Evaluation of the First Polish Web-Based Intervention Aimed at Improving Cancer Prevention (the PORINA Study)
Abstract
1. Introduction
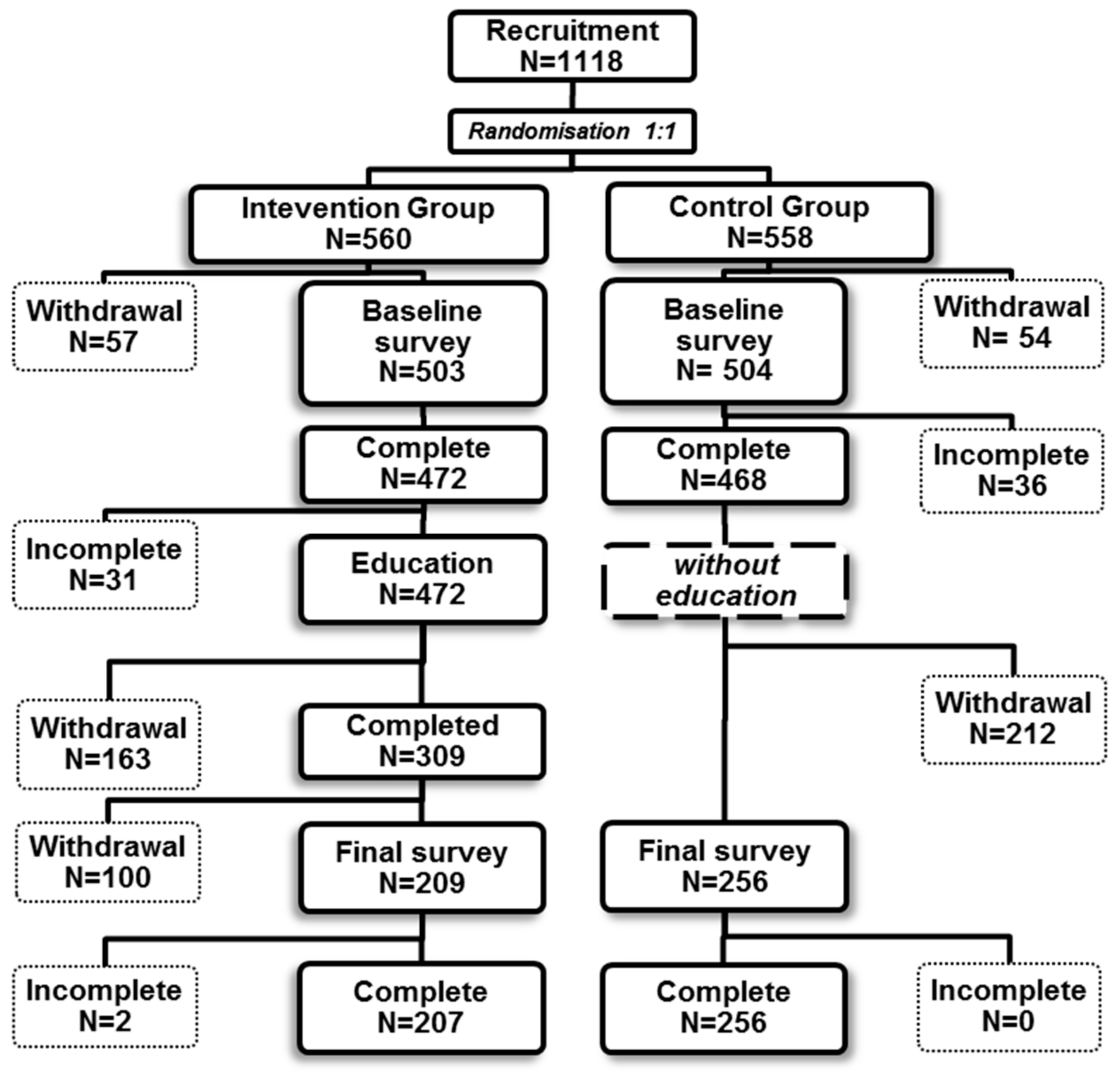
2. Materials and Methods
2.1. Recruitment Process and IT Solutions
2.2. Questionnaire and Educational Materials
2.3. Data Analysis
2.4. Ethical Aspects
3. Results
3.1. Basic Characteristics of the Study Population
3.2. The Validity and Reliability of the Study Instrument
3.3. Findings from the Intervention
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Stevens, G.; Mathers, C. Avoidable mortality—A tool for policy evaluation in developing countries? Eur. J. Public Health 2010, 20, 241–242. [Google Scholar] [CrossRef] [PubMed]
- Quaife, S.; Forbes, L.; Ramirez, A.; Brain, K.; Donnelly, C.; Simon, A.; Wardle, J. Recognition of cancer warning signs and anticipated delay in help-seeking in a population sample of adults in the UK. Br. J. Cancer 2014, 110, 12–18. [Google Scholar] [CrossRef] [PubMed]
- Chojnacka-Szawłowska, G.; Majkowicz, M.; Basiński, K.; Zdun-Ryżewska, A.; Wasilewko, I.; Pankiewicz, P. Knowledge of cancer symptoms and anxiety affect patient delay in seeking diagnosis in patients with heterogeneous cancer locations. Curr. Probl. Cancer 2017, 41, 64–70. [Google Scholar] [CrossRef] [PubMed]
- Hvidberg, L.; Wulff, C.N.; Pedersen, A.F.; Vedsted, P. Barriers to healthcare seeking, beliefs about cancer and the role of socio-economic position: A Danish population-based study. Prev. Med. 2015, 71, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Hvidberg, L.; Pedersen, A.F.; Wulff, C.N.; Vedsted, P. Cancer awareness and socio-economic position: Results from a population-based study in Denmark. BMC Cancer 2014, 14, 581. [Google Scholar] [CrossRef] [PubMed]
- American Cancer Society Cancer Facts & Figures 2016. Available online: https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2016/cancer-facts-and-figures-2016.pdf (accessed on 1 February 2018).
