General Practitioners’ Perceptions of Heat Health Impacts on the Elderly in the Face of Climate Change—A Qualitative Study in Baden-Württemberg, Germany
Abstract
1. Introduction
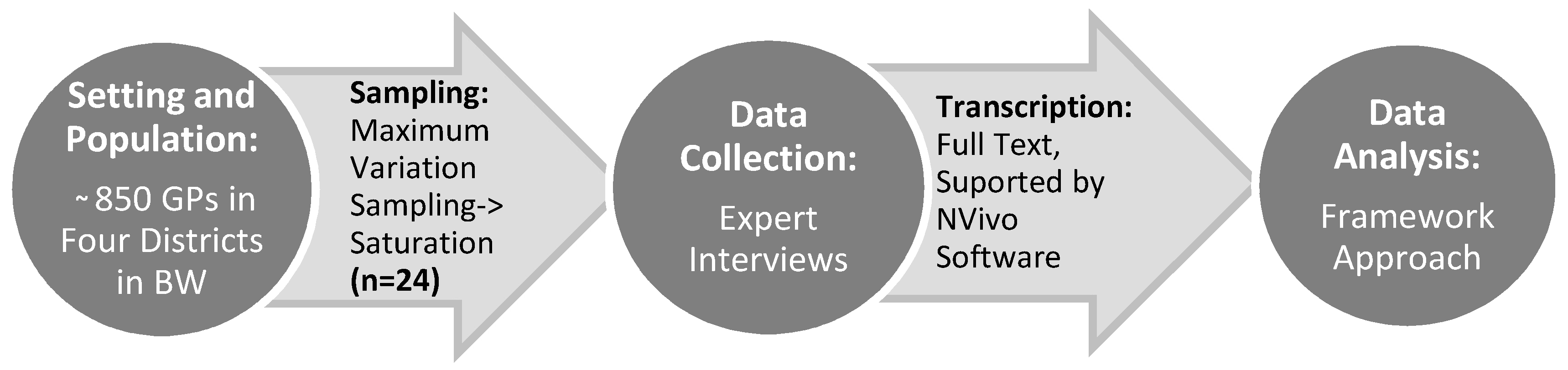
2. Materials and Methods
3. Results
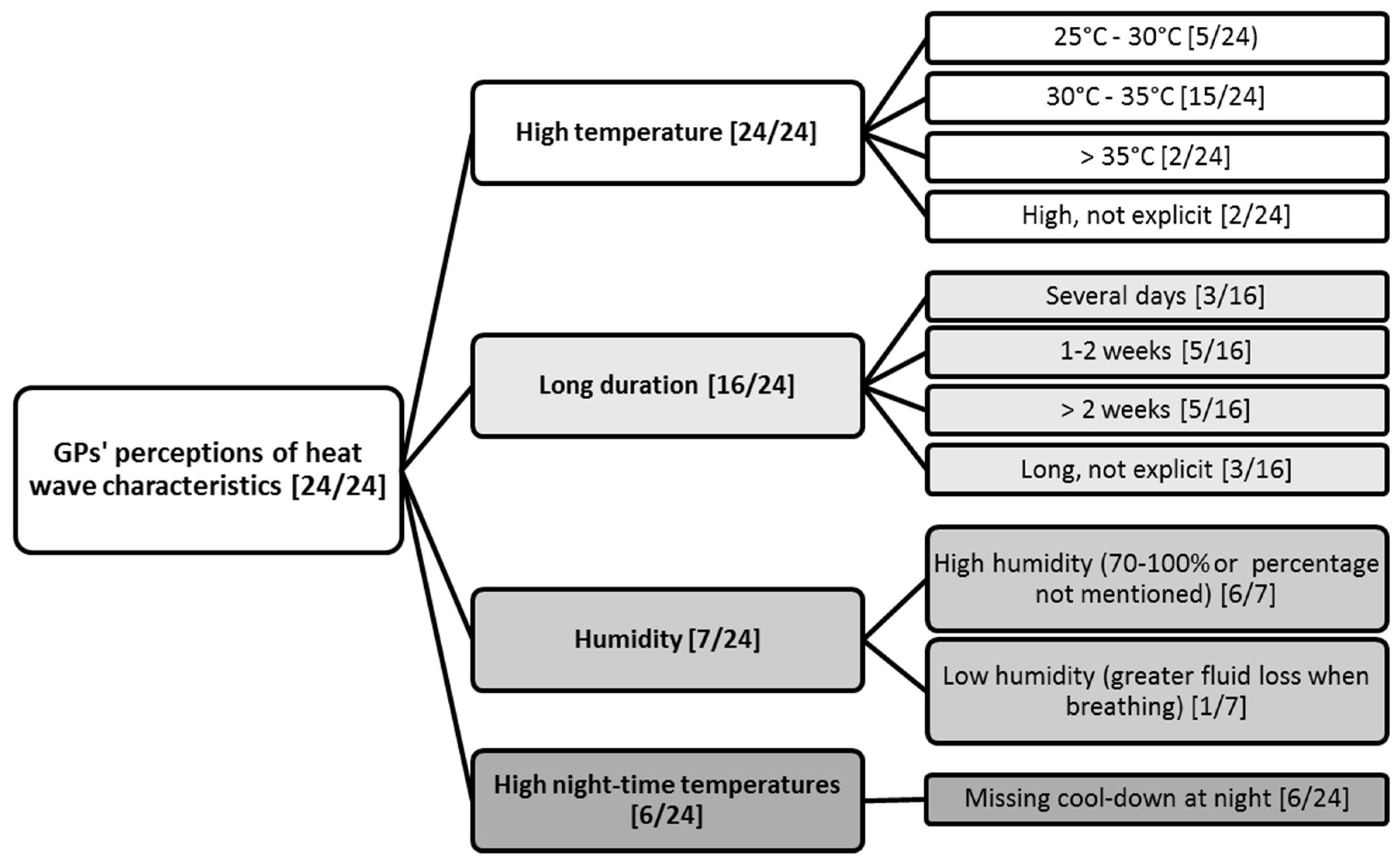
3.1. GPs’ Perceptions of Heat Wave Characteristics
3.2. GPs’ Perceptions of Risk Factors to Suffer from Heat Health Impacts
3.2.1. Pre-existing Disease
3.2.2. Socioeconomic Factors
“If they are living alone, I think they are more at risk, because no one is looking after them. If the family lives with them […], one will look after them. In care homes, for example, they take care that there is sufficient drink and that they don’t go outside, especially in the greatest heat.”GP 11 (female, rural, 51, general medicine, single practice)
3.2.3. Individual Factors
“There are 75 year olds that are fit as a fiddle. So you really can’t lump them together […], others are already frail with 65.”GP 6 (female, urban, 50, general medicine, joint practice)
3.2.4. Intake of Medication
3.3. GPs’ Perceptions of Morbidity and Mortality as Heat Health Impacts
“Well they [the patients] usually come anyways due to blood pressure or due to diabetes or due to circulatory problems, which they always have. And the weather, […] that can intensify the complaints, but that won’t be the cause for the people to come.”GP 11 (female, rural, 51, general medicine, single practice)
3.3.1. Morbidity as Heat Health Impact
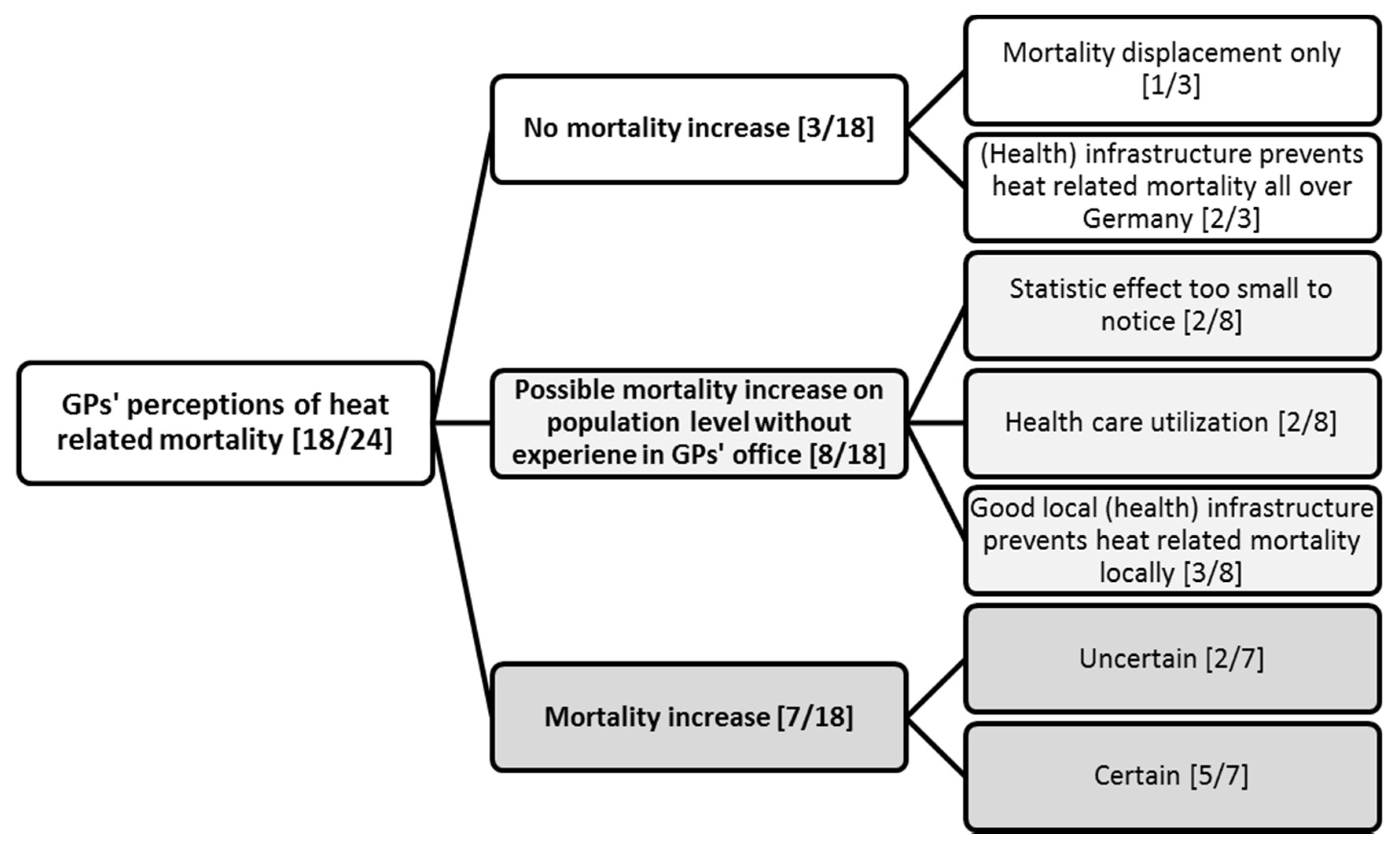
3.3.2. Mortality as Heat Health Impact
“Well, when there are really such heat waves, like e.g., in 2003, then I can imagine, I am even convinced that then a lot of elderly people, who don’t really have the opportunity to adapt through foods or fluids or something like that, that then mortality rises, especially in nursing homes. […] I don’t know if there’s literature about this.”GP 12 (male, rural, 49, general medicine, single practice)
“I don’t know how many GPs there are in Baden-Württemberg? (…) There should be more than thousand, shouldn’t there? If we distribute 1100 more deaths on all the GPs then it would be about half a death more in the summer. You don’t notice that. You can only extricate it out of a statistic.”GP 7 (male, urban, 44, internal medicine, joint practice)
“It is definitely so, that—when someone is already very ill and there is a heat wave and you expect that the person will die soon anyways—then it happens a bit more quickly due to the heat […]. But not so, that there is a greater number of deaths through heat waves, I don’t think so.”(GP 22, female, rural, 44, internal medicine, joint practice)
