Association between the General Practitioner Workforce Crisis and Premature Mortality in Hungary: Cross-Sectional Evaluation of Health Insurance Data from 2006 to 2014
Abstract
1. Introduction
2. Materials and Methods
3. Results
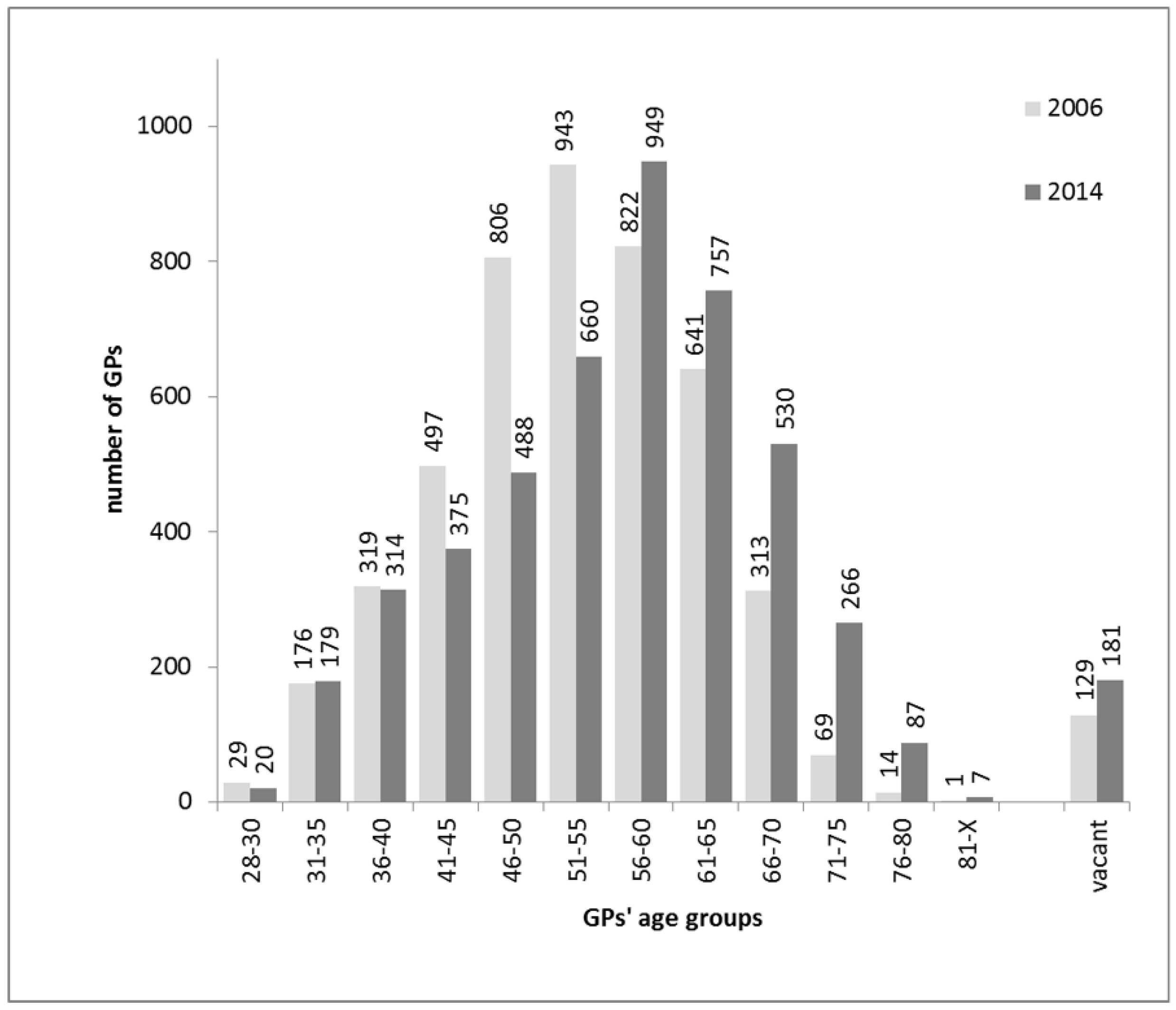
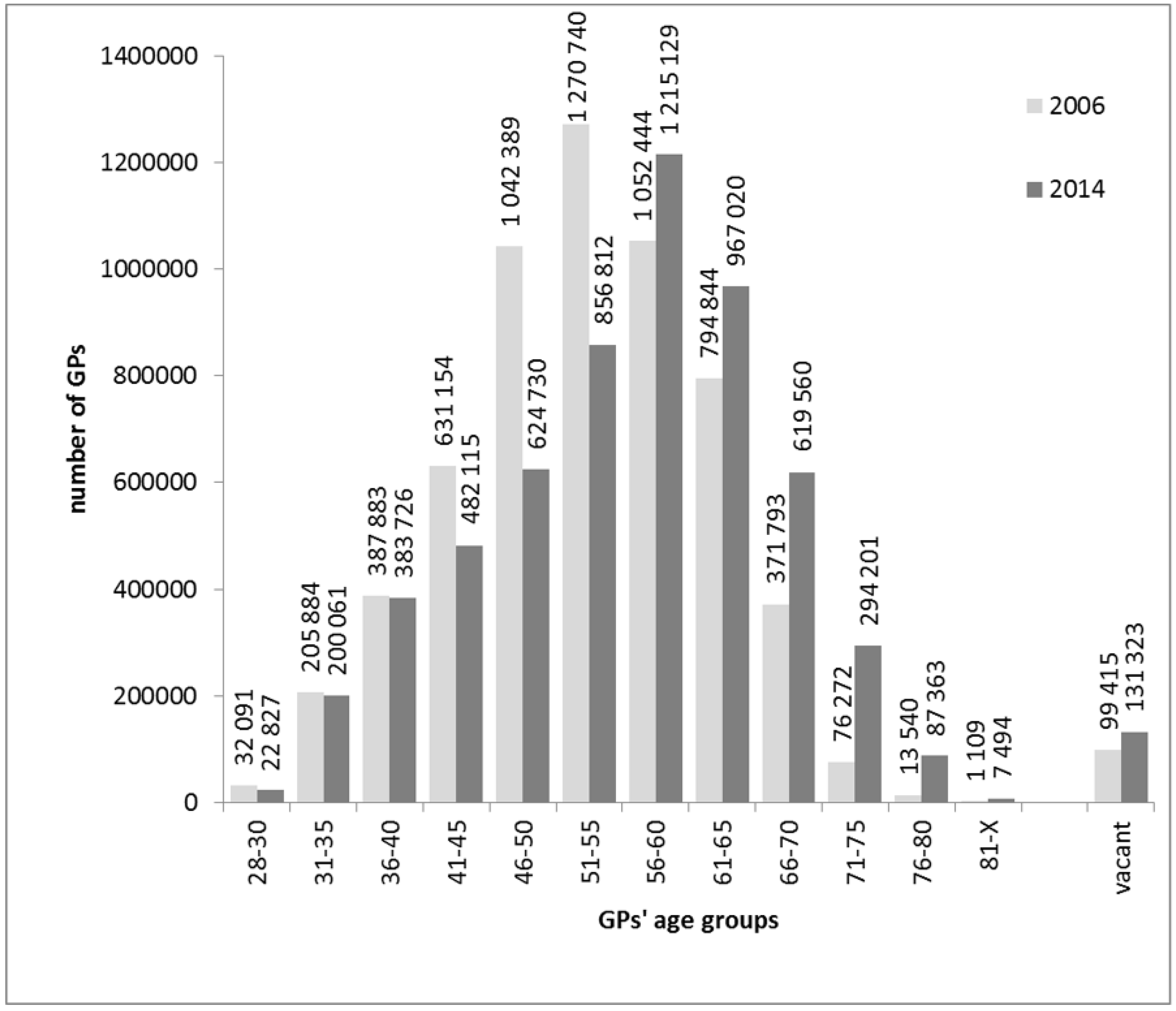
3.1. GMP Characteristics
3.2. GMP Characteristics by Vacancy Status and Age of GP
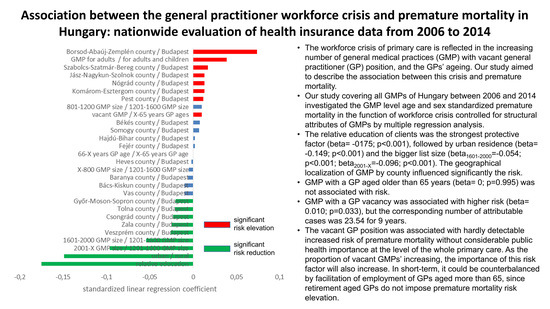
3.3. Risk Factors for Premature Death
4. Discussion
4.1. Main Findings
4.2. Other Findings
4.3. Observations in International Context
4.4. Strengths and Limitations
4.5. Further Research Needs
4.6. Implications
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| GP | general practitioner |
| GMP | general medical practice |
| rEDU | gender and age standardized relative education |
| PHC | primary health care |
| NHIF | National Health Insurance Fund |
| SMR | Standardized Mortality Ratio |
References
- Barriball, L.; Bremner, J.; Buchan, J.; Craveiro, I.; Dieleman, M.; Dix, O.; Dussault, G.; Jansen, C.; Kroezen, M.; Rafferty, A.M.; et al. Recruitment and Retention of the Health Workforce in Europe; Consumers, Health, Agriculture and Food Executive Agency of the European Commission: Brussels, Belgium, 2015. [Google Scholar]
- Bodenheimer, T.; Pham, H.H. Primary care: Current problems and proposed solutions. Health Affairs 2010, 29, 799–805. [Google Scholar] [CrossRef] [PubMed]
- Scott, I.A. Health care workforce crisis in Australia: Too few or too disabled? Med. J. Aust. 2009, 190, 689–692. [Google Scholar] [PubMed]
- European Commission. Towards a Job-Rich Recovery; Commission Staff Working Document on an Action Plan for the EU Health Workforce; European Commission: Brussels, Belgium, 2012. [Google Scholar]
- OECD. Health at a Glance: Europe 2010; OECD Publishing: Paris, France, 2010. [Google Scholar]
- Kringos, D.S.; Boerma, W.G.; Hutchinson, A.; Saltman, R.B. Building Primary Care in a Changing Europe; WHO Regional Office for Europe: Copenhagen, Denmark, 2015. [Google Scholar]