- Gajda, M.; Kowalska, M. The role of an electronic questionnaires in epidemiologic studies aimed at cancer prevention. Przegl. Epidemiol. 2016, 70, 479–489. [Google Scholar] [PubMed]
- Gajda, M.; Kowalska, M. Internet in interventional studies on cancer prevention. Hygeia Public Health 2016, 51, 115–123. (In Polish) [Google Scholar]
- Cugelman, B.; Thelwall, M.; Dawes, P. Online interventions for social marketing health behavior change campaigns: A meta-analysis of psychological architectures and adherence factors. J. Med. Internet Res. 2011, 13, e17. [Google Scholar] [CrossRef] [PubMed]
- Wojtyniak, B.; Goryński, P.; Moskalewicz, B. The Health Situation of the Polish Population and Its Determinants. National Institute of Public Health-National Institute of Hygiene. Warsaw, 2016. Available online: http://www.pzh.gov.pl/stan-zdrowia-ludnosci/sytuacja-zdrowotna-ludnosci-w-polsce/ (accessed on 10 May 2018). (In Polish)
- Ferlay, J.; Soerjomataram, I.; Dikshit, R.; Eser, S.; Mathers, C.; Rebelo, M.; Parkin, D.M.; Forman, D.; Bray, F. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int. J. Cancer 2015, 136, E359–E386. [Google Scholar] [CrossRef] [PubMed]
- Didkowska, J.; Wojciechowska, U.; Olasek, P. Cancer in Poland in 2015. Polish National Cancer Registry, Warsaw 2017. Available online: http://onkologia.org.pl/wp-content/uploads/Nowotwory_2015.pdf (accessed on 2 April 2018).
- Schüz, J.; Espina, C.; Villain, P.; Herrero, R.; Leon, M.E.; Minozzi, S.; Romieu, I.; Segnan, N.; Wardle, J.; Wiseman, M.; et al. European Code against Cancer 4th Edition: 12 ways to reduce your cancer risk. Cancer Epidemiol. 2015, 39, S1–S10. [Google Scholar] [CrossRef] [PubMed]
- R Core Team R. A Language and Environment for Statistical Computing. Available online: http://cran.r-project.org (accessed on 2 May 2016).
