Rethinking the Role of the Public Health Clinic: Comparison of Outpatient Utilization in the Public Health Clinics and Private Clinics in Korea
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
References
- Shin, Y.; Lee, K. The health insurance system in Korea and its implications. World Hosp. Health Serv. 1995, 31, 3–9. [Google Scholar] [PubMed]
- Kim, S.R. The Supply of Beds in Korea and the Assessment of Optimal Supply of Beds. Seoul, 2002. Available online: http://www.snu-dhpm.ac.kr/pds/files/291-%EC%9D%98%EB%A3%8C%EC%8B%9C%EC%84%A4%EA%B3%84%ED%9A%8D_%EC%84%9C%EC%9A%B8%EB%8C%80_%EA%B0%95%EC%9D%98%EC%9A%A9021001.pdf (accessed on 22 March 2018). (In Korean).
- Statistics Korea, Health Care Facilities and Beds in Korea in 2008–2018. 2018. Available online: http://kosis.kr/statHtml/statHtml.do?orgId=110&tblId=DT_11001N_2013_A042# (accessed on 22 March 2018). (In Korean).
- Kim, A.M.; Cho, S.; Kim, H.J.; Jung, H.; Jo, M.W.; Lee, J.Y.; Eun, S.J. Primary Care Patients’ Preference for Hospitals over Clinics in Korea. Int. J. Environ. Res. Public Health 2018, 15, 1119. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health & Welfare, G-Health. 2017. Available online: http:/www.g-health.kr/portal/cts/view.do?cNo=200451&tab=1&menuNo=200456 (accessed on 22 March 2018).
- Statues of the Republic of Korea, Regional Public Health Act. 2016. Available online: http://law.go.kr/lsInfoP.do?lsiSeq=183596&chrClsCd=010203&urlMode=engLsInfoR&viewCls=engLsInfoR#0000 (accessed on 22 March 2018).
- Korea Foundation for International Healthcare Healthcare. Improvement Activities of Public Health Centers in Rural Areas. Ministry of Health and Welfare, 2012. Available online: http://www.who.int/pmnch/about/members/database/kofih/en/ (accessed on 22 March 2018). (In Korean).
- Statistics Korea, The classification of health care facilities In Seoul, Korea. 2017. Available online: http://kosis.kr/statHtml/statHtml.do?orgId=354&tblId=DT_HIRA43 (accessed on 8 February 2018). (In Korean).
- Lee, S.Y. Copayment Waiver for the Elderly in the Public Health Clinic Should Be Redressed. Doctors News. 30 November 2007. Available online: http://www.doctorsnews.co.kr/news/articleView.html?idxno=43846&sc_word= (accessed on 22 March 2018). (In Korean).
- Status of the Republic of Korea, Medical Service Act. 2017. Available online: https://elaw.klri.re.kr/eng_mobile/ganadaDetail.do?hseq=39874&type=abc&key=MEDICAL%20SERVICE%20ACT¶m=M (accessed on 22 March 2018).
- Ha, J.S. Uncomfortable Cohabitation between Private Health Care Facilities and the Public Health Center. Medical Observer. 25 February 2013. Available online: http://www.monews.co.kr/news/articleView.html?idxno=55289 (accessed on 22 March 2018). (In Korean).
- Jeon, K. Debate about the Legality of the Copayment Waiver in the Public Health Centers. Medical Times. 5 December 2003. Available online: http://medicaltimes.com/Users4/News/newsView.html?ID=4373 (accessed on 22 March 2018). (In Korean).
- Uhm, D.Y. Urban Public Health Subcenters Are Pork Barrelling. OhmyNews. 16 March 2010. Available online: http://blog.ohmynews.com/eomdy/260961 (accessed on 22 March 2018). (In Korean).
- Statistics Korea, Health Care Facilities 2008–2018. Seoul, Korea, 2018. Available online: http://kosis.kr/statHtml/statHtml.do?orgId=354&tblId=DT_MIRE01&conn_path=I3 (accessed on 22 March 2018). (In Korean).
