Acute Lymphoblastic Leukemia with Hypereosinophilia in a Child: Case Report and Literature Review
Abstract
1. Background
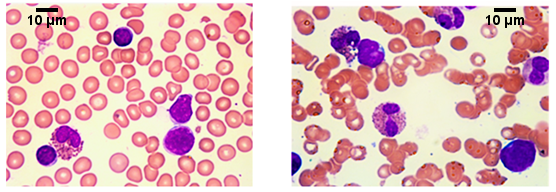
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Ethics, Approval and Consent to Participate
Consent to Publish
Funding
Acknowledgments
Conflicts of Interest
References
- Gotlib, J. World Health Organization-defined eosinophilic disorders: 2017 update on diagnosis, risk stratification, and management. Am. J. Hematol. 2015, 92, 1243–1259. [Google Scholar] [CrossRef] [PubMed]
- Amshalom, A.; Lev, A.; Trakhtenbrot, L.; Golan, H.; Weiss, B.; Amariglio, N.; Rechavi, G.; Somech, R. Severe eosinophilia in children: A diagnostic dilemma. J. Pediatr. Hematol. Oncol. 2013, 35, 303–306. [Google Scholar] [CrossRef] [PubMed]
- Bachhuber, R.; Fitchen, J.H.; Harty-Golder, B. Rash and eosinophilia in a 23-year-old man. West. J. Med. 1982, 137, 221–227. [Google Scholar] [PubMed]
- Spitzer, G.; Garson, O.M. Lymphoblastic leukemia with marked eosinophilia: A report of two cases. Blood 1973, 42, 377–384. [Google Scholar] [PubMed]
- Parasole, R.; Petruzziello, F.; De Matteo, A.; Maisto, G.; Castelli, L.; Errico, M.E.; Menna, G.; Poggi, V. Hypereosoinophilia in childhood acute lymphoblastic leukemia at diagnosis: Report of 2 cases and review of the literature. Ital. J. Pediatr. 2014, 40, 36. [Google Scholar] [CrossRef] [PubMed]
- Kahn, J.E.; Groh, M.; Lefèvre, G. (A Critical Appraisal of) Classification of Hypereosinophilic Disorders. Front. Med. 2017, 4, 216. [Google Scholar] [CrossRef] [PubMed]
- Roufosse, F. Hypereosinophilic syndrome variants: Diagnostic and therapeutic considerations. Haematologica 2009, 94, 1188–1193. [Google Scholar] [CrossRef] [PubMed]
- Hogan, T.F.; Koss, W.; Murgo, A.J.; Amato, R.S.; Fontana, J.A.; VanScoy, F.L. Acute lymphoblastic leukemia with chromosomal 5;14 translocation and hypereosinophilia: Case report and literature review. J. Clin. Oncol. 1987, 5, 382–390. [Google Scholar] [CrossRef] [PubMed]
- Grimaldi, J.C.; Meeker, T.C. The t(5;14) chromosomal translocation in a case of acute lymphocytic leukemia joins the interleukin-3 gene to the immunoglobulin heavy chain gene. Blood 1989, 73, 2081–2085. [Google Scholar] [PubMed]
- Meeker, T.C.; Hardy, D.; Willman, C.; Hogan, T.; Abrams, J. Activation of the interleukin-3 gene by chromosome translocation in acute lymphocytic leukemia with eosinophilia. Blood 1990, 76, 285–289. [Google Scholar] [PubMed]
- Ali, A.M.; Rashidi, A.; DiPersio, J.F. Acute lymphoblastic leukemia presenting with hypereosinophilia: Case report and review of the literature. Blood Cells Mol. Dis. 2017, 65, 97–100. [Google Scholar] [CrossRef] [PubMed]
- Bomken, S.; Haigh, S.; Bown, N.; Carey, P.; Wood, K.; Windebank, K. Cutaneous B-lymphoblastic lymphoma with IL3/IgH translocation presenting with hypereosinophilia and acute endocarditis. Pediatr. Blood Cancer 2015, 62, 1055–1057. [Google Scholar] [CrossRef] [PubMed]
- Sahu, K.K.; Malhotra, P.; Khadwal, A.; Sachdeva, M.S.; Sharma, P.; Varma, N.; Varma, S.C. Hypereosinophilia in Acute Lymphoblastic Leukemia: Two Cases with Review of Literature. Indian J. Hematol. Blood Transfus. 2015, 31, 460–465. [Google Scholar] [CrossRef] [PubMed]
