Psychosocial Problems, Indoor Air-Related Symptoms, and Perceived Indoor Air Quality among Students in Schools without Indoor Air Problems: A Longitudinal Study
Abstract
1. Introduction
1.1. Psychosocial Problems, Subjective IAQ, and IA-Related Symptoms in Schools
1.2. Present Study
2. Materials and Methods
2.1. Participants and Data Collection
2.2. Ethical Considerations
2.3. Measures
2.3.1. Outcome Variables (Time 2)
2.3.2. Predictors (Times 1 and 2)
2.3.3. Background Variables (Times 1 and 2)
2.4. Defining Schools without IA Problems
2.5. Statistical Analysis
3. Results
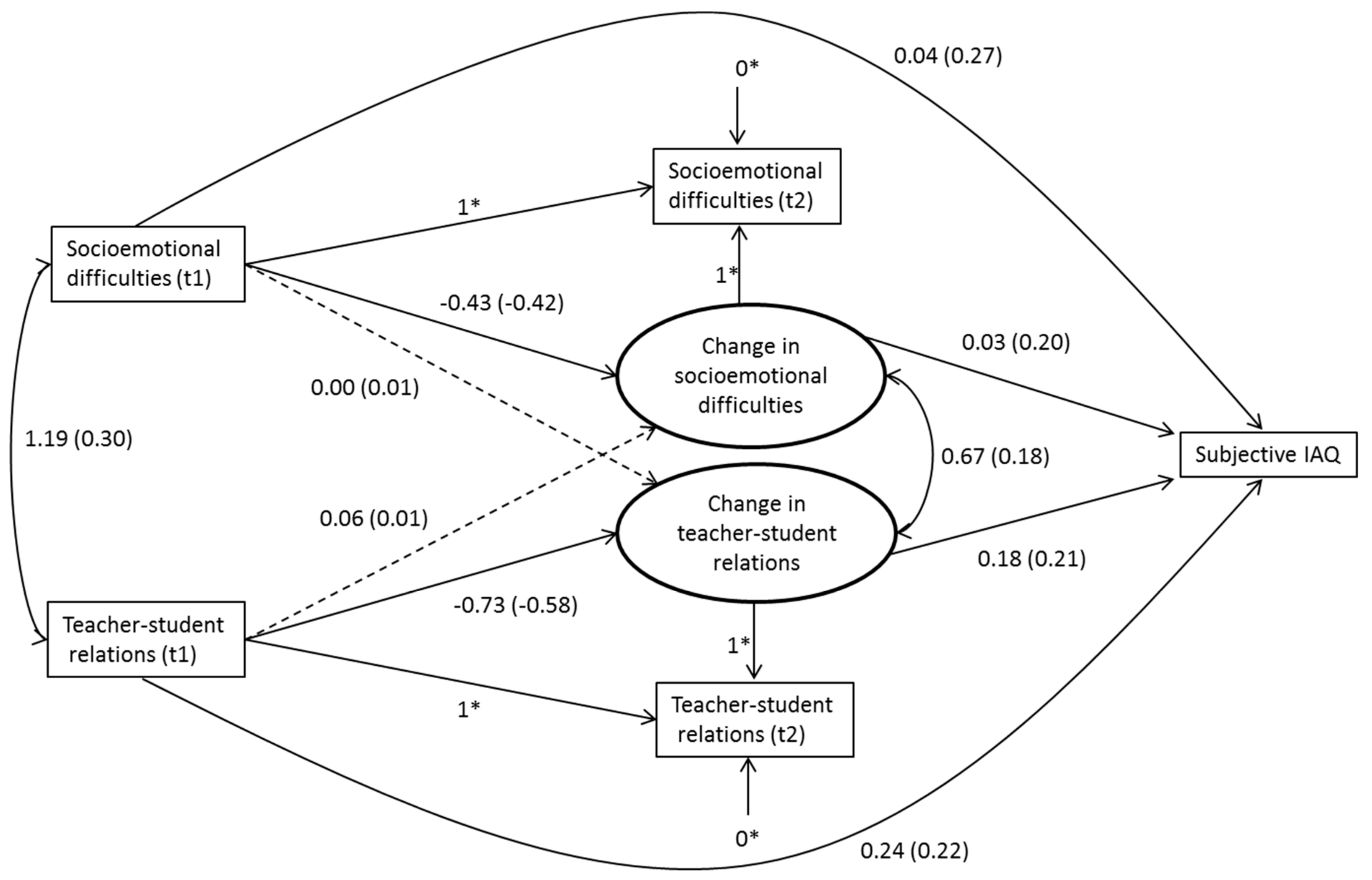
3.1. Associations between Psychosocial Predictors and Subjective IAQ
3.2. Associations between Psychosocial Predictors and IA-Related Symptoms
4. Discussion
Strengths, Limitations, and Future Research
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Dutton, S.; Chan, W.; Mendell, M.; Barrios, M.; Parthasarathy, S.; Sidheswaran, M.; Sullivan, D.; Eliseeva, K.; Fisk, W. Evaluation of the Indoor Air Quality Procedure for Use in Retail Buildings; Lawrence Berkeley National Laboratory: Berkeley, CA, USA, 2013; Available online: http://escholarship.org/uc/item/9v05h2r3 (accessed on 5 February 2018).