- Kim, H.J.; Lee, J.Y.; Jo, M.W.; Eun, S.J. Investigating the Level of Competition between Public Health Centers and Private Clinics in Korea. Korean J. Hosp. Mgmt. 2016, 21, 37–49. [Google Scholar]
- Kim, L.; Kim, J.-A.; Kim, S. A guide for the utilization of Health Insurance Review and Assessment Service National Patient Samples. Epidemiol. Health 2014, 36. [Google Scholar] [CrossRef] [PubMed]
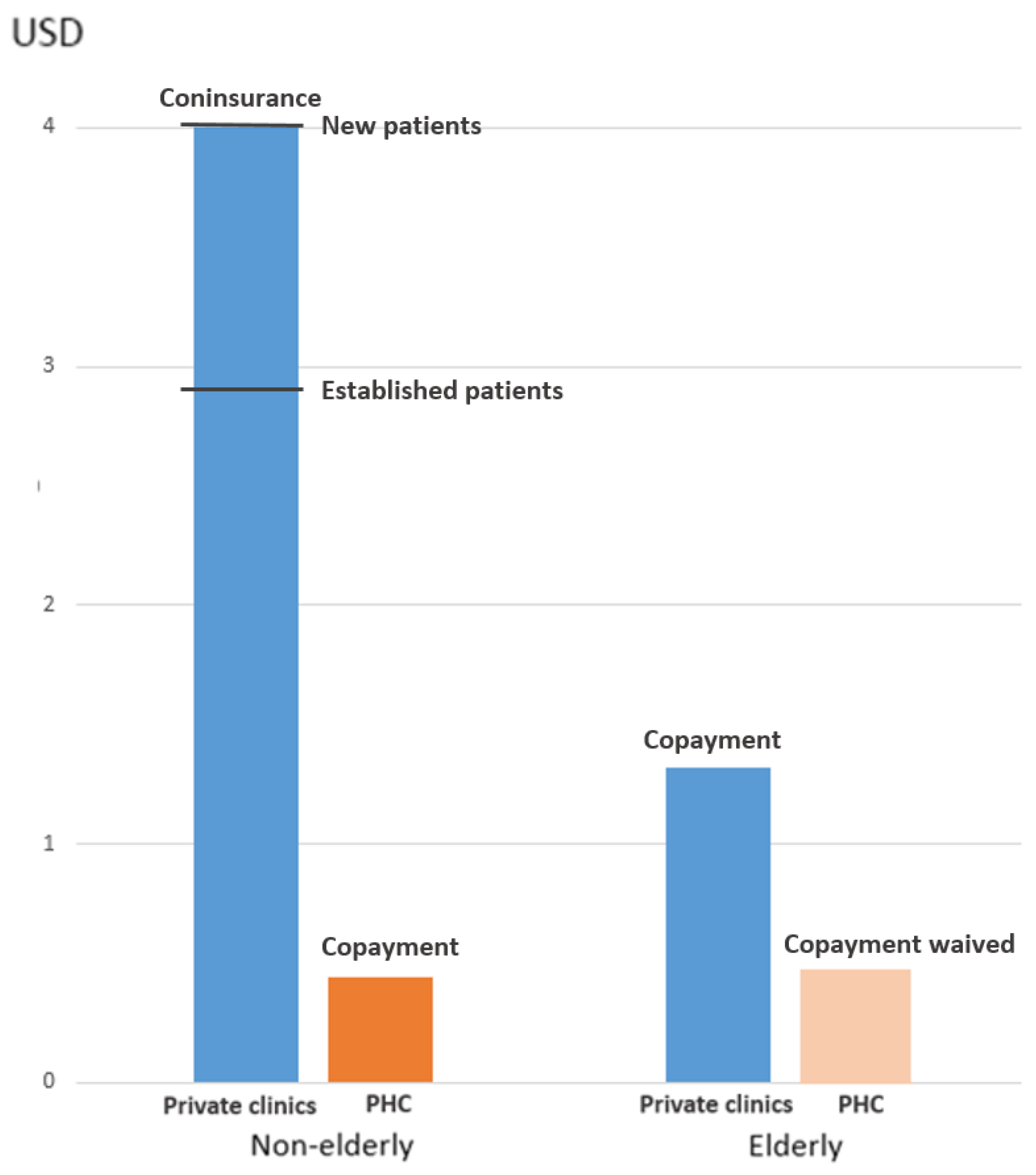