- Kringos, D.; Boerma, W.; Bourgueil, Y.; Cartier, T.; Dedeu, T.; Hasvold, T.; Hutchinson, A.; Lember, M.; Oleszczyk, M.; Rotar Pavlic, D.; et al. The strength of primary care in Europe: An international comparative study. Br. J. Gen. Pract. 2013, 63, e742–e750. [Google Scholar] [CrossRef] [PubMed]
- Dedeu, T.; Bolibar, B.; Gené, J.; Pareja, C.; Violan, C. Building Primary Care in a Changing Europe—Case Studies; European Observatory on Health Systems and Policies: Copenhagen, Denmark, 2015. [Google Scholar]
- WHO. Global Code of Practice on the International Recruitment of Health Personnel; WHO: Geneva, Switzerland, 2010. [Google Scholar]
- Delamaire, M.L.; Lafortune, G. Nurses in Advanced Roles: A Description and Evaluation of Experiences in 12 Developed Countries; OECD Health Working Paper No. 54; OECD: Paris, France, 2010. [Google Scholar]
- Roland, M.; Nolte, E. The future shape of primary care. Br. J. Gen. Pract. 2014, 64, 63–64. [Google Scholar] [CrossRef] [PubMed]
- Morgan, P.A.; Shah, N.D.; Kaufman, J.S.; Albanese, M.A. Impact of physician assistant care on office visit resource use in the United States. Health Serv. Res. 2008, 43, 1906–1922. [Google Scholar] [CrossRef] [PubMed]
- Scutchfield, F.D.; Michener, J.L.; Thacker, S.B. Are we there yet? Seizing the moment to integrate medicine and public health. Am. J. Public Health 2012, 102 (Suppl. 3), S312–S316. [Google Scholar] [CrossRef] [PubMed]
- Phillips, R.L., Jr.; Starfield, B. Why does a U.S. primary care physician workforce crisis matter? Am. Fam. Physician 2004, 70, 440. [Google Scholar] [PubMed]
- Pavlic, D.R.; Sever, M.; Klemenc-Ketis, Z.; Svab, I. Process quality indicators in family medicine: Results of an international comparison. BMC Fam. Pract. 2015, 16, 172. [Google Scholar] [CrossRef] [PubMed]
- Smatana, M.; Pazitny, P.; Kandilaki, D.; Laktisova, M.; Sedlakova, D.; Paluskova, M.; van Ginneken, E.; Spranger, A. Slovakia: Health System Review. Health Syst. Transit. 2016, 18, 1–210. [Google Scholar] [PubMed]
- Krzton-Krolewiecka, A.; Oleszczyk, M.; Schafer, W.; Boerma, W.G.; Windak, A. Quality of primary health care in Poland from the perspective of the physicians providing it. BMC Fam. Pract. 2016, 17, 151. [Google Scholar] [CrossRef] [PubMed]
