Eating Alone is Differentially Associated with the Risk of Metabolic Syndrome in Korean Men and Women
Abstract
:1. Introduction
2. Data and Methods
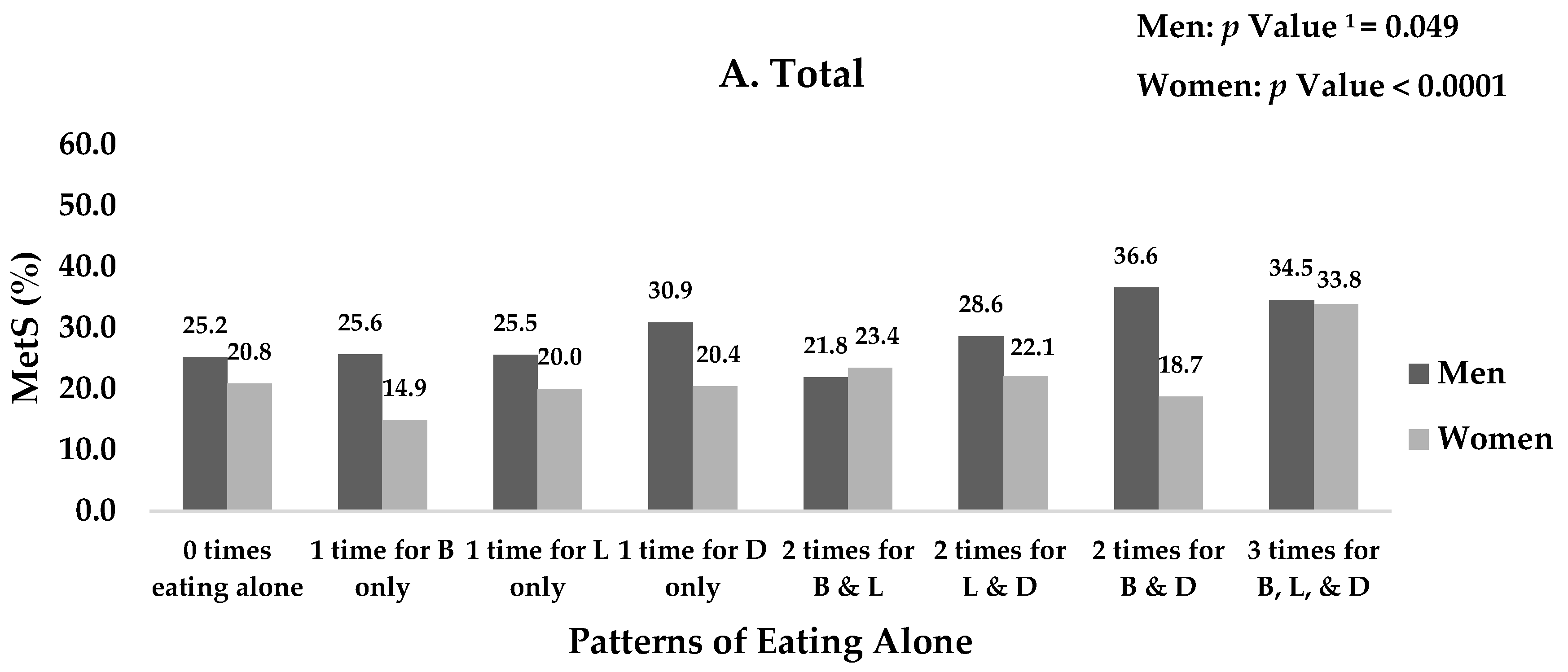
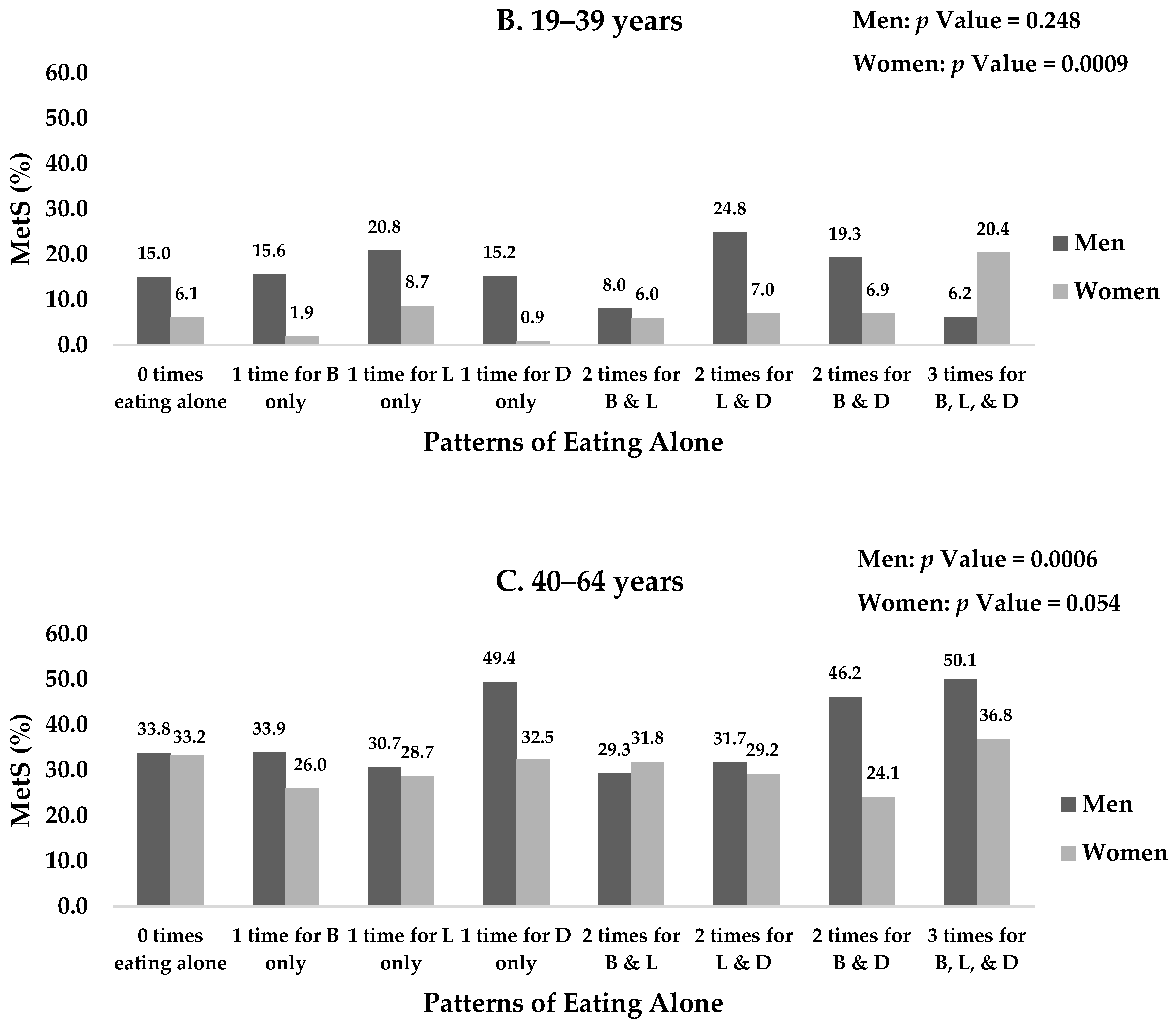
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Lee, C. Why More Koreans Are Eating Alone. Available online: http://www.koreaherald.com/view.php?ud=20160529000252 (accessed on 8 May 2018).