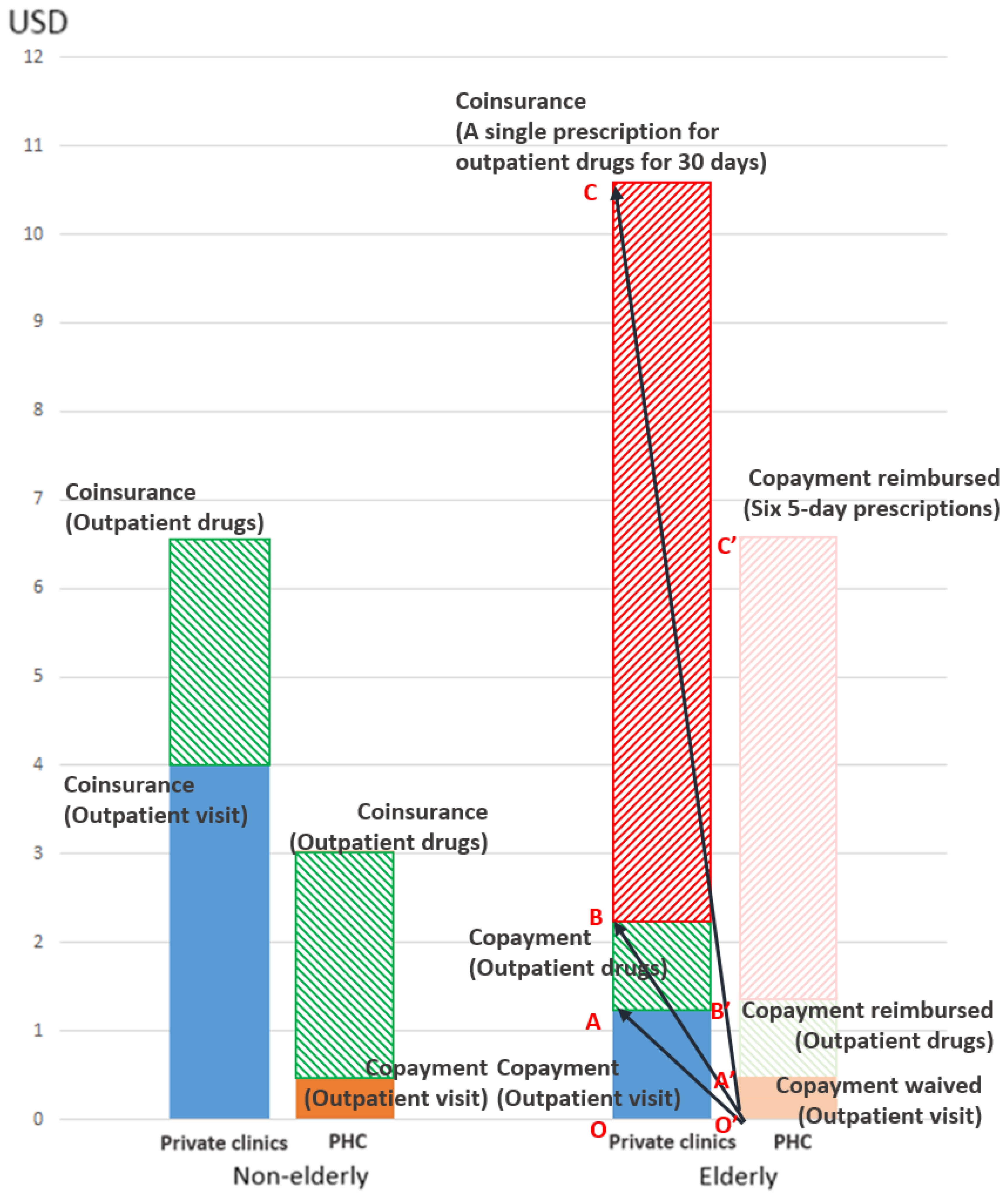
- Ministry of Health & Welfare. The Exception Criteria for out of Pocket Payment. Seoul, Korea, 2017. Available online: http://www.law.go.kr/%ED%96%89%EC%A0%95%EA%B7%9C%EC%B9%99/%EB%B3%B8%EC%9D%B8%EC%9D%BC%EB%B6%80%EB%B6%80%EB%8B%B4%EA%B8%88%20%EC%82%B0%EC%A0%95%ED%8A%B9%EB%A1%80%EC%97%90%20%EA%B4%80%ED%95%9C%20%EA%B8%B0%EC%A4%80 (accessed on 22 March 2018). (In Korean).