- Bland, J.M.; Altman, D.G. Cronbach’s alpha. BMJ 1997, 314, 572. [Google Scholar] [CrossRef] [PubMed]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef] [PubMed]
- Romano, J.; Kromrey, J.D.; Coraggio, J.; Skowronek, J.; Devine, L. Exploring methods for evaluating group differences on the NSSE and other surveys: Are the t-test and Cohen’s d indices the most appropriate choices? Annu. Meet. South. Assoc. Inst. Res. 2006, 14–17. [Google Scholar] [CrossRef]
- Fleisher, L.; Kandadai, V.; Keenan, E.; Miller, S.M.; Devarajan, K.; Ruth, K.J.; Rodoletz, M.; Bieber, E.J.; Weinberg, D.S. Build it, and will they come? Unexpected findings from a study on a Web-based intervention to improve colorectal cancer screening. J. Health Commun. 2012, 17, 41–53. [Google Scholar] [CrossRef] [PubMed]
- Bowen, D.J.; Robbins, R.; Bush, N.; Meischke, H.; Ludwig, A.; Wooldridge, J. Effects of a Web-based intervention on women’s breast health behaviors. Transl. Behav. Med. 2011, 1, 155–164. [Google Scholar] [CrossRef] [PubMed]
- Sarna, L.; Bialous, S.A.; Zou, X.N.; Wang, W.; Hong, J.; Wells, M.; Brook, J. Evaluation of a web-based educational programme on changes in frequency of nurses’ interventions to help smokers quit and reduce second-hand smoke exposure in China. J. Adv. Nurs. 2016, 72, 118–126. [Google Scholar] [CrossRef] [PubMed]
- Richardson, C.G.; Struik, L.L.; Johnson, K.C.; Ratner, P.A.; Gotay, C.; Memetovic, J.; Okoli, C.T.; Bottorff, J.L. Initial impact of tailored web-based messages about cigarette smoke and breast cancer risk on boys’ and girls’ risk perceptions and information seeking: Randomized controlled trial. JMIR Res. Protoc. 2013, 2, e53. [Google Scholar] [CrossRef] [PubMed]
- Choma, K.; McKeever, A.E. Cervical cancer screening in adolescents: An evidence-based internet education program for practice improvement among advanced practice nurses. Worldviews Evid.-Based Nurs. 2015, 12, 51–60. [Google Scholar] [CrossRef] [PubMed]
- Beattie, J.; Brady, L.; Tobias, T. Improving Clinician Confidence and Skills: Piloting a Web-Based Learning Program for Clinicians in Supportive Care Screening of Cancer Patients. J. Cancer Educ. 2014, 29, 38–43. [Google Scholar] [CrossRef] [PubMed]
- Bantum, E.O.; Albright, C.L.; White, K.K.; Berenberg, J.L.; Layi, G.; Ritter, P.L.; Laurent, D.; Plant, K.; Lorig, K. Surviving and thriving with cancer using a Web-based health behavior change intervention: Randomized controlled trial. J. Med. Internet Res. 2014, 16, e54. [Google Scholar] [CrossRef] [PubMed]
- Shahrokni, A.; Mahmoudzadeh, S.; Lu, B.T. In Whom Do Cancer Survivors Trust Online and Offline? Asian Pac. J. Cancer Prev. 2014, 15, 6171–6176. [Google Scholar] [CrossRef] [PubMed]
- Goode, A.D.; Lawler, S.P.; Brakenridge, C.L.; Reeves, M.M.; Eakin, E.G. Telephone, print, and Web-based interventions for physical activity, diet, and weight control among cancer survivors: A systematic review. J. Cancer Surviv. 2015, 9, 660–682. [Google Scholar] [CrossRef] [PubMed]