- Kim, M. A New Generation of Beautiful Loners Is Changing Seoul Fashion for the Better. Available online: https://www.vogue.com/article/single-independence-movement-in-seoul-korean-fashion (accessed on 8 May 2018).
- Dare to Dine Solo. Available online: http://magazine.seoulselection.com/2017/03/24/dare-to-dine-solo/ (accessed on 8 May 2018).
- Statistics Korea. Results of the 2016 Population and Housing Census (Population, Household and Housing). Available online: http://kostat.go.kr/portal/korea/kor_nw/2/1/index.board?bmode=read&aSeq=359629&pageNo=&rowNum=10&amSeq=&sTarget=&sTxt= (accessed on 9 April 2018).
- Fischler, C. Food habits, social change and the nature/culture dilemma. Inf. (Int. Soc. Sci. Counc.) 1980, 19, 937–953. [Google Scholar] [CrossRef]
- Sobal, J.; Nelson, M.K. Commensal eating patterns: A community study. Appetite 2003, 41, 181–190. [Google Scholar] [CrossRef]
- Takeda, W.; Melby, M.K. Spatial, temporal, and health associations of eating alone: A cross-cultural analysis of young adults in urban Australia and Japan. Appetite 2017, 118, 149–160. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.; Cho, W.; Oh, Y. Comparison of eating behavior between commensality and solo-eating of university students by BMI. Korean J. Community Nutr. 2012, 17, 280–289. [Google Scholar] [CrossRef]
- Tani, Y.; Kondo, N.; Takagi, D.; Saito, M.; Hikichi, H.; Ojima, T.; Kondo, K. Combined effects of eating alone and living alone on unhealthy dietary behaviors, obesity and underweight in older Japanese adults: Results of the JAGES. Appetite 2015, 95, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Kimura, Y.; Wada, T.; Okumiya, K.; Ishimoto, Y.; Fukutomi, E.; Kasahara, Y.; Chen, W.; Sakamoto, R.; Fujisawa, M.; Otsuka, K. Eating alone among community-dwelling Japanese elderly: Association with depression and food diversity. J. Nutr. Health Aging 2012, 16, 728–731. [Google Scholar] [CrossRef] [PubMed]
- Kuroda, A.; Tanaka, T.; Hirano, H.; Ohara, Y.; Kikutani, T.; Furuya, H.; Obuchi, S.P.; Kawai, H.; Ishii, S.; Akishita, M.; et al. Eating alone as social disengagement is strongly associated with depressive symptoms in Japanese community-dwelling older adults. J. Am. Med. Dir. Assoc. 2015, 16, 578–585. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Shen, W.; Wang, C.; Zhang, X.; Xiao, Y.; He, F.; Zhai, Y.; Li, F.; Shang, X.; Lin, J. Association between eating alone and depressive symptom in elders: A cross-sectional study. BMC Geriatr. 2016, 16, 19. [Google Scholar] [CrossRef] [PubMed]
- Song, E.G.; Yoon, Y.S.; Yang, Y.J.; Lee, E.S.; Lee, J.H.; Lee, J.Y.; Park, W.J.; Park, S.Y. Factors associated with eating alone in Korean adults: Findings from the Sixth Korea National Health and Nutrition Examination Survey, 2014. Korean J. Fam. Pract. 2017, 7, 698–706. [Google Scholar] [CrossRef]
- Yiengprugsawan, V.; Banwell, C.; Takeda, W.; Dixon, J.; Seubsman, S.A.; Sleigh, A.C. Health, happiness and eating together: What can a large Thai cohort study tell us? Glob. J. Health Sci. 2015, 7, 270–277. [Google Scholar] [CrossRef] [PubMed]
- Alberti, K.G.M.M.; Zimmet, P.; Shaw, J. Metabolic syndrome—A new world-wide definition. A consensus statement from the international diabetes federation. Diabet. Med. 2006, 23, 469–480. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.; Shin, H.; Song, J.H.; Kwak, S.H.; Kang, S.M.; Yoon, J.W.; Choi, S.H.; Cho, S.I.; Park, K.S.; Lee, H.K. Increasing prevalence of metabolic syndrome in Korea: The Korean National Health and Nutrition Examination Survey for 1998–2007. Diabetes Care 2011, 34, 1323–1328. [Google Scholar] [CrossRef] [PubMed]
- Woo, H.D.; Shin, A.; Kim, J. Dietary patterns of Korean adults and the prevalence of metabolic syndrome: A cross-sectional study. PLoS ONE 2014, 9, e111593. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.; Shin, D. A healthy beverage consumption pattern is inversely associated with the risk of obesity and metabolic abnormalities in Korean adults. J. Med. Food 2018. [Google Scholar] [CrossRef] [PubMed]
- Park, H.S.; Oh, S.W.; Cho, S.-I.; Choi, W.H.; Kim, Y.S. The metabolic syndrome and associated lifestyle factors among South Korean adults. Int. J. Epidemiol. 2004, 33, 328–336. [Google Scholar] [CrossRef] [PubMed]
