Oral Health-Related Quality of Life in Young Adults: A Survey of Russian Undergraduate Students
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Setting and Population
2.2. Sampling
2.3. Questionnaires
Oral Health-Related Quality of Life as Measured by the Oral Health Impact Profile-14: Validity and Reliability
2.4. Clinical Dental Examination
2.5. Statistical Analysis
2.6. Ethical Considerations
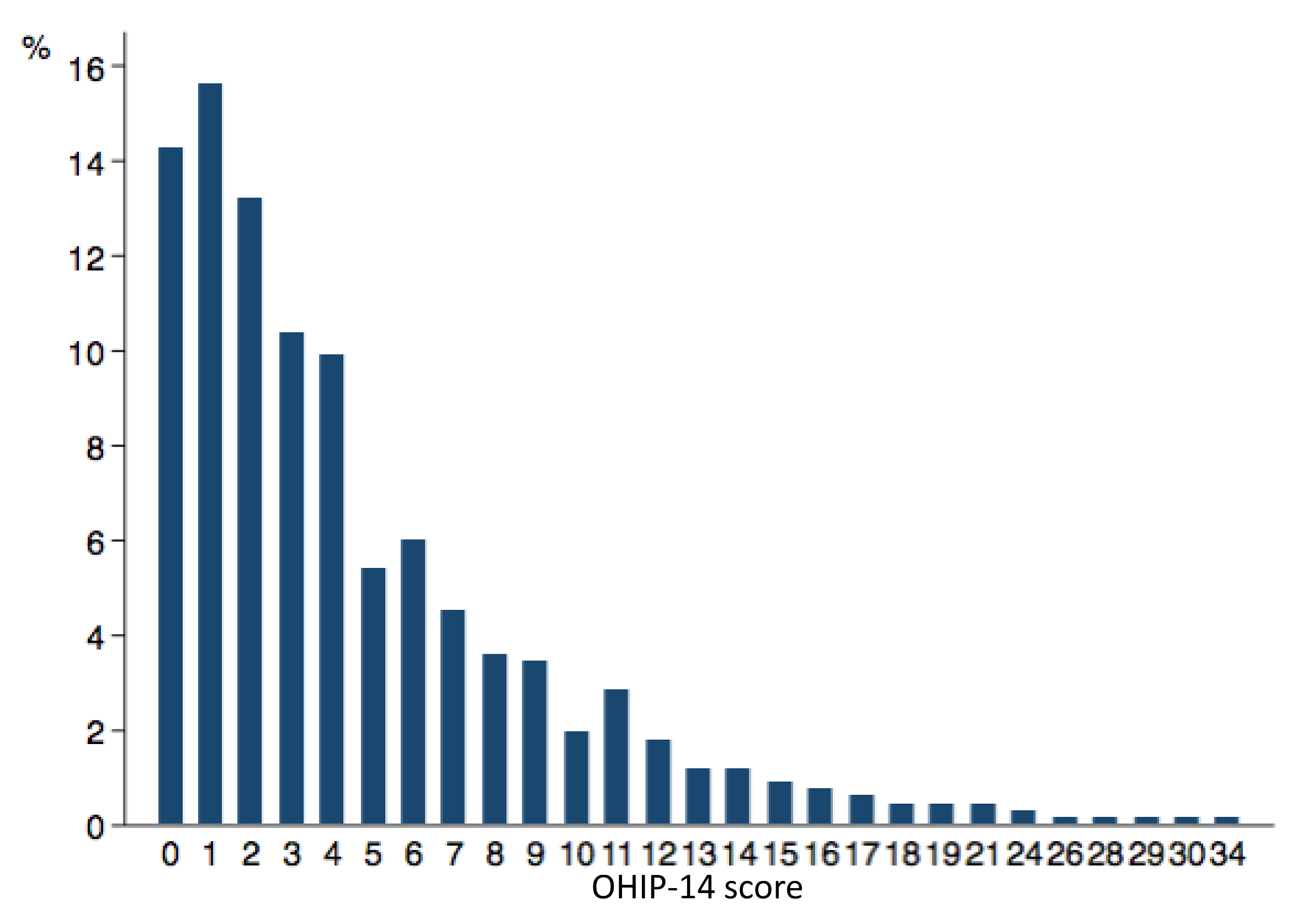
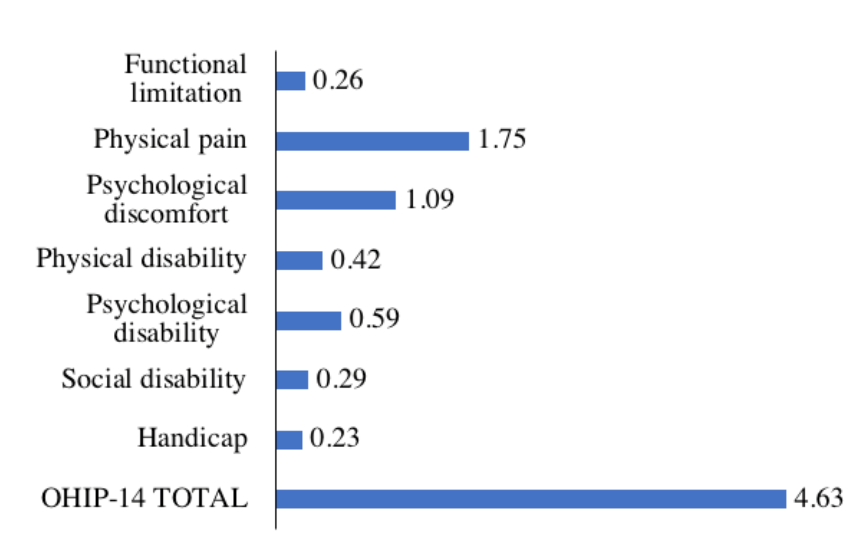
3. Results
4. Discussion
4.1. Main Findings
4.2. Data Interpretation and Comparisons with Previous Studies
4.3. Strengths of the Study
4.4. Limitations of the Study
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Sischo, L.; Broder, H.L. Oral health-related quality of life: What, why, how, and future implications. J. Dent. Res. 2011, 90, 1264–1270. [Google Scholar] [CrossRef] [PubMed]
- Allen, P.F. Assessment of oral health related quality of life. Health Qual. Life Outcomes 2003, 1, 40. [Google Scholar] [CrossRef] [PubMed]
- Locker, D.; Allen, F. What do measures of ‘oral health-related quality of life’ measure? Community Dent. Oral Epidemiol. 2007, 35, 401–411. [Google Scholar] [CrossRef] [PubMed]
- Slade, G.D. Derivation and validation of a short-form oral health impact profile. Community Dent. Oral Epidemiol. 1997, 25, 284–290. [Google Scholar] [CrossRef] [PubMed]
- Locker, D. Measuring oral health: A conceptual framework. Community Dent. Health 1988, 5, 3–18. [Google Scholar] [PubMed]
- Barer, G.M.; Gurevich, K.G.; Smirniagina, V.V.; Fabrikant, E.G. Validation of oral health impact profile (OHIP) quality of life questionnaire in Russian patients with evidence of chronic generalized periodontitis. Stomatologiia (Mosk.) 2007, 86, 27–30. (In Russian) [Google Scholar] [PubMed]