- Short, C.E.; Rebar, A.L.; Vandelanotte, C. Do personalised e-mail invitations increase the response rates of breast cancer survivors invited to participate in a web-based behaviour change intervention? A quasi-randomised 2-arm controlled trial. BMC Med. Res. Methodol. 2015, 15, 66. [Google Scholar] [CrossRef]
- Bottorff, J.L.; Struik, L.L.; Bissell, L.J.L.; Graham, R.; Stevens, J.; Richardson, C.G. A social media approach to inform youth about breast cancer and smoking: An exploratory descriptive study. Collegian 2014, 21, 159–168. [Google Scholar] [CrossRef] [PubMed]
- Webb, T.L.; Joseph, J.; Yardley, L.; Michie, S. Using the Internet to Promote Health Behavior Change: A Systematic Review and Meta-analysis of the Impact of Theoretical Basis, Use of Behavior Change Techniques, and Mode of Delivery on Efficacy. J. Med. Internet Res. 2010, 12, e4. [Google Scholar] [CrossRef] [PubMed]
- Park, B.K.; Lee, E. Effects of my child’s safety web-based program for caregivers of children with cancer in South Korea. Healthc. Inform. Res. 2014, 20, 199–208. [Google Scholar] [CrossRef] [PubMed]
- Lana, A.; Faya-Ornia, G.; López, M.L. Impact of a web-based intervention supplemented with text messages to improve cancer prevention behaviors among adolescents: Results from a randomized controlled trial. Prev. Med. 2014, 59, 54–59. [Google Scholar] [CrossRef] [PubMed]
- Hohwü, L.; Lyshol, H.; Gissler, M.; Jonsson, S.H.; Petzold, M.; Obel, C. Web-Based Versus Traditional Paper Questionnaires: A Mixed-Mode Survey With a Nordic Perspective. J. Med. Internet Res. 2013, 15, e173. [Google Scholar] [CrossRef] [PubMed]
- Greenhalgh, T.; Taylor, R. How to read a paper: Papers that go beyond numbers (qualitative research). BMJ 1997, 315, 740–743. [Google Scholar] [CrossRef] [PubMed]
- Sedgwick, P. Questionnaire surveys: Sources of bias. BMJ 2013, 347, f5265. [Google Scholar] [CrossRef]
- van Gelder, M.M.H.J.; Bretveld, R.W.; Roeleveld, N. Web-based questionnaires: The future in epidemiology? Am. J. Epidemiol. 2010, 172, 1292–1298. [Google Scholar] [CrossRef] [PubMed]
- Rosnow, R.L.; Rosenthal, R. The volunteer subject revisited. Aust. J. Psychol. 1976, 28, 97–108. [Google Scholar] [CrossRef]
- Stopponi, M.A.; Alexander, G.L.; McClure, J.B.; Carroll, N.M.; Divine, G.W.; Calvi, J.H.; Rolnick, S.J.; Strecher, V.J.; Johnson, C.C.; Ritzwoller, D.P. Recruitment to a randomized web-based nutritional intervention trial: Characteristics of participants compared to non-participants. J. Med. Internet Res. 2009, 11, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Robb, K.; Stubbings, S.; Ramirez, A.; Macleod, U.; Austoker, J.; Waller, J.; Hiom, S.; Wardle, J. Public awareness of cancer in Britain: A population-based survey of adults. Br. J. Cancer 2009, 101 (Suppl.), S18–S23. [Google Scholar] [CrossRef] [PubMed]