3.4. GPs’ Perceptions of Relevance of Heat Health Impacts for Elderly
3.4.1. Current Relevance
“A great [relevance], because we already see it in practice, that the number of single elderly rises and that the neighborly support decreases, which used to be much better. I can see and judge this by my long experience. Yes and the same is the case in nursing homes that reduce staff as much as possible, as well as quality, in order to make it cheap. And thus nursing care there is not very good either.”GP 20 (male, urban, 62, GM, JP)
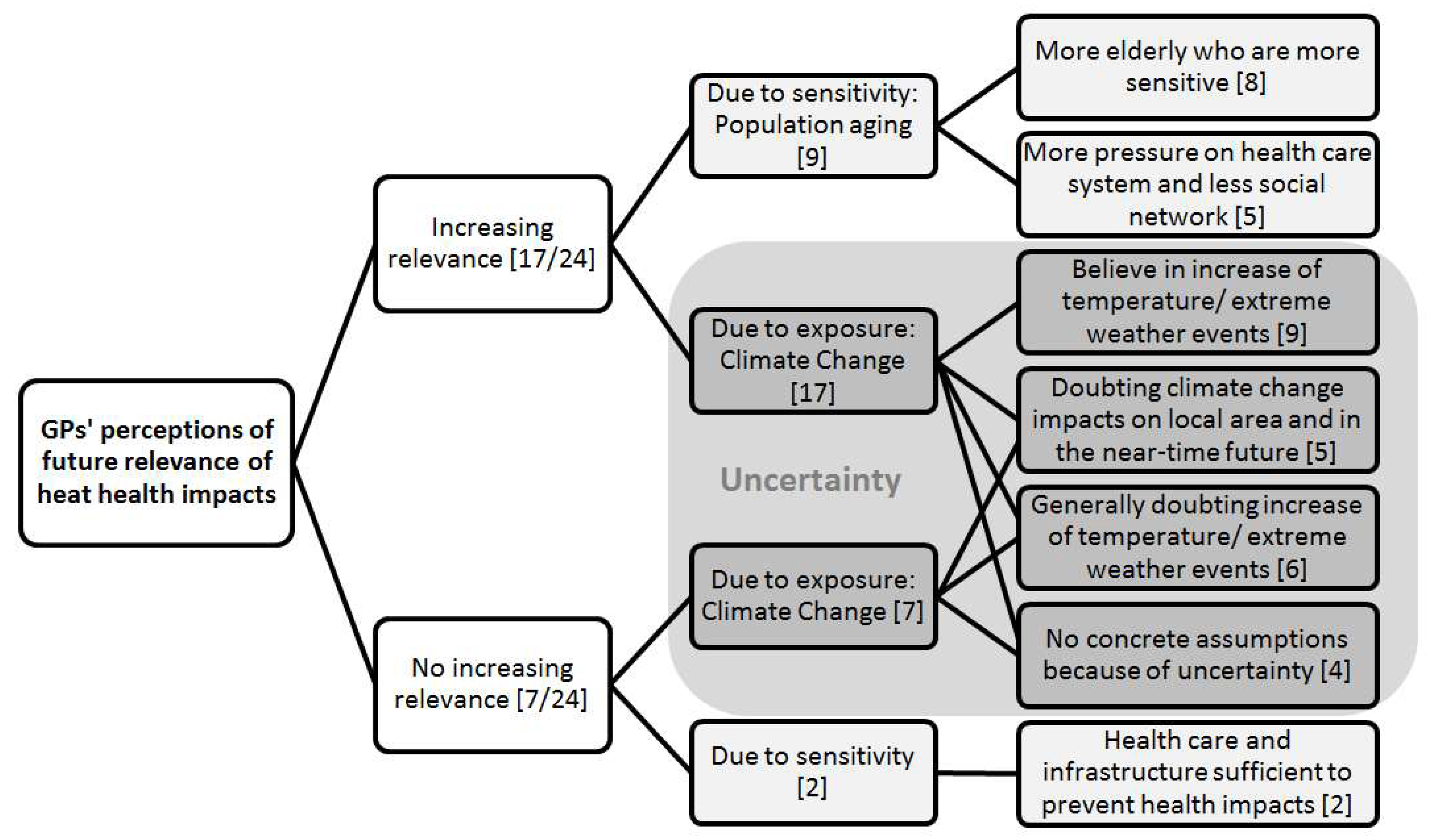
3.4.2. Future Relevance
3.4.3. Increasing Sensitivity through Population Ageing
Interviewer: “What role will this topic play in the future?”, GP: “Rather an increasing role. Not because of the heat alone, but simply because provision for the elderly comes more and more into focus, especially in the care sector. People just get older and older. This is a big question of staffing.”GP 12 (male, rural, 49, general medicine, single practice)
“It is of course not exactly predictable, whether the summers will really become warmer […]. From that point of view, I only see the greater relevance in the fact, that generally people become older and that the part of people over 75-years rises. I wouldn’t, thinking of the last summer, which wasn’t very good, automatically think that all the summers in the future will be hotter. But the proportion of elderly people definitely rises.”GP 15 (female, urban, 51, internal medicine, single practice)
3.4.4. Increasing Exposure through Climate Change
“Well I think that we will have more heat waves due to climate change. And that you have to consider […] how to react to that. Well, I do think that the relevance will rise in the next few decades, because I think that extreme weather will just increase due to climate change. (…) It is possible that then a challenge will arise to care for all those people.”GP 23 (male, suburban, 39, internal medicine, medical care center)
“The other thing is that it is supposed to become warmer and warmer (laughs). But this happens slowly. Presently, I don’t have the impression. Now it’s raining all the time. So, we don’t really know. Maybe it’s getting warmer, maybe we get a rather tropical climate, so we get more rainfall. I am not an expert in these questions. I don’t really believe in these weather prognoses.”GP 3 (male, urban, 53, general medicine, joint practice)
3.5. Overarching Theme: Importance of Social Support and Nursing Care
4. Discussion
4.1. Methodological Strengths and Limitations
4.2. GPs’ Perceptions of Heatwave Characteristics
4.3. GP’s Perceptions of Risk Factors to Suffer from Heat Health Impacts
