Changes in Work Practices for Safe Use of Formaldehyde in a University-Based Anatomy Teaching and Research Facility
Abstract
1. Introduction
2. Materials and Methods
2.1. Building and Facilities
2.2. Ventilation System and Air Exchange Rate
2.3. Stationary Air Sampling
2.4. Full Shift Personal Air Sampling
2.5. Task-Based Personal Air Sampling
2.6. FA Air Sampling and Analysis
2.7. Improved Work Practices
2.8. Calculations and Statistical Analysis
3. Results
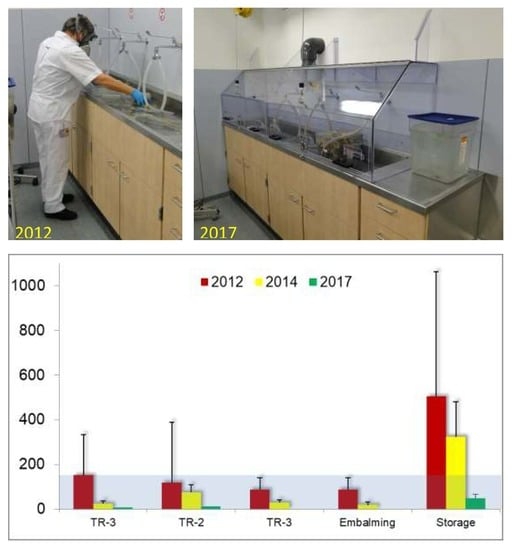
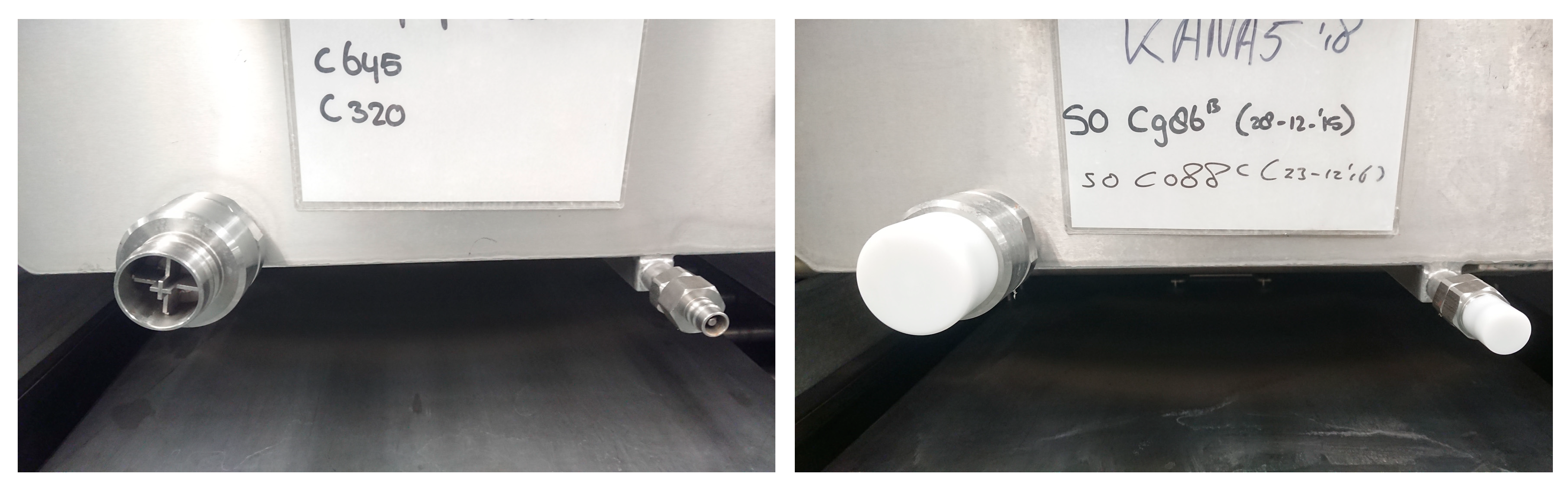
3.1. Infrastructure and Technology
3.2. Improved Work Practices
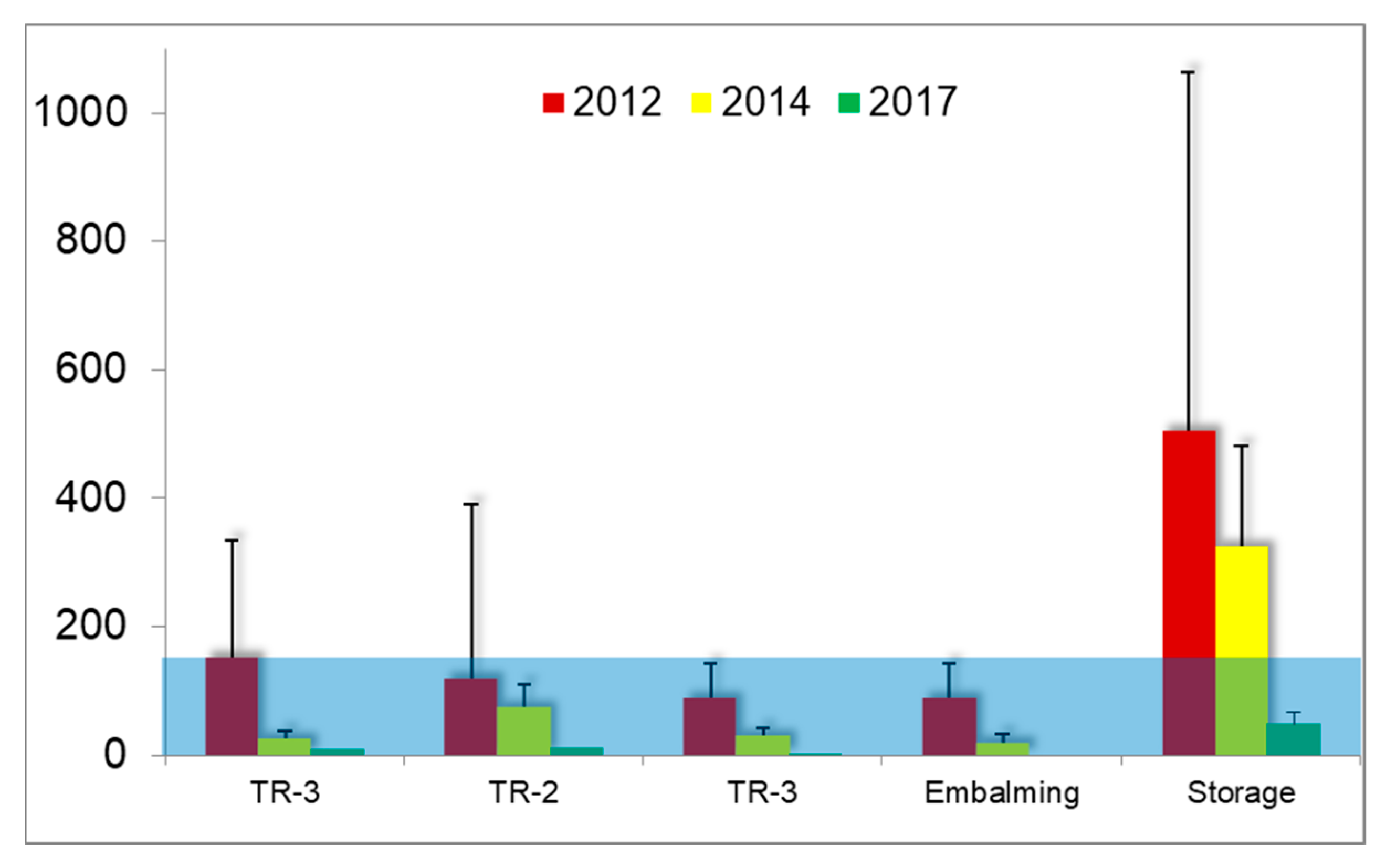
3.3. Measurements at Fixed Locations
3.4. Full Shift Personal Air Sampling
3.5. Task-Based Personal Air Sampling
4. Discussion
4.1. Air Sampling at Fixed Locations
4.2. Personal Air Sampling
4.3. Strengths and Limitations of the Study
4.4. Interpretation of Results in the Context of Published Literature
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Skisak, C.M. Formaldehyde vapor exposures in anatomy laboratories. Am. Ind. Hyg. Assoc. J. 1983, 44, 948–950. [Google Scholar] [CrossRef] [PubMed]
- Perkins, J.L.; Kimbrough, J.D. Formaldehyde exposure in a gross anatomy laboratory. J. Occup. Med. 1985, 27, 813–815. [Google Scholar] [CrossRef] [PubMed]
- Onyije, F.M.; Avwioro, O.G. Excruciating effect of formaldehyde exposure to students in gross anatomy dissection laboratory. Int. J. Occup. Environ. Med. 2012, 3, 92–95. [Google Scholar] [PubMed]
- Vimercati, L.; Carrus, A.; Martino, T.; Galise, I.; Minunni, V.; Caputo, F.; Dell’Erba, A.; Assennato, G. Formaldehyde exposure and irritative effects on medical examiners, pathologic anatomy post-graduate students and technicians. Iran. J. Public Health 2010, 39, 26–34. [Google Scholar] [PubMed]
- Triebig, G.; Schaller, K.H.; Beyer, B.; Müller, J.; Valentin, H. Formaldehyde exposure at various workplaces. Sci. Total Environ. 1989, 79, 191–195. [Google Scholar] [CrossRef]
- Flyvholm, M.A.; Menné, T. Allergic contact dermatitis from FA. A case study focusing on sources of formaldehyde exposure. Contact Dermat. 1992, 27, 27–36. [Google Scholar] [CrossRef]