- Shim, H.-Y.; Shin, J.-Y.; Kim, J.H.; Kim, S.-Y.; Yang, H.-K.; Park, J.-H. Negative Public Attitudes towards Cancer Survivors Returning to Work: A Nationwide Survey in Korea. Cancer Res. Treat. 2016, 48, 815–824. [Google Scholar] [CrossRef] [PubMed]
- Ruffin, M.T.; Nease, D.E.; Sen, A.; Pace, W.D.; Wang, C.; Acheson, L.S.; Rubinstein, W.S.; O’Neill, S.; Gramling, R.; Family History Impact Trial (FHITr) Group. Effect of preventive messages tailored to family history on health behaviors: The Family Healthware Impact Trial. Ann. Fam. Med. 2011, 9, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Lin, Z.-C.; Effken, J.A. Effects of a tailored web-based educational intervention on women’s perceptions of and intentions to obtain mammography. J. Clin. Nurs. 2010, 19, 1261–1269. [Google Scholar] [CrossRef] [PubMed]
- Kyle, R.G.; Nicoll, A.; Forbat, L.; Hubbard, G. Adolescents’ awareness of cancer risk factors and associations with health-related behaviours. Health Educ. Res. 2013, 28, 816–827. [Google Scholar] [CrossRef] [PubMed]
- Robb, K.A.; Miles, A.; Campbell, J.; Evans, P.; Wardle, J. Can cancer risk information raise awareness without increasing anxiety? A randomized trial. Prev. Med. 2006, 43, 187–190. [Google Scholar] [CrossRef] [PubMed]
- Kim, A.R.; Park, H. Web-based Self-management Support Interventions for Cancer Survivors: A Systematic Review and Meta-analyses. Stud. Health Technol. Inform. 2015, 216, 142–147. [Google Scholar] [CrossRef] [PubMed]
- de Vries, H.; Logister, M.; Krekels, G.; Klaasse, F.; Servranckx, V.; van Osch, L. Internet based computer tailored feedback on sunscreen use. J. Med. Internet Res. 2012, 14, e48. [Google Scholar] [CrossRef] [PubMed]
- Jander, A.; Crutzen, R.; Mercken, L.; de Vries, H. A Web-based computer-tailored game to reduce binge drinking among 16 to 18 year old Dutch adolescents: Development and study protocol. BMC Public Health 2014, 14, 1054. [Google Scholar] [CrossRef] [PubMed]
- Puckett, M.; Neri, A.; Thompson, T.; Underwood, J.M.; Momin, B.; Kahende, J.; Zhang, L.; Stewart, S.L.; Centers for Disease Control and Prevention (CDC). Tobacco cessation among users of telephone and web-based interventions—Four states, 2011–2012. MMWR Morb. Mortal. Wkly. Rep. 2015, 63, 1217–1221. [Google Scholar] [PubMed]
- Crutzen, R.; Cyr, D.; de Vries, N.K. The role of user control in adherence to and knowledge gained from a website: Randomized comparison between a tunneled version and a freedom-of-choice version. J. Med. Internet Res. 2012, 14, e45. [Google Scholar] [CrossRef] [PubMed]
- Uhlig, C.E.; Seitz, B.; Eter, N.; Promesberger, J.; Busse, H. Efficiencies of Internet-based digital and paper-based scientific surveys and the estimated costs and time for different-sized cohorts. PLoS ONE 2014, 9, e108441. [Google Scholar] [CrossRef] [PubMed]

| Characteristic | Group | ||||
|---|---|---|---|---|---|
| Variables | Overall | Control | Interventional | p | |