4.4. GPs’ Perceptions of Morbidity as Heat Health Impact
4.5. GPs’ Perceptions of Mortality as Heat Health Impact
4.6. GPs’ Perceptions of Current and Future Relevance of Heat Health Impacts for the Elderly
5. Conclusions
Supplementary Materials
Author Contributions
Acknowledgments
Conflicts of Interest
Appendix A
| Introduction |
|---|
| Greeting and introduction of the interviewer |
Repetition of:
|
Definition of terms:
|
Repetition of ethical aspects as described and signed beforehand in the informed consent:
|
Note on procedure of interviews:
|
| A. Perceptions of Heat Health Impacts |
|
| B. Perceptions of Heat Health Impact Prevention |
|
| Pre-existing Disease [23/24] | Cardiovascular diseases (CVD) [15]: CVD in general [6], congestive heart failure [4], high blood pressure [4], arrhythmia [2], coronary heart disease [2], heart attack in patient history [1], stroke [1] |
| Multi-morbidity [8] | |
| Dementia or other cognitive impairment [8] | |
| Respiratory diseases (RD) [6]: Chronic Obstructive Pulmonary Disease (COPD) [4], RD in general [2], asthma [1] | |
| Renal Disease [6] | |
| Diabetes [6] | |
| Psychiatric disorder, e.g., depression [2] | |
| Other impairments: Electrolyte imbalance [2], acute infections (esp. diarrheal disease) [3], chronic disease in general [2], adiposity [1], collapse in patient history [1], dehydration in patient history [1] | |
| Socioeconomic Factors [19/24] | Social support and nursing care situation [14]: living alone without support [11], living alone in general [3], living alone or in care homes with insufficient support [2] |
| Housing [7]: warm housing situation [4], impaired access to logistics [3] | |
| Social status [4]: low financial capacity [3], low education [1] | |
| Individual Factors [18/24] | Age [16]: Old age [12], young age [4], old age as insufficient criteria [2] |
| Male Sex [1] (weaker social network) | |
| Genetics [3] | |
| Intake of Medication [14/24] | Cardiovascular medication [13]: antihypertensive medication in general [8], diuretics [9], beta-blocker [2], calcium antagonists [1], antiarrhythmic agents [1], |
| Other medication [4]: antibiotics [1], antidiabetics [1], St. John’s wort (photosensitivity) [1], non-prescribed medication (e.g., pain killers) [1]. | |
| Functional Impairments [5/24] | Impaired mobility or confinement to bed [5] |
| Alcohol Intake [2/24] | Alcohol intake [2] |
| Groups | Specific Diseases (ICD-10 Coding) [Number of GPs Mentioning It] |
|---|---|
| ICD-10 E86 Volume depletion/ E87 Other disorders of fluid, electrolyte and acid-base balance [22/24] | E86 Volume depletion OR T67.3 Heat exhaustion due to water depletion [18] |