- Dahl, K.E.; Wang, N.J.; Skau, I.; Ohrn, K. Oral health-related quality of life and associated factors in Norwegian adults. Acta Odontol. Scand. 2011, 69, 208–214. [Google Scholar] [CrossRef] [PubMed]
- Sanders, A.E.; Slade, G.D.; Lim, S.; Reisine, S.T. Impact of oral disease on quality of life in the US and Australian populations. Community Dent. Oral Epidemiol. 2009, 37, 171–181. [Google Scholar] [CrossRef] [PubMed]
- Slade, G.D.; Sanders, A.E. The paradox of better subjective oral health in older age. J. Dent. Res. 2011, 90, 1279–1285. [Google Scholar] [CrossRef] [PubMed]
- Yamane-Takeuchi, M.; Ekuni, D.; Mizutani, S.; Kataoka, K.; Taniguchi-Tabata, A.; Azuma, T.; Furuta, M.; Tomofuji, T.; Iwasaki, Y.; Morita, M. Associations among oral health-related quality of life, subjective symptoms, clinical status, and self-rated oral health in Japanese university students: A cross-sectional study. BMC Oral Health 2016, 16, 127. [Google Scholar] [CrossRef] [PubMed]
- Oscarson, N.; Kallestal, C.; Lindholm, L. A pilot study of the use of oral health-related quality of life measures as an outcome for analysing the impact of caries disease among Swedish 19-year-olds. Caries Res. 2007, 41, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Masalu, J.R.; Astrom, A.N. Social and behavioral correlates of oral quality of life studied among university students in Tanzania. Acta Odontol. Scand. 2002, 60, 353–359. [Google Scholar] [CrossRef] [PubMed]
- Masood, Y.; Masood, M.; Zainul, N.N.; Araby, N.B.; Hussain, S.F.; Newton, T. Impact of malocclusion on oral health related quality of life in young people. Health Qual. Life Outcomes 2013, 11, 25. [Google Scholar] [CrossRef] [PubMed]
- Brennan, D.S.; Spencer, A.J. Life events and oral-health-related quality of life among young adults. Qual. Life Res. 2009, 18, 557–565. [Google Scholar] [CrossRef] [PubMed]
- Lu, H.-X.; Wong, M.; Lo, E.; McGrath, C. Oral health related quality of life among young adults. Appl. Res. Qual. Life 2015, 10, 37–47. [Google Scholar] [CrossRef]