- Cho, W.; Takeda, W.; Oh, Y.; Aiba, N.; Lee, Y. Perceptions and practices of commensality and solo-eating among Korean and Japanese university students: A cross-cultural analysis. Nutr. Res. Pract. 2015, 9, 523–529. [Google Scholar] [CrossRef] [PubMed]
- Kwon, A.R.; Yoon, Y.S.; Min, K.P.; Lee, Y.K.; Jeon, J.H. Eating alone and metabolic syndrome: A population-based Korean National Health and Nutrition Examination Survey 2013–2014. Obes. Res. Clin. Pract. 2017. [Google Scholar] [CrossRef] [PubMed]
- Hong, S.-Y. Association between meal companionship and depression in older adults: Data from KNHANES IV-2. J. Korean Soc. Living Environ. Syst. 2016, 23, 617–627. [Google Scholar] [CrossRef]
- Expert Panel on Detection, E. Executive summary of the Third Report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA 2001, 285, 2486. [Google Scholar]
- Alberti, K.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.-C.; James, W.P.T.; Loria, C.M.; Smith, S.C. Harmonizing the metabolic syndrome: A joint interim statement of the international diabetes federation task force on epidemiology and prevention; national heart, lung, and blood institute; American heart association; world heart federation; international atherosclerosis society; and international association for the study of obesity. Circulation 2009, 120, 1640–1645. [Google Scholar] [PubMed]
- Kweon, S.; Kim, Y.; Jang, M.-J.; Kim, Y.; Kim, K.; Choi, S.; Chun, C.; Khang, Y.-H.; Oh, K. Data resource profile: The Korea National Health and Nutrition Examination Survey (KNHANES). Int. J. Epidemiol. 2014, 43, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Korea National Statistical Office. Projections of the Number of Households: 2015~2014. Available online: http://kostat.go.kr/portal/korea/kor_nw/2/2/6/index.board?bmode=read&bSeq=&aSeq=359963&pageNo=1&rowNum=10&navCount=10&currPg=&sTarget=title&sTxt= (accessed on 11 April 2018).
- Kim, K.; Kim, M.K.; Shin, Y.-J.; Lee, S.S. Factors related to household food insecurity in the Republic of Korea. Public Health Nutr. 2011, 14, 1080–1087. [Google Scholar] [CrossRef] [PubMed]
- Tani, Y.; Kondo, N.; Noma, H.; Miyaguni, Y.; Saito, M.; Kondo, K. Eating alone yet living with others is associated with mortality in older men: The JAGES Cohort Survey. J. Gerontol. B Psychol. Sci. Soc. Sci. 2017. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, A.; Iso, H.; Toyoshima, H.; Fujino, Y.; Mizoue, T.; Yoshimura, T.; Inaba, Y.; Tamakoshi, A. Marital status and mortality among Japanese men and women: The Japan Collaborative Cohort Study. BMC Public Health 2007, 7, 73. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, R.M.; Kronick, R.G. Marital status and longevity in the United States population. J. Epidemiol. Community Health 2006, 60, 760–765. [Google Scholar] [CrossRef] [PubMed]
- Floud, S.; Balkwill, A.; Canoy, D.; Wright, F.L.; Reeves, G.K.; Green, J.; Beral, V.; Cairns, B.J. Marital status and ischemic heart disease incidence and mortality in women: A large prospective study. BMC Med. 2014, 12, 42. [Google Scholar] [CrossRef] [PubMed]
- Baek, Y.; Joung, H.; Shin, S. The association between vegetable intake and marital status in Korean adults aged 30 years and over: Based on the 2007~2010 Korea National Health and Nutrition Examination Survey. J. Nutr. Health 2015, 48, 192–198. [Google Scholar] [CrossRef]
- Jung, C.H.; Lee, J.S.; Ahn, H.J.; Choi, J.S.; Noh, M.Y.; Lee, J.J.; Lee, E.Y.; Lim, J.H.; Lee, Y.R.; Yoon, S.Y.; et al. Association of meal frequency with metabolic syndrome in Korean adults: From the Korea National Health and Nutrition Examination Survey (KNHANES). Diabetol. Metab. Syndr. 2017, 9, 77. [Google Scholar] [CrossRef] [PubMed]
- Devaraj, S.; Wang-Polagruto, J.; Polagruto, J.; Keen, C.L.; Jialal, I. High-fat, energy-dense, fast-food-style breakfast results in an increase in oxidative stress in metabolic syndrome. Metab. Clin. Exp. 2008, 57, 867–870. [Google Scholar] [CrossRef] [PubMed]