- Hellgren, U.-M.; Hyvärinen, M.; Holopainen, R.; Reijula, K. Perceived indoor air quality, air-related symptoms and ventilation in Finnish hospitals. Int. J. Occup. Med. Environ. Health 2011, 24, 48–56. [Google Scholar] [CrossRef] [PubMed]
- Ung-Lanki, S.; Lampi, J.; Pekkanen, J. Analyzing symptom data in indoor air questionnaires for primary schools. Indoor Air 2017, 27, 900–908. [Google Scholar] [CrossRef] [PubMed]
- Pereira, L.D.; Raimondo, D.; Corgnati, S.P.; da Silva, M.G. Assessment of indoor air quality and thermal comfort in Portuguese secondary classrooms: Methodology and results. Build. Environ. 2014, 81, 69–80. [Google Scholar] [CrossRef]
- Bakke, J.V.; Moen, B.E.; Wieslander, G.; Norbäck, D. Gender and the physical and psychosocial work environments are related to indoor air symptoms. J. Occup. Environ. Med. 2007, 49, 641–650. [Google Scholar] [CrossRef] [PubMed]
- Mečiarová, Ľ.; Vilčeková, S.; Burdová, E.K.; Kapalo, P.; Mihaľová, N. The real and subjective indoor environmental quality in schools. Int. J. Environ. Health Res. 2018, 28, 102–123. [Google Scholar] [CrossRef] [PubMed]
- Simoni, M.; Baldacci, S.; Canciani, M.; Pini, C.; Brunetti, L.M.; Indinnimeo, L.; Carrer, P.; Biggeri, A.; Sestini, P.; Maio, S.; et al. How do children perceive indoor air quality (IAQ) at school? Eur. Respir. J. 2016, 48 (Suppl. 60), PA4923. [Google Scholar] [CrossRef]
- Jaakkola, M.S.; Quansah, R.; Hugg, T.T.; Heikkinen, S.A.M.; Jaakkola, J.J.K. Association of indoor dampness and molds with rhinitis risk: A systematic review and meta-analysis. J. Allergy Clin. Immunol. 2013, 132, 1099–1110. [Google Scholar] [CrossRef] [PubMed]
- Mendell, M.J.; Mirer, A.G.; Cheung, K.; Tong, M.; Douwes, J. Respiratory and allergic health effects of dampness, mold, and dampness-related agents: A review of the epidemiologic evidence. Environ. Health Perspect. 2011, 119, 748–756. [Google Scholar] [CrossRef] [PubMed]
- Tischer, C.; Chen, C.-M.; Heinrich, J. Association between domestic mould and mould components, and asthma and allergy in children: A systematic review. Eur. Respir. J. 2011, 38, 812–824. [Google Scholar] [CrossRef] [PubMed]
- Brauer, C.; Mikkelsen, S. The influence of individual and contextual psychosocial work factors on the perception of the indoor environment at work: A multilevel analysis. Int. Arch. Occup. Environ. Health 2010, 83, 639–651. [Google Scholar] [CrossRef] [PubMed]
- Frontczak, M.; Wargocki, P. Literature survey on how different factors influence human comfort in indoor environments. Build. Environ. 2011, 46, 922–937. [Google Scholar] [CrossRef]
- Bluyssen, P.M.; Roda, C.; Mandin, C.; Fossati, S.; Carrer, P.; de Kluizenaar, Y.; Mihucz, V.G.; de Oliveira Fernandes, E.; Bartzis, J. Self-reported health and comfort in “modern” office buildings: First results from the European OFFICAIR study. Indoor Air 2016, 26, 298–317. [Google Scholar] [CrossRef] [PubMed]
- Amritwar, A.U.; Lowry, C.A.; Brenner, L.A.; Hoisington, A.J.; Stiller, J.W.; Hamilton, R.; Stiller, J.W.; Postolache, T.T. Mental health in allergic rhinitis: Depression and suicidal behavior. Curr. Treat. Options Allergy 2017, 4, 71–97. [Google Scholar] [CrossRef] [PubMed]