| E87 Other disorders of fluid, electrolyte and acid-base balance OR T67.4 Heat exhaustion due to salt depletion [4] | |
| Circulatory diseases, ICD10-I00-I99 [15/24] | I99 Other and unspecified disorders of circulatory system [9]: usually naming circulatory collapse and circulatory dysregulation |
| I95 Hypotension [4] | |
| Other [3]: I74 Arterial embolism and thrombosis [1], I64 Stroke, not specified as hemorrhage or infarction [1], I49.9 Cardiac arrhythmia, unspecified [1] | |
| T67 Effects of heat and light [8/24] | T67.6 Heat fatigue, transient [5]; T67.0 Heatstroke and sunstroke [3]; T67.5 Heat exhaustion, unspecified [2], T67.1 Heat syncope [2]; T76.7 Heat edema [1] |
| Infectious diseases, ICD10-A00-B99 [7/24] | A00–A09 Intestinal infectious diseases [6] |
| Other [3]: B37.2 Candidiasis of skin and nail [1], L00–L08 Infections of the skin and subcutaneous tissue [2], N39.0 Urinary tract infection, site not specified [1] | |
| Organic mental disorders, ICD-F00-F09 [5/24] | Disorientation, cognitive or emotional impairment [4] (in line with F05–F07 *) |
| Aggravation of dementia [2] (F00–F003) | |
| Others [5/24] | N17 Acute renal failure [2]; J98.9 Respiratory disorder, unspecified [1]; L55 Sunburn [1]; Injuries from fall [3] |
References
- Schär, C.; Jendritzky, G. Climate Change: Hot news from summer 2003. Nature 2004, 432, 559. [Google Scholar] [CrossRef] [PubMed]
- Robine, J.-M.; Cheung, S.L.K.; Le Roy, S.; Van Oyen, H.; Griffiths, C.; Michel, J.-P.; Herrmann, F.R. Death toll exceeded 70,000 in Europe during the summer of 2003. Comptes Rendus Biol. 2008, 331, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Kendrovski, V.; Baccini, M.; Martinez, G.S.; Wolf, T.; Paunovic, E.; Menne, B. Quantifying Projected Heat Mortality Impacts under 21st-Century Warming Conditions for Selected European Countries. Int. J. Environ. Res. Public Health 2017, 14, 729. [Google Scholar] [CrossRef] [PubMed]
- Astrom, C.; Astrom, D.O.; Andersson, C.; Ebi, K.; Forsberg, B. Vulnerability Reduction Needed to Maintain Current Burdens of Heat-Related Mortality in a Changing Climate-Magnitude and Determinants. Int. J. Environ. Res. Public Health 2017, 14, 741. [Google Scholar] [CrossRef] [PubMed]
- Meehl, G.A.; Tebaldi, C. More intense, more frequent, and longer lasting heat waves in the 21st century. Science 2004, 305, 994–997. [Google Scholar] [CrossRef] [PubMed]
- Robinson, J.A. On the definition of a heat wave. J. Appl. Meteorol. 2000, 40, 762–775. [Google Scholar] [CrossRef]
- Erläuterungen und Kriterien zu Hitzewarnungen. Available online: http://www.wettergefahren.de/warnungen/hitzewarnungen.html (accessed on 31 July 2016).