- Murauskiene, L.; Janoniene, R.; Veniute, M.; van Ginneken, E.; Karanikolos, M. Lithuania: Health system review. Health Syst. Transit. 2013, 15, 1–150. [Google Scholar] [PubMed]
- WHO. European Health for All Database; WHO Regional Office for Europe: Copenhagen, Denmark, 2016. [Google Scholar]
- Box, G.E.; Cox, D.R. An Analysis of Transformations. J. R. Stat. Soc. Ser. B Stat. Methodol. 1964, 26, 211–252. [Google Scholar]
- Levene, L.S.; Bankart, J.; Khunti, K.; Baker, R. Association of primary care characteristics with variations in mortality rates in England: An observational study. PLoS ONE 2012, 7, e47800. [Google Scholar] [CrossRef] [PubMed]
- Baker, R.; Honeyford, K.; Levene, L.S.; Mainous, A.G., 3rd; Jones, D.R.; Bankart, M.J.; Stokes, T. Population characteristics, mechanisms of primary care and premature mortality in England: A cross-sectional study. BMJ Open 2016, 6, e009981. [Google Scholar] [CrossRef] [PubMed]
- Honeyford, K.; Baker, R.; Bankart, M.J.; Jones, D. Modelling factors in primary care quality improvement: A cross-sectional study of premature CHD mortality. BMJ Open 2013, 3, e003391. [Google Scholar] [CrossRef] [PubMed]
- Kontopantelis, E.; Springate, D.A.; Ashworth, M.; Webb, R.T.; Buchan, I.E.; Doran, T. Investigating the relationship between quality of primary care and premature mortality in England: A spatial whole-population study. BMJ 2015, 350, h904. [Google Scholar] [CrossRef] [PubMed]
- Juhasz, A.; Nagy, C.; Paldy, A.; Beale, L. Development of a Deprivation Index and its relation to premature mortality due to diseases of the circulatory system in Hungary, 1998–2004. Soc. Sci. Med. 2010, 70, 1342–1349. [Google Scholar] [CrossRef] [PubMed]
- Thomas, B.; Dorling, D.; Smith, G.D. Inequalities in premature mortality in Britain: Observational study from 1921 to 2007. BMJ 2010, 341, c3639. [Google Scholar] [CrossRef] [PubMed]
- Taulbut, M.; Walsh, D.; McCartney, G.; Parcell, S.; Hartmann, A.; Poirier, G.; Strniskova, D.; Hanlon, P. Spatial inequalities in life expectancy within postindustrial regions of Europe: A cross-sectional observational study. BMJ Open 2014, 4, e004711. [Google Scholar] [CrossRef] [PubMed]