- Cheng, H.; Deighton, J.; Wolpert, M.; Chapman, B.P.; Kornilaki, E.N.; Treglown, L.; Furnham, A. Hay fever in childhood, traits neuroticism and conscientiousness as independent predictors of the occurrence of hay fever in adulthood. J. Health Psychol. 2016, 21, 2367–2375. [Google Scholar] [CrossRef] [PubMed]
- Tsiakiris, G.; Neely, G.; Lind, N.; Nordin, S. Comorbidity in allergic asthma and allergic rhinitis: Functional somatic syndromes. Psychol. Health Med. 2017, 22, 1163–1168. [Google Scholar] [CrossRef] [PubMed]
- Uçal, Y.O.; Tansuker, H.D.; Bakım, B.; Yıldırım, Ö.; Sözen, E.; Uslu Coşkun, B. Psychiatric analysis of treatment-resistant allergic rhinitis and evaluation of the effects of antidepressant use. ENT Updates 2017, 7, 9–16. [Google Scholar] [CrossRef]
- Basara, L.; Begic, N.; Grle, S.; Jakopovic, M.; Samaržija, M. Dyspnea from neuropsychiatric perspective: A narrative review. Psychiatr. Danub. 2018, 30, 11–20. [Google Scholar] [CrossRef] [PubMed]
- De Peuter, S.; Van Diest, I.; Lemaigre, V.; Verleden, G.; Demedts, M.; Van den Bergh, O. Dyspnea: The role of psychological processes. Clin. Psychol. Rev. 2004, 24, 557–581. [Google Scholar] [CrossRef] [PubMed]
- Janssens, T.; Verleden, G.; De Peuter, S.; Van Diest, I.; Van den Bergh, O. Inaccurate perception of asthma symptoms: A cognitive-affective framework and implications for asthma treatment. Clin. Psychol. Rev. 2009, 29, 317–327. [Google Scholar] [CrossRef] [PubMed]
- Hulme, K.; Deary, V.; Dogan, S.; Parker, S.M. Psychological profile of individuals presenting with chronic cough. ERJ Open Res. 2017, 3, 00099–2016. [Google Scholar] [CrossRef] [PubMed]
- Csobod, E.; Annesi-Maesano, I.; Carrer, P.; Kephalopoulos, S.; Madureira, J.; Rudnai, P.; de Oliveira Fernandes, E. Sinphonie. Schools Indoor Pollution and Health. Observatory Network in Europe. Final Report; European Union: Luxembourg, 2014. [Google Scholar]
- Simoni, M.; Annesi-Maesano, I.; Sigsgaard, T.; Norback, D.; Wieslander, G.; Nystad, W.; Canciani, M.; Sestini, P.; Viegi, G. School air quality related to dry cough, rhinitis and nasal patency in children. Eur. Respir. J. 2010, 35, 742–749. [Google Scholar] [CrossRef] [PubMed]
- Haverinen-Shaughnessy, U.; Shaughnessy, R.J. Effects of classroom ventilation rate and temperature on students’ test scores. PLoS ONE 2015, 10, e0136165. [Google Scholar] [CrossRef] [PubMed]
- Simons, E.; Hwang, S.-A.; Fitzgerald, E.F.; Kielb, C.; Lin, S. The impact of school building conditions on student absenteeism in upstate New York. Am. J. Public Health 2010, 100, 1679–1686. [Google Scholar] [CrossRef] [PubMed]
- Finell, E.; Tolvanen, A.; Haverinen-Shaughnessy, U.; Laaksonen, S.; Karvonen, S.; Sund, R.; Luopa, P.; Pekkanen, J.; Ståhl, T. Indoor air problems and the perceived social climate in schools: A multilevel structural equation analysis. Sci. Total Environ. 2018, 624, 1504–1512. [Google Scholar] [CrossRef] [PubMed]
- Haverinen-Shaughnessy, U.; Borras-Santos, A.; Turunen, M.; Zock, J.-P.; Jacobs, J.; Krop, E.J.M.; Casas, L.; Shaughnessy, R.; Täubel, M.; Heederik, D.; et al. Occurrence of moisture problems in schools in three countries from different climatic regions of Europe based on questionnaires and building inspections—The HITEA study. Indoor Air 2012, 22, 457–466. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). School Environment: Policies and Current Status; WHO Regional Office for Europe: Copenhagen, Denmark, 2015. [Google Scholar]
