Geographical Accessibility of Community Health Assist Scheme General Practitioners for the Elderly Population in Singapore: A Case Study on the Elderly Living in Housing Development Board Flats
Abstract
1. Introduction
2. Methodological Considerations
3. Case Study
3.1. Background Information
3.2. Data Sources
3.2.1. Address Points
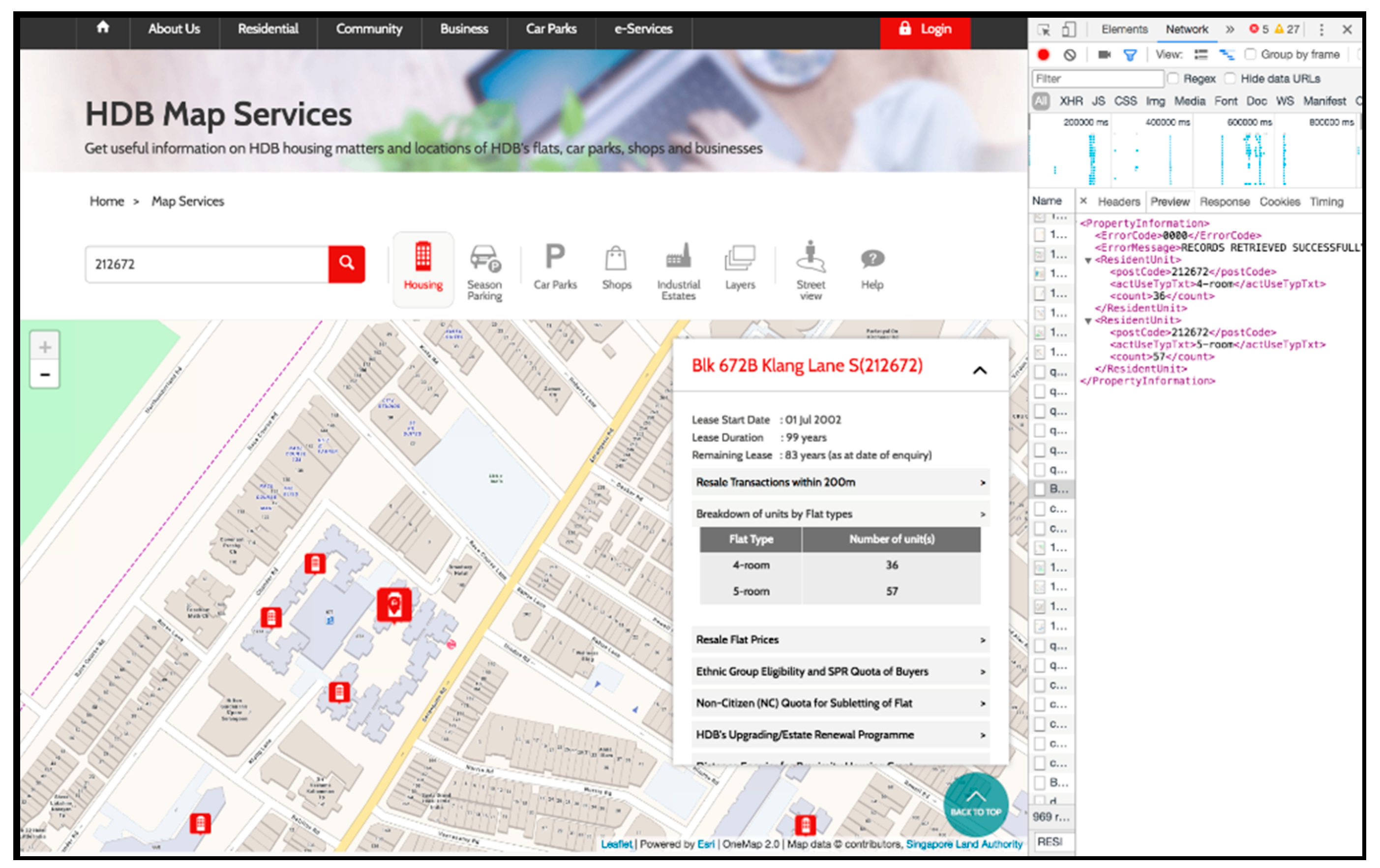
3.2.2. HDB Address Points with Flat Type Information
3.2.3. Masterplan 2014 Planning Area
3.3. Data Pre-Processing for Calculating Spatial Accessibility