- Becker, P.; Bucher, K.; Grätz, A.; Koppe, C.; Laschewski, G. Das medizin-meteorologische Informationsangebot für den Gesundheitssektor und die Öffentlichkeit. Promet Biometeorol. Des Menschen 2007, 33, 140–147. [Google Scholar]
- Havenith, G. Temperature Regulation, Heat Balance and Climatic Stress. In Extreme Weather Events and Public Health Responses; Kirch, W., Bertollini, R., Menne, B., Eds.; Springer: Berlin/Heidelberg, Germany, 2005; pp. 69–80. [Google Scholar]
- Zacharias, S.; Koppe, C.; Mücke, H.-G. Climate Change Effects on Heat Waves and Future Heat Wave-2005. Climate 2014, 3, 100–117. [Google Scholar] [CrossRef]
- Hajat, S.; O’Connor, M.; Kosatsky, T. Health effects of hot weather: from awareness of risk factors to effective health protection. Lancet 2010, 375, 856–863. [Google Scholar] [CrossRef]
- Astrom, D.O.; Forsberg, B.; Rocklov, J. Heat wave impact on morbidity and mortality in the elderly population: A review of recent studies. Maturitas 2011, 69, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Jendritzky, G.; Koppe, C.; Holst, T. Kapitel 3: Auswirkungen auf die menschliche Gesundheit. In PIK Report No, 99: KLARA, Klimawandel—Auswirkungen, Risiken, Anpassung in Baden-Württemberg; Stock, M., Gerstengarbe, F.-W., Eds.; Potsdam-Institut für Klimafolgenforschung: Potsdam, Germany, 2005. [Google Scholar]
- Vandentorren, S.; Bretin, P.; Zeghnoun, A.; Mandereau-Bruno, L.; Croisier, A.; Cochet, C.; Riberon, J.; Siberan, I.; Declercq, B.; Ledrans, M. August 2003 heat wave in France: Risk factors for death of elderly people living at home. Eur. J. Public Health 2006, 16, 583–591. [Google Scholar] [CrossRef] [PubMed]
- Westaway, K.; Frank, O.; Husband, A.; McClure, A.; Shute, R.; Edwards, S.; Curtis, J.; Rowett, D. Medicines can affect thermoregulation and accentuate the risk of dehydration and heat-related illness during hot weather. J. Clin. Pharm. Ther. 2015, 40, 363–367. [Google Scholar] [CrossRef] [PubMed]
- Schifano, P.; Cappai, G.; De Sario, M.; Michelozzi, P.; Marino, C.; Bargagli, A.M.; Perucci, C.A. Susceptibility to heat wave-related mortality: A follow-up study of a cohort of elderly in Rome. Environ. Health Glob. Access Sci. Source 2009, 8, 50. [Google Scholar] [CrossRef] [PubMed]
- Kovats, R.S.; Hajat, S. Heat stress and public health: A critical review. Annu. Rev. Public Health 2008, 29, 41–55. [Google Scholar] [CrossRef] [PubMed]
- Hirata, A.; Nomura, T.; Laakso, I. Computational estimation of decline in sweating in the elderly from measured body temperatures and sweating for passive heat exposure. Physiol. Meas. 2012, 33, N51–N60. [Google Scholar] [CrossRef] [PubMed]
- Petrofsky, J.S.; McLellan, K.; Bains, G.S.; Prowse, M.; Ethiraju, G.; Lee, S.; Gunda, S.; Lohman, E., III; Schwab, E. The influence of ageing on the ability of the skin to dissipate heat. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2009, 15, CR261–CR268. [Google Scholar]
- Hertel, S.; Le Tertre, A.; Jockel, K.H.; Hoffmann, B. Quantification of the heat wave effect on cause-specific mortality in Essen, Germany. Eur. J. Epidemiol. 2009, 24, 407–414. [Google Scholar] [CrossRef] [PubMed]
- Breitner, S.; Wolf, K.; Peters, A.; Schneider, A. Short-term effects of air temperature on cause-specific cardiovascular mortality in Bavaria, Germany. Heart Br. Card. Soc. 2014, 100, 1272–1280. [Google Scholar] [CrossRef] [PubMed]
- Bunker, A.; Wildenhain, J.; Vandenbergh, A.; Henschke, N.; Rocklov, J.; Hajat, S.; Sauerborn, R. Effects of Air Temperature on Climate-Sensitive Mortality and Morbidity Outcomes in the Elderly; a Systematic Review and Meta-analysis of Epidemiological Evidence. EBioMedicine 2016, 6, 258–268. [Google Scholar] [CrossRef] [PubMed]
- Michelozzi, P.; Accetta, G.; De Sario, M.; D’Ippoliti, D.; Marino, C.; Baccini, M.; Biggeri, A.; Anderson, H.R.; Katsouyanni, K.; Ballester, F.; et al. High temperature and hospitalizations for cardiovascular and respiratory causes in 12 European cities. Am. J. Respir. Crit. Care Med. 2009, 179, 383–389. [Google Scholar] [CrossRef] [PubMed]
- Lowe, R.; Garcia-Diez, M.; Ballester, J.; Creswick, J.; Robine, J.M.; Herrmann, F.R.; Rodo, X. Evaluation of an Early-Warning System for Heat Wave-Related Mortality in Europe: Implications for Sub-seasonal to Seasonal Forecasting and Climate Services. Int. J. Environ. Res. Public Health 2016, 13, 206. [Google Scholar] [CrossRef] [PubMed]