- Hansen, Å.M.; Meyer, H.W.; Gyntelberg, F. Building-related symptoms and stress indicators. Indoor Air 2008, 18, 440–446. [Google Scholar] [CrossRef] [PubMed]
- Norbäck, D.; Torgén, M.; Edling, C. Volatile organic compounds, respirable dust, and personal factors related to prevalence and incidence of sick building syndrome in primary schools. Br. J. Ind. Med. 1990, 47, 733–741. [Google Scholar] [CrossRef] [PubMed]
- Smedje, G.; Norbäck, D.; Edling, C. Subjective indoor air quality in schools in relation to exposure. Indoor Air 1997, 7, 143–150. [Google Scholar] [CrossRef]
- Finell, E.; Haverinen-Shaughnessy, U.; Tolvanen, A.; Laaksonen, S.; Karvonen, S.; Sund, R.; Saaristo, V.; Luopa, P.; Ståhl, T.; Putus, T.; et al. The associations of indoor environment and psychosocial factors on subjective evaluation of indoor air quality among lower secondary school students: A multilevel analysis. Indoor Air 2017, 27, 329–337. [Google Scholar] [CrossRef] [PubMed]
- Savelieva, K.; Ung-Lanki, S.; Lampi, J.; Elovainio, M.; Pekkanen, J. Psychosocial factors and symptom reporting in indoor air questionnaires among primary and secondary students. J. Psychosom. Res. 2018, 109, 131–132. [Google Scholar] [CrossRef]
- Hammen, C. Stress and depression. Annu. Rev. Clin. Psychol. 2005, 1, 293–319. [Google Scholar] [CrossRef] [PubMed]
- Lätsch, A. Do perceived helpfulness and competition in classroom contexts moderate or mediate the association between perceived stress and socio-emotional strengths and difficulties from early to middle adolescence? Learn. Individ. Differ. 2017, 58, 31–40. [Google Scholar] [CrossRef]
- Sigfusdottir, I.D.; Kristjansson, A.L.; Agnew, R. Comparative analysis of general strain theory. J. Crim. Justice 2012, 40, 117–127. [Google Scholar] [CrossRef]
- Chida, Y.; Hamer, M.; Steptoe, A. A bidirectional relationship between psychosocial factors and atopic disorders: A systematic review and meta-analysis. Psychosom. Med. 2008, 70, 102–116. [Google Scholar] [CrossRef] [PubMed]
- Dave, N.D.; Xiang, L.; Rehm, K.E.; Marshall, G.D. Stress and allergic diseases. Immunol. Allergy Clin. N. Am. 2011, 31, 55–68. [Google Scholar] [CrossRef] [PubMed]
- Finell, E.; Seppälä, T. Indoor air problems and experiences of injustice in the workplace: A quantitative and a qualitative study. Indoor Air 2018, 28, 125–134. [Google Scholar] [CrossRef] [PubMed]
- Lahtinen, M.; Huuhtanen, P.; Kähkönen, E.; Reijula, K. Psychosocial dimensions of solving an indoor air problem. Indoor Air 2002, 12, 33–46. [Google Scholar] [CrossRef] [PubMed]
- Karvala, K.; Uitti, J.; Luukkonen, R.; Nordman, H. Quality of life of patients with asthma related to damp and moldy work environments. Scand. J. Work. Environ. Health 2013, 39, 96–105. [Google Scholar] [CrossRef] [PubMed]
- Laviolette, L.; Laveneziana, P. Dyspnoea: A multidimensional and multidisciplinary approach. Eur. Respir. J. 2014, 43, 1750–1762. [Google Scholar] [CrossRef] [PubMed]