- Friis, U.F.; Dahlin, J.; Bruze, M.; Menné, T.; Johansen, J.D. Hidden exposure to formaldehyde in a swab caused allergic contact dermatitis. Contact Dermat. 2014, 70, 258–260. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, G.D.; Larsen, S.T.; Wolkoff, P. Re-evaluation of the WHO (2010) formaldehyde indoor air quality guideline for cancer risk assessment. Arch. Toxicol. 2017, 91, 35–61. [Google Scholar] [CrossRef] [PubMed]
- IARC. Chemical agents and related occupations. In IARC Monographs on the Evaluation of Carcinogenic Risks to Humans; International Agency for Research on Cancer: Lyon, France, 2012. [Google Scholar]
- Hauptmann, M.; Stewart, P.A.; Lubin, J.H.; Beane Freeman, L.E.; Hornung, R.W.; Herrick, R.F.; Hoover, R.N.; Fraumeni, J.F., Jr.; Blair, A.; Hayes, R.B. Mortality from lymphohematopoietic malignancies and brain cancer among embalmers exposed to formaldehyde. J. Natl. Cancer Inst. 2009, 101, 1696–1708. [Google Scholar] [CrossRef] [PubMed]
- Kwon, S.C.; Kim, I.; Song, J.; Park, J. Does Formaldehyde have a causal association with nasopharyngeal cancer and leukaemia? Ann. Occup. Environ. Med. 2018, 30, 5. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Tang, X.; Rothman, N.; Vermeulen, R.; Ji, Z.; Shen, M.; Qiu, C.; Guo, W.; Liu, S.; Reiss, B.; et al. Occupational exposure to formaldehyde, hematotoxicity, and leukemia-specific chromosome changes in cultured myeloid progenitor cells. Cancer Epidemiol. Prev. Biomark. 2010, 19, 80–88. [Google Scholar] [CrossRef] [PubMed]
- Gentry, P.R.; Rodricks, J.V.; Turnbull, D.; Bachand, A.; Van Landingham, C.; Shipp, A.M.; Albertini, R.J.; Irons, R. Formaldehyde exposure and leukemia: Critical review and reevaluation of the results from a study that is the focus for evidence of biological plausibility. Crit. Rev. Toxicol. 2013, 43, 661–670. [Google Scholar] [CrossRef] [PubMed]
- Bono, R.; Romanazzi, V.; Munnia, A.; Piro, S.; Allione, A.; Ricceri, F.; Guarrera, S.; Pignata, C.; Matullo, G.; Wang, P.; et al. Malondialdehyde-deoxyguanosine adduct formation in workers of pathology wards: The role of air FA exposure. Chem. Res. Toxicol. 2010, 23, 1342–1348. [Google Scholar] [CrossRef] [PubMed]
