Mature or Emerging? The Impact of Treatment-Related Internet Health Information Seeking on Patients’ Trust in Physicians
Abstract
1. Introduction
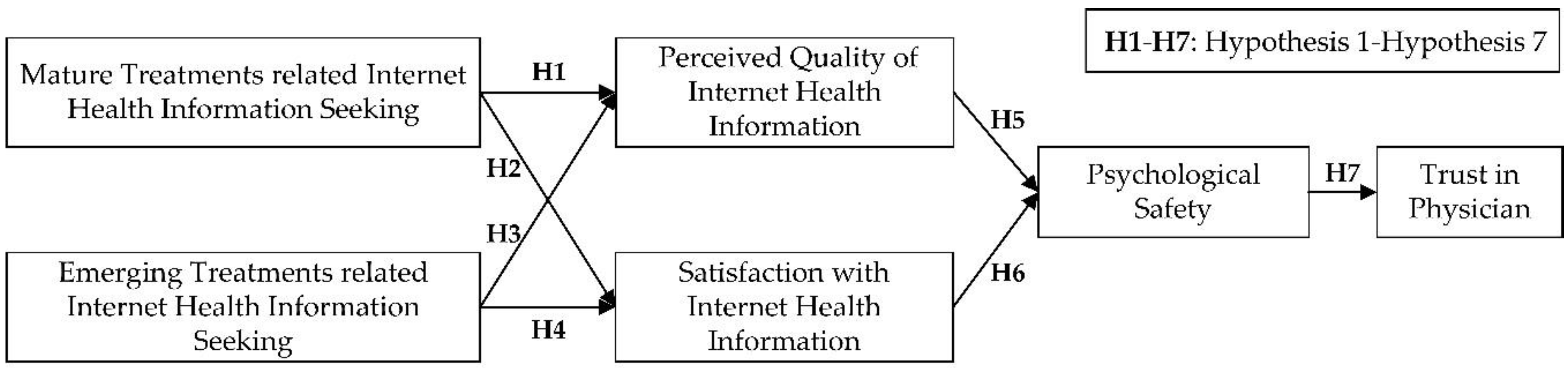
2. Research Model and Hypotheses
3. Materials and Methods
3.1. Instrument Development
3.2. Analysis Tool Selection
3.3. Data Collection and Respondent Profile
4. Results
4.1. Data Analysis
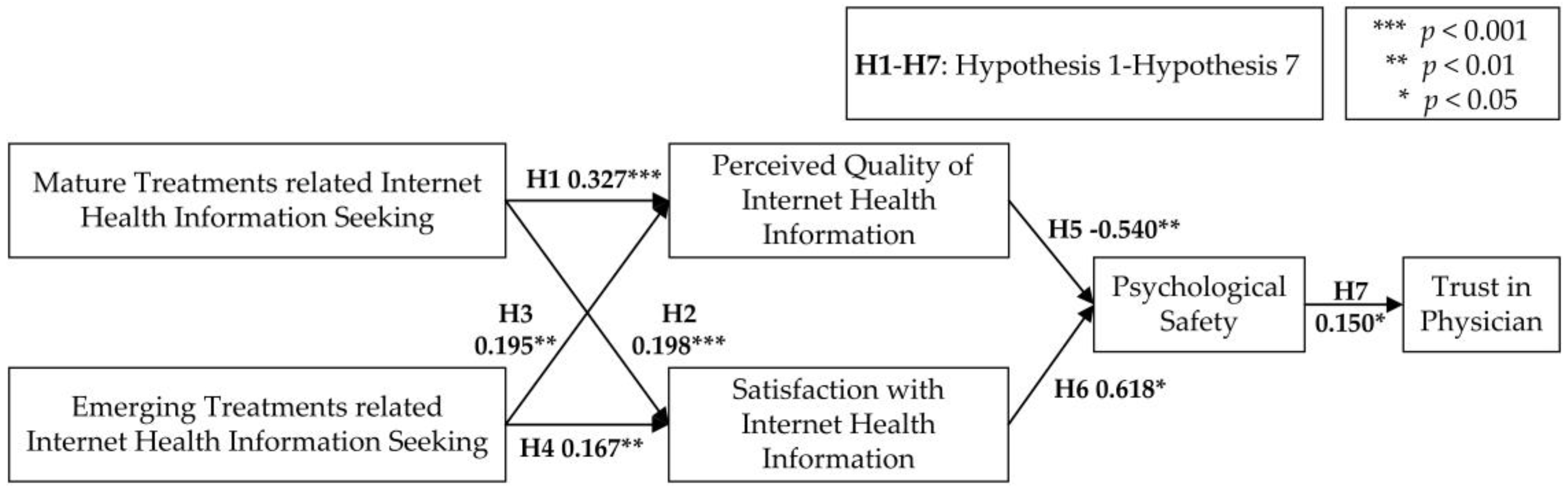
4.2. Hypotheses Testing
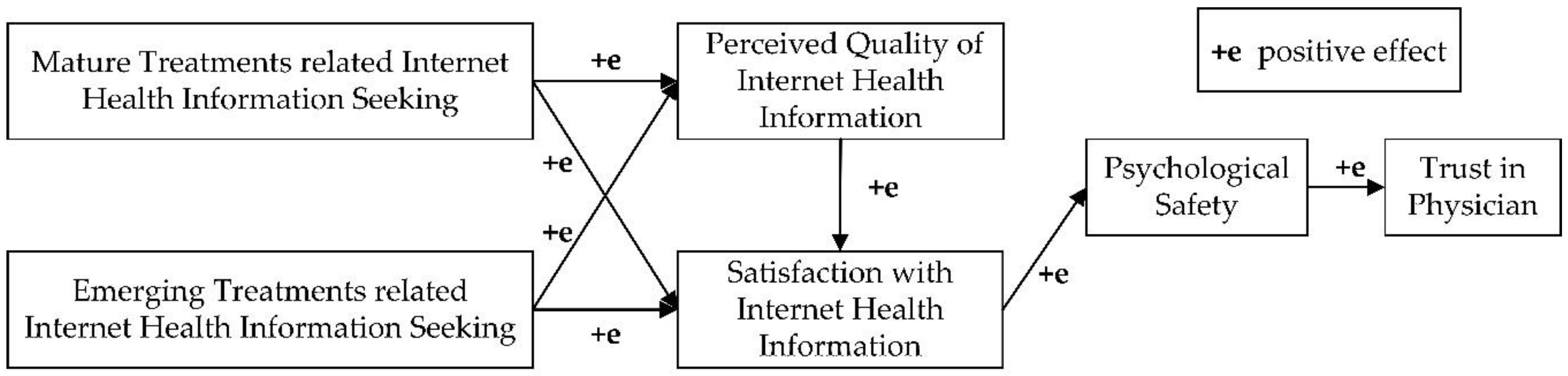
5. Discussion
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Construct | Items |
|---|---|
| Emerging Treatments related Internet Health Information Seeking | 1. I frequently seek emerging treatments related Internet health information to understand a health problem or an illness. 2. I frequently seek emerging treatments related Internet health information to obtain different points of view from those offered by mainstream medicine. 3. I frequently seek emerging treatments related Internet health information to prevent illness by adopting a healthy lifestyle. 4. I frequently seek emerging treatments related Internet health information to find a specific solution to or treatment for a health problem. 5. I frequently seek emerging treatments related Internet health information to help a friend or family member who is ill. |
| Mature Treatments related Internet Health Information Seeking | 1. I frequently seek mature treatments related Internet health information to understand a health problem or an illness. 2. I frequently seek mature treatments related Internet health information to obtain different points of view from those offered by mainstream medicine. 3. I frequently seek mature treatments related Internet health information to prevent illness by adopting a healthy lifestyle. 4. I frequently seek mature treatments related Internet health information to find a specific solution to or treatment for a health problem. 5. I frequently seek mature treatments related Internet health information to help a friend or family member who is ill. |
| Perceived Quality of Internet Health Information | Relevance 1. For your health information needs, to what degree do you believe the Internet Health Information (IHI) provided by the website was applicable to your needs? 2. For your health information needs, to what degree do you believe Internet Health Information (IHI) provided by the website was related to your needs? 3. For your health information needs, to what degree do you believe Internet Health Information (IHI) provided by the website was pertinent to your needs? 4. For your health information needs, to what degree do you believe Internet Health Information (IHI) provided by the website was relevant to your needs? Understandability 1. For your health information needs, to what degree do you believe Internet Health Information (IHI) provided by the website was clear in meaning? 2. For your health information needs, to what degree do you believe Internet Health Information (IHI) provided by the website was easy to read? 3. For your health information needs, to what degree do you believe Internet Health Information (IHI) provided by the website was easy to comprehend? 4. For your health information needs, to what degree do you believe Internet Health Information (IHI) provided by the website was understandable? Adequacy 1. For your health information needs, to what degree do you believe Internet Health Information (IHI) provided by the website was sufficient? 2. For your health information needs, to what degree do you believe Internet Health Information (IHI) provided by the website was complete? 