| N = 463 | N = 256 | N = 207 | |||
| Age (years) | median (IQR) | 33 (22–47) | 31 (22–47) | 35 (21–47) | 0.9 # |
| Baseline CKI | median (IQR) | 14 (12–16) | 14 (12–16) | 14 (11–16) | 0.2 # |
| Final CKI | median (IQR) | 16 (13–18) | 14 (12–16) | 17 (15–18) | <0.001 # |
| Gender | Male | 179 (38.7%) | 100 (39.1%) | 79 (38.2%) | 0.8 & |
| Female | 284 (61.3%) | 156 (60.9%) | 128 (61.8%) | ||
| Place of residence | Village | 101 (21.8%) | 60 (23.4%) | 41 (19.8%) | 0.6 & |
| Small city | 117 (25.3%) | 64 (25.0%) | 53 (25.6%) | ||
| Large city | 245 (52.9%) | 132 (51.6%) | 113 (54.6%) | ||
| Level of education | Primary | 29 (6.3%) | 12 (4.7%) | 17 (8.2%) | 0.2 & |
| Secondary | 167 (36.1%) | 93 (36.3%) | 74 (35.7%) | ||
| High school | 238 (51.4%) | 131 (51.2%) | 107 (51.7%) | ||
| Higher medical | 29 (6.3%) | 20 (7.8%) | 9 (4.3%) | ||
| Medical occupation | No | 388 (83.8%) | 215 (84.0%) | 173 (83.6%) | 0.9 & |
| Yes | 75 (16.2%) | 41 (16.0%) | 34 (16.4%) | ||
| Positive family history of cancer | -overall | ||||
| No | 120 (25.9%) | 61 (23.8%) | 59 (28.5%) | 0.3 & | |
| Yes | 343 (74.1%) | 195 (76.2%) | 148 (71.5%) | ||
| -parents | |||||
| No | 333 (71.9%) | 180 (70.3%) | 153 (73.9%) | 0.4 & | |
| Yes | 130 (28.1%) | 76 (29.7%) | 54 (26.1%) | ||
| -grandparents | |||||
| No | 250 (54.0%) | 141 (55.1%) | 109 (52.7%) | 0.6 & | |
| Yes | 213 (46.0%) | 115 (44.9%) | 98 (47.3%) | ||
| -siblings | |||||
| No | 440 (95.0%) | 241 (94.1%) | 199 (96.1%) | 0.4 & | |
| Yes | 23 (5.0%) | 15 (5.9%) | 8 (3.9%) | ||
| Participant with diagnosis of cancer | No | 413 (89.2%) | 225 (87.9%) | 188 (90.8%) | 0.4 & |
| Yes | 50 (10.8%) | 31 (12.1%) | 19 (9.2%) | ||
| Participant treated oncologically | No | 415 (89.6%) | 229 (89.5%) | 186 (89.9%) | 1 & |
| Yes | 48 (10.4%) | 27 (10.5%) | 21 (10.1%) | ||
| Self-declaration of sufficient level cancer-related level of knowledge | No | 362 (78.2%) | 201 (78.5%) | 161 (77.8%) | 0.9 & |
| Yes | 101 (21.8%) | 55 (21.5%) | 46 (22.2%) | ||
| Self-declaration of willingness to improve the level of cancer-related knowledge | No | 35 (7.6%) | 20 (7.8%) | 15 (7.2%) | 0.9 & |
| Yes | 428 (92.4%) | 236 (92.2%) | 192 (92.8%) | ||
| Group with Education Interventional | Group without Education Control | |||||||
|---|---|---|---|---|---|---|---|---|
| Statement (Percentage of Agreement) | B | F | R | p | B | F | R | p |
| Cancer is a destiny which cannot be prevented | 86.0 | 90.3 | 4.3 | 0.1 | 84.8 | 85.2 | 0.4 | 0.99 |
| Consuming smaller amounts of food slows down while larger ones accelerates the growth of cancer | 58.0 | 70.0 | 12.0 | 0.002 | 61.7 | 59.0 | −2.7 | 0.4 |
| Patients treated with chemotherapy should drink red beet juice | 9.2 | 50.7 | 41.5 | <0.001 | 10.2 | 12.9 | 2.7 | 0.3 |
| Tobacco smokers with lung cancer can only blame themselves | 53.1 | 49.8 | −3.3 | 0.4 | 55.5 | 46.9 | −8.6 | 0.009 |
| Cancer is always pain and suffering | 40.1 | 75.8 | 35.7 | <0.001 | 42.6 | 50.8 | 8.2 | 0.009 |