- Musak, L.; Smerhovsky, Z.; Halasova, E.; Osina, O.; Letkova, L.; Vodickova, L.; Polakova, V.; Buchancova, J.; Hemminki, K.; Vodicka, P. Chromosomal damage among medical staff occupationally exposed to volatile anesthetics, antineoplastic drugs, and formaldehyde. Scand. J. Work Environ. Health 2013, 39, 618–630. [Google Scholar] [CrossRef] [PubMed]
- Costa, S.; Carvalho, S.; Costa, C.; Coelho, P.; Silva, S.; Santos, L.S.; Gaspar, J.F.; Porto, B.; Laffon, B.; Teixeira, J.P. Increased levels of chromosomal aberrations and DNA damage in a group of workers exposed to formaldehyde. Mutagenesis 2015, 30, 463–473. [Google Scholar] [CrossRef] [PubMed]
- Duong, A.; Steinmaus, C.; McHale, C.M.; Vaughan, C.P.; Zhang, L. Reproductive and developmental toxicity of Formaldehyde: A systematic review. Mutat. Res. 2011, 728, 118–138. [Google Scholar] [CrossRef] [PubMed]
- Haffner, M.J.; Oakes, P.; Demerdash, A.; Yammine, K.C.; Watanabe, K.; Loukas, M.; Tubbs, R.S. Formaldehyde exposure and its effects during pregnancy: Recommendations for laboratory attendance based on available data. Clin. Anat. 2015, 28, 972–979. [Google Scholar] [CrossRef] [PubMed]
- Maroziene, L.; Grazuleviciene, R. Maternal exposure to low-level air pollution and pregnancy outcomes: A population-based study. Environ. Health 2002, 1, 6. [Google Scholar] [CrossRef] [PubMed]
- Scheepers, P.T.; Van Wel, L.; Beckmann, G.; Anzion, R. Chemical characterization of the indoor air quality of a university hospital: Penetration of outdoor air pollutants. Int. J. Environ. Res. Public Health 2017, 14, 497. [Google Scholar] [CrossRef] [PubMed]
- Scheepers, P.T.; Van Hout, S. Health-related indicators of indoor air quality. In Environmental Indicators; Armon, R., Hänninen, O., Eds.; Springer: Berlin, Germany, 2015; pp. 925–944. [Google Scholar]
- Scheepers, P.T.; Beckmann, G.; Van Hout, S.; Van Der Kroon, E.; Leenders, P. Determination of the filter capture efficiency for safe use of fixative solutions in the biological glove box of the International Space Station. Environ. Technol. Innov. 2015, 3, 86–96. [Google Scholar] [CrossRef]
- Norppa, H.; Bonassi, S.; Hansteen, I.L.; Hagmar, L.; Strömberg, U.; Rössner, P.; Boffetta, P.; Lindholm, C.; Gundy, S.; Lazutka, J.; et al. Chromosomal aberrations and SCEs as biomarkers of cancer risk. Mutat. Res. 2006, 600, 37–45. [Google Scholar] [CrossRef] [PubMed]