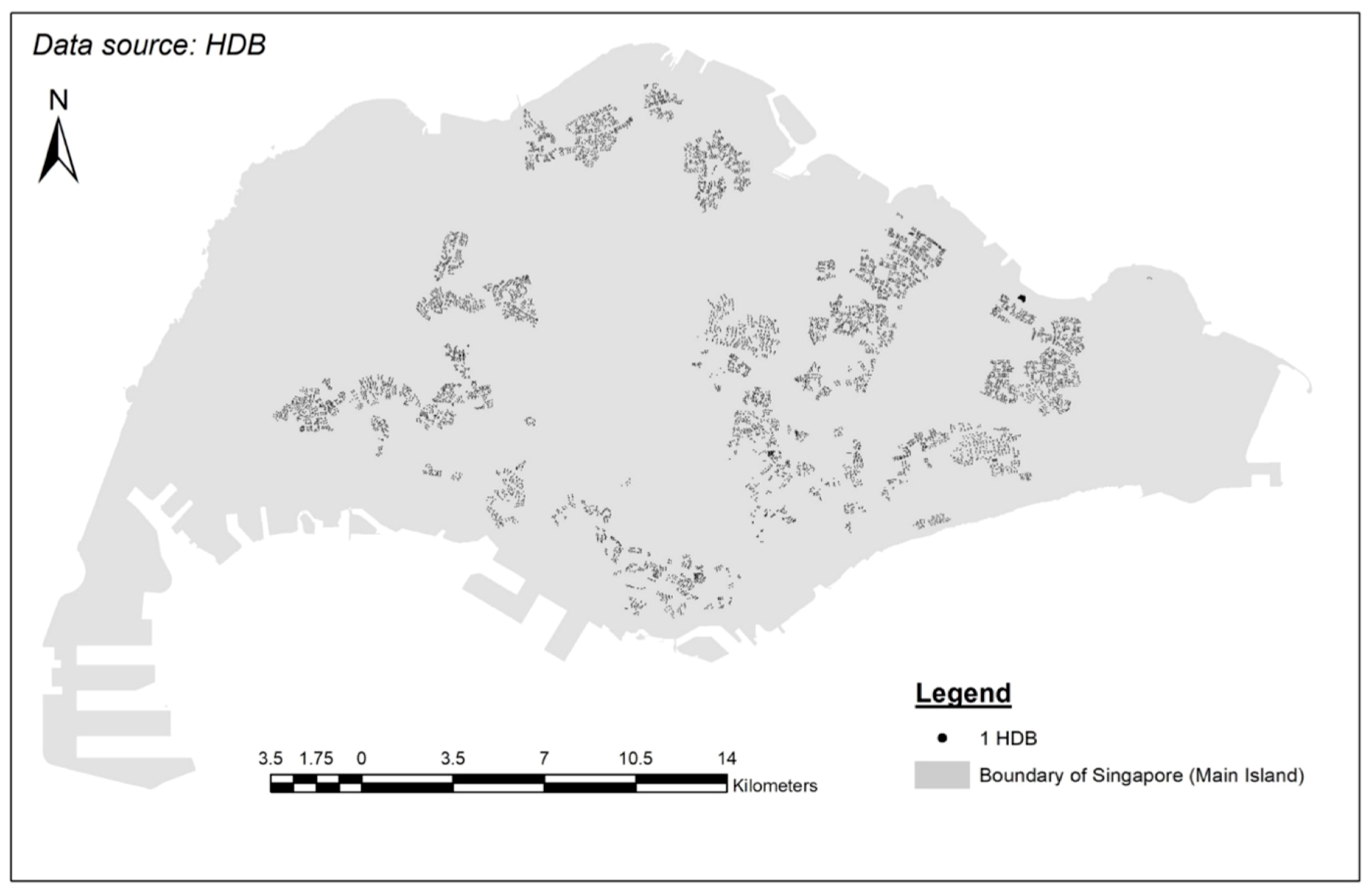
3.3.1. Location of HDBs in Singapore
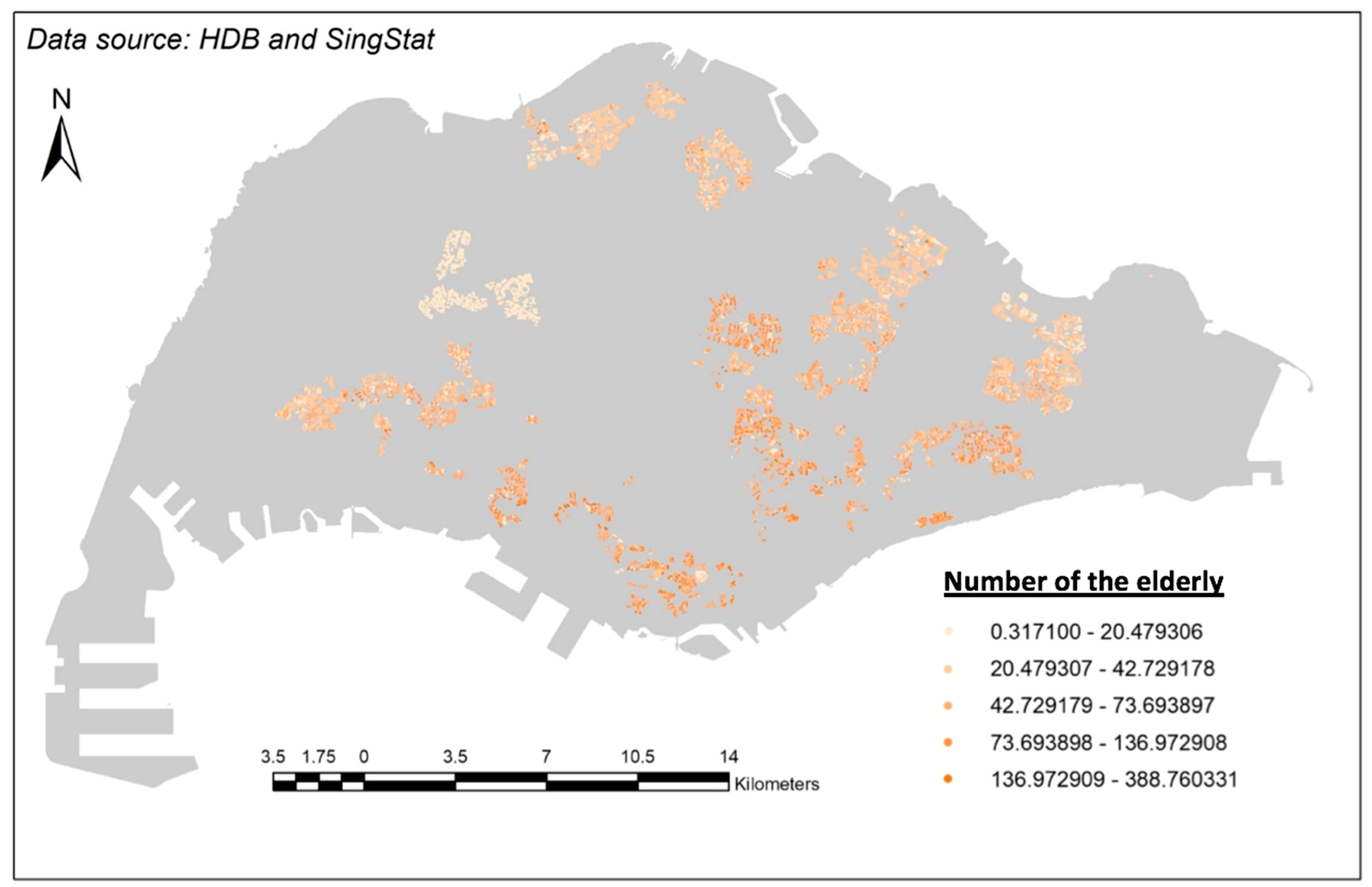
3.3.2. Population Density of Singapore Elderly Living in HDBs
3.3.3. Parameter Setting
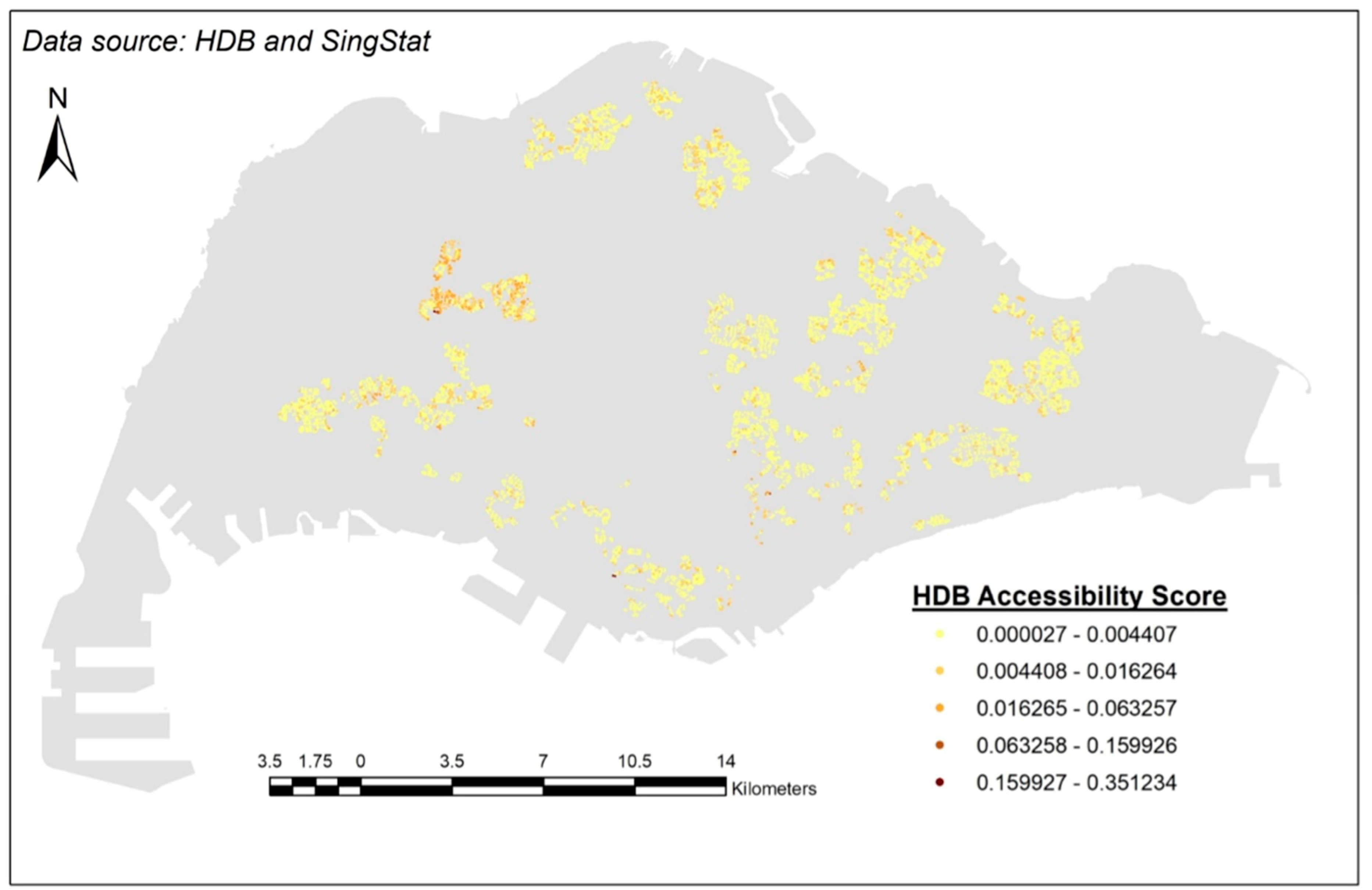
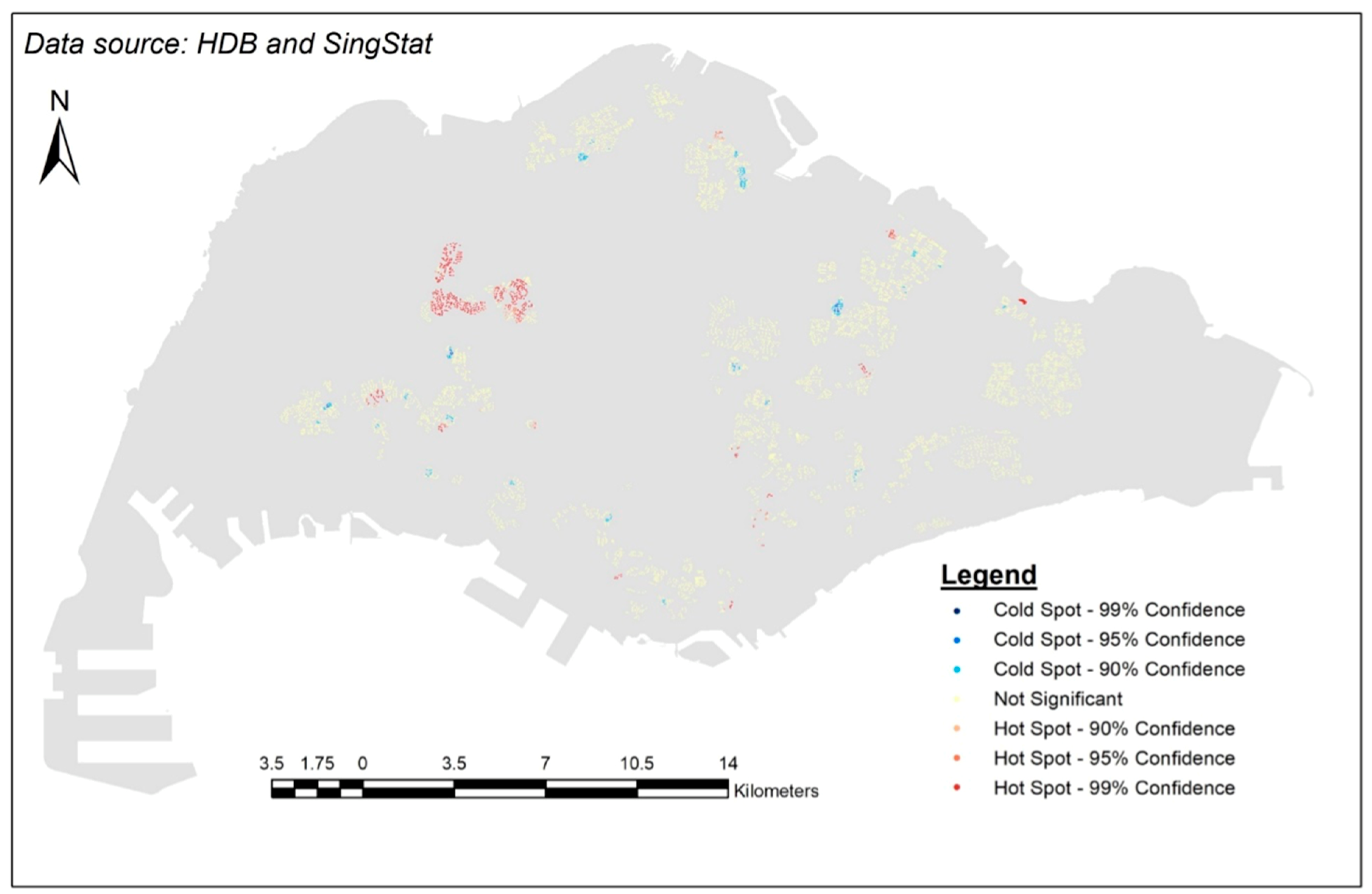
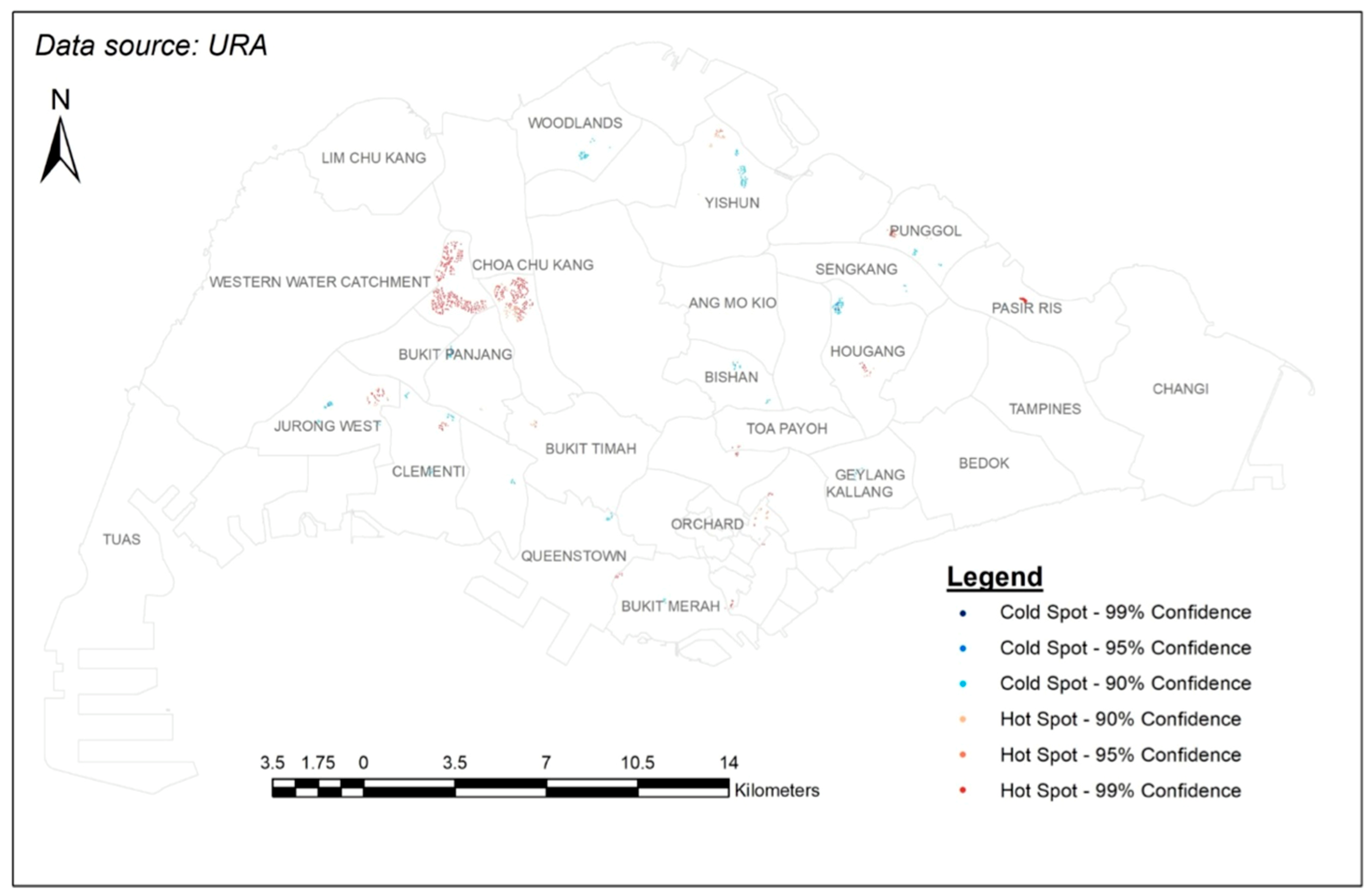
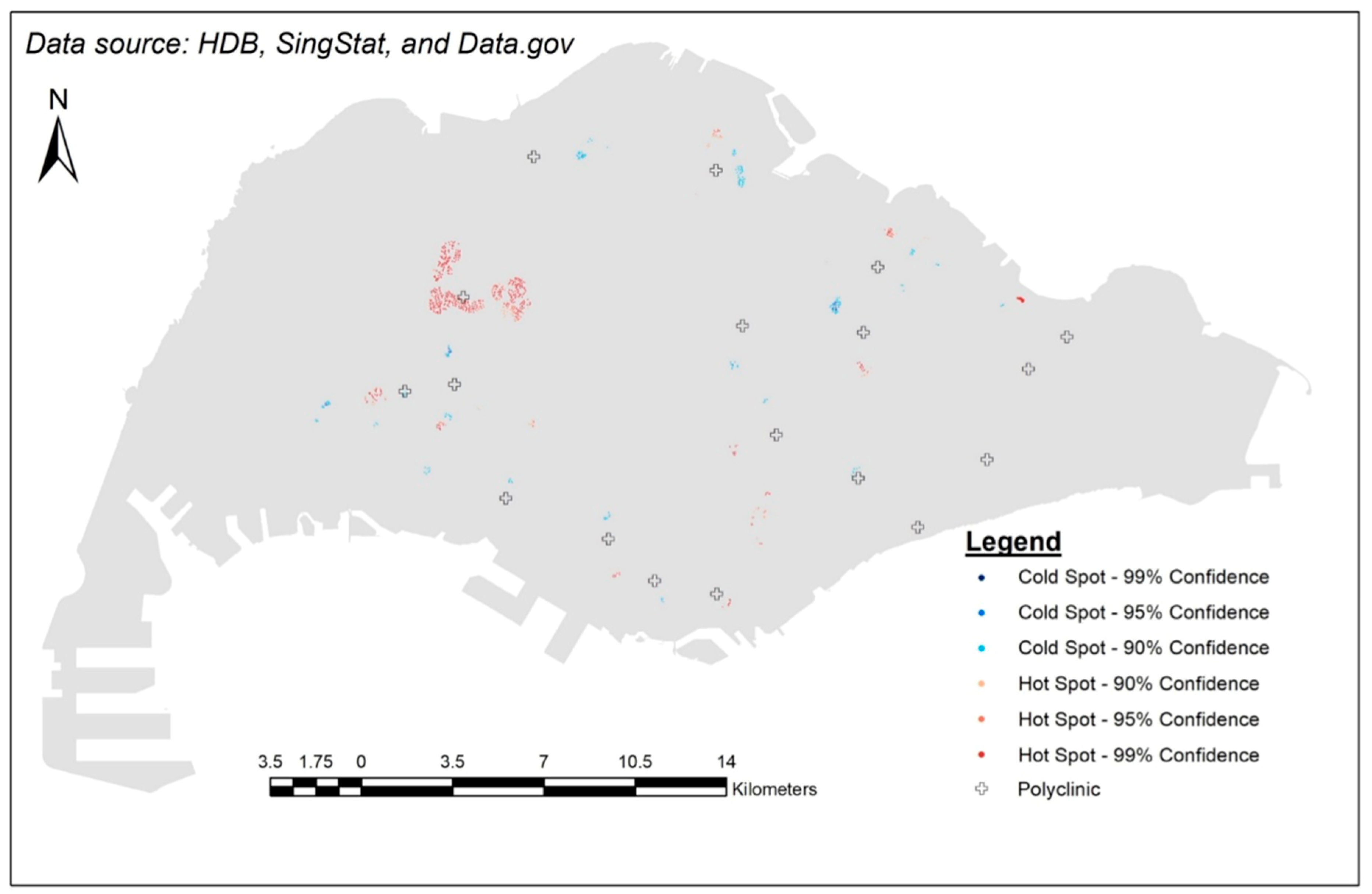
3.4. Results
4. Discussion
4.1. Explanations on the Hot Spots
4.2. Explanations on the Cold Spots
4.3. More Implications