3. For your health information needs, to what degree do you believe Internet Health Information (IHI) provided by the website was adequate? 4. For your health information needs, to what degree do you believe Internet Health Information (IHI) provided by the website contained the necessary topics/categories? Usefulness 1. For your health information needs, to what degree do you believe Internet Health Information (IHI) provided by the website was informative? 2. For your health information needs, to what degree do you believe Internet Health Information (IHI) provided by the website was valuable? 3. For your health information needs, to what degree do you believe Internet Health Information (IHI) provided by the website was helpful? 4. For your health information needs, to what degree do you believe Internet Health Information (IHI) provided by the website was useful? |
| Satisfaction with Internet Health Information | 1. The information available on the Internet is reliable. 2. The information available on the Internet is complete. 3. The information available on the Internet is clear and understandable. 4. The information available on the Internet is well structured. 5. This doctor was interested in me as a person and not just my illness. 6. It is quite simple to surf the Internet. 7. I quickly became comfortable surfing the Internet. 8. I can easily find the information I need on the Internet. 9. The Internet is a useful tool. 10. The Internet satisfies all of my health information needs. 11. The Internet always has an answer to my question. |
| Psychological Safety | 1. In treatment, I am still not afraid to be myself. 2. I am afraid to express my opinions in treatment. 3. I think there is a threatening medical environment. |
| Trust in Physician | 1. In general, doctors care about their patient’s health just as much as, or more than their patients do. 2. Sometimes doctors care more about what is convenient for them than about their patient’s medical needs. 3. Doctors are extremely thorough and careful 4. I completely trust doctor’s decisions about which medical treatments are best. 5. Doctors are totally honest in telling their patients about all of the treatment options available for their conditions. 6. Sometimes doctors do not pay full attention to what patients are trying to tell them. 7. Doctors always use their very best skill and effort on behalf of their patients. 8. I have no worries about putting my life in hands of doctors. 9. A doctor would never mislead you about anything. 10. All in all, I trust doctors completely. |
References
- Blomstedt, P.; Sjöberg, R.L.; Hansson, M.; Bodlund, O.; Hariz, M.I. Deep brain stimulation in the treatment of depression. Acta Psychiatr. Scand. 2015, 123, 4–11. [Google Scholar] [CrossRef] [PubMed]
- Choi, H.H.; Cho, Y.-S. Fecal microbiota transplantation: Current applications, effectiveness, and future perspectives. Clin. Endosc. 2016, 49, 257–265. [Google Scholar] [CrossRef] [PubMed]
- Song, H.; Lahood, N.; Mostaghimi, A. Intravenous immunoglobulin as adjunct therapy for refractory pyoderma gangrenosum: Systematic review of cases and case series. Br. J. Dermatol. 2017, 178, e164. [Google Scholar] [CrossRef]
- Bylund, C.L.; Gueguen, J.A.; Sabee, C.M.; Imes, R.S.; Li, Y.; Sanford, A.A. Provider-patient dialogue about Internet health information: An exploration of strategies to improve the provider-patient relationship. Patient Educ. Couns. 2007, 66, 346–352. [Google Scholar] [CrossRef] [PubMed]