- Lorenzoni, D.C.; Pinheiro, L.P.; Nascimento, H.S.; Menegardo, C.S.; Silva, R.G.; Bautz, W.G.; Henriques, J.F.; Almeida-Coburn, K.L.; da Gama-de-Souza, L.N. Could formaldehyde induce mutagenic and cytotoxic effects in buccal epithelial cells during anatomy classes? Med. Oral Patol. Oral Cir. Bucal 2017, 22, 58–63. [Google Scholar] [CrossRef]
- Salthammer, T. Critical evaluation of approaches in setting indoor air quality guidelines and reference values. Chemosphere 2011, 82, 1507–1517. [Google Scholar] [CrossRef] [PubMed]
- Saowakon, N.; Ngernsoungnern, P.; Watcharavitoon, P.; Ngernsoungnern, A.; Kosanlavit, R. Formaldehyde exposure in gross anatomy laboratory of Suranaree University of Technology: A comparison of area and personal sampling. Environ. Sci. Pollut. Res. 2015, 22, 19002–19012. [Google Scholar] [CrossRef] [PubMed]
- Higashikubo, I.; Miyauchi, H.; Yoshida, S.; Tanaka, S.; Matsuoka, M.; Arito, H.; Araki, A.; Shimizu, H.; Sakurai, H. Assessment of workplace air concentrations of formaldehyde during and before working hours in medical facilities. Ind. Health 2017, 55, 192–198. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Guidelines for Indoor Air Quality: Selected Compounds; The WHO European Centre for Environment and Health: Bonn, Germany, 2009. [Google Scholar]
- Coleman, R.; Kogan, I. An improved low-formaldehyde embalming fluid to preserve cadavers for anatomy teaching. J. Anat. 1998, 192, 443–446. [Google Scholar] [CrossRef] [PubMed]
- Ohmichi, K.; Komiyama, M.; Matsuno, Y.; Takanashi, Y.; Miyamoto, H.; Kadota, T.; Maekawa, M.; Toyama, Y.; Tatsugi, Y.; Kohno, T.; et al. Formaldehyde exposure in a gross anatomy laboratory—Personal exposure level is higher than indoor concentration. Environ. Sci. Pollut. Res. 2006, 13, 120–124. [Google Scholar] [CrossRef]
- Klein, R.C.; King, C.; Castagna, P. Controlling Formaldehyde exposures in an academic gross anatomy laboratory. J. Occup. Environ. Hyg. 2014, 11, 127–132. [Google Scholar] [CrossRef] [PubMed]
- Scarselli, A.; Corfiati, M.; Di Marzio, D.; Iavicoli, S. National estimates of exposure to formaldehyde in italian workplaces. Ann. Work Expo. Health 2017, 61, 33–43. [Google Scholar] [PubMed]