| A person diagnosed with cancer can work | 78.3 | 87.9 | 9.6 | 0.002 | 81.2 | 82.4 | 1.2 | 0.7 |
| It’s better not to remove suspicious skin lesions as they will become malignant | 66.7 | 76.3 | 9.6 | 0.006 | 73.0 | 75.0 | 2.0 | 0.5 |
| Cancer is contagious | 93.7 | 94.7 | 1.0 | 0.8 | 95.3 | 94.9 | −0.4 | 0.99 |
| It is better not to perform a biopsy of the cancer, because the disease will spread throughout the organism | 75.8 | 87.4 | 11.6 | <0.001 | 85.2 | 85.2 | 0.0 | 0.99 |
| There is no treatment in the hospice | 68.6 | 83.6 | 15.0 | <0.001 | 70.7 | 69.9 | −0.8 | 0.9 |
| The vaccine against HPV human papilloma virus may protect against cervical cancer | 55.1 | 70.0 | 14.9 | <0.001 | 57.0 | 60.9 | 3.9 | 0.2 |
| Only women get breast cancer | 67.6 | 95.2 | 27.6 | <0.001 | 70.7 | 76.6 | 5.9 | 0.01 |
| Lung cancer occurs only in smokers | 98.6 | 98.1 | -0.5 | 0.99 | 97.7 | 97.7 | 0.0 | 0.99 |
| Smokers have a higher risk of developing pancreatic cancer | 48.8 | 72.9 | 24.1 | <0.001 | 50.8 | 55.9 | 5.1 | 0.1 |
| Blacks do not get melanoma skin cancer | 45.9 | 76.8 | 30.9 | <0.001 | 51.6 | 51.6 | 0.0 | 0.99 |
| Breast cancer occurs predominantly in women under the age of 30, rarely in later life | 87.4 | 87.0 | −0.4 | 0.99 | 84.0 | 85.5 | 1.5 | 0.6 |
| The presence of blood in stool can be a symptom of cancer of the colon cancer | 88.9 | 96.1 | 7.2 | 0.005 | 90.2 | 91.8 | 1.6 | 0.6 |
| Invalid lifestyle may increase the risk of cancer | 97.6 | 97.1 | -0.5 | 0.99 | 96.1 | 96.9 | 0.8 | 0.7 |
| It is enough to apply sunscreen once a day preferably in the morning to protect against ultraviolet UV | 84.5 | 87.0 | 2.5 | 0.4 | 84.4 | 87.5 | 3.1 | 0.2 |
| Normal level of tumor markers excludes the diagnosis of cancer | 50.2 | 84.1 | 33.9 | <0.001 | 52.7 | 57.4 | 4.7 | 0.1 |
| Group with Education (Interventional) | Group without Education (Control) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| B | F | D | p | δ | B | F | D | p | δ | ||
| Overall | 14 | 17 | 18 | <0.001 | 0.53 | 14 | 14 | 0 | <0.001 | 0.09 | |
| By category | |||||||||||
| Age group (years) | <24 | 13 | 17 | 18 | <0.001 | 0.55 | 14 | 14 | 0 | 0.3 | 0.05 |
| 24–41 | 14 | 16 | 18 | <0.001 | 0.48 | 14 | 15 | 0 | 0.004 | 0.12 | |
| >41 | 13 | 17 | 20 | <0.001 | 0.56 | 14 | 14 | 5 | 0.01 | 0.1 | |
| Gender | Male | 14 | 17 | 18 | <0.001 | 0.50 | 14 | 14 | 0 | 0.02 | 0.09 |
| Female | 13 | 17 | 20 | <0.001 | 0.54 | 14 | 14 | 0 | 0.002 | 0.09 | |
| Number of inhabitants in the place of residence | ≤100,000 | 13 | 17 | 18 | <0.001 | 0.50 | 14 | 14 | 0 | 0.002 | 0.1 |
| >100,000 | 13 | 17 | 20 | <0.001 | 0.55 | 14 | 15 | 0 | 0.02 | 0.08 | |
| Level of education | Primary | 12 | 17 | 25 | 0.002 | 0.64 | 14 | 14.5 | −6 | 0.5 | 0.01 |
| Secondary | 13 | 17 | 15 | <0.001 | 0.42 | 13 | 13 | 0 | 0.02 | 0.09 | |
| High school | 13 | 17 | 21 | <0.001 | 0.62 | 14 | 14 | 0 | 0.005 | 0.09 | |