4.4. Limitations
5. Conclusions
Author Contributions
Acknowledgements
Conflicts of Interest
References and Note
- Bynum, J.; Chang, C.; Austin, A.; Carmichael, D.; Meara, E. Outcomes in Older Adults with Multimorbidity Associated with Predominant Provider of Care Specialty. J. Am. Geriatr. Soc. 2017, 65, 1916–1923. [Google Scholar] [CrossRef] [PubMed]
- Edwards, S.; Landon, B. Seeking Value in Healthcare: The Importance of Generalists as Primary Care Physicians. J. Am. Geriatr. Soc. 2017, 65, 1900–1901. [Google Scholar] [CrossRef] [PubMed]
- Deraas, T.; Berntsen, G.; Jones, A.; Førde, O.; Sund, E. Associations between primary healthcare and unplanned medical admissions in Norway: A multilevel analysis of the entire elderly population. BMJ Open 2014, 4, e004293. [Google Scholar] [CrossRef] [PubMed]
- Luo, W.; Wang, F. Measure of spatial accessibility to healthcare in a GIS environment: Synthesis and a case study in the Chicago region. Environ. Plan. B 2003, 30, 865–884. [Google Scholar] [CrossRef]
- Guagliardo, M. Spatial accessibility of primary care: Concept, methods and challenges. Int. J. Health Geogr. 2004, 3. [Google Scholar] [CrossRef] [PubMed]
- Joseph, A.E.; Phillips, D.R. Accessibility and Utilization: Geographical Perspectives on Health Care Delivery; Sage: Newcastle upon Tyne, UK, 1984. [Google Scholar]
- DOS. Population Trends. 2017. Available online: https://www.singstat.gov.sg/statistics/visualising-data/storyboards/population-trends (accessed on 12 November 2017).