- Bell, R.A.; Hu, X.; Orrange, S.E.; Kravitz, R.L. Lingering questions and doubts: Online information-seeking of support forum members following their medical visits. Patient Educ. Couns. 2011, 85, 525–528. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.R.; Sillence, E.; Briggs, P. Perceived threat and corroboration: Key factors that improve a predictive model of trust in Internet-based health information and advice. J. Med. Internet Res. 2011, 13, e51. [Google Scholar] [CrossRef] [PubMed]
- Seçkin, G.; Yeatts, D.; Hughes, S.; Hudson, C.; Bell, V. Being an informed consumer of health information and assessment of electronic health literacy in a national sample of Internet users: Validity and reliability of the e-HLS instrument. J. Med. Internet Res. 2016, 18, e161. [Google Scholar] [CrossRef] [PubMed]
- Graffigna, G.; Barello, S.; Bonanomi, A.; Riva, G. Factors affecting patients’ online health information—Seeking behaviours: The role of the Patient Health Engagement (PHE) Model. Patient Educ. Couns. 2017, 100, 1918–1927. [Google Scholar] [CrossRef] [PubMed]
- Marcinkiewicz, M.; Mahboobi, H. The impact of the Internet on the doctor-patient relationship. Australas. Med. J. 2009, 1, 102–104. [Google Scholar] [CrossRef]
- Mah, J.K. Current and emerging treatment strategies for Duchenne muscular dystrophy. Neuropsychiatr. Dis. Treat. 2016, 12, 1795–1807. [Google Scholar] [CrossRef] [PubMed]
- Dean, C.A.; Geneus, C.J.; Rice, S.; Johns, M.; Quasie-Woode, D.; Broom, K.; Elder, K. Assessing the significance of health information seeking in chronic condition management. Patient Educ. Couns. 2017, 100, 1519–1526. [Google Scholar] [CrossRef] [PubMed]
- Laugesen, J.; Hassanein, K.; Yuan, Y.F. The impact of Internet health information on patient compliance: A research model and an empirical study. J. Med. Internet Res. 2015, 7, e143. [Google Scholar] [CrossRef] [PubMed]
- Jiang, S. How does patient-centered communication improve emotional health? An exploratory study in China. Asian J. Commun. 2018, 28, 298–314. [Google Scholar] [CrossRef]
- Samal, L.; Saha, S.; Chander, G.; Korthuis, P.T.; Sharma, R.K.; Sharp, V.; Cohn, J.; Moore, R.D.; Beach, M.C. Internet health information seeking behavior and antiretroviral adherence in persons living with HIV/AIDS. AIDS Patient Care STDs 2011, 25, 445–449. [Google Scholar] [CrossRef] [PubMed]
- Tustin, N. The role of patient satisfaction in online health information seeking. J. Health Commun. 2010, 15, 3–17. [Google Scholar] [CrossRef] [PubMed]
- Lu, X.; Zhang, R.; Wu, W.; Shang, X.; Liu, M. The relationship between Internet health information and patient compliance based on trust: An empirical study. J. Med. Internet Res. 2018, 20, e253. [Google Scholar] [CrossRef] [PubMed]
- Krot, K. Online Information Seeking and Trust in Doctors: An Empirical Study. In Proceedings of the 24th International Scientific Conference on Economic and Social Development—Managerial Issues in Modern Business, Warsaw, Poland, 13–14 October 2017. [Google Scholar]
- Maloney, E.K.; D’Agostino, T.A.; Heerdt, A.; Dickler, M.; Li, Y.; Ostroff, J.S.; Bylund, C.L. Sources and types of online information that breast cancer patients read and discuss with their doctors. Palliat. Support. Care 2015, 13, 107–114. [Google Scholar] [CrossRef] [PubMed]
- Wilson, T.D. Human information behavior. Inform. Sci. 2000, 3, 49–56. [Google Scholar] [CrossRef]
- Dobransky, K.; Hargittai, E. Inquiring minds acquiring wellness: Uses of online and offline sources for health information. Health Commun. 2012, 27, 331–343. [Google Scholar] [CrossRef] [PubMed]
- Neter, E.; Brainin, E. eHealth literacy: Extending the digital divide to the realm of health information. J. Med. Internet Res. 2012, 14, e19. [Google Scholar] [CrossRef] [PubMed]