- Furukawa, S.; Fujita, T.; Shimabukuro, M.; Iwaki, M.; Yamada, Y.; Nakajima, Y.; Nakayama, O.; Makishima, M.; Matsuda, M.; Shimomura, I. Increased oxidative stress in obesity and its impact on metabolic syndrome. J. Clin. Investig. 2004, 114, 1752–1761. [Google Scholar] [CrossRef] [PubMed]
- Chung, H.-K.; Yang, H.J.; Shin, D.; Chung, K.R. Aesthetics of Korean foods: The symbol of Korean culture. J. Ethn. Foods 2016, 3, 178–188. [Google Scholar] [CrossRef]
- Symons, M. Simmel’s gastronomic sociology: An overlooked essay. Food Foodways 1994, 5, 333–351. [Google Scholar] [CrossRef]
| Sociodemographic and Lifestyle Characteristics | Men | Women | Total | p Value 1 | ||
|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | ||
| Age (years) | ||||||
| 19–29 | 607 | (23.0) | 755 | (20.3) | 1362 | <0.0001 |
| 30–39 | 740 | (22.5) | 1122 | (21.1) | 1862 | |
| 40–49 | 859 | (25.2) | 1366 | (25.8) | 2225 | |
| 50–59 | 950 | (23.4) | 1481 | (24.6) | 2431 | |
| 60–64 | 468 | (5.9) | 640 | (8.3) | 1108 | |
| Education | ||||||
| ≤Elementary School | 299 | (5.8) | 692 | (10.2) | 991 | <0.0001 |
| Middle School Graduate | 319 | (7.1) | 575 | (9.7) | 894 | |
| High School Graduate | 1444 | (42.7) | 2110 | (40.8) | 3554 | |
| ≥College Graduate | 1562 | (44.4) | 1987 | (39.3) | 3549 | |
| Income | ||||||
| Highest | 927 | (25.4) | 1385 | (26.1) | 2312 | 0.3706 |
| Upper Middle | 902 | (24.6) | 1384 | (25.5) | 2286 | |
| Lower Middle | 945 | (26.2) | 1332 | (24.7) | 2277 | |
| Lowest | 850 | (23.9) | 1263 | (23.7) | 2113 | |
| Occupation | ||||||
| Employed | 2990 | (81.4) | 3062 | (57.3) | 6052 | <0.0001 |
| Unemployed | 634 | (18.6) | 2302 | (42.7) | 2936 | |
| No. of Family Members in a Household | ||||||
| 1 | 256 | (7.1) | 277 | (4.5) | 533 | <0.0001 |
| 2 | 783 | (18.0) | 1253 | (20.5) | 2036 | |
| 3 | 1031 | (29.3) | 1536 | (30.2) | 2567 | |
| 4 | 1141 | (33.8) | 1626 | (31.7) | 2767 | |
| 5 | 315 | (9.1) | 498 | (9.9) | 813 | |
| ≥6 | 98 | (2.7) | 174 | (3.2) | 272 | |
| Household Generation Types | ||||||
| Single-Person Household | 256 | (7.1) | 277 | (4.5) | 533 | <0.0001 |
| 1 Generation Households | 641 | (14.1) | 954 | (15.2) | 1595 | |
| 2 Generations Households | 2442 | (71.1) | 3636 | (71.2) | 6078 | |
| ≥3 Generations Households | 285 | (7.7) | 497 | (9.1) | 782 | |
| Marital Status | ||||||
| Married | 2759 | (69.3) | 4501 | (78.5) | 7260 | <0.0001 |
| Unmarried | 865 | (30.7) | 863 | (21.5) | 1728 | |
| Physical Activity | ||||||
| Yes | 1596 | (47.2) | 2095 | (41.5) | 3691 | <0.0001 |
| No | 2028 | (52.8) | 3269 | (58.5) | 5297 | |
| Smoking Status | ||||||
| Nonsmoker | 989 | (29.8) | 4894 | (90.7) | 5883 | <0.0001 |
| Former Smoker | 1142 | (28.1) | 214 | (4.3) | 1356 | |
| Current Smoker | 1493 | (42.1) | 256 | (5.0) | 1749 | |
| Men | 0 Times Eating Alone (n = 1975) | 1 Time for B Only (n = 572) | 1 Time for L Only (n = 312) | 1 Time for D Only (n = 192) | 2 Times for B & L (n = 127) | 2 Times for L & D (n = 133) | 2 Times for B & D (n = 163) | 3 Times for B, L, & D (n = 150) | p Value 1 | ||||||||
| n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | ||
| Age (years) | |||||||||||||||||
| 19–29 | 303 | (20.6) | 87 | (20.8) | 71 | (32.7) | 45 | (32.0) | 22 | (24.5) | 34 | (34.9) | 22 | (18.3) | 23 | (23.0) | <0.0001 |
| 30–39 | 457 | (25.2) | 125 | (24.4) | 55 | (19.7) | 40 | (22.2) | 13 | (10.4) | 13 | (10.7) | 24 | (17.4) | 13 | (12.5) | |
| 40–49 | 505 | (27.4) | 154 | (26.7) | 55 | (18.2) | 44 | (23.3) | 30 | (29.4) | 24 | (20.5) | 30 | (19.7) | 17 | (14.1) | |
| 50–59 | 481 | (21.7) | 146 | (23.8) | 77 | (21.2) | 47 | (19.0) | 34 | (25.5) | 47 | (28.6) | 64 | (37.8) | 54 | (33.5) | |
| 60–64 | 229 | (5.2) | 60 | (4.4) | 54 | (8.3) | 16 | (3.4) | 28 | (10.2) | 15 | (5.2) | 23 | (6.8) | 43 | (16.9) | |
| Education | |||||||||||||||||
| ≤Elementary School | 137 | (4.6) | 31 | (4.0) | 32 | (7.6) | 19 | (6.4) | 13 | (7.9) | 17 | (9.0) | 18 | (9.5) | 32 | (14.8) | <0.0001 |
| Middle School Graduate | 158 | (6.5) | 45 | (6.5) | 25 | (5.3) | 13 | (5.7) | 18 | (12.3) | 27 | (15.8) | 10 | (5.9) | 23 | (12.6) | |
| High School Graduate | 793 | (43.0) | 211 | (39.3) | 130 | (45.8) | 81 | (44.6) | 46 | (37.0) | 51 | (44.1) | 79 | (49.7) | 53 | (38.2) | |