- Holmes, A.; Coviello, J.; Velagaleti, G. Acute multilineage (B/myeloid) leukemia with RUNX1 duplication/amplification and hypereosinophilia. Eur. J. Haematol. 2014, 93, 449–452. [Google Scholar] [CrossRef] [PubMed]
- Rezamand, A.; Ghorashi, Z.; Ghorashi, S.; Nezami, N. Eosinophilic presentation of acute lymphoblastic leukemia. Am. J. Case Rep. 2013, 14, 143–146. [Google Scholar] [PubMed]
- Ayhan, A.C.; Timur, C.; Ayhan, Y.; Cakir, B.; Erguven, M. Does Hypereosinophilic Syndrome Precede Common B Acute Lymphoblastic Leukemia in Childhood? A Case Report. Acta Haematol. 2012, 127, 90. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, D.; Kogawa, K.; Imai, K.; Tanaka, T.; Sada, A.; Nonoyama, S. Hyper-eosinophilia in granular acute B-cell lymphoblastic leukemia with myeloid antigen expression. Pediatr. Int. 2012, 54, 543–546. [Google Scholar] [CrossRef] [PubMed]
- Guo, Y.; Chen, X.J.; Wang, S.C. Childhood acute lymphoblastic leukemia with hypereosinophilia: Two cases and literature review. Zhonghua Xue Ye Xue Za Zhi 2012, 33, 131–132. [Google Scholar] [PubMed]
- George, S.; Kumar, P.; Quarta, G.; Shankar, A.; Hough, R.; Samarasinghe, S. Loeffler myocarditis in pre-B acute lymphoblastic leukemia with t(5;14)(q31;q32). Br. J. Haematol. 2012, 157, 517. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.H.; Tsai, I.C.; Jan, S.L.; Tsai, W.L.; Chen, C.C. MDCT evaluation of cardiac involvement in hypereosinophilic syndrome. Tex. Heart Inst. J. 2011, 38, 166–169. [Google Scholar] [PubMed]
- Nesheli, M.H.; Moghaddam, T.G.; Zahedpasha, Y.; Norouzi, A.R. Acute Lymphoblastic Leukemia with Eosinophilia and Strongyloides stercoralis Hyperinfection. Iran. J. Pediatr. 2011, 21, 549–552. [Google Scholar] [PubMed]
- Nie, Y.L.; Jan, S.L.; Fu, L.S.; Chang, T.K.; Wang, J.D. Congestive heart failure as presentation of acute lymphoblastic leukemia with eosinophilia. Br. J. Haematol. 2010, 149, 633. [Google Scholar] [CrossRef] [PubMed]
- Files, M.D.; Zenel, J.A.; Armsby, L.B.; Langley, S.M. A child with eosinophilia, Loffler endocarditis, and acute lymphoblastic leukemia. Pediatr. Cardiol. 2009, 30, 530–532. [Google Scholar] [CrossRef] [PubMed]
- Sutton, R.; Lonergan, M.; Tapp, H.; Venn, N.C.; Haber, M.; Norris, M.D.; O’Brien, T.A.; Alvaro, F.; Revesz, T. Two cases of hypereosinophilia and high-risk acute lymphoblastic leukemia. Leukemia 2008, 22, 1463–1465. [Google Scholar] [CrossRef] [PubMed]
- Rezk, S.A.; Wheelock, L.; Fletcher, J.A.; Oliveira, A.M.; Keuker, C.P.; Newberger, P.E.; Xu, B.; Woda, B.A.; Miron, P.M. Acute lymphoblastic leukemia with eosinophilia and unusual karyotype. Leuk. Lymphoma 2006, 47, 1176–1179. [Google Scholar] [CrossRef] [PubMed]
- Rapanotti, M.C.; Caruso, R.; Bernardini, S.; Coletti, V.; Lo-Coco, F.; De Rossi, G. Idiopathic hypereosinophilic syndrome: A case evolving in B-lymphoblastic lymphoma. Leuk. Res. 2005, 29, 975–979. [Google Scholar] [CrossRef] [PubMed]
- Horigome, H.; Sumazaki, R.; Iwasaki, N.; Imoto, N.; Kinugasa, H.; Saito, M.; Matsui, A. Fatal eosinophilic heart disease in a child with neurofibromatosis-1 complicated by acute lymphoblastic leukemia. Heart Vessels 2005, 20, 120–122. [Google Scholar] [CrossRef] [PubMed]
- Wilson, F.; Tefferi, A. Acute lymphocytic leukemia with eosinophilia: Two case reports and a literature review. Leuk. Lymphoma 2005, 46, 1045–1050. [Google Scholar] [CrossRef] [PubMed]