- Suri, V.R.; Majid, S.; Chang, Y.K.; Foo, S. Assessing the influence of health literacy on health information behaviors: A multi-domain skills-based approach. Patient Educ. Couns. 2016, 99, 1038–1045. [Google Scholar] [CrossRef] [PubMed]
- Hodgetts, D.; Bolam, B.; Stephens, C. Mediation and the construction of contemporary understandings of health and lifestyle. J. Health Psychol. 2005, 10, 123–136. [Google Scholar] [CrossRef] [PubMed]
- Li, F.; Li, M.; Guan, P.; Ma, S.; Cui, L. Mapping publication trends and identifying hot spots of research on Internet health information seeking behavior: A quantitative and co-word biclustering analysis. J. Med. Internet Res. 2015, 17, e81. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Guo, X.; Wu, T. Exploring the influence of the online physician service delivery process on patient satisfaction. Decis. Support Syst. 2015, 78, 113–121. [Google Scholar] [CrossRef]
- Nath, C.; Huh, J.; Adupa, A.K.; Jonnalagadda, S.R. Website sharing in online health communities: A descriptive analysis. J. Med. Internet Res. 2016, 18, e11. [Google Scholar] [CrossRef] [PubMed]
- Richardson, A.; Allen, J.A.; Xiao, H.; Vallone, D. Effects of race/ethnicity and socioeconomic status on health information-seeking, confidence, and trust. J. Health Care Poor Underserv. 2012, 23, 1477–1493. [Google Scholar] [CrossRef] [PubMed]
- Jiang, S.; Street, R.L. Pathway linking Internet health information seeking to better health: A moderated mediation study. Health Commun. 2017, 32, 1024–1031. [Google Scholar] [CrossRef] [PubMed]
- Berger, M.; Wagner, T.H.; Baker, L.C. Internet use and stigmatized illness. Soc. Sci. Med. 2005, 61, 1821–1827. [Google Scholar] [CrossRef] [PubMed]
- Pang, P.C.; Chang, S.; Verspoor, K.; Pearce, J. Designing health websites based on users’ web-based information–seeking behaviors: A mixed-method observational study. J. Med. Internet Res. 2016, 18, e145. [Google Scholar] [CrossRef] [PubMed]
- Salancik, G.R.; Pfeffer, J.A. Social information processing approach to job attitudes and task design. Adm. Sci. Q. 1978, 23, 224–253. [Google Scholar] [CrossRef] [PubMed]
- Young, G.J.; Meterko, M.M.; Mohr, D.; Shwartz, M.; Lin, H. Congruence in the assessment of service quality between employees and customers: A study of a public health care delivery system. J. Bus. Res. 2009, 62, 1127–1135. [Google Scholar] [CrossRef]
- Hsiung, H.H.; Tsai, W.C. The joint moderating effects of activated negative moods and group voice climate on the relationship between power distance orientation and employee voice behavior. Appl. Psychol. 2017, 66, 487–514. [Google Scholar] [CrossRef]
- Higgins, E.T. Beyond pleasure and pain. Am. Psychol. 1997, 52, 1280–1300. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.; Modrek, S.; Anyanti, J.; Nwokolo, E.; Cruz, A.D.L.; Schatzkin, E.; Isiguzo, C.; Ujuju, C.; Montagu, D. How do risk preferences relate to malaria care-seeking behavior and the acceptability of a new health technology in Nigeria. BMC Health Serv. Res. 2014, 14, 374. [Google Scholar] [CrossRef] [PubMed]
- Edmondson, A. Psychological safety and learning behavior in work teams. Adm. Sci. Q. 1999, 44, 350–383. [Google Scholar] [CrossRef]
- Edmondson, A.C.; Lei, Z. Psychological safety: The history, renaissance, and future of an interpersonal construct. Annu. Rev. Organ. Psychol. Organ. Behav. 2014, 1, 23–43. [Google Scholar] [CrossRef]
- Halbesleben, J.R.; Leroy, H.; Dierynck, B.; Simons, T.; Savage, G.T.; McCaughey, D.; Leon, M.R. Living up to safety values in health care: The effect of leader behavioral integrity on occupational safety. J. Occup. Health Psychol. 2013, 18, 395–405. [Google Scholar] [CrossRef] [PubMed]