| ≥College Graduate | 887 | (46.0) | 285 | (50.1) | 125 | (41.3) | 79 | (43.3) | 50 | (42.8) | 38 | (31.1) | 56 | (35.0) | 42 | (34.4) | |
| Income | |||||||||||||||||
| Highest | 525 | (26.9) | 170 | (28.7) | 66 | (19.5) | 48 | (25.7) | 25 | (20.4) | 21 | (16.8) | 48 | (24.8) | 24 | (14.7) | <0.0001 |
| Upper Middle | 512 | (25.6) | 156 | (26.4) | 73 | (23.0) | 39 | (16.6) | 29 | (24.1) | 28 | (21.1) | 41 | (27.0) | 24 | (19.0) | |
| Lower Middle | 496 | (24.5) | 164 | (30.4) | 83 | (25.8) | 52 | (29.7) | 34 | (25.2) | 37 | (27.5) | 38 | (24.3) | 41 | (30.2) | |
| Lowest | 442 | (23.0) | 82 | (14.5) | 90 | (31.7) | 53 | (27.9) | 39 | (30.3) | 47 | (34.6) | 36 | (23.9) | 61 | (36.1) | |
| Occupation | |||||||||||||||||
| Employed | 1691 | (84.8) | 513 | (88.9) | 213 | (66.7) | 162 | (81.5) | 89 | (66.3) | 90 | (63.7) | 135 | (81.6) | 97 | (65.1) | <0.0001 |
| Unemployed | 284 | (15.2) | 59 | (11.1) | 99 | (33.3) | 30 | (18.5) | 38 | (33.7) | 43 | (36.3) | 28 | (18.4) | 53 | (34.9) | |
| No. of Family Members in a Household | |||||||||||||||||
| 1 | 62 | (3.5) | 20 | (3.3) | 12 | (4.3) | 37 | (20.2) | 4 | (2.6) | 30 | (23.0) | 34 | (20.8) | 57 | (31.8) | <0.0001 |
| 2 | 444 | (18.0) | 103 | (15.4) | 77 | (20.6) | 51 | (26.3) | 30 | (20.8) | 24 | (14.4) | 30 | (15.7) | 24 | (14.3) | |
| 3 | 585 | (30.5) | 177 | (32.9) | 92 | (30.8) | 33 | (17.4) | 38 | (31.0) | 29 | (19.2) | 44 | (27.0) | 33 | (24.7) | |
| 4 | 647 | (35.2) | 189 | (33.9) | 101 | (35.3) | 59 | (30.5) | 39 | (32.9) | 43 | (36.6) | 38 | (26.2) | 25 | (20.7) | |
| 5 | 181 | (9.8) | 65 | (11.6) | 22 | (6.6) | 9 | (4.0) | 12 | (10.2) | 6 | (6.1) | 12 | (7.9) | 8 | (5.8) | |
| ≥6 | 56 | (2.9) | 18 | (2.9) | 8 | (2.4) | 3 | (1.7) | 4 | (2.5) | 1 | (0.7) | 5 | (2.5) | 3 | (2.8) | |
| Household Generation Types | |||||||||||||||||
| Single-Person Household | 62 | (3.5) | 20 | (3.3) | 12 | (4.3) | 37 | (20.2) | 4 | (2.6) | 30 | (23.0) | 34 | (20.8) | 57 | (31.8) | <0.0001 |
| 1 Generation Households | 382 | (15.3) | 89 | (12.9) | 60 | (14.6) | 29 | (12.8) | 22 | (15.8) | 19 | (11.1) | 21 | (9.2) | 19 | (10.8) | |
| 2 Generations Households | 1364 | (72.6) | 413 | (75.4) | 224 | (77.1) | 112 | (60.9) | 90 | (75.3) | 75 | (57.5) | 101 | (65.3) | 63 | (50.0) | |
| ≥3 Generations Households | 167 | (8.5) | 50 | (8.4) | 16 | (3.9) | 14 | (6.1) | 11 | (6.4) | 9 | (8.4) | 7 | (4.7) | 11 | (7.5) | |
| Marital Status | |||||||||||||||||
| Married | 1568 | (74.0) | 461 | (74.5) | 219 | (60.6) | 108 | (45.5) | 98 | (70.1) | 83 | (52.4) | 118 | (64.1) | 104 | (57.7) | <0.0001 |
| Unmarried | 407 | (26.0) | 111 | (25.5) | 93 | (39.4) | 84 | (54.5) | 29 | (29.9) | 50 | (47.6) | 45 | (35.9) | 46 | (42.3) | |
| Smoking | |||||||||||||||||
| Nonsmoker | 530 | (29.0) | 176 | (33.6) | 73 | (26.0) | 51 | (28.1) | 39 | (33.1) | 35 | (28.2) | 51 | (35.9) | 34 | (26.9) | 0.0715 |
| Former Smoker | 613 | (28.3) | 188 | (30.4) | 108 | (29.3) | 47 | (19.3) | 40 | (27.1) | 42 | (27.9) | 52 | (24.0) | 52 | (32.2) | |
| Current Smoker | 832 | (42.7) | 208 | (36.0) | 131 | (44.7) | 94 | (52.6) | 48 | (39.8) | 56 | (43.9) | 60 | (40.0) | 64 | (40.8) | |
| Physical Activity | |||||||||||||||||
| Yes | 847 | (45.9) | 276 | (51.1) | 131 | (45.9) | 91 | (49.5) | 58 | (49.3) | 60 | (48.5) | 73 | (48.2) | 60 | (43.5) | 0.6344 |
| No | 1128 | (54.1) | 296 | (48.9) | 181 | (54.1) | 101 | (50.5) | 69 | (50.7) | 73 | (51.5) | 90 | (51.8) | 90 | (56.5) | |
| Total | 1975 | (100.0) | 572 | (100.0) | 312 | (100.0) | 192 | (100.0) | 127 | (100.0) | 133 | (100.0) | 163 | (100.0) | 150 | (100.0) | |
| Women | 0 Times Eating Alone (n = 2360) | 1 Time for B Only (n = 584) | 1 Time for L Only (n = 1004) | 1 Time for D Only (n = 251) | 2 Times for B & L (n = 406) | 2 Times for L & D (n = 255) | 2 Times for B & D (n = 234) | 3 Times for B, L, & D (n = 270) | p Value 1 | ||||||||
| n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | ||
| Age (years) | |||||||||||||||||
| 19–29 | 371 | (23.0) | 119 | (27.5) | 88 | (13.6) | 46 | (23.9) | 42 | (13.9) | 36 | (19.2) | 36 | (22.5) | 17 | (10.0) | <0.0001 |
| 30–39 | 537 | (22.8) | 118 | (18.7) | 292 | (29.7) | 30 | (14.5) | 81 | (18.7) | 26 | (12.6) | 21 | (9.1) | 17 | (7.9) | |