- Girodon, F.; Bergoin, E.; Favre, B.; Martha, S.A.; Mugneret, F.; Couillaut, G.; Carli, P.M.; Maynadié, M. Hypereosinophilia in acute B-lineage lymphoblastic leukemia. Br. J. Haematol. 2005, 129, 568. [Google Scholar] [CrossRef] [PubMed]
- Lamb, L.S., Jr.; Neuberg, R.; Welsh, J.; Best, R.; Stetler-Stevenson, M.; Sorrell, A. T-Cell lymphoblastic leukemia/lymphoma syndrome with eosinophilia and acute myeloid leukemia. Cytom. Part B Clin. Cytom. 2005, 65, 37–41. [Google Scholar] [CrossRef] [PubMed]
- Chien, A.J.; Argeny, Z.B.; Colven, R.M.; Kirby, P. Acute lymphoblastic leukemia presenting with urticarial plaques and hypereosinophilia in a child. J. Am. Acad. Dermatol. 2004, 51, S151–S155. [Google Scholar] [CrossRef] [PubMed]
- Nuñez, C.A.; Zipf, T.F.; Roberts, W.M.; Medeiros, L.J.; Hayes, K.; Bueso-Ramos, C.E. Molecular monitoring of cerebrospinal fluid can predict clinical relapse in acute lymphoblastic leukemia with eosinophilia. Arch. Pathol. Lab. Med. 2003, 127, 601–605. [Google Scholar] [PubMed]
- Wynn, T.T.; Heerema, N.A.; Hammond, S.; Ranalli, M.; Kahwash, S.B. Acute lymphoblastic leukemia with hypereosinophilia: Report of a case with 5q deletion and review of the literature. Pediatr. Dev. Pathol. 2003, 6, 558–563. [Google Scholar] [CrossRef] [PubMed]
- Hill, A.; Metry, D. Urticarial lesions in a child with acute lymphoblastic leukemia and eosinophilia. Pediatr. Dermatol. 2003, 20, 502–505. [Google Scholar] [CrossRef] [PubMed]
- Donahue, T.P. Images in cardiology: Loeffler’s Endocarditis Resulting from Acute Lymphoblastic Leukemia. Clin. Cardiol. 2002, 25, 345. [Google Scholar] [CrossRef] [PubMed]
- Bjerregaard, L.L.; Rosthoøj, S. Vertebral compression and eosinophilia in a child with acute lymphatic leukemia. J. Pediatr. Hematol. Oncol. 2002, 24, 313–315. [Google Scholar] [CrossRef] [PubMed]
- Bernasconi, C. Hypereosinophilia in acute lymphoblastic leukemia: An association to be remembered. Haematologica 2001, 86, 893. [Google Scholar] [PubMed]
- Jain, P.; Kumar, R.; Gujral, S.; Kumar, A.; Singh, A.; Jain, Y.; Dubey, S.; Anand, M.; Arya, L.S. Granular acute lymphoblastic leukemia with hypereosinophilic syndrome. Ann. Hematol. 2000, 79, 272–274. [Google Scholar] [CrossRef] [PubMed]
- Narayanan, G.; Hussain, B.M.; Chandralekha, B.; Sivasankar, C.; Nair, M.K. Hyperosinophilia syndrome in acute lymphoblastic leukemia, case report and leterature review. Acta Oncol. 2000, 39, 241–243. [Google Scholar] [PubMed]
- Kita, R.; Enokihara, H.; Nagashima, S.; Tsunogake, S.; Yamato, H.; Saito, K.; Furusawa, S.; Shishido, H.; Fukushima, Y.; Fukuda, T. GM-CSF and eosinophil chemotactic factors in an acute lymphoblastic leukemia patient with eosinophilia. Acta Haematol. 1993, 90, 144–147. [Google Scholar] [CrossRef] [PubMed]
- Blatt, J.; Proujansky, R.; Horn, M.; Phebus, C.; Longworth, D.; Penchansky, L. Idiopathic hypereosinophilic syndrome terminating in acute lymphoblastic leukemia. Pediatr. Hematol. Oncol. 1992, 9, 151–155. [Google Scholar] [CrossRef] [PubMed]
- Rios-Herranz, E.; Fores-Cachon, R.; Diez-Martin, J.L.; Fernandez, M.N. Hypereosinophilia and acute lymphoblastic leukemia. Postgrad. Med. J. 1991, 67, 702–703. [Google Scholar] [CrossRef] [PubMed]