- Collins, C.J.; Smith, K.G. Knowledge exchange and combination: The role of human resource practices in the performance of high-technology firms. Acad. Manag. J. 2006, 49, 544–560. [Google Scholar] [CrossRef]
- Triplett, S.M.; Loh, J.M.I. The moderating role of trust in the relationship between work locus of control and psychological safety in organisational work teams. Aust. J. Psychol. 2017, 70, 76–84. [Google Scholar] [CrossRef]
- Yanchus, N.J.; Derickson, R.; Moore, S.C.; Bologna, D.; Osatuke, K. Communication and psychological safety in veterans health administration work environments. J. Health Organ. Manag. 2014, 28, 754–776. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.Y.; Liu, W.; Shi, H.; Liu, C.; Wang, Y. Measuring patient safety culture in maternal and child health institutions in China: A qualitative study. BMJ Open 2017, 7, e015458. [Google Scholar] [CrossRef] [PubMed]
- Ducket, J.; Hunt, K.; Munro, N.; Sutton, M. Does distrust in providers affect health–care utilization in China? Health Policy Plan. 2016, 31, 1001–1009. [Google Scholar] [CrossRef] [PubMed]
- Erden, Z.; Krogh, G.V.; Kim, S. Knowledge sharing in an online community of volunteers: The role of community munificence. Eur. Manag. Rev. 2012, 9, 213–227. [Google Scholar] [CrossRef]
- Lee, Y.Y.; Lin, J.L. The effects of trust in physician on self-efficacy, adherence and diabetes outcomes. Soc. Sci. Med. 2009, 68, 1060–1068. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.Y.; Lin, J.L. Trust but verify: The interactive effects of trust and autonomy preferences on health outcomes. Health Care Anal. 2009, 17, 244–260. [Google Scholar] [CrossRef] [PubMed]
- Zhao, D.H.; Rao, K.Q.; Zhang, Z.R. Patient trust in physicians: Empirical evidence from Shanghai, China. Chin. Med. J. 2016, 129, 814–818. [Google Scholar] [CrossRef] [PubMed]
- Chunli, S.; Torsten, B.; Sven, V. Antecedents of employee’s preference for knowledge-sharing tool. Int. J. Hum. Resour. Man. 2012, 23, 3613–3635. [Google Scholar] [CrossRef]
- Mcallister, D.J. Affect- and cognition-based trust as foundations for interpersonal cooperation in organizations. Acad. Manag. J. 1995, 38, 24–59. [Google Scholar] [CrossRef]
- Rodríguez, V.; Andrade, A.D.; Garcíaretamero, R.; Anam, R.; Rodríguez, R.; Lisigurski, M.; Sharit, J.; Ruiz, J.G. Health literacy, numeracy, and graphical literacy among veterans in primary care and their effect on shared decision making and trust in physicians. J. Health Commun. 2013, 18, 273–289. [Google Scholar] [CrossRef] [PubMed]
- Thom, D.H.; Hall, M.A.; Pawlson, L.G. Measuring patients’ trust in physicians when assessing quality of care. Health Aff. 2004, 23, 124–132. [Google Scholar] [CrossRef] [PubMed]
- Graham, J.L.; Shahani, L.; Grimes, R.M.; Hartman, C.; Giordano, T.P. The influence of trust in physicians and trust in the healthcare system on linkage, retention, and adherence to HIV care. AIDS Patient Care STDs 2015, 29, 661–667. [Google Scholar] [CrossRef] [PubMed]
- Doescher, M.P.; Saver, B.G.; Franks, P.; Fiscella, K. Racial and ethnic disparities in perceptions of physician style and trust. Arch. Fam. Med. 2000, 9, 1156–1163. [Google Scholar] [CrossRef] [PubMed]
- Jones, D.E.; Carson, K.A.; Bleich, S.N.; Cooper, L.A. Patient trust in physicians and adoption of lifestyle behaviors to control high blood pressure. Patient Educ. Couns. 2012, 89, 57–62. [Google Scholar] [CrossRef] [PubMed]
- Rawaf, M.M.; Kressin, N.R. Exploring racial and sociodemographic trends in physician behavior, physician trust and their association with blood pressure control. J. Natl. Med. Assoc. 2007, 99, 1248–1254. [Google Scholar] [PubMed]