- Abrahamson, V.; Raine, R. Health and social care responses to the Department of Health Heatwave Plan. J. Public Health 2009, 31, 478–489. [Google Scholar] [CrossRef] [PubMed]
- Bleijenberg, N.; Ten Dam, V.H.; Drubbel, I.; Numans, M.E.; de Wit, N.J.; Schuurmans, M.J. Development of a Proactive Care Program (U-CARE) to Preserve Physical Functioning of Frail Older People in Primary Care. J. Nurs. Scholarsh. 2013, 45, 230–237. [Google Scholar] [CrossRef] [PubMed]
- Damschroder, L.J.; Aron, D.C.; Keith, R.E.; Kirsh, S.R.; Alexander, J.A.; Lowery, J.C. Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implement. Sci. IS 2009, 4, 50. [Google Scholar] [CrossRef] [PubMed]
- Matthies, F.; Bickler, G.; Marin, N.C. Heat-Health Action Plans: Guidance; WHO Regional Office for Europe: Kopenhagen, Denmark, 2008. [Google Scholar]
- Bittner, M.I.; Stossel, U. Perceptions of heatwave risks to health: Results of an qualitative interview study with older people and their carers in Freiburg, Germany. Psycho-Soc. Med. 2012, 9. [Google Scholar] [CrossRef]
- Nitschke, M.; Hansen, A.; Bi, P.; Pisaniello, D.; Newbury, J.; Kitson, A.; Tucker, G.; Avery, J.; Grande, E.D. Risk Factors, Health Effects and Behaviour in Older People during Extreme Heat: A Survey in South Australia. Int. J. Environ. Res. Public Health 2013, 10, 6721–6733. [Google Scholar] [CrossRef] [PubMed]
- Wilson, L.; Black, D.; Veitch, C. Heatwaves and the elderly: The role of the GP in reducing morbidity. Aust. Fam. Phys. 2011, 40, 637. [Google Scholar]
- McInnes, J.A.; Ibrahim, J.E. Minimising harm to older Victorians from heatwaves: A qualitative study of the role of community-based health profession and carer organisations. Aust. J. Ageing 2010, 29, 104–110. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, J.; McInnes, J.; Andrianopoulos, N.; Evans, S. Minimising harm from heatwaves: A survey of awareness, knowledge, and practices of health professionals and care providers in Victoria, Australia. Int. J. Public Health 2012, 57, 297–304. [Google Scholar] [CrossRef] [PubMed]
- Williams, S.; Bi, P.; Newbury, J.; Robinson, G.; Pisaniello, D.; Saniotis, A.; Hansen, A. Extreme heat and health: perspectives from health service providers in rural and remote communities in South Australia. Int. J. Environ. Res. Public Health 2013, 10, 5565–5583. [Google Scholar] [CrossRef] [PubMed]
- Capellaro, M.; Sturm, D. Evaluation von Informationssystemen zu Klimawandel und Gesundheit Band 2: Anpassung an den Klimawandel: Strategie für die Versorgung bei Extremwetterereignissen; Umweltbundesamt: Dessau-Roßlau, Germany, 2015. [Google Scholar]
- Chaudoir, S.R.; Dugan, A.G.; Barr, C.H. Measuring factors affecting implementation of health innovations: A systematic review of structural, organizational, provider, patient, and innovation level measures. Implement. Sci. IS 2013, 8, 22. [Google Scholar] [CrossRef] [PubMed]
- Durlak, J.A.; DuPre, E.P. Implementation matters: A review of research on the influence of implementation on program outcomes and the factors affecting implementation. Am. J. Commun. Psychol. 2008, 41, 327–350. [Google Scholar] [CrossRef] [PubMed]
- Mays, N.; Pope, C. Qualitative research: Observational methods in health care settings. BMJ 1995, 311, 182. [Google Scholar] [CrossRef] [PubMed]
- Jendritzky, G.; Grätz, A.; Laschewski, G.; Scheid, G. Das Bioklima in Deutschland. Bioklimakarte mit Begleittext und Information zur Wohnortwahl; Flöttmann Verlag: Gütersloh, Germany, 2003. [Google Scholar]
- Loidl-Stuppi, J. Wie sieht das Durchschnittseinkommen in Baden-Württemberg aus? Erkenntnisse aus der Einkommensteuerstatistik 2004. Stat. Monatsheft Baden Württ. 2009, 7, 39–42. [Google Scholar]
- Flaig, B.B. Heidelberger Migrantenstudie 2008—Lebenslagen und Milieus der Heidelberger mit Migrationshintergrund. In Schriften zur Stadtentwicklung; Bürgeramt Heidelberg, Amt für Stadtentwicklung und Statistik: Heidelberg, Germany, 2008. [Google Scholar]
- Kommunale Statistikstelle Mannheim Einwohnerdaten zum 31.12.2013. Available online: https://www.mannheim.de/stadt-gestalten/bevoelkerung (accessed on 13 May 2014).
- Kassenärztliche Vereinigung Baden-Württemberg. Suche nach Ärzten und Psychotherapeuten. 2014. Available online: http://www.arztsuche-bw.de/ (accessed on 13 April 2013).