- NPTD. Ageing. 2017. Available online: https://www.population.sg/ageing (accessed on 12 November 2017).
- MOH. Speech by Mr Gan Kim Yong, Minister for Health, at the SG50 Scientific Conference on Ageing, on 19 March 2015, ‘Ageing in Singapore in the Next 50 Years’.
- Cheng, Y. Residential Care for Elderly People in Beijing; A Study of the Relationship between Health and Place: Beijing, China, 2010. [Google Scholar]
- Loo, B.P.; Lam, W.W.Y. Geographic accessibility around health care facilities for elderly residents in Hong Kong: A microscale walkability assessment. Environ. Plan. B Plan. Des. 2012, 39, 629–646. [Google Scholar]
- Wei, Z. A Study of Accessibility to Health Facilities for Elderly People in Metro Atlanta Using a Categorical Multi-Step Floating Catchment Area Method. Master’s Thesis, University of Georgia, Athens, GA, USA, 2013. [Google Scholar]
- MOH. Life Expectancy in Singapore. 2016. Available online: http://www.singstat.gov.sg/docs/default-source/default-document-library/publications/publications_and_papers/births_and_deaths/lifetable15-16.pdf (accessed on 12 November 2017).
- Khan, A. An integrated approach to measuring potential spatial access to health care services. Soc.-Econ. Plan. Sci. 1992, 26, 275–287. [Google Scholar] [CrossRef]
- Wing, P.; Reynolds, C. The availability of physician services: A geographic analysis. Health Serv. Res. 1988, 23, 649–667. [Google Scholar] [PubMed]
- Huff, D.L. A probabilistic analysis of shopping center trade areas. Land Econ. 1963, 39, 81–90. [Google Scholar] [CrossRef]
- Huff, D.L. Defining and estimating a trading area. J. Mark. 1964, 28, 34–38. [Google Scholar] [CrossRef]
- Luo, W.; Qi, Y. An enhanced two-step floating catchment area (E2SFCA) method for measuring spatial accessibility to primary care physicians. Health Place 2009, 15, 110–1107. [Google Scholar] [CrossRef] [PubMed]
- Joseph, A.E.; Bantock, P.R. Measuring potential physical accessibility to general practitioners in rural areas: A method and case study. Soc. Sci. Med. 1982, 16, 85–90. [Google Scholar] [CrossRef]
- Seow, L.S.E.; Subramaniam, M.; Abdin, E.; Vaingankar, J.A.; Chong, S.A. Hypertension and its associated risks among Singapore elderly residential population. J. Clin. Gerontol. Geriatr. 2015, 6, 125–132. [Google Scholar] [CrossRef]
- Lim, W.S.; Ding, Y.Y. Evidence-balance Medicine: “Real” Evidence-based Medicine in the Elderly. Ann. Acad. Med. 2015, 44, 1–5. [Google Scholar]
- Tan, N.E.; Sagayadevan, V.; Abdin, E.; Picco, L.; Vaingankar, J.; Chong, S.A.; Subramaniam, M. Employment status among the Singapore elderly and its correlates. Psychogeriatrics 2017, 17, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Kua, E.H. Colours of Ageing: 30 Years of Research on the Mental Health of the Singapore Elderly; Write Editions: Singapore, 2017. Available online: http://www.nlb.gov.sg/biblio/202747162 (accessed on 12 November 2017).
- Chen, A.J.; Cheung PP, L. The Elderly in Singapore; ASEAN Population Co-ordinating Unit: Singapore, 1988. [Google Scholar]
- Wee, L.E.; Yong, Y.Z.; Chng, M.W.X.; Chew, S.H.; Cheng, L.; Chua, Q.H.A.; Yek, J.J.L.; Lau, L.J.F.; Anand, P.; Hoe, J.T.M.; et al. Individual and area-level socioeconomic status and their association with depression amongst community-dwelling elderly in Singapore. Aging Ment. Health 2014, 18, 628–641. [Google Scholar] [CrossRef] [PubMed]
- Yap, M.T. State of the Elderly in Singapore 2008–2009; Ministry of Community Development, Youth and Sports: Singapore, 2010.