- Rasella, D.; Harhay, M.O.; Pamponet, M.L.; Aquino, R.; Barreto, M.L. Impact of primary health care on mortality from heart and cerebrovascular diseases in Brazil: A nationwide analysis of longitudinal data. BMJ 2014, 349, g4014. [Google Scholar] [CrossRef] [PubMed]
- Shi, L.; Starfield, B. The effect of primary care physician supply and income inequality on mortality among blacks and whites in US metropolitan areas. Am. J. Public Health 2001, 91, 1246–1250. [Google Scholar] [CrossRef] [PubMed]
- Shin, D.W.; Cho, J.; Yang, H.K.; Park, J.H.; Lee, H.; Kim, H.; Oh, J.; Hwang, S.; Cho, B.; Guallar, E. Impact of continuity of care on mortality and health care costs: A nationwide cohort study in Korea. Ann. Fam. Med. 2014, 12, 534–541. [Google Scholar] [CrossRef] [PubMed]
- Choudhry, N.K.; Fletcher, R.H.; Soumerai, S.B. Systematic review: The relationship between clinical experience and quality of health care. Ann. Intern. Med. 2005, 142, 260–273. [Google Scholar] [CrossRef] [PubMed]
- Tsugawa, Y.; Newhouse, J.P.; Zaslavsky, A.M.; Blumenthal, D.M.; Jena, A.B. Physician age and outcomes in elderly patients in hospital in the US: Observational study. BMJ 2017, 357, j1797. [Google Scholar] [CrossRef] [PubMed]
- Saunders, C.; Abel, G. Ecological studies: Use with caution. Br. J. Gen. Pract. 2014, 64, 65–66. [Google Scholar] [CrossRef] [PubMed]
- Jakab, Z. Public health, primary care and the ‘cluster’ model. Eur. J. Public Health 2013, 23, 528. [Google Scholar] [CrossRef] [PubMed]
- Adany, R.; Kosa, K.; Sandor, J.; Papp, M.; Furjes, G. General practitioners’ cluster: A model to reorient primary health care to public health services. Eur. J. Public Health 2013, 23, 529–530. [Google Scholar] [CrossRef] [PubMed]
- Sandor, J.; Kosa, K.; Furjes, G.; Papp, M.; Csordas, A.; Rurik, I.; Adany, R. Public health services provided in the framework of general practitioners’ clusters. Eur. J. Public Health 2013, 23, 530–532. [Google Scholar] [CrossRef] [PubMed]
| GMP Characteristics | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2006–2014 |
|---|---|---|---|---|---|---|---|---|---|---|