- Xu, W.; Stewart, E.J. A comparison of engineering controls for formaldehyde exposure during grossing activities in health care anatomic pathology laboratories. J. Occup. Environ. Hyg. 2016, 13, 529–537. [Google Scholar] [CrossRef] [PubMed]
- Keil, C.B.; Akbar-Khanzadeh, F.; Konecny, K.A. Characterizing Formaldehyde emission rates in a gross anatomy laboratory. Appl. Occup. Environ. Hyg. 2001, 16, 967–972. [Google Scholar] [CrossRef] [PubMed]
- Gressel, M.G.; Hughes, R.T. Effective local exhaust ventilation for controlling formaldehyde exposures during embalming. Appl. Occup. Environ. Hyg. 1992, 7, 840–845. [Google Scholar] [CrossRef]
- Yamato, H.; Nakashima, T.; Kikuta, A.; Kunugita, N.; Arashidani, K.; Nagafuchi, Y.; Tanaka, I. A novel local ventilation system to reduce the levels of formaldehyde exposure during a gross anatomy dissection course and its evaluation using real-time monitoring. J. Occup. Health 2005, 47, 450–453. [Google Scholar] [CrossRef] [PubMed]
- Kikuta, A.; Yamato, H.; Kunugita, N.; Nakashima, T.; Hayashi, H. Reducing the levels of formaldehyde exposure during a gross anatomy dissection course with a local ventilation system. Kaibogaku Zasshi 2010, 85, 17–27. [Google Scholar] [PubMed]
- Dahncke, M.; Hohenberger, L.; Klusmann, H.; Stockmann, R.; Thiel, P.; Thullner, I. Formaldehyde in preclinical medical training (anatomy)—Reduction of formaldehyde exposure during practical anatomical sessions: Technical ventilation measures. Gefahrst. Reinhalt. Luft 2016, 76, 387–397. [Google Scholar]
- Takahashi, M.; Abe, M.; Yamagishi, T.; Nakatani, K.; Okade, T.; Ogawa, T.; Konishi, H.; Kiryu-Seo, S.; Kiyama, H.; Nakajima, Y. Local ventilation system successfully reduced FA exposure during gross anatomy dissection classes. Anat. Sci. Int. 2010, 85, 251–252. [Google Scholar] [CrossRef] [PubMed]
- Vohra, M.S. Personal formaldehyde exposure level in the gross anatomy dissecting room at College of Medicine King Saud University Riyadh. Int. J. Occup. Med. Environ. Health 2011, 24, 108–113. [Google Scholar] [CrossRef] [PubMed]
- Lakchayapakorn, K.; Watchalayarn, P. Formaldehyde exposure of medical students and instructors and clinical symptoms during gross anatomy laboratory in Thammasat University. J. Med. Assoc. Thai 2010, 93, S92–S98. [Google Scholar] [PubMed]