| 40–49 | 601 | (25.3) | 145 | (24.8) | 283 | (28.2) | 56 | (21.1) | 110 | (30.4) | 51 | (19.1) | 71 | (31.2) | 49 | (21.3) | |
| 50–59 | 573 | (20.9) | 155 | (23.9) | 249 | (21.7) | 94 | (33.4) | 119 | (27.5) | 95 | (34.7) | 83 | (31.7) | 113 | (40.7) | |
| 60–64 | 278 | (8.0) | 47 | (5.2) | 92 | (6.8) | 25 | (7.1) | 54 | (9.5) | 47 | (14.3) | 23 | (5.4) | 74 | (20.0) | |
| Education | |||||||||||||||||
| ≤Elementary School | 305 | (10.1) | 47 | (7.0) | 93 | (6.9) | 36 | (12.3) | 55 | (11.9) | 48 | (15.3) | 35 | (10.1) | 73 | (21.0) | <0.0001 |
| Middle School Graduate | 241 | (9.0) | 55 | (7.8) | 90 | (8.6) | 28 | (11.8) | 43 | (9.6) | 36 | (12.8) | 35 | (12.0) | 47 | (18.5) | |
| High School Graduate | 926 | (40.8) | 247 | (42.8) | 409 | (42.3) | 100 | (38.1) | 158 | (41.1) | 106 | (41.4) | 83 | (38.5) | 81 | (32.6) | |
| ≥College Graduate | 888 | (40.1) | 235 | (42.4) | 412 | (42.2) | 87 | (37.7) | 150 | (37.4) | 65 | (30.5) | 81 | (39.3) | 69 | (28.0) | |
| Income | |||||||||||||||||
| Highest | 597 | (25.7) | 185 | (32.6) | 241 | (22.9) | 64 | (23.2) | 101 | (24.1) | 68 | (28.8) | 64 | (28.8) | 65 | (28.7) | <0.0001 |
| Upper Middle | 611 | (25.5) | 153 | (25.7) | 276 | (26.6) | 65 | (27.6) | 119 | (28.8) | 63 | (22.6) | 51 | (21.9) | 46 | (17.5) | |
| Lower Middle | 569 | (24.1) | 143 | (23.1) | 254 | (25.8) | 84 | (34.2) | 105 | (26.5) | 52 | (19.5) | 61 | (25.5) | 64 | (21.0) | |
| Lowest | 583 | (24.7) | 103 | (18.7) | 233 | (24.6) | 38 | (15.1) | 81 | (20.6) | 72 | (29.1) | 58 | (23.8) | 95 | (32.8) | |
| Occupation | |||||||||||||||||
| Employed | 1530 | (64.9) | 392 | (67.0) | 383 | (39.2) | 181 | (72.1) | 153 | (38.1) | 115 | (43.0) | 174 | (75.7) | 134 | (49.0) | <0.0001 |
| Unemployed | 830 | (35.1) | 192 | (33.0) | 621 | (60.8) | 70 | (27.9) | 253 | (61.9) | 140 | (57.0) | 60 | (24.3) | 136 | (51.0) | |
| No. of Family Members in a Household | |||||||||||||||||
| 1 | 38 | (1.8) | 23 | (3.6) | 14 | (1.6) | 30 | (11.2) | 13 | (2.4) | 28 | (8.6) | 52 | (17.7) | 79 | (22.7) | <0.0001 |
| 2 | 541 | (19.4) | 107 | (16.8) | 197 | (17.0) | 80 | (28.7) | 90 | (20.4) | 86 | (30.3) | 70 | (27.8) | 82 | (28.5) | |
| 3 | 676 | (30.1) | 164 | (29.6) | 314 | (32.2) | 63 | (28.0) | 118 | (29.7) | 81 | (36.2) | 57 | (25.2) | 63 | (26.4) | |
| 4 | 742 | (32.7) | 201 | (34.4) | 374 | (38.8) | 56 | (24.1) | 134 | (33.8) | 45 | (18.9) | 42 | (20.7) | 32 | (16.6) | |
| 5 | 256 | (11.5) | 65 | (11.7) | 86 | (8.8) | 16 | (5.9) | 42 | (11.3) | 14 | (5.5) | 10 | (7.0) | 9 | (4.6) | |
| ≥6 | 107 | (4.6) | 24 | (3.7) | 19 | (1.7) | 6 | (2.2) | 9 | (2.5) | 1 | (0.6) | 3 | (1.6) | 5 | (1.3) | |
| Household Generation Types | |||||||||||||||||
| Single-Person Household | 38 | (1.8) | 23 | (3.6) | 14 | (1.6) | 30 | (11.2) | 13 | (2.4) | 28 | (8.6) | 52 | (17.7) | 79 | (22.7) | <0.0001 |
| 1 Generation Households | 464 | (16.2) | 71 | (11.5) | 153 | (12.6) | 54 | (20.5) | 68 | (15.1) | 62 | (21.0) | 37 | (13.7) | 45 | (15.0) | |
| 2 Generations Households | 1584 | (70.4) | 434 | (76.3) | 759 | (78.2) | 148 | (60.8) | 292 | (74.4) | 151 | (64.6) | 136 | (64.6) | 132 | (56.4) | |
| ≥3 Generations Households | 274 | (11.5) | 56 | (8.6) | 78 | (7.6) | 19 | (7.6) | 33 | (8.1) | 14 | (5.8) | 9 | (4.0) | 14 | (5.9) | |
| Marital Status | |||||||||||||||||
| Married | 1962 | (76.9) | 437 | (67.7) | 922 | (88.5) | 187 | (67.8) | 359 | (85.4) | 219 | (81.6) | 178 | (70.4) | 237 | (84.5) | <0.0001 |
| Unmarried | 398 | (23.1) | 147 | (32.3) | 82 | (11.5) | 64 | (32.2) | 47 | (14.6) | 36 | (18.4) | 56 | (29.6) | 33 | (15.5) | |
| Smoking | |||||||||||||||||
| Nonsmoker | 2148 | (90.0) | 539 | (92.1) | 905 | (89.0) | 228 | (89.8) | 387 | (95.7) | 235 | (91.3) | 210 | (91.1) | 242 | (91.2) | 0.0269 |
| Former Smoker | 94 | (4.3) | 18 | (3.1) | 50 | (5.7) | 7 | (3.8) | 11 | (3.0) | 10 | (4.2) | 15 | (6.4) | 9 | (2.6) | |
| Current Smoker | 118 | (5.7) | 27 | (4.8) | 49 | (5.3) | 16 | (6.4) | 8 | (1.3) | 10 | (4.5) | 9 | (2.5) | 19 | (6.2) | |
| Physical Activity | |||||||||||||||||
| Yes | 885 | (39.9) | 233 | (43.2) | 407 | (42.1) | 92 | (39.9) | 164 | (42.3) | 102 | (41.3) | 106 | (48.3) | 106 | (44.2) | 0.4743 |