| Providing service for adults and children (%) | 1475 | 1498 | 1480 | 1473 | 1476 | 1480 | 1487 | 1486 | 1481 | 13,336 |
| (30.99) | (31.41) | (30.95) | (30.77) | (30.80) | (30.83) | (30.93) | (30.96) | (30.77) | (30.93) | |
| Providing service for adults only (%) | 3284 | 3271 | 3302 | 3314 | 3316 | 3321 | 3321 | 3314 | 3332 | 29,775 |
| (69.01) | (68.59) | (69.05) | (69.23) | (69.20) | (69.17) | (69.07) | (69.04) | (69.23) | (69.07) | |
| Rural (%) | 1788 | 1802 | 1797 | 1796 | 1784 | 1665 | 1667 | 1624 | 1624 | 15,547 |
| (37.57) | (37.79) | (37.58) | (37.52) | (37.23) | (34.68) | (34.67) | (33.83) | (33.74) | (36.06) | |
| Urban (%) | 2971 | 2967 | 2985 | 2991 | 3008 | 3136 | 3141 | 3176 | 3189 | 27,564 |
| (62.43) | (62.21) | (62.42) | (62.48) | (62.77) | (65.32) | (65.33) | (66.17) | (66.26) | (63.94) | |
| Age of GP (%) | ||||||||||
| Vacant (%) | 129 | 149 | 127 | 121 | 127 | 135 | 149 | 166 | 181 | 1284 |
| (2.71) | (3.12) | (2.66) | (2.53) | (2.65) | (2.81) | (3.10) | (3.46) | (3.76) | (2.98) | |
| X-65 years | 4145 | 4067 | 4050 | 3990 | 3921 | 3870 | 3923 | 3694 | 3609 | 35,269 |
| (87.10) | (85.28) | (84.69) | (83.35) | (81.82) | (80.61) | (81.59) | (76.96) | (74.98) | (81.81) | |
| 66-X years | 485 | 553 | 605 | 676 | 744 | 796 | 736 | 940 | 1023 | 6558 |
| (10.19) | (11.60) | (12.65) | (14.12) | (15.53) | (16.58) | (15.31) | (19.58) | (21.25) | (15.21) | |
| Size of GMP (%) | ||||||||||
| X-800 clients | 83 | 108 | 101 | 102 | 110 | 127 | 401 | 141 | 157 | 1330 |
| (1.74) | (2.26) | (2.11) | (2.13) | (2.30) | (2.65) | (2,80) | (2.94) | (3.26) | (3.09) | |
| 801–1200 clients | 609 | 609 | 595 | 601 | 638 | 655 | 1523 | 663 | 670 | 6563 |
| (12.80) | (12.77) | (12.44) | (12.55) | (13.31) | (13.64) | (13,73) | (13.81) | (13.92) | (15.22) | |
| 1201–1600 clients | 1531 | 1500 | 1492 | 1484 | 1480 | 1477 | 1797 | 1495 | 1526 | 13,782 |
| (32.17) | (31.45) | (31.20) | (31.00) | (30.88) | (30.76) | (30,96) | (31.15) | (31.71) | (31.97) | |
| 1601–2000 clients | 1542 | 1580 | 1604 | 1600 | 1576 | 1555 | 810 | 1530 | 1508 | 13,305 |
| (32.40) | (33.13) | (33.54) | (33.42) | (32.89) | (32.39) | (32,14) | (31.88) | (31.33) | (30.86) | |