- Kwak, M.H.; Kim, J.E.; Go, J.; Koh, E.K.; Song, S.H.; Sung, J.E.; Yang, S.Y.; An, B.S.; Jung, Y.J.; Lee, J.H.; et al. Characterization of allergic response induced by repeated dermal exposure of IL-4/Luc/CNS-1 transgenic mice to low dose formaldehyde. Lab. Anim. Res. 2014, 30, 95–103. [Google Scholar] [CrossRef] [PubMed]
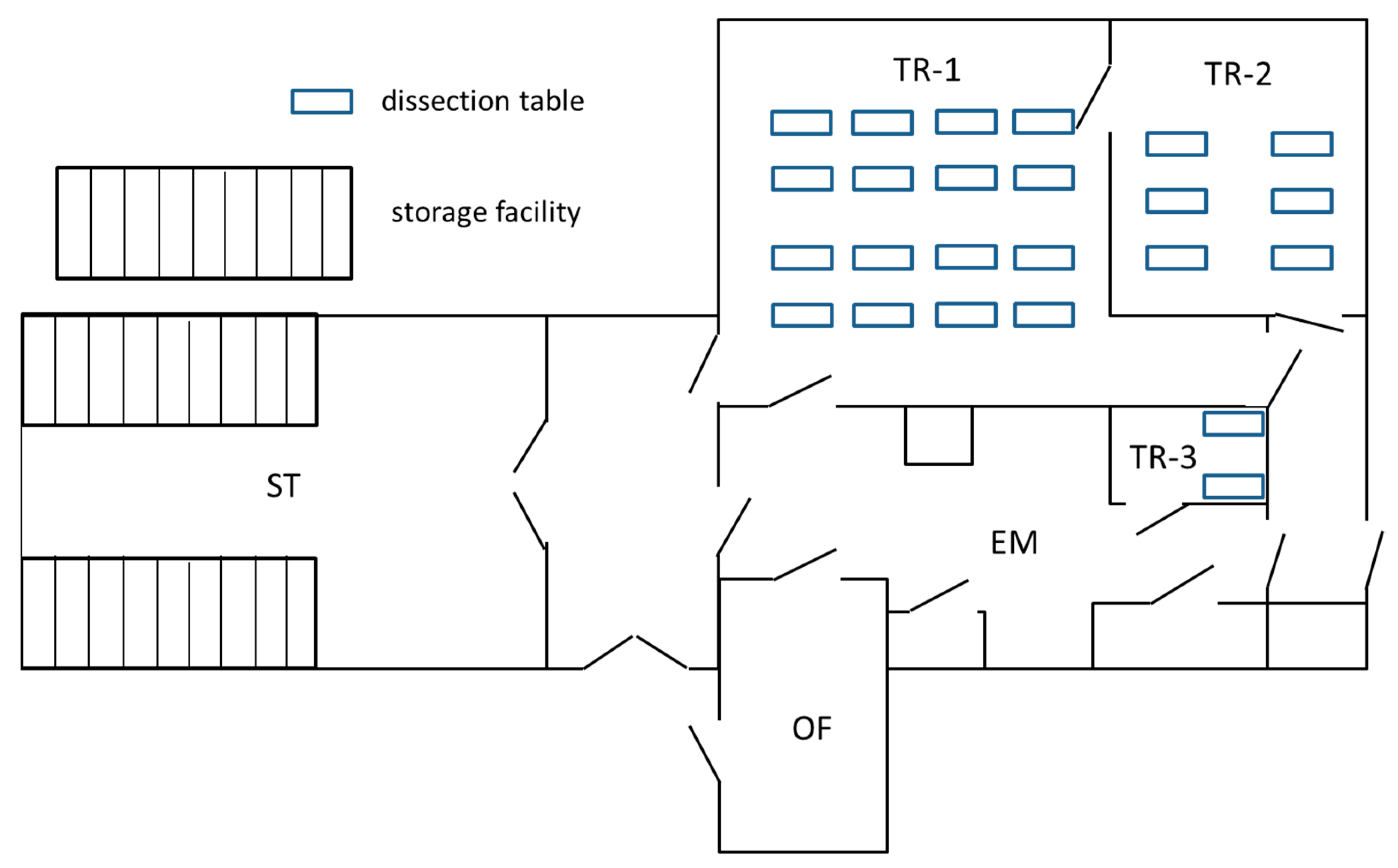







| Room | Size (m2) | Function | Facilities | Air Exchange Rate (h−1) | Air Exchange Per Section Table (h−1) | ||
|---|---|---|---|---|---|---|---|
| Design | Effective a | Design | Effective a | ||||
| Storage | 164 | Storage of cadavers and specimens | Storage of human remains in 75 tanks with lifting equipment and 37% FA stock | 6.1 | 6.3 | - c | - c |
| Embalming | 89 | Tap water flushing | Work bench with water taps | 8.8 | 9.0 | - c | - |
| TR-1 | 199 | Instruction | 16 dissection tables | 15.3 | 14.2 | 0.96 | 0.89 |
| TR-2 | 64 | Instruction | 6 dissection tables | 31.3 | 23.7 | 5.2 | 4.0 |
| TR-3 | 17 | Research projects | 2 dissection tables | 19.5 | 4.6 b | 9.8 | 2.3 b |
| Category | No. | Description | Old Work Practice | New Work Practice | Rationale | Location/Room | Figure No. |
|---|---|---|---|---|---|---|---|
| Technical | T-1 | Leak prevention | Leaking of formalin by dripping of residual fluid from the tap of a storage tank | Placing a cap on the open connector to prevent leakage from taps of storage tanks | Leak reduction | Storage | 2 |
| T-2 | Elimination of disposable absorbent sheets | Specimens were placed on a disposable sheet to collect residual formalin draining from the specimens | Elimination of the disposable sheet and collection of residual formalin leakage in a closed container | Reduction of evaporation surface | Teaching | 3 | |
| T-3 | Introduction of local exhaust ventilation (LEV) | Specimens are rinsed with water to remove residual formalin. For this a workbench was used with no LEV. | Placement of a Perspex containment with LEV. The containment can be opened for introduction or removal of specimens | Removal of vapors at the source | Embalming | 4 | |
| T-4 | Improvement of down flow ventilation (DFV) | Create a down flow at the location where specimens are lifted from the storage tank | Improvement of ventilation equipment capacity and performance | Reduction of vapors in breathing zone | Storage | 5 | |