- Sundararajan, V.; Quan, H.; Halfon, P.; Fushimi, K.; Luthi, J.; Burnand, B.; Ghali, W. International Methodology Consortium for Coded Health Information (IMECCHI) Cross-national comparative performance of three versions of the ICD-10 Charlson index. Med. Care 2007, 45, 1210–1215. [Google Scholar] [CrossRef] [PubMed]
- Zeratsion, H.T. The Effect of Exemption from Co-Payment on Adolescent Utilization of Primary Health Care: The Case of Norway. Master’s Thesis, University of Oslo, Oslo, Norway, 2013. [Google Scholar]
- Khatami, S.; Xuan, L.; Roman, R.; Zhang, S.; McConnel, C.; Halm, E.A.; Gupta, S. Modestly increased use of colonoscopy when copayments are waived. Clin. Gastroenterol. Hepatol. 2012, 10, 761–766. [Google Scholar] [CrossRef] [PubMed]
- Department of Welfare and Health Plan for Support the COPAYMENt for Drugs for the Elderly. Seoul, Korea, 2013. Available online: http://yesan.seoul.go.kr/upload/4/4/6/kcube2700445053299728724.pdf (accessed on 22 March 2018). (In Korean).
- Cheonan, Support for the Copayment for Drugs for the Elderly. Cheonan: 2017. Available online: https://www.cheonan.go.kr/dhealth/sub04_01.do (accessed on 22 March 2018). (In Korean).
- Gangnam Community Health Center. The Invoice form from Pharmacies to the Public Health Clinics. Seoul, 2018. Available online: www.gangnam.go.kr/file/0/get/FILE_000000000068927/download.do (accessed on 22 May 2018). (In Korean).
- Lim, S. Arbitrary Support of Local Governments for the cOPAYMENT of Drugs for the Elderly. Kiho Ilbo. 3 April 2017. Available online: http://www.kihoilbo.co.kr/?mod=news&act=articleView&idxno=692453 (accessed on 22 March 2018). (In Korean).
- Health Insurance Review & Assessment Service. Cost Sharing for the Medical Aid Beneficiaries. 2017. Available online: http://m.hira.or.kr/pay/bur/06.do (accessed on 8 February 2018). (In Korean).
- Korea Medical Association, Annual Report Membership Statistics. Seoul, Korea, 2015. Available online: mdon.co.kr/news/download.html?no=4980&atno=11288 (accessed on 8 February 2018). (In Korean).
- Lachs, M.S.; Sindelar, J.L.; Horwitz, R.I. The forgiveness of coinsurance: charity or cheating? N. Engl. J. Med. 1990, 322, 1599–1602. [Google Scholar] [CrossRef] [PubMed]
- Dafny, L.; Ody, C.; Schmitt, M. When Discounts Raise Costs: The Effect of Copay Coupons on Generic Utilization. Available online: https://www.hbs.edu/faculty/Pages/item.aspx?num=51757 (accessed on 23 March 2018).
- Ubel, P. Copay assistance programs lead to higher healthcare costs. PharmacoEcon. Outcomes News 2016, 764, 1–22. [Google Scholar]
- Constitutional Court of Korea Decision on the Constitutionality of the Article of the Medical Service Act Which Punishes Patient Inducements by Copayment Reduction: Seoul. 2018. Available online: https://ecourt.ccourt.go.kr/coelec/websquare/websquare.html?w2xPath=/ui/coelec/dta/casesrch/EP4100_M01.xml&eventno=2016%ED%97%8C%EB%B0%94311 (accessed on 8 February 2018). (In Korean).
- Seoul Medical Association, Recommendation to the Health Insurance Review & Assessment Service. Seoul, 2008. Available online: https://m.blog.naver.com/PostView.nhn?blogId=39954&logNo=50120350696&proxyReferer=https%3A%2F%2Fwww.google.co.kr%2F (accessed on 8 February 2018). (In Korean).
- Lee, S.W. Ministry of Health & Welfare, “Waiver of Copayment in the Public Health Clinics Is NOT Illegal”. 2010. Available online: http://www.docdocdoc.co.kr/news/articleView.html?newscd=2010071200017 (accessed on 8 February 2018). (In Korean).