| 2001-X clients | 994 | 972 | 990 | 1000 | 988 | 987 | 277 | 971 | 952 | 8131 |
| (20.89) | (20.38) | (20.70) | (20.89) | (20.62) | (20.56) | (20,40) | (20.23) | (19.78) | (18.86) | |
| Standardized education (%) | ||||||||||
| Less than median level | 2373 | 2408 | 2384 | 2384 | 2387 | 2392 | 2394 | 2390 | 2386 | 21,498 |
| (49.86) | (50.49) | (49.85) | (49.80) | (49.81) | (49.82) | (49.79) | (49.79) | (49.57) | (49.87) | |
| Above median level | 2386 | 2361 | 2398 | 2403 | 2405 | 2409 | 2414 | 2410 | 2427 | 21,613 |
| (50.14) | (49.51) | (50.15) | (50.20) | (50.19) | (50.18) | (50.21) | (50.21) | (50.43) | (50.13) | |
| Number of premature deaths | 29,282 | 29,553 | 28,525 | 28,485 | 27,450 | 26,792 | 26,279 | 25,135 | 24,784 | 246,285 |
| Number of registered clients | 5,979,558 | 5,988,278 | 6,019,392 | 6,028,690 | 5,987,701 | 5,976,905 | 5,976,288 | 5,931,136 | 5,892,361 | 53,780,309 |
| Total number of GMPs | 4759 | 4769 | 4782 | 4787 | 4792 | 4801 | 4808 | 4800 | 4813 | 43,111 |
| GP Age X-65 Years | GP Age 66 ≤ Years | Vacant | Hungary | |
|---|---|---|---|---|
| Proportion of practices provided care for adults only | 69.46% [68.98–69.94] | 73.24% [72.17–74.31] | 36.84% [34.2–39.48] | 69.07% [68.63–69.5] |
| Proportion of urban practices | 64.39% [63.89–64.88] | 69.49% [68.37–70.6] | 23.29% [20.97–25.6] | 63.94% [63.48–64.39] |
| Proportion of practices with less than 800 list size | 1.86% [1.72–2.00] | 4.18% [3.69–4.66] | 31.15% [28.62–33.69] | 3.09% [2.92–3.25] |
| Proportion of practices with 801–1200 list size | 13.63% [13.27–13.98] | 19.91% [18.95–20.88] | 35.12% [32.51–37.74] | 15.22% [14.88–15.56] |
| Proportion of practices with 1201–1600 list size | 31.76% [31.28–32.25] | 34.78% [33.63–35.93] | 23.21% [20.9–25.52] | 31.97% [31.53–32.41] |
| Proportion of practices with 1601–2000 list size | 32.41% [31.92–32.9] | 26.94% [25.87–28.02] | 8.33% [6.82–9.85] | 30.86% [30.43–31.3] |
| Proportion of practices with more than 2000 list size | 50.11% [49.59–50.63] | 56.25% [55.05–57.45] | 19.47% [17.3–21.64] | 50.13% [49.66–50.61] |
| Above median standardized relative education of clients | 50.11% [49.59–50.63] | 56.25% [55.05–57.45] | 19.47% [17.3–21.64] | 50.13% [49.66–50.61] |