| Higher medical | 17 | 18 | 5 | 0.2 | 0.35 | 16 | 16 | 5 | 0.03 | 0.2 | |
| Medical occupation | No | 13 | 17 | 20 | <0.001 | 0.55 | 14 | 14 | 0 | <0.001 | 0.09 |
| Yes | 16 | 17 | 11 | <0.001 | 0.40 | 15 | 16 | 0 | 0.09 | 0.1 | |
| Positive family history of cancer | No | 12 | 16 | 20 | <0.001 | 0.49 | 13 | 13 | 0 | 0.2 | 0.04 |
| Yes | 14 | 17 | 18 | <0.001 | 0.56 | 14 | 15 | 0 | <0.001 | 0.11 | |
| Participants with diagnosis of cancer | No | 13 | 17 | 20 | <0.001 | 0.52 | 14 | 14 | 0 | <0.001 | 0.09 |
| Yes | 15 | 18 | 18 | <0.001 | 0.67 | 14 | 15 | 5 | 0.1 | 0.14 | |
| Treated oncologically | No | 13 | 17 | 20 | <0.001 | 0.54 | 14 | 14 | 0 | <0.001 | 0.09 |
| Yes | 15 | 17 | 18 | 0.005 | 0.42 | 14 | 14 | 0 | 0.2 | 0.08 | |
| Self-esteem level of knowledge about cancer as sufficient | No | 13 | 17 | 20 | <0.001 | 0.56 | 13 | 14 | 5 | <0.001 | 0.12 |
| Yes | 14.5 | 17 | 14 | <0.001 | 0.44 | 15 | 15 | 0 | 0.6 | 0.02 | |
| The readiness to improve the level of cancer-related knowledge | No | 15 | 18 | 20 | 0.004 | 0.59 | 14.5 | 14 | 0 | 0.5 | 0.01 |
| Yes | 13 | 17 | 18 | <0.001 | 0.53 | 14 | 14 | 0 | <0.001 | 0.1 | |
| What Was the Purpose of the Intervention? | The Size of the Study Group | Effect of Intervention (Relative Difference in Percentages) 1 | Author and Year of Publication |
|---|---|---|---|
| Reduce the lifestyle-related risk of cancer | Intervention | Lana, 2014 [31] | |
| 177 | standard: 16.9% | ||
| 244 | supplemented with SMS: 27.2% | ||
| Cancer-related knowledge of nurses | 48 | 18.3% | Choma, 2015 [22] |
| Insomnia level | 156 | −4.3% | Bantum, 2014 [24] |
| Strenuous exercise | 156 | 37.2% | |
| Stretching | 156 | 32.6% | |
| The level of awareness of medical staff | 29 | 12.1% | Park, 2014 [30] |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gajda, M.; Kowalska, M.; Zejda, J.E. Evaluation of the First Polish Web-Based Intervention Aimed at Improving Cancer Prevention (the PORINA Study). Int. J. Environ. Res. Public Health 2018, 15, 1167. https://doi.org/10.3390/ijerph15061167
Gajda M, Kowalska M, Zejda JE. Evaluation of the First Polish Web-Based Intervention Aimed at Improving Cancer Prevention (the PORINA Study). International Journal of Environmental Research and Public Health. 2018; 15(6):1167. https://doi.org/10.3390/ijerph15061167
Chicago/Turabian StyleGajda, Maksymilian, Małgorzata Kowalska, and Jan E. Zejda. 2018. "Evaluation of the First Polish Web-Based Intervention Aimed at Improving Cancer Prevention (the PORINA Study)" International Journal of Environmental Research and Public Health 15, no. 6: 1167. https://doi.org/10.3390/ijerph15061167
APA StyleGajda, M., Kowalska, M., & Zejda, J. E. (2018). Evaluation of the First Polish Web-Based Intervention Aimed at Improving Cancer Prevention (the PORINA Study). International Journal of Environmental Research and Public Health, 15(6), 1167. https://doi.org/10.3390/ijerph15061167