- Dervanian, P.; Acar, C.; Jebara, V.A.; Deloche, A.; Fabiani, J.N.; Carpentier, A. Mitral valvuloplasty for endomyocardial fibrosis in a child with acute leukemia and hypereosinophilia. Arch. Mal. Coeur Vaiss. 1991, 84, 1861–1864. [Google Scholar] [PubMed]
- Baumgarten, E.; Wegner, R.D.; Fengler, R.; Ludwig, W.D.; Schulte-Overberg, U.; Domeyer, C.; Schüürmann, J.; Henze, G. Calla-positive acute leukemia with t(5q;14q) translocation and hypereosinophilia—A unique entity? Acta Hematol. 1989, 82, 85–90. [Google Scholar] [CrossRef] [PubMed]
- McConnell, T.S.; Foucar, K.; Hardy, W.R.; Saiki, J. Three-way reciprocal chromosomal traslocation in an acute lymphoblastic leukemia patient with hypereosinophilia syndrome. J. Clin. Oncol. 1987, 5, 2042–2044. [Google Scholar] [CrossRef] [PubMed]
- Keene, P.; Mendelow, B.; Pinto, M.R.; Bezwoda, W.; MacDougall, L.; Falkson, G.; Ruff, P.; Bernstein, R. Abnormalities of chromosome 12p13 and malignant proliferation of eosinophils: A nonrandom association. Br. J. Haematol. 1987, 67, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Tan, A.M.; Downie, P.J.; Ekert, H. Hypereosinophilia syndrome with pneumonia in acute lymphoblastic leukemia. Aust. Pediatr. J. 1987, 23, 359–361. [Google Scholar]
- Troxell, M.L.; Mills, G.M.; Allen, R.C. The hypereosinophilic syndrome in acute lymphocytic leukemia. Cancer 1984, 54, 1058–1061. [Google Scholar] [CrossRef]
- Gaynon, P.S.; Gonzalez-Crussi, F. Exaggerated eosinophilia and acute lymphoid leukemia. Am. J. Pediatr. Hematol. Oncol. 1984, 6, 334–337. [Google Scholar] [CrossRef] [PubMed]
- Chilcote, R.R.; Pergament, E.; Kretschmer, R.; Mikuta, J.C. The hypereosinophilic syndrome and lymphoblastic leukemia with extra C-group chromosome and q14+ marker. J. Pediatr. 1982, 101, 57–60. [Google Scholar] [CrossRef]
- Bottone, E.; Macchia, P.; Consolini, R. Acute lymphoblastic leukemia first appearing as hypereosinophilia. Eur. J. Pediatr. 1982, 132, 85–88. [Google Scholar] [CrossRef]
- Catovsky, D.; Bernasconi, C.; Verdonck, P.J.; Postma, A.; Hows, J.; van der Does-van den Berg, A.; Rees, J.K.; Castelli, G.; Morra, E.; Galton, D.A. The association of eosinophilia with lymphoblastic leukemia or lymphoma: A study of seven patients. Br. J. Haematol. 1980, 45, 523–543. [Google Scholar] [CrossRef] [PubMed]
- Wimmer, R.S.; Raney, R.B.; Naiman, J.L. Hypereosinophilia with acute lymphocytic and acute myelocytic leukemia in childhood. J. Pediatr. 1978, 92, 244–246. [Google Scholar] [CrossRef]
- Geltner, D.; Friedman, G.; Naparstek, E.; Granot, H.; Polliack, A. Acute lymphoblastic leukemia its occurrence with hypereosinophilic syndrome and bilateral spontaneous pneumothorax. Arch. Intern. Med. 1978, 138, 292–293. [Google Scholar] [CrossRef] [PubMed]
- Pereira, F.; Moreno, H.; Crist, W.; Ermocilla, R. Loffler’s endomyocardial fibrosis, eosinophilia, and acute lymphoblastic leukemia. Pediatrics 1977, 59, 950–951. [Google Scholar] [PubMed]
- Nelken, R.P.; Stockman, J.A. , 3rd. The hypereosinophilic syndrome in association with acute lymphoblastic leukemia. J. Pediatr. 1976, 89, 771–773. [Google Scholar] [CrossRef]
- Rizzo, S.C.; Fontana, G.; Marini, G.; Balduini, C.L. Marked eosinophilia associated with acute lymphoblastic leukemia. Haematologica 1976, 61, 81–85. [Google Scholar] [PubMed]