- Patton, M.Q. Qualitative Evaluation and Research Methods; SAGE Publications, Inc.: Thousand Oaks, CA, USA, 1990. [Google Scholar]
- Marshall, M.N. Sampling for qualitative research. Fam. Pract. 1996, 13, 522–526. [Google Scholar] [CrossRef] [PubMed]
- Ritchie, J.; Spencer, L. Qualitative data analysis for applied policy research. In The Qualitative Researcher’s Companion; Huberman, M., Miles, M.B., Eds.; SAGE Publications: Thousand Oaks, CA, USA; London, UK; New Delhi, India, 2002; pp. 305–329. [Google Scholar]
- Meuser, M.; Nagel, U. Das Experteninterview—Konzeptionelle Grundlagen und methodische Anlage. In Methoden Der Vergleichenden Politik- und Sozialwissenschaft; Pickel, S., Pickel, G., Lauth, H.-J., Jahn, D., Eds.; VS Verlag für Sozialwissenschaften: Berlin, Germany, 2009; pp. 465–479. [Google Scholar]
- Gläser, J.; Laudel, G. Experteninterviews und Qualitative Inhaltsanalyse; VS Verlag: Berlin, Germany, 2006. [Google Scholar]
- Dresing, T.; Pehl, T. Praxisbuch Interview & Transkription. Regelsysteme und Anleitungen für Qualitative ForscherInnen; Thorsten Dresing, T.P., Ed.; Eigenverlag: Marburg, Germany, 2012; p. 72. [Google Scholar]
- QSR_International_Pty_Ltd. NVivo; QSR International Pty Ltd.: Melbourne, Australia, 2016. [Google Scholar]
- Abrahamson, V.; Wolf, J.; Lorenzoni, I.; Fenn, B.; Kovats, S.; Wilkinson, P.; Adger, W.N.; Raine, R. Perceptions of heatwave risks to health: Interview-based study of older people in London and Norwich, UK. J. Public Health 2008, 31, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Cope, D.G. Methods and meanings: Credibility and trustworthiness of qualitative research. In Oncology Nursing Forum; Oncology Nursing Society: Pittsburgh, PA, USA, 2014; Volume 41. [Google Scholar]
- Lowe, D.; Ebi, K.L. Forsberg B: Heatwave early warning systems and adaptation advice to reduce human health consequences of heatwaves. Int. J. Environ. Res. Public Health 2011, 8. [Google Scholar] [CrossRef] [PubMed]
- World Meteorological Organization (WMO). Heatwave. 2016. Available online: http://www.metoffice.gov.uk/learning/learn-about-the-weather/weather-phenomena/heatwave (accessed on 26 October 2016).
- Xu, Z.; FitzGerald, G.; Guo, Y.; Jalaludin, B.; Tong, S. Impact of heatwave on mortality under different heatwave definitions: A systematic review and meta-analysis. Environ. Int. 2016, 89–90, 193–203. [Google Scholar] [CrossRef] [PubMed]
- Stafoggia, M.; Forastiere, F.; Agostini, D.; Biggeri, A.; Bisanti, L.; Cadum, E.; Caranci, N.; de’ Donato, F.; De Lisio, S.; De Maria, M.; et al. Vulnerability to heat-related mortality: A multicity, population-based, case-crossover analysis. Epidemiol. Camb. Mass 2006, 17, 315–323. [Google Scholar] [CrossRef] [PubMed]
- Zanobetti, A.; O’Neill, M.S.; Gronlund, C.J.; Schwartz, J.D. Summer temperature variability and long-term survival among elderly people with chronic disease. Proc. Natl. Acad. Sci. USA 2012, 109, 6608–6613. [Google Scholar] [CrossRef] [PubMed]
- Belmin, J.; Auffray, J.C.; Berbezier, C.; Boirin, P.; Mercier, S.; de Reviers, B.; Golmard, J.L. Level of dependency: A simple marker associated with mortality during the 2003 heatwave among French dependent elderly people living in the community or in institutions. Age Ageing 2007, 36, 298–303. [Google Scholar] [CrossRef] [PubMed]
- Smith, S.; Elliot, A.J.; Hajat, S.; Bone, A.; Smith, G.E.; Kovats, S. Estimating the burden of heat illness in England during the 2013 summer heatwave using syndromic surveillance. J. Epidemiol. Community Health 2016, 70, 459–465. [Google Scholar] [CrossRef] [PubMed]
- Smith, S.; Elliot, A.J.; Hajat, S.; Bone, A.; Bates, C.; Smith, G.E.; Kovats, S. The Impact of Heatwaves on Community Morbidity and Healthcare Usage: A Retrospective Observational Study Using Real-Time Syndromic Surveillance. Int. J. Environ. Res. Public Health 2016, 13, 132. [Google Scholar] [CrossRef] [PubMed]
- D’Ippoliti, D.; Michelozzi, P.; Marino, C.; de’Donato, F.; Menne, B.; Katsouyanni, K.; Kirchmayer, U.; Analitis, A.; Medina-Ramón, M.; Paldy, A.; et al. The impact of heat waves on mortality in 9 European cities: Results from the EuroHEAT project. Environ. Health A Glob. Access Sci. Source 2010, 9, 37–45. [Google Scholar] [CrossRef] [PubMed]
- Kassenärztliche Bundesvereinigung. Statistische Informationen aus dem Bundesarztregister (Bundesgebiet Insgesamt). Available online: http://www.kbv.de/media/sp/2013_12_31.pdf (accessed on 13 May 2014).