- Choi, S.H.; Kim, B.I.; Cha, J.Y.; Hwang, C.J. Impact of malocclusion and common oral diseases on oral health-related quality of life in young adults. Am. J. Orthod. Dentofacial. Orthop. 2015, 147, 587–595. [Google Scholar] [CrossRef] [PubMed]
- Gonzales-Sullcahuaman, J.A.; Ferreira, F.M.; de Menezes, J.V.; Paiva, S.M.; Fraiz, F.C. Oral health-related quality of life among Brazilian dental students. Acta Odontol. Latinoam. 2013, 26, 76–83. [Google Scholar] [PubMed]
- Acharya, S.; Sangam, D.K. Oral health-related quality of life and its relationship with health locus of control among Indian dental university students. Eur. J. Dent. Educ. 2008, 12, 208–212. [Google Scholar] [CrossRef] [PubMed]
- Priya, H.; Sequeira, P.S.; Acharya, S.; Kumar, M. Oral health related quality of life among dental students in a private dental institution in India. J. Int. Soc. Prev. Community Dent. 2011, 1, 65–70. [Google Scholar] [CrossRef] [PubMed]
- Abaev, Z.M.; Berkutova, I.S.; Domashev, D.I.; Rekhviashvili, B.A.; Zorina, O.A. The quality of life of patients with various forms of periodontitis. Problemy Sotsial’Noi Gigieny Zdravookhraneniia I Istorii Meditsiny 2012, 4, 33–35. (In Russian) [Google Scholar]
- Makeeva, I.M.; Doroshina, V.; Protsenko, A.S. Prevalence of dental diseases among Moscow students and need of dentistry. Stomatologiia (Mosk.) 2009, 88, 4–8. (In Russian) [Google Scholar] [PubMed]
- Drachev, S.N.; Brenn, T.; Trovik, T.A. Dental caries experience and determinants in young adults of the Northern State Medical University, Arkhangelsk, North-West Russia: A cross-sectional study. BMC Oral Health 2017, 17, 136. [Google Scholar] [CrossRef] [PubMed]
- The MacArthur Scale of Subjective Social Status. Available online: http://www.macses.ucsf.edu/research/psychosocial/subjective.php (accessed on 10 November 2017).