- Wong, L.Y.; Heng, B.H.; Cheah, J.T.S.; Tan, C.B. Using spatial accessibility to identify polyclinic service gaps and volume of under-served population in Singapore using Geographic Information System. Int. J. Health Plan. Manag. 2012, 27. [Google Scholar] [CrossRef] [PubMed]
- Koh, P.; Leow, B.; Wong, Y. Mobility of the elderly in densely populated neighbourhoods in Singapore. Sustain. Cities Soc. 2015, 14, 126–132. [Google Scholar] [CrossRef]
- Peng, Z. The job-housing balance and urban commuting. Urban Stud. 1997, 34, 1215–1235. [Google Scholar] [CrossRef]
- Wang, F. Modeling commuting patterns in Chicago in a GIS environment: A job accessibility perspective. Prof. Geogr. 2000, 52, 120–133. [Google Scholar] [CrossRef]
- Silverman, B.W. Density Estimation for Statistics and Data Analysis; Chapman and Hall: London, UK, 1986. [Google Scholar]
- Luo, W.; Qi, Y. Using a GIS-based floating catchment method to assess areas with shortage of physicians. Health Place 2004, 10, 1–11. [Google Scholar] [CrossRef]
- Kanuganti, S.; Sarkar, A.; Singh, A. Evaluation of access to health care in rural areas using enhanced two-step floating catchment area (E2SFCA) method. J. Transp. Geogr. 2016, 56, 45–52. [Google Scholar] [CrossRef]
- Donohoe, J.; Marshall, V.; Tan, X.; Camacho, F.; Anderson, R.; Balkrishnan, R. Predicting Late-stage Breast Cancer Diagnosis and Receipt of Adjuvant Therapy: Applying Current Spatial Access to Care Methods in Appalachia. Med. Care 2015, 53, 980–988. [Google Scholar] [CrossRef] [PubMed]
- McGrail, M.R.; Humphreys, J.S. Measuring spatial accessibility to primary healthcare services: Utilising dynamic catchment sizes. Appl. Geogr. 2014, 54, 182–188. [Google Scholar] [CrossRef]
- Kwan, M.P. Space-time and integral measures of individual accessibility: A comparative analysis using a point-based framework. Geogr. Anal. 1998, 30, 191–216. [Google Scholar] [CrossRef]
- Langford, M.; Fry, R.; Higgs, G. Measuring transit system accessibility using a modified two-step floating catchment technique. Int. J. Geogr. Inf. Sci. 2012, 26, 193–214. [Google Scholar] [CrossRef]
- Delamater, P.L. Spatial accessibility in suboptimally configured health care systems: A modified two-step floating catchment area (M2SFCA) metric. Health Place 2013, 24, 30–43. [Google Scholar] [CrossRef] [PubMed]
- Dai, D. Black residential segregation, disparities in spatial access to health care facilities, and late-stage breast cancer diagnosis in metropolitan Detroit. Health Place 2010, 16, 1038–1052. [Google Scholar] [CrossRef] [PubMed]
- Wang, F. Measurement, optimization, and impact of health care accessibility: A methodological review. Ann. Assoc. Am. Geogr. 2012, 102, 1104–1112. [Google Scholar] [CrossRef] [PubMed]
- Dai, D.; Wang, F. Geographic disparities in accessibility to food stores in southwest Mississippi. Environ. Plan. B Plan. Des. 2011, 38, 659–677. [Google Scholar] [CrossRef]
- Yang, D.H.; Goerge, R.; Mullner, R. Comparing GIS-based methods of 187 measuring spatial accessibility to health services. J. Med. Syst. 2006, 30, 23–32. [Google Scholar] [CrossRef] [PubMed]
- Luo, W.; Whippo, T. Variable catchment sizes for the two-step floating catchment area (2SFCA) method. Health Place 2012, 18, 789–795. [Google Scholar] [CrossRef] [PubMed]
- Schuurman, N.; Bérubé, M.; Crooks, V. Measuring potential spatial access to primary health care physicians using a modified gravity model. Can. Geogr. Géogr. Can. 2010, 54, 29–45. [Google Scholar] [CrossRef]
- MOF. Pioneer Generation Package is Adequately Funded and will be Transparent. 2014. Available online: http://www.mof.gov.sg/news-reader/articleid/1446/parentId/59/year/undefined?wmode=transparent (accessed on 12 November 2017).
- Singapore_Government. Pioneer Generation Package Overview. 2017. Available online: https://www.pioneers.sg/en-sg/Pages/Overview.aspx (accessed on 12 November 2017).
- DOS. Resident Population by Planning Area, Age Group and Type of Dwelling Jun 2017; DOS: Singapore, 2017. [Google Scholar]
- MOH. Healthcare Institution Statistics. 2017. Available online: https://www.moh.gov.sg/content/moh_web/home/statistics/healthcare_institutionstatistics.html (accessed on 12 November 2017).
- MOH. Polyclinics. 2011. Available online: https://www.moh.gov.sg/content/moh_web/home/pressRoom/Parliamentary_QA/2011/polyclinics.html (accessed on 12 November 2017).
- NHGP. Our Clinics. 2017. Available online: https://www.nhgp.com.sg/Find_A_Polyclinic_Near_You/ (accessed on 12 November 2017).
- SingHealth. About Us. 2014. Available online: https://polyclinic.singhealth.com.sg/aboutus/ourpolyclinics/Pages/home.aspx (accessed on 12 November 2017).
- Saultz, J.; Lochner, J. Interpersonal Continuity of Care and Care Outcomes: A Critical Review. Ann. Fam. Med. 2005, 3, 159–166. [Google Scholar] [CrossRef] [PubMed]
- MOH. Primary Care Subsidies. 2017. Available online: https://www.moh.gov.sg/content/moh_web/home/pressRoom/Current_Issues/2014/s-3ms-resources/primary-care-subsidies.html (accessed on 12 November 2017).
- CHAS. About CHAS. 2017. Available online: http://www.chas.sg/content.aspx?id=636 (accessed on 12 November 2017).
- MOH. Health Manpower. 2017. Available online: https://www.moh.gov.sg/content/moh_web/home/statistics/Health_Facts_Singapore/Health_Manpower.html (accessed on 12 November 2017).
- Kang, S.; Tan, E.; Yap, M. National Survey of Senior Citizens 2011. 2013. Available online: Duke-nus.edu.sg: https://www.duke-nus.edu.sg/care/wp-content/uploads/National-Survey-of-Senior-Citizens-2011.pdf (accessed on 12 November 2017).
- MOH. Bulk of Clinics Are in CHAS Scheme. 2017. Available online: https://www.moh.gov.sg/content/moh_web/home/pressRoom/Media_Forums/2017/bulk-of-clinics-are-in-chas-scheme.html (accessed on 12 November 2017).
- LTA. Enhancing Physical Accessibility for All. Making Travel Easier For You; Public Transport; 2017. Available online: https://www.lta.gov.sg/content/ltaweb/en/public-transport/system-design/enhancing-physical-accessibility-for-all.html (accessed on 12 November 2017).
- Krishnasamy, C.; Unsworth, C.; Howie, L. Exploring the mobility preferences and perceived difficulties in using transport and driving with a sample of healthy and outpatient older adults in Singapore. Aust. Occup. Ther. J. 2013, 60, 129–137. [Google Scholar] [CrossRef] [PubMed]
- DOS. Table 11A. Average Monthly Household Income from Work (Including Employer CPF Contributions) Among Resident Employed Households by Type of Dwelling, 2000–2016. 2017. Available online: http://www.tablebuilder.singstat.gov.sg/publicfacing/createSpecialTable.action?refId=12315 (accessed on 12 November 2017).