- Ha, H.Y.; John, J.; John, J.D.; Chung, Y.K. Temporal effects of information from social networks on online behavior. Internet Res. 2016, 26, 213–235. [Google Scholar] [CrossRef]
- Lapidot, Y.; Kark, R.; Shamir, B. The impact of situational vulnerability on the development and erosion of followers’ trust in their leader. Leadersh. Q. 2007, 18, 16–34. [Google Scholar] [CrossRef]
- Blau, P.M. Exchange and Power in Social Life; Routledge: New York, NY, USA, 1964. [Google Scholar]
- Foa, E.B.; Foa, U.G. Resource theory of social exchange. In Contemporary Topics in Sociology; Thibault, J.W., Spence, J.B., Carson, R.C., Eds.; General Learning Press: Morristown, NJ, USA, 1976; pp. 99–131. [Google Scholar]
- Foa, U.G.; Foa, E.B. Societal Structures of the Mind; Thomas: Springfield, IL, USA, 1974. [Google Scholar]
- Zhang, Y.; Fang, Y.; Wei, K.; Wang, Z. Promoting the intention of students to continue their participation in e-learning systems. Inf. Technol. People 2012, 25, 356–375. [Google Scholar] [CrossRef]
- Gordon, H.S.; Pugach, O.; Berbaum, M.L.; Ford, M.E. Examining patients’ trust in physicians and the VA healthcare system in a prospective cohort followed for six-months after an exacerbation of heart failure. Patient Educ. Couns. 2014, 97, 173–179. [Google Scholar] [CrossRef] [PubMed]
- Lemire, M.; Paré, G.; Sicotte, C.; Harvey, C. Determinants of Internet use as a preferred source of information on personal health. Int. J. Med. Inform. 2008, 77, 723–734. [Google Scholar] [CrossRef] [PubMed]
- Chikoko, G.L.; Buitendach, J.H.; Kanengoni, H. The psychological conditions that predict work engagement among tertiary education employees. J. Psychol. Afr. 2014, 24, 469–474. [Google Scholar] [CrossRef]
- Torbit, L.A.; Albiani, J.J.; Aronson, M.; Holter, S.; Semotiuk, K.; Cohen, Z.; Hart, T.L. Physician trust moderates the relationship between intolerance of uncertainty and cancer worry interference among women with Lynch syndrome. J. Behav. Med. 2016, 39, 420–428. [Google Scholar] [CrossRef] [PubMed]
- Sardeshmukh, S.; Vandenberg, R.J. Integrating moderation and mediation: A structural equation modeling approach. Organ. Res. Methods 2017, 20, 721–745. [Google Scholar] [CrossRef]
- Bu, X.Q.; You, L.M.; Li, Y.; Liu, K.; Zheng, J.; Yan, T.B.; Chen, S.X.; Zhang, L.F. Psychometric properties of the Kessler 10 scale in Chinese parents of children with cancer. Cancer Nurs. 2016, 40, 297–304. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Y.Y.; Li, T.; Xiao, L.; Wang, S.W.; Wang, S.Q.; Wang, H.X.; Wang, B.B.; Gao, Y.L. The Chinese version of instrument of professional attitude for student nurses (IPASN): Assessment of reliability and validity. Nurse Educ. Today 2017, 49, 79–83. [Google Scholar] [CrossRef] [PubMed]
- Wong, W.S.; Chen, P.P.; Chow, Y.F.; Wong, S.; Fielding, R. A study of the reliability and concurrent validity of the Chinese version of the pain medication attitude questionnaire (ChPMAQ) in a sample of Chinese patients with chronic pain. Pain Med. 2016, 17, 1137–1144. [Google Scholar] [CrossRef] [PubMed]
- Wimble, M. Understanding health and health–related behavior of users of Internet health information. Telemed. J. E-Health 2016, 22, 809–815. [Google Scholar] [CrossRef] [PubMed]
- Buysse, H.E.; Coorevits, P.; Van Maele, G.; Hutse, A.; Kaufman, J.; Ruige, J.; De Moor, G.J. Introducing telemonitoring for diabetic patients: Development of a telemonitoring ‘Health Effect and Readiness’ questionnaire. Int. J. Med. Inform. 2010, 79, 576–584. [Google Scholar] [CrossRef] [PubMed]
- Biasutti, M.; Frate, S. A validity and reliability study of the attitudes toward sustainable development scale. Environ. Educ. Res. 2016, 23, 1–17. [Google Scholar] [CrossRef]