- Streiner, D.L.; Norman, G.R. Health Measurement Scales: A Practical Guide to Their Development and Use, 4th ed.; Oxford University Press: Oxford, UK, 2008; ISBN 978-01-9923-188-1. [Google Scholar]
- World Health Organization. Oral Health Surveys: Basic Methods, 5th ed.; World Health Organization: Geneva, Switzerland, 2013; ISBN 978-92-4-154864-9. [Google Scholar]
- Greene, J.C.; Vermillion, J.R. The Simplified Oral Hygiene Index. J. Am. Dent. Assoc. 1964, 68, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Loe, H.; Silness, J. Periodontal disease in pregnancy. I. Prevalence and severity. Acta Odontol. Scand. 1963, 21, 533–551. [Google Scholar] [CrossRef] [PubMed]
- Carr, A.J.; Gibson, B.; Robinson, P.G. Is quality of life determined by expectations or experience? BMJ 2001, 322, 1240–1243. [Google Scholar] [CrossRef] [PubMed]
- Locker, D.; Gibson, B. Discrepancies between self-ratings of and satisfaction with oral health in two older adult populations. Community Dent. Oral. Epidemiol. 2005, 33, 280–288. [Google Scholar] [CrossRef] [PubMed]
- Gaber, A.; Galarneau, C.; Feine, J.S.; Emami, E. Rural-urban disparity in oral health-related quality of life. Community Dent. Oral Epidemiol. 2017. [Google Scholar] [CrossRef] [PubMed]
- Rosstat. Population and Area of Russia by Regions. Available online: http://www.statdata.ru/ (accessed on 10 November 2017). (In Russian)
- Widstrom, E.; Koposova, N.; Nordengen, R.; Bergdahl, M.; Eriksen, H.; Fabrikant, E. Oral health care and dental treatment needs in the Barents region. Int. J. Circumpolar Health 2010, 69, 486–499. [Google Scholar] [CrossRef] [PubMed]
- Ushmanova, T.N.; Obraztsov, U.L. Oral Health of Population in North-West of Russia; Northern State Medical University: Arkhangelsk, Russia, 2001; ISBN 5-86279-022-5. (In Russian) [Google Scholar]
- Racine, M.; Tousignant-Laflamme, Y.; Kloda, L.A.; Dion, D.; Dupuis, G.; Choiniere, M. A systematic literature review of 10 years of research on sex/gender and pain perception—Part 2: Do biopsychosocial factors alter pain sensitivity differently in women and men? Pain 2012, 153, 619–635. [Google Scholar] [CrossRef] [PubMed]
| Dimension | Item | n (%) | ||||
|---|---|---|---|---|---|---|
| Never (OHIP-14 = 0) | Hardly Ever (OHIP-14 = 1) | Occasionally (OHIP-14 = 2) | Fairly Often (OHIP-14 = 3) | Very Often (OHIP-14 = 4) | ||
| Functional limitations | Trouble pronouncing words | 562 (84.4) | 77 (11.6) | 21 (3.2) | 5 (0.8) | 1 (0.2) |
| Worsened sense of taste | 637 (95.6) | 23 (3.5) | 4 (0.6) | 2 (0.3) | 0 (0.0) | |
| Physical pain | Painful aching in mouth | 164 (24.6) | 256 (38.4) | 225 (33.8) | 17 (2.6) | 4 (0.6) |
| Uncomfortable to eat food | 410 (61.6) | 139 (20.9) | 98 (14.7) | 17 (2.6) | 2 (0.3) | |
| Psychological discomfort | Being self-conscious | 465 (69.8) | 95 (14.3) | 83 (12.5) | 16 (2.4) | 7 (1.1) |
| Feeling tense | 414 (62.2) | 144 (21.6) | 84 (12.6) | 17 (2.6) | 7 (1.1) | |
| Physical disability | Unsatisfactory diet | 597 (89.6) | 54 (8.1) | 11 (1.7) | 3 (0.5) | 1 (0.2) |
| Interrupting meals | 522 (78.4) | 103 (15.5) | 36 (5.4) | 4 (0.6) | 1 (0.2) | |