- Bollard, E.; Fleming, H. A study to investigate the walking speed of elderly adults with relation to pedestrian crossings. Physiother. Theory Pract. 2013, 29, 142–149. [Google Scholar] [CrossRef] [PubMed]
- Fiser, W.; Hays, N.; Rogers, S.; Kajkenova, O.; Williams, A.; Evans, C.; Evans, W. Energetics of Walking in Elderly People: Factors Related to Gait Speed. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2010, 65, 1332–1337. [Google Scholar] [CrossRef] [PubMed]
- Harwood, R.; Conroy, S. Slow walking speed in elderly people. BMJ 2009, 339, b4236. [Google Scholar] [CrossRef] [PubMed]
- Lindemann, U.; Najafi, B.; Zijlstra, W.; Hauer, K.; Muche, R.; Becker, C.; Aminian, K. Distance to achieve steady state walking speed in frail elderly persons. Gait Posture 2008, 27, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Yeo, S.; He, Y. Commuter characteristics in mass rapid transit stations in Singapore. Fire Saf. J. 2009, 44, 183–191. [Google Scholar] [CrossRef]
- HDB. Public Housing in Singapore: Residents’ Profile, Housing Satisfaction and Preferences; HDB: Singapore, 2014.
- HDB. History. 2017. Available online: http://www.hdb.gov.sg/cs/infoweb/about-us/history (accessed on 12 November 2017).
- Remember_Singapore. From Villages to Flats (Part 2)—Public Housing in Singapore. 2012. Available online: https://remembersingapore.org/2012/05/11/from-villages-to-flats-part-2/ (accessed on 12 November 2017).
- HDB. Remaking Our Heartland. 2017. Available online: http://www20.hdb.gov.sg/fi10/fi10349p.nsf/hdbroh/index.html (accessed on 12 November 2017).
- Karthigayan, R. Remarking Our Heartland—Rejuvenating Singapore. 2017. Available online: https://www.gov.sg/news/content/remaking-our-heartlands-rejuvenating-singapore (accessed on 12 November 2017).
- Abdullah, Z. Punggol: Singapore’s Baby Town. The Straits Times. 8 June 2017. Available online: http://www.straitstimes.com/singapore/singapores-baby-town (accessed on 12 November 2017).
- Kuai, X.; Zhao, Q. Examining healthy food accessibility and disparity in Baton Rouge, Louisiana. Ann. GIS 2017, 23, 103–116. [Google Scholar] [CrossRef]
- Yu, J.C. GIS-Based Approach to the Characterisation of Spatial Accessibility to Primary Health Care Facilities in the Melbourne Metropolitan Area. Master’s Thesis, RMIT University, RMIT University Research Repository, Melbourne, Australia, 2014. [Google Scholar]
- Dai, D. Racial/ethnic and socioeconomic disparities in urban green space accessibility: Where to intervene. Landsc. Urban Plan. 2011, 102, 234–244. [Google Scholar] [CrossRef]
- Ni, J.; Wang, J.; Rui, Y.; Qian, T.; Wang, J. An Enhanced Variable Two-Step Floating Catchment Area Method for Measuring Spatial Accessibility to Residential Care Facilities in Nanjing. Int. J. Environ. Res. Public Health 2015, 12, 14490–14504. [Google Scholar] [CrossRef] [PubMed]
- Polo, G.; Acosta, C.M.; Ferreira, F.; Dias, R.A. Location-Allocation and Accessibility Models for Improving Spatial Planning of Public Health Services. PLoS ONE 2015, 10, e0119190. [Google Scholar] [CrossRef] [PubMed]
- Zhan, Q.; Wang, X.; Sliuzas, R. A GIS-based method to assess the shortage areas of community health service. In Proceedings of the 2011 International Conference On Remote Sensing, Environment and Transportation Engineering, Nanjing, China, 24–26 June 2011; pp. 5654–5657. [Google Scholar] [CrossRef]
- Polo, G.; Acosta, C.M.; Dias, R.A. Spatial accessibility to vaccination sites in a campaign against rabies in São Paulo city, Brazil. Prev. Vet. Med. 2013, 111, 10–16. [Google Scholar] [CrossRef] [PubMed]
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Deborah, O.M.L.; Chiu, M.Y.L.; Cao, K. Geographical Accessibility of Community Health Assist Scheme General Practitioners for the Elderly Population in Singapore: A Case Study on the Elderly Living in Housing Development Board Flats. Int. J. Environ. Res. Public Health 2018, 15, 1988. https://doi.org/10.3390/ijerph15091988
Deborah OML, Chiu MYL, Cao K. Geographical Accessibility of Community Health Assist Scheme General Practitioners for the Elderly Population in Singapore: A Case Study on the Elderly Living in Housing Development Board Flats. International Journal of Environmental Research and Public Health. 2018; 15(9):1988. https://doi.org/10.3390/ijerph15091988
Chicago/Turabian StyleDeborah, Ong Ming Lee, Marcus Yu Lung Chiu, and Kai Cao. 2018. "Geographical Accessibility of Community Health Assist Scheme General Practitioners for the Elderly Population in Singapore: A Case Study on the Elderly Living in Housing Development Board Flats" International Journal of Environmental Research and Public Health 15, no. 9: 1988. https://doi.org/10.3390/ijerph15091988
APA StyleDeborah, O. M. L., Chiu, M. Y. L., & Cao, K. (2018). Geographical Accessibility of Community Health Assist Scheme General Practitioners for the Elderly Population in Singapore: A Case Study on the Elderly Living in Housing Development Board Flats. International Journal of Environmental Research and Public Health, 15(9), 1988. https://doi.org/10.3390/ijerph15091988