| No | 1475 | (60.1) | 351 | (56.8) | 597 | (57.9) | 159 | (60.1) | 242 | (57.7) | 153 | (58.7) | 128 | (51.7) | 164 | (55.8) | |
| Total | 2360 | (100.0) | 584 | (100.0) | 1004 | (100.0) | 251 | (100.0) | 406 | (100.0) | 255 | (100.0) | 234 | (100.0) | 270 | (100.0) | |
| Men | 0 Times Eating Alone (n = 1975) | 1 Time for B Only (n = 572) | 1 Time for L Only (n = 312) | 1 Time for D Only (n = 192) | 2 Times for B & L (n = 127) | 2 Times for L & D (n = 133) | 2 Times for B & D (n = 163) | 3 Times for B, L, & D (n = 150) | ||||||||
| Mean | (SE) | Mean | (SE) | Mean | (SE) | Mean | (SE) | Mean | (SE) | Mean | (SE) | Mean | (SE) | Mean | (SE) | |
| BMI (kg/m2) | 24.4 | (0.1) | 24.6 | (0.2) | 24.6 | (0.2) | 24.5 | (0.3) | 24.2 | (0.4) | 25.4 | (0.5) | 24.8 | (0.3) | 24.4 | (0.3) |
| WC (cm) | 84.5 | (0.2) | 85.0 | (0.4) | 85.0 | (0.6) | 84.4 | (0.8) | 83.6 | (1.0) | 87.7 | (1.1) | 86.3 | (0.8) | 85.4 | (0.9) |
| SBP (mmHg) | 117.4 | (0.3) | 117.4 | (0.6) | 117.3 | (0.9) | 117.7 | (0.8) | 119.4 | (1.6) | 118.8 | (1.2) | 120.3 | (1.5) | 120.0 | (1.3) |
| DBP (mmHg) | 78.5 | (0.3) | 78.5 | (0.4) | 78.3 | (0.6) | 78.6 | (0.7) | 78.5 | (1.1) | 79.8 | (1.1) | 79.6 | (1.0) | 78.5 | (1.1) |
| FBG (mg/dL) | 99.5 | (0.5) | 99.6 | (0.9) | 97.7 | (1.1) | 101.3 | (2.3) | 97.2 | (1.7) | 101.0 | (2.2) | 103.5 | (2.3) | 103.7 | (2.5) |
| Total Cholesterol (mg/dL) | 190.2 | (0.9) | 190.7 | (1.7) | 188.5 | (2.2) | 185.1 | (2.6) | 186.7 | (4.0) | 190.8 | (3.3) | 186.5 | (3.0) | 182.0 | (3.3) |
| HDL-C (mg/dL) | 47.4 | (0.3) | 48.3 | (0.5) | 47.7 | (0.7) | 46.9 | (0.8) | 48.6 | (1.0) | 46.0 | (1.0) | 46.6 | (0.9) | 47.3 | (1.0) |
| TG (mg/dL) | 168.8 | (3.7) | 163.9 | (5.6) | 152.1 | (8.8) | 166.7 | (13.1) | 149.1 | (10.2) | 188.3 | (15.8) | 175.1 | (13.0) | 154.0 | (8.7) |
| Energy Intake (kcal/d) | 2467 b | (21) | 2663 a | (43) | 2366 b | (57) | 2262 b | (64) | 2420 a,b | (92) | 2308 b,c | (92) | 2451 a,b | (75) | 2422 a,b | (103) |
| Women | 0 Times Eating Alone (n = 2360) | 1 Time for B Only (n = 584) | 1 Time for L Only (n = 1004) | 1 Time for D Only (n = 251) | 2 Times for B & L (n = 406) | 2 Times for L & D (n = 255) | 2 Times for B & D (n = 234) | 3 Times for B, L, & D (n = 270) | ||||||||
| Mean | (SE) | Mean | (SE) | Mean | (SE) | Mean | (SE) | Mean | (SE) | Mean | (SE) | Mean | (SE) | Mean | (SE) | |
| BMI (kg/m2) | 23.0 a,b | (0.1) | 22.6 b | (0.2) | 23.0 a,b | (0.1) | 23.3 a,b | (0.3) | 22.8 a,b | (0.2) | 23.3 a,b | (0.3) | 22.6 a,b | (0.2) | 23.6 a | (0.3) |
| WC (cm) | 76.5 b | (0.2) | 74.9 c | (0.4) | 76.8 a,b | (0.4) | 76.9 a,b | (0.7) | 76.8 a,b | (0.5) | 77.0 a,b | (0.8) | 75.5 b,c | (0.6) | 78.8 a | (0.7) |
| SBP (mmHg) | 111.1 b | (0.4) | 109.5 b | (0.7) | 110.7 b | (0.5) | 110.7 b | (1.0) | 111.1 b | (0.8) | 112.6 a,b | (1.1) | 111.1 b,c | (1.0) | 116.5 a | (1.2) |
| DBP (mmHg) | 72.5 b | (0.3) | 72.2 b | (0.5) | 72.9 a,b | (0.3) | 72.3 a,b | (0.7) | 73.0 a,b | (0.5) | 73.1 a,b | (0.7) | 73.5 a,b | (0.7) | 75.1 a | (0.7) |
| FBG (mg/dL) | 95.2 | (0.4) | 94.1 | (0.7) | 95.3 | (0.9) | 94.8 | (1.1) | 95.7 | (1.0) | 95.1 | (1.6) | 92.9 | (1.0) | 98.4 | (1.5) |
| Total Cholesterol (mg/dL) | 185.8 b,c | (0.8) | 183.0 c | (1.4) | 189.0 a,b | (1.2) | 191.6 a,b | (2.5) | 189.8 a,b | (1.9) | 191.6 a,b | (2.3) | 188.7 a,b | (2.6) | 194.9 a | (2.5) |
| HDL-C (mg/dL) | 55.3 a,b | (0.3) | 56.6 a | (0.6) | 55.2 a,b | (0.4) | 55.2 a,b | (0.8) | 55.5 a,b | (0.7) | 55.4 a,b | (0.8) | 55.2 a,b | (0.8) | 53.3 b,c | (0.8) |
| TG (mg/dL) | 101.9 b,c | (1.6) | 94.0 c | (2.8) | 109.9 a,b | (2.7) | 105.9 a,c | (5.3) | 110.2 a,c | (4.7) | 110.1 a,b | (5.1) | 102.3 b,c | (4.3) | 129.8 a | (6.5) |
| Energy Intake (kcal/d) | 1793 | (15) | 1853 | (33) | 1781 | (22) | 1800 | (44) | 1821 | (43) | 1774 | (47) | 1859 | (59) | 1798 | (49) |
| Patterns of Eating Alone | Men | Women | ||
|---|---|---|---|---|
| AOR 1 | (95% CI) | AOR 1 | (95% CI) | |
| Metabolic Syndrome | ||||
| 0 times eating alone | 1.00 | (Reference) | 1.00 | (Reference) |
| 1 time for B only | 1.04 | (0.82–1.33) | 0.70 | (0.53–0.94) |
| 1 time for L only | 1.06 | (0.75–1.49) | 0.93 | (0.75–1.14) |