| Organisation | O-1 | Optimizing storage system a | Specimens storage methods did not match with teaching programme requiring opening of many storage tanks to find the required preparation for a specific class/course | Storage of specimens needed for a specific class/course in one or a few labeled tanks to reduce on the number of tanks to be opened to retrieve the required specimens. | Reduction of the work amount | Storage | 6 |
| O-2 | Tap water flushes and reduction of exposure time | Overnight flushing of specimens by tap water | Extension of the flush time duration for specimens with a high formalin residue; reduction of the time that specimens are put on display on the dissection tables. | Removal of formalin | Embalming | 7 |
| Room | 2012 | 2014 | 2017 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| n | GM | Range | n | GM | Range | n | GM | Range | |
| TR-1 | 10 | 80.4 | 49–618.3 | 4 | 21.2 | 7.7–38.6 | 1 | 9.0 d | - d |
| TR-2 | 6 | 10.9 | 2.2–672.2 a | 4 | 69.8 | 50.3–124.6 | 1 | 13.0 d | - d |
| TR-3 | - b | - b | - b | 4 | 16.2 | 10.1–40.0 | 1 | 1.6 d | - d |
| Embalming | 10 | 74.7 | 37.3–169.9 | 4 | 27.4 | 16.7–41.7 | 0 | - d | - d |
| Storage | 10 | 290.9 | 89.7–1506.2 | 4 | 301.7 | 206.5–554.0 | 2 | 62.5, 34.9 b,d | - d |
| Year | Group | n | GM | P95 | Range | Non-Compliance (%) |
|---|---|---|---|---|---|---|
| 2012 | Workers | 21 | 123.0 | 407.9 | 17.2–519.7 | 42.8 |
| Students | 5 | 174.7 | 930.0 | 117.0–1120 | 60.0 | |
| Total | 26 | 131.6 | 491.7 | 17.2–1120 | 46.2 | |
| 2014 | Workers | 8 | 121.3 | 252.8 | 55.6–287.3 | 37.5 |
| Students | 5 | 102.8 | 405.6 | 49.6–468.9 | 40.0 | |
| Total | 13 | 113.6 | 359.9 | 49.6–468.9 | 38.5 | |
| 2017 | Workers | 6 | 26.5 | 61.9 | 10.6–71.8 | 0 |
| Students | 7 | 30.9 | 68.0 | 19.6–80.1 | 0 | |
| Total | 13 | 28.8 | 75.1 | 10.6–80.1 | 0 |
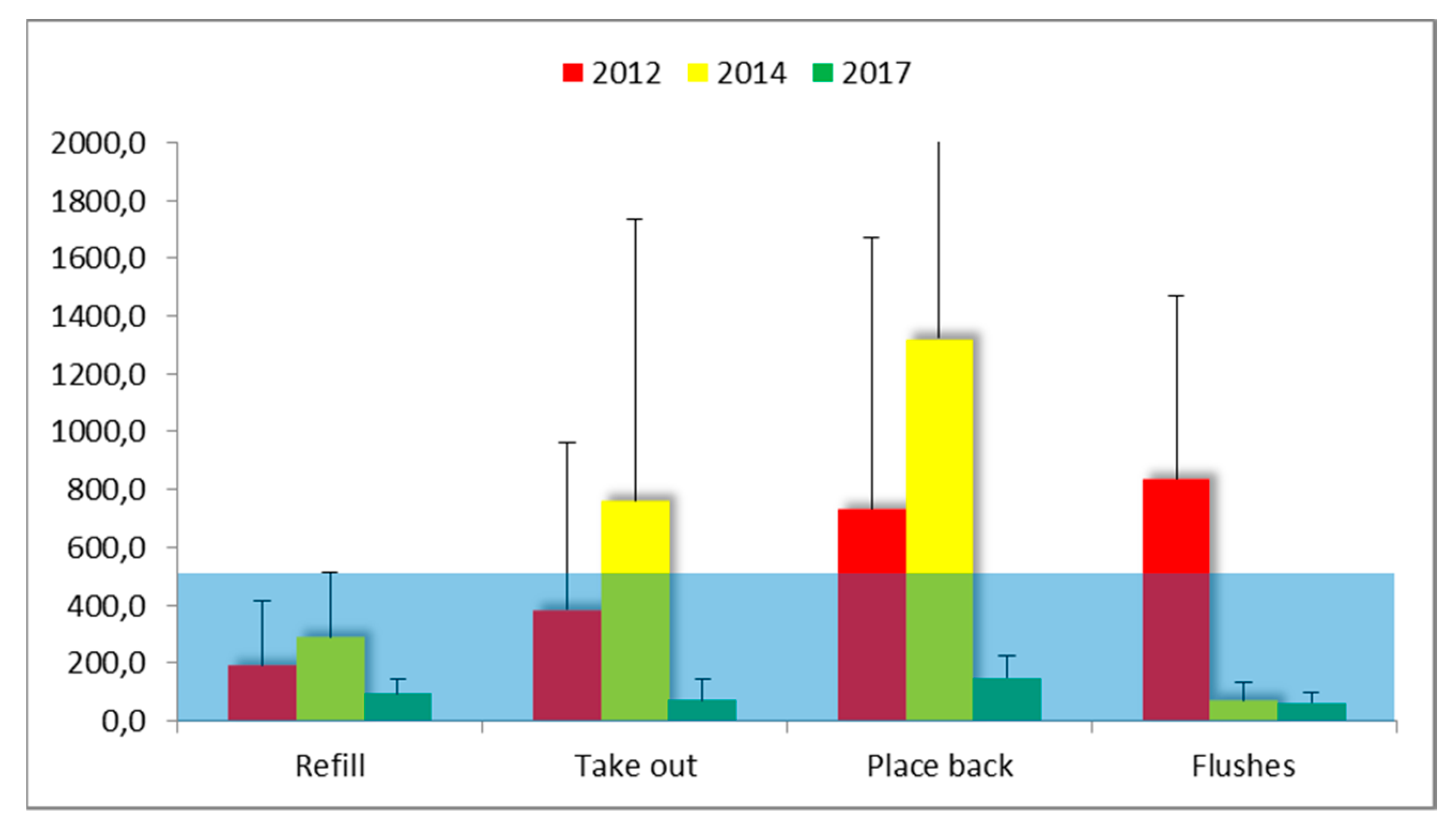
| Year | Description of Task | n | GM | P95 | Range | Non-Compliance (%) b |
|---|---|---|---|---|---|---|
| 2012 | Refill | 4 | 104.1 | 460.8 | 35.4–510.1 | 25.0 |
| Take out | 9 | 166.4 | 1423.9 | 58.6–1552.1 | 22.2 | |
| Place back | 3 | 345.6 | 1659.9 | 72.9–1809.6 | 33.3 | |
| Flushes | 3 | 588.3 | 1352.0 | 151.6–1395.3 | 66.7 | |