- Lee, J.Y.; Eun, S.J.; Kim, H.J.; Jo, M.-W. Finding the Primary Care Providers in the Specialist-Dominant Primary Care Setting of Korea: A Cluster Analysis. PLoS ONE 2016, 11, e0161937. [Google Scholar] [CrossRef] [PubMed]
- Yoon, J.R.; Moon, O.R.; Huh, J. Characteristics of Primary Health Practice and Diagnosis-Cluster Patterns in Health Insurance. Korean J. Health Policy Adm. 1993, 3, 100–129. [Google Scholar]
- Lee, H. Determinants of Outpatient Cost in Primary Care Setting in Korea. PhD Thesis, Korea University, Seoul, Korea, July 2014. (In Korean). [Google Scholar]
- Enforcement Decree of the National Health Insurance Act. Korea, 2017. Available online: http://www.law.go.kr/%EB%B2%95%EB%A0%B9/%EA%B5%AD%EB%AF%BC%EA%B1%B4%EA%B0%95%EB%B3%B4%ED%97%98%EB%B2%95%20%EC%8B%9C%ED%96%89%EB%A0%B9 (accessed on 8 February 2018). (In Korean).
- Health Insurance Review & Assessment Service, Guide to Cost-Sharing for Outpatient Visits. Health Insurance Review & Assessment Service: 2017. Available online: https://www.hira.or.kr/dummy.do?pgmid=HIRAA030056020110 (accessed on 22 March 2018). (In Korean).
- Health Insurance Review & Assessment Service, Calculation of Out-of-Pocket Expense for Outpatient Drugs. 2017. Available online: https://www.hira.or.kr/dummy.do?pgmid=HIRAA030037000000&isPopupYn=Y&isNewWindow=Y&cmsurl=/cms/popup/03/03/1341894_26965.html&subject=%EC%95%BD%EC%A0%9C%EB%B9%84%EA%B3%84%EC%82%B0%EC%8B%9D (accessed on 29 May 2018). (In Korean).
- Health Insurance Review & Assessment Service, Outpatient Drugs Expense Calculator. 2017. Available online: https://www.hira.or.kr/rf/medicine/calculator/form.do?pgmid=HIRAA030037000000 (accessed on 29 May 2018). (In Korean).
- Park, M.R. Top 10 Most Prescribed, Top Selling Drugs. Newspim. 24 November 2017. Available online: http://www.newspim.com/news/view/20171124000108 (accessed on 29 May 2018). (In Korean).
| Characteristic | No. of Outpatient Visits (%) | p-Value | ||
|---|---|---|---|---|
| Total | PHC 1 | Private Clinics | ||
| Total | 417,664,423 (100.0) | 11,798,425 (100.0) | 405,865,998 (100.0) | |
| Age group (years) | ||||
| 0–19 | 77,658,372 (18.6) | 232,464 (2.0) | 77,425,908 (19.1) | <0.001 |
| 20–39 | 70,478,935 (16.9) | 342,464 (2.9) | 70,136,471 (17.3) | |
| 40–64 | 162,393,179 (38.9) | 3,685,685 (31.2) | 158,707,494 (39.1) | |
| >64 | 107,133,938 (25.7) | 7,537,812 (63.9) | 99,596,126 (24.5) | |
| Gender | ||||
| Female | 244,815,159 (58.0) | 6,900,386 (58.5) | 237,914,773 (58.6) | <0.001 |
| Male | 172,849,264 (41.4) | 4,898,039 (41.5) | 167,951,225 (41.4) | |
| Type of health insurance | ||||
| NHI 2 | 397,902,947 (95.3) | 11,160,933 (94.6) | 386,742,014 (95.3) | <0.001 |
| Medical Aid | 19,761,477 (4.7) | 637,492 (5.4) | 19,123,984 (4.7) | |
| Region | ||||
| Metropolitan | 283,169,896 (67.8) | 4,260,084 (36.1) | 278,909,813 (68.7) | <0.001 |
| Non-metropolitan | 134,494,527 (32.2) | 7,538,341 (63.9) | 126,956,186 (31.3) | |
| Visits for SMDGs 4 | ||||
| Yes | 332,383,732 (79.6) | 8,347,599 (70.8) | 324,036,133 (79.8) | <0.001 |
| No | 85,280,691 (20.4) | 3,450,826 (29.2) | 81,829,865 (20.2) | |
| CCI 5 | ||||
| 0 | 377,073,942 (90.3) | 11,034,668 (93.5) | 366,039,274 (90.2) | <0.001 |
