 0.89 |
| Never incarcerated | 435 | 71.6% | 213 | 64.9% | 360 | 61.3% | 60 | 48.8% | ||
| Not known/refused/missing | 24 | 4.0% | 44 | 13.4% | 90 | 15.3% | 41 | 33.3% | ||
| Group sex | ||||||||||
| Ever had group sex | 128 | 21.1% | 40 | 12.2% | 0.41 | 149 | 42.5% | 15 | 12.2% | 0.004 |
| No previous group sex | 361 | 59.4% | 134 | 40.9% | 202 | 29.5% | 49 | 39.8% | ||
| Not known/refused/missing | 119 | 19.6% | 154 | 47.0% | 234 | 40.0% | 59 | 48.0% | ||
| Sex drug use | ||||||||||
| Ever used drugs during sex | 169 | 39.3% | 0 | 0.0% | <0.00 | 229 | 53.4% | 22 | 17.9% | 0.005 |
| Never used drugs during sex | 261 | 60.7% | 77 | 23.5% | 200 | 46.5% | 42 | 34.2% | ||
| Not known/refused/missing | 178 | 29.3% | 251 | 76.5% | 158 | 26.9% | 59 | 48.0% | ||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Duncan, D.T.; Hickson, D.A.; Goedel, W.C.; Callander, D.; Brooks, B.; Chen, Y.-T.; Hanson, H.; Eavou, R.; Khanna, A.S.; Chaix, B.; et al. The Social Context of HIV Prevention and Care among Black Men Who Have Sex with Men in Three U.S. Cities: The Neighborhoods and Networks (N2) Cohort Study. Int. J. Environ. Res. Public Health 2019, 16, 1922. https://doi.org/10.3390/ijerph16111922
Duncan DT, Hickson DA, Goedel WC, Callander D, Brooks B, Chen Y-T, Hanson H, Eavou R, Khanna AS, Chaix B, et al. The Social Context of HIV Prevention and Care among Black Men Who Have Sex with Men in Three U.S. Cities: The Neighborhoods and Networks (N2) Cohort Study. International Journal of Environmental Research and Public Health. 2019; 16(11):1922. https://doi.org/10.3390/ijerph16111922
Chicago/Turabian StyleDuncan, Dustin T., DeMarc A. Hickson, William C. Goedel, Denton Callander, Brandon Brooks, Yen-Tyng Chen, Hillary Hanson, Rebecca Eavou, Aditya S. Khanna, Basile Chaix, and et al. 2019. "The Social Context of HIV Prevention and Care among Black Men Who Have Sex with Men in Three U.S. Cities: The Neighborhoods and Networks (N2) Cohort Study" International Journal of Environmental Research and Public Health 16, no. 11: 1922. https://doi.org/10.3390/ijerph16111922
APA StyleDuncan, D. T., Hickson, D. A., Goedel, W. C., Callander, D., Brooks, B., Chen, Y.-T., Hanson, H., Eavou, R., Khanna, A. S., Chaix, B., Regan, S. D., Wheeler, D. P., Mayer, K. H., Safren, S. A., Carr Melvin, S., Draper, C., Magee-Jackson, V., Brewer, R., & Schneider, J. A. (2019). The Social Context of HIV Prevention and Care among Black Men Who Have Sex with Men in Three U.S. Cities: The Neighborhoods and Networks (N2) Cohort Study. International Journal of Environmental Research and Public Health, 16(11), 1922. https://doi.org/10.3390/ijerph16111922