| Total | 19 | 276.5 | 1577.8 | 58.6–1552.1 | 31.6 | |
| 2014 | Refill | 9 | 224.5 | 641.4 | 88.2–646.3 | 22.2 |
| Take out | 6 | 418.0 | 2216.4 | 104.9–266.2 | 50.0 | |
| Place back | 3 | 947.6 | 2575.0 | 371.6–2769.2 a | 66.7 | |
| Flushes | 3 | 58.8 | 131.3 | 37.7–141.7 | 0.0 | |
| Total | 21 | 272.0 | 2666.2 | 37.7–2769.2 | 33.3 | |
| 2017 | Refill | 2 | - | - | 61.5–128.0 | 0.0 |
| Take out | 2 | - | - | 20.4–123.0 | 0.0 | |
| Place back | 3 | 134.6 | 212.6 | 68.2–218.0 | 0.0 | |
| Flushes | 3 | 54.4 | 100.5 | 35.8–107.0 | 0.0 | |
| Total | 12 | 77.5 | 193.7 | 20.4–218.0 | 0.0 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scheepers, P.T.J.; Graumans, M.H.F.; Beckmann, G.; Van Dael, M.; Anzion, R.B.M.; Melissen, M.; Pinckaers, N.; Van Wel, L.; De Werdt, L.M.A.; Gelsing, V.; et al. Changes in Work Practices for Safe Use of Formaldehyde in a University-Based Anatomy Teaching and Research Facility. Int. J. Environ. Res. Public Health 2018, 15, 2049. https://doi.org/10.3390/ijerph15092049
Scheepers PTJ, Graumans MHF, Beckmann G, Van Dael M, Anzion RBM, Melissen M, Pinckaers N, Van Wel L, De Werdt LMA, Gelsing V, et al. Changes in Work Practices for Safe Use of Formaldehyde in a University-Based Anatomy Teaching and Research Facility. International Journal of Environmental Research and Public Health. 2018; 15(9):2049. https://doi.org/10.3390/ijerph15092049
Chicago/Turabian StyleScheepers, Paul T. J., Martien H. F. Graumans, Gwendolyn Beckmann, Maurice Van Dael, Rob B. M. Anzion, Maarten Melissen, Nicole Pinckaers, Luuk Van Wel, Laurie M. A. De Werdt, Vera Gelsing, and et al. 2018. "Changes in Work Practices for Safe Use of Formaldehyde in a University-Based Anatomy Teaching and Research Facility" International Journal of Environmental Research and Public Health 15, no. 9: 2049. https://doi.org/10.3390/ijerph15092049
APA StyleScheepers, P. T. J., Graumans, M. H. F., Beckmann, G., Van Dael, M., Anzion, R. B. M., Melissen, M., Pinckaers, N., Van Wel, L., De Werdt, L. M. A., Gelsing, V., & Van Linge, A. (2018). Changes in Work Practices for Safe Use of Formaldehyde in a University-Based Anatomy Teaching and Research Facility. International Journal of Environmental Research and Public Health, 15(9), 2049. https://doi.org/10.3390/ijerph15092049