| Standardized mortality ratio | 0.996 [0.992–1.001] | 0.992 [0.981–1.002] | 1.247 [1.215–1.280] | 1 [0.996–1.004] |
| GMP Indicators | linear Regression Coefficient | p-Value | Standardized Linear Regression Coefficient | Semipartial Correlation Coefficient | Number of Attributable Cases |
|---|---|---|---|---|---|
| Type of GMP | |||||
| GMP for adults only/GMP for adults and children | 0.024 | <0.001 | 0.039 | 0.025 | 154.37 |
| urban/rural | −0.089 | <0.001 | −0.149 | −0.100 | −2441.45 |
| Age/vacancy of GP | |||||
| 66-X years GP age/X-65 years GP age | 0 | 0.995 | 0 | 0 | 0 |
| vacant GMP/X-65 years GP ages | 0.018 | 0.033 | 0.010 | 0.010 | 23.54 |
| Size of GMP | |||||
| X-800 GMP size/1201–1600 GMP size | −0.009 | 0.279 | −0.005 | −0.005 | −6.09 |
| 801–1200 GMP size/1201–1600 GMP size | 0.008 | 0.058 | 0.010 | 0.009 | 18.69 |
| 1601–2000 GMP size/1201–1600 GMP size | −0.033 | <0.001 | −0.054 | −0.045 | −509.24 |
| 2001-X GMP size/1201–1600 GMP size | −0.071 | <0.001 | −0.096 | −0.082 | −1647.91 |
| Relative education | |||||
| above median/less than median | −0.101 | <0.001 | −0.175 | −0.132 | −4316.52 |
| Counties: | |||||
| Bács-Kiskun county/Budapest | −0.013 | 0.062 | −0.010 | −0.009 | −18.12 |
| Baranya county/Budapest | −0.008 | 0.276 | −0.006 | −0.005 | −6.17 |
| Békés county/Budapest | 0.011 | 0.147 | 0.008 | 0.007 | 10.94 |
| Borsod-Abaúj-Zemplén county/Budapest | 0.080 | <0.001 | 0.074 | 0.061 | 909.57 |
| Csongrád county/Budapest | −0.034 | <0.001 | −0.023 | −0.021 | −108.18 |
| Fejér county/Budapest | 0.003 | 0.715 | 0.002 | 0.002 | 0.69 |
| Győr-Moson-Sopron county/Budapest | −0.029 | <0.001 | −0.02 | −0.018 | −81.13 |
| Hajdú-Bihar county/Budapest | 0.002 | 0.735 | 0.002 | 0.002 | 0.60 |
| Heves county/Budapest | −0.003 | 0.759 | −0.002 | −0.001 | −0.49 |
| Jász-Nagykun-Szolnok county/Budapest | 0.02 | 0.012 | 0.013 | 0.012 | 33.10 |
| Komárom-Esztergom county/Budapest | 0.023 | 0.008 | 0.013 | 0.012 | 36.43 |
| Nógrád county/Budapest | 0.025 | 0.008 | 0.013 | 0.012 | 36.32 |
| Pest county/Budapest | 0.012 | 0.036 | 0.012 | 0.010 | 22.83 |