- Erdogan, M.; Ok, A.; Marcinkowski, T.J. Development and validation of children’s responsible environmental behavior scale. Environ. Educ. Res. 2012, 18, 507–540. [Google Scholar] [CrossRef]
- Kaiser, H.F. A second generation little jiffy. Psychometrika 1970, 35, 401–415. [Google Scholar] [CrossRef]
- Kurtuldu, M.K.; Bulut, D. Development of a self–efficacy scale toward piano lessons. Educ. Sci. Theory Pract. 2017, 17, 835–857. [Google Scholar] [CrossRef]
- Bentler, P.M.; Bonett, D.G. Significance tests and goodness of fit in the analysis of covariance structures. Psychol. Bull. 1980, 88, 588–606. [Google Scholar] [CrossRef]
- Bentler, P.M.; Kano, Y. On the equivalence of factors and components. Multivar. Behav. Res. 1990, 25, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Mu, G.M.; Hu, Y. Validation of the Chinese version of the 12-item child and youth resilience measure. Child. Youth Serv. Rev. 2016, 70, 332–339. [Google Scholar] [CrossRef]
- Polanco, N.T.; Solinis, R.N.; Arce, R.S.; Zabalegui, I.B. Development of a questionnaire to assess the collaboration between clinicians from different levels of care. Int. J. Integr. Care 2012, 12, e187. [Google Scholar] [CrossRef]
- Steiger, J.H.; Lind, J. Statistically based tests for the number of common factors. In Proceedings of the Annual Meeting of the Psychometric Society, Iowa City, IA, USA, 30 May 1980. [Google Scholar]
- Fornell, C.; Larcker, D.F. Evaluating structural equation models with unobservable variables and measurement error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- Sobral, M.P.; Costa, M.E.; Schmidt, L.; Martins, M.V. COMPI Fertility Problem Stress Scales is a brief, valid and reliable tool for assessing stress in patients seeking treatment. Hum. Reprod. 2016, 32, 375–382. [Google Scholar] [CrossRef] [PubMed]
- Jiang, S.; Street, R.L. Factors influencing communication with doctors via the Internet: A cross–sectional analysis of 2014 HINTS survey. Health Commun. 2017, 32, 180–188. [Google Scholar] [CrossRef] [PubMed]
- Kowalski, C.; Nitzsche, A.; Scheibler, F.; Steffen, P.; Albert, U.S.; Pfaff, H. Breast cancer patients’ trust in physicians: The impact of patients’ perception of physicians’ communication behaviors and hospital organizational climate. Patient Educ. Couns. 2009, 77, 344–348. [Google Scholar] [CrossRef] [PubMed]
| Demographic Characteristics | Number | Percentage | |
|---|---|---|---|
| (1) Age | <20 | 22 | 6.55% |
| 21–29 | 83 | 24.70% | |
| 30–39 | 107 | 31.84% | |
| 40–49 | 59 | 17.56% | |
| 50–59 | 47 | 13.99% | |
| 60 and above | 18 | 5.36% | |
| (2) Gender | Male | 156 | 46.43% |
| Female | 180 | 53.57% | |
| (3) Resident Status | Urban | 184 | 54.76% |
| Rural | 152 | 45.24% | |
| (4) Education Level | Junior middle school | 31 | 9.22% |
| High school | 96 | 28.57% | |
| Junior college | 68 | 20.24% | |
| Bachelor’s degree | 127 | 37.80% | |
| Master’s degree | 9 | 2.68% | |
| Doctor’s degree | 5 | 1.49% | |
| (5) Job | Private business owners | 28 | 8.33% |
| Factory workers | 31 | 9.23% | |
| Professional and technical workers | 77 | 22.92% | |
| Commercial service workers | 63 | 18.75% | |
| Students | 38 | 11.31% | |
| Liberal professionals | 27 | 8.04% | |
| Employees in government offices and public institutions | 40 | 11.90% | |
| Retirees | 22 | 6.55% | |
| Farmers | 10 | 2.98% | |
| Construct a | Cronbach’s α |
|---|---|
| MTIHIS | 0.854 |
| ETIHIS | 0.844 |
| PQIHI | 0.933 |
| SIHI | 0.891 |
| PS | 0.867 |
| TP | 0.842 |
| Total | 0.936 |
| Fit Indices | Values | Threshold for a Good Fit |
|---|---|---|
| Pearson’s Chi-square (χ2) | 1015.968 | - |