- Kinnunen, J.M.; Ollila, H.; Minkkinen, J.; Lindfors, P.L.; Rimpelä, A. A longitudinal study of predictors for adolescent electronic cigarette experimentation and comparison with conventional smoking. Int. J. Environ. Res. Public Health 2018, 15, 305. [Google Scholar] [CrossRef] [PubMed]
- Minkkinen, J.; Lindfors, P.L.; Kinnunen, J.M.; Finell, E.; Vainikainen, M.-P.; Karvonen, S.; Rimpelä, A. Health as a predictor of students’ academic achievement: A 3-level longitudinal study of Finnish adolescents. J. Sch. Health 2017, 87, 902–910. [Google Scholar] [CrossRef] [PubMed]
- Brauer, C.; Budtz-Jørgensen, E.; Mikkelsen, S. Structural equation analysis of the causal relationship between health and perceived indoor environment. Int. Arch. Occup. Environ. Health 2008, 81, 769–776. [Google Scholar] [CrossRef] [PubMed]
- Goodman, R.; Meltzer, H.; Bailey, V. The strengths and difficulties questionnaire: A pilot study on the validity of the self-report version. Eur. Child Adolesc. Psychiatry 1998, 7, 125–130. [Google Scholar] [CrossRef] [PubMed]
- Koskelainen, M. The Strengths and Difficulties Questionnaire among Finnish Children and Adolescents; University of Turku, Department of Child Psychiatry: Turku, Finland, 2008; Available online: https://www.utupub.fi/bitstream/handle/10024/39796/D809.pdf (accessed on 16 May 2018).
- Koskelainen, M.; Sourander, A.; Kaljonen, A. The strengths and difficulties questionnaire among Finnish school-aged children and adolescents. Eur. Child Adolesc. Psychiatry 2000, 9, 277–284. [Google Scholar] [CrossRef] [PubMed]
- Karvonen, S.; Vikat, A.; Rimpelä, M. The role of school context in the increase in young people’s health complaints in Finland. J. Adolesc. 2005, 28, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Virtanen, M.; Kivimäki, M.; Luopa, P.; Vahtera, J.; Elovainio, M.; Jokela, J.; Pietikainen, M. Staff reports of psychosocial climate at school and adolescents’ health, truancy and health education in Finland. Eur. J. Public Health 2009, 19, 554–560. [Google Scholar] [CrossRef] [PubMed]
- Hietanen-Peltola, M.; Korpilahti, U. Terveellinen, Turvallinen ja Hyvinvoiva Oppilaitos. Opas Ympäristön ja Yhteisön Monialaiseen Tarkastamiseen (A Healthy, Safe and Wellbeing School: A Guide to the Multidisciplinary Inspection of the Environment and the Community); THL: Helsinki, Finland, 2015; Available online: http://www.julkari.fi/bitstream/handle/10024/126936/URN_ISBN_978-952-302-505-9.pdf (accessed on 16 May 2018).
- Steyer, R.; Eid, M.; Schwenkmezger, P. Modeling true intraindividual change: True change as a latent variable. Methods Psychol. Res. Online 1997, 2, 21–33. [Google Scholar]
- Muthén, L.K.; Muthén, B.O. Mplus User’s Guide, 7th ed.; Muthén & Muthén: Los Angeles, CA, USA, 1998–2012; Available online: https://www.statmodel.com/download/usersguide/Mplus%20user%20guide%20Ver_7_r6_web.pdf (accessed on 1 June 2018).
- Maas, C.J.M.; Hox, J.J. Sufficient sample sizes for multilevel modeling. Methodology 2005, 1, 86–92. [Google Scholar] [CrossRef]
- Hox, J.J. Multilevel Analysis: Techniques and Applications, 2nd ed.; Routledge: New York, NY, USA, 2010. [Google Scholar]
- Muthén, B.O. Mplus Technical Appendices; Muthén & Muthén: Los Angeles, CA, USA, 1998–2004; Available online: https://www.statmodel.com/download/techappen.pdf (accessed on 1 June 2018).