| Somogy county/Budapest | 0.010 | 0.188 | 0.007 | 0.006 | 9.00 |
| Szabolcs-Szatmár-Bereg county/Budapest | 0.022 | 0.002 | 0.017 | 0.014 | 51.20 |
| Tolna county/Budapest | −0.038 | <0.001 | −0.021 | −0.019 | −88.55 |
| Vas county/Budapest | −0.017 | 0.056 | −0.010 | −0.009 | −18.94 |
| Veszprém county/Budapest | −0.041 | <0.001 | −0.026 | −0.023 | −135.19 |
| Zala county/Budapest | −0.043 | <0.001 | −0.025 | −0.023 | −131.9 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sándor, J.; Pálinkás, A.; Vincze, F.; Sipos, V.; Kovács, N.; Jenei, T.; Falusi, Z.; Pál, L.; Kőrösi, L.; Papp, M.; et al. Association between the General Practitioner Workforce Crisis and Premature Mortality in Hungary: Cross-Sectional Evaluation of Health Insurance Data from 2006 to 2014. Int. J. Environ. Res. Public Health 2018, 15, 1388. https://doi.org/10.3390/ijerph15071388
Sándor J, Pálinkás A, Vincze F, Sipos V, Kovács N, Jenei T, Falusi Z, Pál L, Kőrösi L, Papp M, et al. Association between the General Practitioner Workforce Crisis and Premature Mortality in Hungary: Cross-Sectional Evaluation of Health Insurance Data from 2006 to 2014. International Journal of Environmental Research and Public Health. 2018; 15(7):1388. https://doi.org/10.3390/ijerph15071388
Chicago/Turabian StyleSándor, János, Anita Pálinkás, Ferenc Vincze, Valéria Sipos, Nóra Kovács, Tibor Jenei, Zsófia Falusi, László Pál, László Kőrösi, Magor Papp, and et al. 2018. "Association between the General Practitioner Workforce Crisis and Premature Mortality in Hungary: Cross-Sectional Evaluation of Health Insurance Data from 2006 to 2014" International Journal of Environmental Research and Public Health 15, no. 7: 1388. https://doi.org/10.3390/ijerph15071388
APA StyleSándor, J., Pálinkás, A., Vincze, F., Sipos, V., Kovács, N., Jenei, T., Falusi, Z., Pál, L., Kőrösi, L., Papp, M., & Ádány, R. (2018). Association between the General Practitioner Workforce Crisis and Premature Mortality in Hungary: Cross-Sectional Evaluation of Health Insurance Data from 2006 to 2014. International Journal of Environmental Research and Public Health, 15(7), 1388. https://doi.org/10.3390/ijerph15071388