| Degrees of freedom (df) | 893 | - |
| χ2/df | 1.138 | <3 |
| Probability level (p) | 0.000 | <0.001 |
| Root mean square error of approximation (RMSEA) | 0.020 | <0.05 |
| Root mean square residual (RMR) | 0.078 | <1 |
| Goodness of fit index (GFI) | 0.895 | ≥0.900 |
| Comparative fit index (CFI) | 0.986 | ≥0.900 |
| Normed Fit Index (NFI) | 0.895 | ≥0.900 |
| Relative Fit Index (RFI) | 0.862 | ≥0.900 |
| Incremental Fit Index (IFI) | 0.986 | ≥0.900 |
| Tucker-Lewis Index (TLI) | 0.981 | ≥0.900 |
| Construct a | Mean | S.D. | CR | AVE | Sqrt AVE |
|---|---|---|---|---|---|
| MTIHIS | 4.685 | 0.827 | 0.878 | 0.591 | 0.769 |
| ETIHIS | 4.214 | 0.916 | 0.874 | 0.582 | 0.763 |
| PQIHI | 4.503 | 0.748 | 0.905 | 0.426 | 0.653 |
| SIHI | 4.473 | 0.822 | 0.847 | 0.445 | 0.667 |
| PS | 3.638 | 1.123 | 0.748 | 0.599 | 0.774 |
| TP | 4.180 | 0.826 | 0.915 | 0.522 | 0.723 |
| Construct a | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| MTIHIS | 0.769 | |||||
| ETIHIS | 0.291 | 0.763 | ||||
| PQIHI | 0.362 | 0.286 | 0.653 | |||
| SIHI | 0.305 | 0.295 | 0.749 | 0.667 | ||
| PS | −0.149 | −0.019 | −0.119 | −0.001 | 0.774 | |
| TP | 0.361 | 0.212 | 0.495 | 0.525 | 0.115 | 0.723 |
| Hypothesis | Path Coefficient | pa |
|---|---|---|
| H1: Mature treatments related Internet health information seeking (MTIHIS) has a positive impact on patients’ perceived quality of Internet health information (PQIHI). | 0.327 | *** |
| H2: Mature treatments related Internet health information seeking (MTIHIS) has a positive impact on patients’ satisfaction with Internet health information (SIHI). | 0.198 | *** |
| H3: Emerging treatments related Internet health information seeking (ETIHIS) has a negative impact on patients’ perceived quality of Internet health information (PQIHI). | 0.195 | 0.002 ** |
| H4: Emerging treatments related Internet health information seeking (ETIHIS) has a negative impact on patients’ satisfaction with Internet health information (SIHI). | 0.167 | 0.001 ** |
| H5: Patients’ perceived quality of Internet health information (PQIHI) has a positive impact on patients’ psychological safety (PS). | −0.540 | 0.002 ** |
| H6: Patients’ satisfaction with Internet health information (SIHI) has a positive impact on patients’ psychological safety (PS). | 0.618 | 0.018 * |
| H7: Patients’ psychological safety (PS) has a positive impact on patients’ trust in physicians (TP). | 0.150 | 0.045 * |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, R.; Lu, X.; Wu, W.; Shang, X.; Liu, M. Mature or Emerging? The Impact of Treatment-Related Internet Health Information Seeking on Patients’ Trust in Physicians. Int. J. Environ. Res. Public Health 2018, 15, 1855. https://doi.org/10.3390/ijerph15091855
Zhang R, Lu X, Wu W, Shang X, Liu M. Mature or Emerging? The Impact of Treatment-Related Internet Health Information Seeking on Patients’ Trust in Physicians. International Journal of Environmental Research and Public Health. 2018; 15(9):1855. https://doi.org/10.3390/ijerph15091855
Chicago/Turabian StyleZhang, Runtong, Xinyi Lu, Wen Wu, Xiaopu Shang, and Manlu Liu. 2018. "Mature or Emerging? The Impact of Treatment-Related Internet Health Information Seeking on Patients’ Trust in Physicians" International Journal of Environmental Research and Public Health 15, no. 9: 1855. https://doi.org/10.3390/ijerph15091855
APA StyleZhang, R., Lu, X., Wu, W., Shang, X., & Liu, M. (2018). Mature or Emerging? The Impact of Treatment-Related Internet Health Information Seeking on Patients’ Trust in Physicians. International Journal of Environmental Research and Public Health, 15(9), 1855. https://doi.org/10.3390/ijerph15091855