| 1 time for D only | 1.51 | (1.06–2.16) | 0.84 | (0.57–1.24) |
| 2 times for B & L | 0.75 | (0.46–1.20) | 0.94 | (0.69–1.27) |
| 2 times for L & D | 1.26 | (0.68–2.33) | 0.70 | (0.47–1.06) |
| 2 times for B & D | 1.54 | (1.05–2.25) | 0.77 | (0.49–1.23) |
| 3 times for B, L, & D | 1.30 | (0.83–2.03) | 1.02 | (0.70–1.47) |
| Abdominal Obesity | ||||
| 0 times eating alone | 1.00 | (Reference) | 1.00 | (Reference) |
| 1 time for B only | 1.13 | (0.90–1.43) | 0.85 | (0.67–1.07) |
| 1 time for L only | 1.19 | (0.88–1.59) | 0.97 | (0.80–1.17) |
| 1 time for D only | 1.16 | (0.81–1.66) | 1.20 | (0.88–1.65) |
| 2 times for B & L | 0.78 | (0.48–1.26) | 0.98 | (0.74–1.30) |
| 2 times for L & D | 2.01 | (1.27–3.20) | 0.74 | (0.52–1.03) |
| 2 times for B & D | 1.50 | (1.00–2.25) | 0.79 | (0.54–1.15) |
| 3 times for B, L, & D | 1.60 | (1.01–2.51) | 1.12 | (0.81–1.55) |
| Low HDL-C | ||||
| 0 times eating alone | 1.00 | (Reference) | 1.00 | (Reference) |
| 1 time for B only | 0.98 | (0.76–1.27) | 0.86 | (0.69–1.06) |
| 1 time for L only | 0.78 | (0.57–1.08) | 0.98 | (0.81–1.18) |
| 1 time for D only | 1.23 | (0.86–1.75) | 1.07 | (0.77–1.48) |
| 2 times for B & L | 0.66 | (0.40–1.08) | 0.87 | (0.67–1.12) |
| 2 times for L & D | 1.35 | (0.84–2.16) | 0.71 | (0.52–0.96) |
| 2 times for B & D | 0.86 | (0.57–1.30) | 1.07 | (0.75–1.53) |
| 3 times for B, L, & D | 0.73 | (0.45–1.18) | 0.95 | (0.68–1.31) |
| Elevated TG | ||||
| 0 times eating alone | 1.00 | (Reference) | 1.00 | (Reference) |
| 1 time for B only | 1.09 | (0.88–1.34) | 0.85 | (0.66–1.10) |
| 1 time for L only | 0.86 | (0.64–1.16) | 1.24 | (1.00–1.53) |
| 1 time for D only | 1.19 | (0.84–1.70) | 0.88 | (0.62–1.25) |
| 2 times for B & L | 0.90 | (0.59–1.35) | 1.05 | (0.78–1.42) |
| 2 times for L & D | 1.17 | (0.78–1.77) | 1.02 | (0.71–1.46) |
| 2 times for B & D | 1.27 | (0.87–1.86) | 1.03 | (0.69–1.54) |
| 3 times for B, L, & D | 1.27 | (0.81–1.98) | 1.25 | (0.89–1.77) |
| Elevated FBG | ||||
| 0 times eating alone | 1.00 | (Reference) | 1.00 | (Reference) |
| 1 time for B only | 1.08 | (0.86–1.34) | 0.85 | (0.65–1.11) |
| 1 time for L only | 0.95 | (0.68–1.32) | 0.85 | (0.69–1.05) |
| 1 time for D only | 1.19 | (0.83–1.71) | 1.01 | (0.70–1.47) |
| 2 times for B & L | 0.78 | (0.49–1.24) | 0.93 | (0.70–1.24) |
| 2 times for L & D | 1.00 | (0.63–1.56) | 0.79 | (0.54–1.15) |
| 2 times for B & D | 1.24 | (0.85–1.81) | 0.59 | (0.38–0.92) |
| 3 times for B, L, & D | 1.19 | (0.79–1.78) | 0.73 | (0.51–1.05) |
| Elevated BP | ||||
| 0 times eating alone | 1.00 | (Reference) | 1.00 | (Reference) |
| 1 time for B only | 1.01 | (0.80–1.28) | 0.84 | (0.64–1.09) |
| 1 time for L only | 1.22 | (0.90–1.64) | 0.82 | (0.65–1.05) |
| 1 time for D only | 1.30 | (0.92–1.83) | 0.97 | (0.68–1.40) |
| 2 times for B & L | 1.08 | (0.73–1.61) | 0.91 | (0.65–1.26) |
| 2 times for L & D | 1.46 | (0.90–2.36) | 0.96 | (0.65–1.41) |
| 2 times for B & D | 1.54 | (1.03–2.30) | 1.11 | (0.72–1.70) |
| 3 times for B, L, & D | 1.13 | (0.74–1.71) | 0.84 | (0.59–1.20) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, C.-K.; Kim, H.-j.; Chung, H.-K.; Shin, D. Eating Alone is Differentially Associated with the Risk of Metabolic Syndrome in Korean Men and Women. Int. J. Environ. Res. Public Health 2018, 15, 1020. https://doi.org/10.3390/ijerph15051020
Kim C-K, Kim H-j, Chung H-K, Shin D. Eating Alone is Differentially Associated with the Risk of Metabolic Syndrome in Korean Men and Women. International Journal of Environmental Research and Public Health. 2018; 15(5):1020. https://doi.org/10.3390/ijerph15051020
Chicago/Turabian StyleKim, Chul-Kyoo, Hyun-jin Kim, Hae-Kyung Chung, and Dayeon Shin. 2018. "Eating Alone is Differentially Associated with the Risk of Metabolic Syndrome in Korean Men and Women" International Journal of Environmental Research and Public Health 15, no. 5: 1020. https://doi.org/10.3390/ijerph15051020
APA StyleKim, C.-K., Kim, H.-j., Chung, H.-K., & Shin, D. (2018). Eating Alone is Differentially Associated with the Risk of Metabolic Syndrome in Korean Men and Women. International Journal of Environmental Research and Public Health, 15(5), 1020. https://doi.org/10.3390/ijerph15051020