- Martiello, M.A.; Giacchi, M.V. High temperatures and health outcomes: A review of the literature. Scand. J. Public Health 2010, 38, 826–837. [Google Scholar] [CrossRef] [PubMed]
- Baccini, M.; Kosatsky, T.; Analitis, A.; Anderson, H.R.; D’Ovidio, M.; Menne, B.; Michelozzi, P.; Biggeri, A. Impact of heat on mortality in 15 European cities: Attributable deaths under different weather scenarios. J. Epidemiol. Community Health 2011, 65, 64–70. [Google Scholar] [CrossRef] [PubMed]
- Gasparrini, A.; Armstrong, B.; Kovats, S.; Wilkinson, P. The effect of high temperatures on cause-specific mortality in England and Wales. Occup. Environ. Med. 2012, 69, 56–61. [Google Scholar] [CrossRef] [PubMed]
- Gasparrini, A.; Armstrong, B. The impact of heat waves on mortality. Epidemiol. Camb. Mass 2011, 22, 68–73. [Google Scholar] [CrossRef] [PubMed]
- Hondula, D.M.; Davis, R.E.; Leisten, M.J.; Saha, M.V.; Veazey, L.M. Wegner CR: Fine-scale spatial variability of heat-related mortality in Philadelphia County, USA, from 1983–2008: A case-series analysis. Environ. Health A Glob. Access Sci. Source 2012, 11, 16. [Google Scholar]
- Blattner, B.; Heckenhahn, M.; Georgy, S.; Grewe, H.A.; Kupski, S. Identifying residential areas with heat-related health risks. Sociodemographic and climate data mapping as a planning tool for targeted prevention strategies. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2010, 53, 75–81. [Google Scholar] [PubMed]
- Wolf, T.; McGregor, G. The development of a heat wave vulnerability index for London, United Kingdom. Weather Clim. Extrem. 2013, 1, 59–68. [Google Scholar] [CrossRef]
- Van der Linden, S. The social-psychological determinants of climate change risk perceptions: Towards a comprehensive model. J. Environ. Psychol. 2015, 41, 112–124. [Google Scholar] [CrossRef]
- Anaker, A.; Nilsson, M.; Holmner, A.; Elf, M. Nurses’ perceptions of climate and environmental issues: A qualitative study. J. Adv. Nurs. 2015, 71, 1883–1891. [Google Scholar] [CrossRef] [PubMed]
- Prasad, V.; Thistlethwaite, W.; Dale, W. Effect of clinical vignettes on senior medical students’ opinions of climate change. South. Med. J. 2011, 104, 401–404. [Google Scholar] [CrossRef] [PubMed]
- Gifford, R. The dragons of inaction: Psychological barriers that limit climate change mitigation and adaptation. Am. Psychol. 2011, 66, 290. [Google Scholar] [CrossRef] [PubMed]
- Lorenzoni, I.; Nicholson-Cole, S.; Whitmarsh, L. Barriers perceived to engaging with climate change among the UK public and their policy implications. Glob. Environ. Chang. 2007, 17, 445–459. [Google Scholar] [CrossRef]
- Recommendations for Action—Heat Action Plans to Protect Human Health; Federal Ministry for the Environment, Nature Conservation, Building and Nuclear Safety: Bonn, Germany, 2017.
- Capellaro, M.; Sturm, D. Evaluation von Informationssystemen zu Klimawandel und Gesundheit Band 1: Anpassung an den Klimawandel: Evaluation Bestehender Nationaler Informationssysteme (UVIndex, Hitzewarnsystem, Pollenflug- und Ozonvorhersage) aus Gesundheitlicher Sicht—Wie Erreichen Wir Die Empfindlichen Bevölkerungsgruppen? Umweltbundesamt: Dessau-Roßlau, Germany, 2015. [Google Scholar]
- Bundesregierung, D. Aktionsplan zur Deutschen Anpassungsstrategie an den Klimawandel; Bundeskabinett: Berlin, Germany, 2011. [Google Scholar]
- Bittighofer, P.M.; Fischer, G.; Geisel, B.; Härtig, E.; Jaroni, H.; Jovanovic, S.; Kluge, S.; Link, B.; Otzelberger, K.; Rebmann, A.; et al. Anpassungsstrategie Baden-Württemberg an die Folgen des Klimawandels, Fachgutachten für das Handlungsfeld Gesundheit. In Teil A: Langfassung: Ministeriums für Umwelt; Klima und Energiewirtschaft Baden-Württemberg: Stuttgart, Germany, 2013. [Google Scholar]
- Krampen, R.; Oppermann, A.; Schetzkens, R. Außergewöhnliche Hitzeperioden: Vorbereitung und Vorgehen in Stationären Einrichtungen der Alten-und Behindertenhilfe; Regierungspräsidium Gießen: Gießen, Germany, 2017; Volume 2. [Google Scholar]
| Drug Groups | Possible Effects in Heat Waves |
|---|---|
| Antidepressants, anticonvulsants, antipsychotics, anticholinergic drugs, diuretics, antihypertensive drugs such as Angiotensin Converting Enzyme (ACE) inhibitors or Angiotensin II Receptor Blockers (ARBs), benzodiazepines, opioids | Impairment of physiological or behavioral adaptation to heat:
|
| Oral antidiabetics, opioids, novel oral anticoagulants, digoxin, lithium | Drug toxicity in dehydrated patients due to reduced renal function |
| GP’s Rationales for Attributed Relevance | Attributed Current Relevance | ||
|---|---|---|---|
| Low Relevance [6/24] | Balanced Attitude [9/24] | High Relevance [9/24] | |
| Sensitivity: Individual risk factors Social support and nursing care |
|
|
|
|
|
| |
| Exposure |
|
|
|
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Herrmann, A.; Sauerborn, R. General Practitioners’ Perceptions of Heat Health Impacts on the Elderly in the Face of Climate Change—A Qualitative Study in Baden-Württemberg, Germany. Int. J. Environ. Res. Public Health 2018, 15, 843. https://doi.org/10.3390/ijerph15050843
Herrmann A, Sauerborn R. General Practitioners’ Perceptions of Heat Health Impacts on the Elderly in the Face of Climate Change—A Qualitative Study in Baden-Württemberg, Germany. International Journal of Environmental Research and Public Health. 2018; 15(5):843. https://doi.org/10.3390/ijerph15050843
Chicago/Turabian StyleHerrmann, Alina, and Rainer Sauerborn. 2018. "General Practitioners’ Perceptions of Heat Health Impacts on the Elderly in the Face of Climate Change—A Qualitative Study in Baden-Württemberg, Germany" International Journal of Environmental Research and Public Health 15, no. 5: 843. https://doi.org/10.3390/ijerph15050843
APA StyleHerrmann, A., & Sauerborn, R. (2018). General Practitioners’ Perceptions of Heat Health Impacts on the Elderly in the Face of Climate Change—A Qualitative Study in Baden-Württemberg, Germany. International Journal of Environmental Research and Public Health, 15(5), 843. https://doi.org/10.3390/ijerph15050843