| 1 and more | 40,590,481 (9.7) | 763,757 (6.5) | 39,826,724 (9.8) | |
| Total claim costs (million USD 3) (total (mean ± SD 6)) | 6,827.9 (16.3 ± 67.8) | 117.9 (10.0 ± 14.2) | 6,710.0 (16.5 ± 68.8) | <0.001 |
| NHI 2 costs (million USD 3) (total (mean ± SD 6)) | 5,161.2 (12.4 ± 60.4) | 92.3 (7.8 ± 10.1) | 5,069.0 (12.5 ± 61.2) | <0.001 |
| OOP 7 costs (million USD 3) (total (mean ± SD 6)) | 1,666.6 (4.0 ± 8.6) | 16.9 (2.2 ± 4.4) | 1,641.0 (4.0 ± 8.6) | <0.001 |
| Variable | Adjusted Odds Ratio | 95% Confidence Interval (Lower Limit–Upper Limit) | p-Value |
|---|---|---|---|
| Age group (years) | |||
| 0–19 | 1.00 (Reference) | ||
| 20–39 | 1.71 | 1.68–1.75 | <0.001 |
| 40–64 | 2.82 | 2.79–2.86 | <0.001 |
| >65 | 6.04 | 5.97–6.12 | <0.001 |
| Gender | |||
| Female | 1.00 (Reference) | ||
| Male | 1.12 | 1.11–1.12 | <0.001 |
| Type of health insurance | |||
| Medical Aid | 1.00 (Reference) | ||
| NHI 1 | 7.06 | 6.96–7.15 | <0.001 |
| Region | |||
| Metropolitan area | 1.00 (Reference) | ||
| Non-metropolitan area | 4.48 | 4.48–4.49 | <0.001 |
| CCI 2 | |||
| 1 or more | 1.00 (Reference) | ||
| 0 | 2.84 | 2.83–2.85 | <0.001 |
| Visits for SMDGs 3 | |||
| Yes | 1.00 (Reference) | ||
| No | 1.22 | 1.22–1.23 | <0.001 |
| Total claim costs (average per visit, USD 4) | |||
| >14.4 | 1.00 (Reference) | ||
| <9.6 | 33.31 | 33.12–33.50 | <0.001 |
| 9.6–11.6 | 5.48 | 5.44–5.51 | <0.001 |
| 11.6–14.4 | 0.29 | 0.28–0.29 | <0.001 |
| Out-of-pocket costs (average per visit, USD 4) | |||
| >4.0 | 1.00 (Reference) | ||
| <1.3 | 5.97 | 5.94–6.00 | <0.001 |
| 1.3–2.9 | 0.01 | 0.01–0.01 | <0.001 |
| 2.9–4.0 | 0.10 | 0.099–0.101 | <0.001 |
| Insurance 5*Age group | 1.00 (Reference) | ||
| NHI 1*Age1b 6 | 1.46 | 1.43–1.49 | <0.001 |
| NHI 1*Age2c 7 | 2.63 | 2.60–2.67 | <0.001 |
| NHI 1*Age3d 8 | 7.58 | 7.47–7.68 | <0.001 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, A.M.; Cho, S.; Kim, H.J.; Jo, M.-W.; Eun, S.J.; Lee, J.Y. Rethinking the Role of the Public Health Clinic: Comparison of Outpatient Utilization in the Public Health Clinics and Private Clinics in Korea. Int. J. Environ. Res. Public Health 2018, 15, 1312. https://doi.org/10.3390/ijerph15071312
Kim AM, Cho S, Kim HJ, Jo M-W, Eun SJ, Lee JY. Rethinking the Role of the Public Health Clinic: Comparison of Outpatient Utilization in the Public Health Clinics and Private Clinics in Korea. International Journal of Environmental Research and Public Health. 2018; 15(7):1312. https://doi.org/10.3390/ijerph15071312
Chicago/Turabian StyleKim, Agnus M., Seongcheol Cho, Hyun Joo Kim, Min-Woo Jo, Sang Jun Eun, and Jin Yong Lee. 2018. "Rethinking the Role of the Public Health Clinic: Comparison of Outpatient Utilization in the Public Health Clinics and Private Clinics in Korea" International Journal of Environmental Research and Public Health 15, no. 7: 1312. https://doi.org/10.3390/ijerph15071312
APA StyleKim, A. M., Cho, S., Kim, H. J., Jo, M.-W., Eun, S. J., & Lee, J. Y. (2018). Rethinking the Role of the Public Health Clinic: Comparison of Outpatient Utilization in the Public Health Clinics and Private Clinics in Korea. International Journal of Environmental Research and Public Health, 15(7), 1312. https://doi.org/10.3390/ijerph15071312