- Blatt, P.M.; Rothstein, G.; Miller, H.L.; Cathey, W.J. Loffler’s andomyocardial fibrosis with eosinophilia in association with acute lymphoblastic leukemia. Blood 1974, 44, 489–493. [Google Scholar] [PubMed]
- Weller, P.F.; Bubley, G.J. The idiopathic hypereosinophilic syndrome. Blood 1994, 83, 2759–2779. [Google Scholar] [PubMed]
- Hardy, W.R.; Andreson, R.E. The hyperosinophilic syndromes. Ann. Intern. Med. 1968, 68, 1220–1229. [Google Scholar] [CrossRef] [PubMed]
- Utsunomiya, A.; Ishida, T.; Inagaki, A.; Ishii, T.; Yano, H.; Komatsu, H.; Iida, S.; Yonekura, K.; Takeuchi, S.; Takatsuka, Y.; et al. Clinical significance of a blood eosinophilia in adult T-cell leukemia/lymphoma: A blood eosinophilia is a significant unfavorable prognostic factor. Leuk. Res. 2007, 31, 915–920. [Google Scholar] [CrossRef] [PubMed]
| Data | Characteristic (n = 61) |
|---|---|
| Gender, male (%) | 34 (55.7%) |
| Age, median years (range) | 10 (1–25) |
| Main clinical characteristics (%) | Fever (62.3%), respiratory symptoms (42.6%), organomegaly (31.1%), osteoarticular pain (29.5%), rash (29.5%), asthenia (24.6%), lymphoadenopathy (18%), cardiovascular symptoms (9.8%) |
| First blood cell count | |
| White blood count, median cells/µL (range) | 48,300 (15,000–218,000) |
| Eosinophil count, median cells/µL (range) | 30,000 (270–135,000) |
| Platelets, median cells/µL (range) | 121,000 (100,000–440,000) |
| Hemoglobin, median value in g/dL (range) | 10.5 (4.7–14.2) |
| Blasts, median % (range) | Present in 16 cases (26.3%): 7% (3–90%) |
| Diagnosis | |
| B-cell ALL, n. (%) | 29 (47.5%) |
| Pre-B ALL, n. (%) | 12 (19.7%) |
| Common ALL, n. (%) | 5 (8.0%) |
| Other, n. (%) | 15 (24.8%) |
| Cytogenetics | |
| 46 XX, n. (%) | 18 (29.5%) |
| Other forms, n. (%) | t (5; 14) 8 (13%), iperdiploid 8 (13%), del (5) 2 (3.3%), other 4 (6.7%) |
| Not available, n. (%) | 21 (34.5%) |
| Outcome | |
| Complete resolution, n. (%) | 24 (39.3%) |
| Complete resolution after bone marrow transplantation, n. (%) | 3 (5%) |
| Death, n. (%) | 22 (36%) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferruzzi, V.; Santi, E.; Gurdo, G.; Arcioni, F.; Caniglia, M.; Esposito, S. Acute Lymphoblastic Leukemia with Hypereosinophilia in a Child: Case Report and Literature Review. Int. J. Environ. Res. Public Health 2018, 15, 1169. https://doi.org/10.3390/ijerph15061169
Ferruzzi V, Santi E, Gurdo G, Arcioni F, Caniglia M, Esposito S. Acute Lymphoblastic Leukemia with Hypereosinophilia in a Child: Case Report and Literature Review. International Journal of Environmental Research and Public Health. 2018; 15(6):1169. https://doi.org/10.3390/ijerph15061169
Chicago/Turabian StyleFerruzzi, Valentina, Elisa Santi, Grazia Gurdo, Francesco Arcioni, Maurizio Caniglia, and Susanna Esposito. 2018. "Acute Lymphoblastic Leukemia with Hypereosinophilia in a Child: Case Report and Literature Review" International Journal of Environmental Research and Public Health 15, no. 6: 1169. https://doi.org/10.3390/ijerph15061169
APA StyleFerruzzi, V., Santi, E., Gurdo, G., Arcioni, F., Caniglia, M., & Esposito, S. (2018). Acute Lymphoblastic Leukemia with Hypereosinophilia in a Child: Case Report and Literature Review. International Journal of Environmental Research and Public Health, 15(6), 1169. https://doi.org/10.3390/ijerph15061169