- Rubin, D.B. Inference and missing data. Biometrika 1976, 63, 581–592. [Google Scholar] [CrossRef]
- Enders, C.; Bandalos, D. The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Struct. Equ. Model. Multidiscip. J. 2001, 8, 430–457. [Google Scholar] [CrossRef]
- Barnett, A.G.; van der Pols, J.C.; Dodson, A.J. Regression to the mean: What it is and how to deal with it. Int. J. Epidemiol. 2005, 34, 215–220. [Google Scholar] [CrossRef] [PubMed]
- Magnavita, N. Work-related symptoms in indoor environments: A puzzling problem for the occupational physician. Int. Arch. Occup. Environ. Health 2015, 88, 185–196. [Google Scholar] [CrossRef] [PubMed]
- Lampi, J.; Ung-Lanki, S.; Santalahti, P.; Pekkanen, J. Test-retest repeatability of child’s respiratory symptoms and perceived indoor air quality—Comparing self- and parent-administered questionnaires. BMC Pulm. Med. 2018, 18, 32. [Google Scholar] [CrossRef] [PubMed]
- Goodman, R. Psychometric properties of the strengths and difficulties questionnaire. J. Am. Acad. Child Adolesc. Psychiatry 2001, 40, 1337–1345. [Google Scholar] [CrossRef] [PubMed]
- Lahtinen, M.; Huuhtanen, P.; Vähämäki, K.; Kähkönen, E.; Mussalo-Rauhamaa, H.; Reijula, K. Good practices in managing work-related indoor air problems: A psychosocial perspective. Am. J. Ind. Med. 2004, 46, 71–85. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). WHO Guidelines for Indoor Air Quality: Dampness and Mould; WHO Regional Office for Europe: Copenhagen, Denmark, 2009; Available online: http://www.who.int/airpollution/guidelines/dampness-mould/en/ (accessed on 12 July 2018).
- Torresin, S.; Pernigotto, G.; Cappelletti, F.; Gasparella, A. Combined effects of environmental factors on human perception and objective performance: A review of experimental laboratory works. Indoor Air 2018, 28, 525–538. [Google Scholar] [CrossRef] [PubMed]

| N | % Or Mean | SD 2 | Min. | Max. | |
|---|---|---|---|---|---|
| Outcome variables ninth grade | |||||
| Subjective IAQ 1 | 959 | 1.90 | 0.81 | 1 | 4 |
| IA-related symptoms 1 | 971 | 1.66 | 0.63 | 1 | 4 |
| Predictors seventh grade | |||||
| Teacher–student relations 1 | 973 | 2.60 | 0.76 | 1 | 5 |
| Socioemotional difficulties 1 | 978 | 8.86 | 5.30 | 0 | 32 |
| Predictors ninth grade | |||||
| Teacher–student relations 1 | 961 | 2.74 | 0.80 | 1 | 5 |
| Socioemotional difficulties 1 | 968 | 10.88 | 5.74 | 0 | 30 |
| Background variables | |||||
| Gender (female %) | 495 | 50 | |||
| Ethnic background (Finnish- or Swedish-speaking %) | 916 | 94 | |||
| Parents’ highest education (%) | |||||
| Low | 52 | 6 | |||
| Middle | 524 | 58 | |||
| High | 327 | 36 | |||
| Asthma/allergy seventh grade (yes %) | 132 | 13 3 | |||
| Asthma/allergy ninth grade (yes %) | 243 | 25 3 |
| 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|
| 1. Subjective IAQ (t2) | 1 | ||||
| 2. IA-related symptoms (t2) | 0.26 *** | 1 | |||
| 3. Teacher–student relations (t1) | 0.15 *** | 0.09 * | 1 | ||
| 4. Socioemotional difficulties (t1) | 0.22 *** | 0.22 *** | 0.30 *** | 1 | |
| 5. Teacher–student relations (t2) | 0.24 *** | 0.10 * | 0.26 *** | 0.09 ** | 1 |
| 6. Socioemotional difficulties (t2) | 0.30 *** | 0.29 *** | 0.16 *** | 0.53 *** | 0.19 *** |
| Model 1: Predictors in Seventh Grade | Model 2: Predictors in Ninth Grade | |||
|---|---|---|---|---|
| 1 f | 2 g | 1 f | 2 g | |
| B (SE) | B (SE) | B (SE) | B (SE) | |
| Predictors seventh grade: | ||||
| Teacher–student relations (t1) a | 0.10 (0.033) ** | 0.10 (0.033) ** | ||
| Socioemotional difficulties (t1) a | 0.19 (0.024) *** | 0.18 (0.024) *** | ||
| Predictors ninth grade: | ||||
| Teacher–student relations (t2) a | 0.19 (0.043) *** | 0.19 (0.043) *** | ||
| Socioemotional difficulties (t2) a | 0.26 (0.032) *** | 0.26 (0.034) *** | ||
| Background variables: | ||||
| Gender b | −0.03 (0.030) | 0.01 (0.028) | ||
| Ethnic background c | −0.03 (0.026) | −0.02 (0.030) | ||
| Parents’ highest education d | −0.03 (0.035) | −0.01 (0.036) | ||
| Asthma/allergy (t1) e | 0.04 (0.042) | |||
| Asthma/allergy (t2) e | 0.04 (0.038) | |||
| R2 | 0.06 | 0.06 | 0.12 | 0.12 |
| Model 3: Predictors in Seventh Grade | Model 4: Predictors in Ninth Grade | |||
|---|---|---|---|---|
| 1 f | 2 g | 1 f | 2 g | |
| B (SE) | B (SE) | B (SE) | B (SE) | |
| Predictors seventh grade: | ||||
| Teacher–student relations (t1) a | 0.02 (0.042) | 0.03 (0.044) | ||
| Socioemotional difficulties (t1) a | 0.22 (0.031) *** | 0.21 (0.030) *** | ||
| Predictors ninth grade: | ||||
| Teacher–student relations (t2) a | 0.04 (0.037) | 0.05 (0.036) | ||
| Socioemotional difficulties (t2) a | 0.29 (0.037) *** | 0.26 (0.038) *** | ||
| Background variables: | ||||
| Gender b | −0.06 (0.026) * | −0.04 (0.030) | ||
| Ethnic background c | 0.01 (0.042) | 0.02 (0.034) | ||
| Parents’ highest education d | 0.03 (0.036) | 0.06 (0.033) | ||
| Asthma/allergy (t1) e | 0.12 (0.042) ** | |||
| Asthma/allergy (t2) e | 0.32 (0.038) *** | |||
| R2 | 0.05 | 0.07 | 0.09 | 0.19 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Finell, E.; Tolvanen, A.; Pekkanen, J.; Minkkinen, J.; Ståhl, T.; Rimpelä, A. Psychosocial Problems, Indoor Air-Related Symptoms, and Perceived Indoor Air Quality among Students in Schools without Indoor Air Problems: A Longitudinal Study. Int. J. Environ. Res. Public Health 2018, 15, 1497. https://doi.org/10.3390/ijerph15071497
Finell E, Tolvanen A, Pekkanen J, Minkkinen J, Ståhl T, Rimpelä A. Psychosocial Problems, Indoor Air-Related Symptoms, and Perceived Indoor Air Quality among Students in Schools without Indoor Air Problems: A Longitudinal Study. International Journal of Environmental Research and Public Health. 2018; 15(7):1497. https://doi.org/10.3390/ijerph15071497
Chicago/Turabian StyleFinell, Eerika, Asko Tolvanen, Juha Pekkanen, Jaana Minkkinen, Timo Ståhl, and Arja Rimpelä. 2018. "Psychosocial Problems, Indoor Air-Related Symptoms, and Perceived Indoor Air Quality among Students in Schools without Indoor Air Problems: A Longitudinal Study" International Journal of Environmental Research and Public Health 15, no. 7: 1497. https://doi.org/10.3390/ijerph15071497
APA StyleFinell, E., Tolvanen, A., Pekkanen, J., Minkkinen, J., Ståhl, T., & Rimpelä, A. (2018). Psychosocial Problems, Indoor Air-Related Symptoms, and Perceived Indoor Air Quality among Students in Schools without Indoor Air Problems: A Longitudinal Study. International Journal of Environmental Research and Public Health, 15(7), 1497. https://doi.org/10.3390/ijerph15071497