| Psychological disability | Difficulty relaxing | 559 (83.9) | 77 (11.6) | 25 (3.8) | 3 (0.5) | 2 (0.3) |
| Embarrassed | 509 (76.4) | 85 (12.8) | 58 (8.7) | 10 (1.5) | 4 (0.6) | |
| Social disability | Irritable with other people | 593 (89.0) | 51 (7.7) | 20 (3.0) | 1 (0.2) | 1 (0.2) |
| Difficulty doing usual jobs | 593 (89.0) | 51 (7.7) | 20 (3.0) | 2 (0.3) | 0 (0.0) | |
| Handicap | Life less satisfying | 594 (89.2) | 49 (7.4) | 22(3.3) | 1 (0.2) | 0 (0.0) |
| Unable to function | 624 (93.4) | 31 (4.7) | 10 (1.5) | 1 (0.2) | 0 (0.0) | |
| Variable | n (%) | Low OHRQoL 1, n (%) | p 2 |
|---|---|---|---|
| Age group (years) | 0.027 | ||
| 18–20 | 390 (58.6) | 195 (50.0) | |
| 21–25 | 276 (41.4) | 162 (58.7) | |
| Sex | 0.004 | ||
| Male | 164 (24.6) | 72 (43.9) | |
| Female | 502 (75.4) | 285 (56.8) | |
| Faculty | <0.001 | ||
| Medical | 391 (58.7) | 232 (59.3) | |
| Dental | 275 (41.3) | 125 (45.5) | |
| Place of childhood residence | 0.011 | ||
| Urban | 479 (71.9) | 242 (50.5) | |
| Rural | 187 (28.1) | 115 (61.5) | |
| Subjective SES | 0.323 | ||
| Low (less than 6.0) | 222 (33.3) | 125 (56.3) | |
| High (6.0 and more) | 444 (66.7) | 232 (52.3) | |
| Mother’s education | 0.445 | ||
| <University | 308 (46.2) | 170 (55.2) | |
| University | 358 (53.8) | 187 (52.2) | |
| Self-assessed oral health | <0.001 | ||
| Good | 425 (63.8) | 187 (44.0) | |
| Poor | 241 (36.2) | 170 (70.5) | |
| Self-assessed dental aesthetic | <0.001 | ||
| Good | 415 (62.3) | 180 (43.4) | |
| Poor | 251 (37.7) | 177 (70.5) | |
| Satisfaction with mouth and teeth | <0.001 | ||
| Yes | 296 (44.4) | 109 (36.8) | |
| No | 279 (41.9) | 196 (70.3) | |
| Difficult to answer | 91 (13.7) | 52 (57.1) |
| Variable | n (%) | Low OHRQoL 1, n (%) | p 2 |
|---|---|---|---|
| Regularity of dental visits | 0.462 | ||
| Irregular | 153 (23.0) | 86 (56.2) | |
| Regular | 513 (77.0) | 271 (52.8) | |
| Toothpaste | 0.457 | ||
| Without fluoride/difficult to answer | 353 (53.0) | 194 (55.0) | |
| With fluoride | 313 (47.0) | 163 (52.1) | |
| Tooth-brushing | 0.527 | ||
| Infrequent | 132 (19.8) | 74 (56.1) | |
| Frequent | 534 (80.2) | 283 (53.0) | |
| Skipping tooth-brushing | 0.021 | ||
| Yes | 222 (33.3) | 133 (59.9) | |
| No | 444 (66.7) | 224 (50.5) |
| Variable | Without Low OHRQoL 1 | With Low OHRQoL 1 | p 2 |
|---|---|---|---|
| Mean (SD) | Mean (SD) | ||
| DT | 0.49 (1.02) | 0.69 (1.25) | 0.020 |
| MT | 0.07 (0.29) | 0.15 (0.47) | 0.017 |
| FT | 6.08 (3.98) | 7.34 (4.18) | <0.001 |
| DMFT | 6.63 (4.14) | 8.18 (4.55) | <0.001 |
| OHI-S | 1.04 (0.51) | 1.14 (0.49) | 0.012 |
| GI | 0.26 (0.24) | 0.28 (0.24) | 0.082 |
| Variables | Adjusted OR (95% CI) | p 1 |
|---|---|---|
| Age group (years) | 0.187 | |
| 18–20 | Reference | |
| 21–25 | 1.26 (0.89–1.77) | |
| Sex | 0.050 | |
| Male | Reference | |
| Female | 1.48 (1.00–2.19) | |
| Faculty | 0.164 | |
| Medical | Reference | |
| Dental | 0.78 (0.55–1.11) | |
| Place of childhood residence | 0.023 | |
| Urban | Reference | |
| Rural | 1.56 (1.06–2.28) | |
| Self-assessed dental aesthetic | 0.008 | |
| Good | Reference | |
| Poor | 1.75 (1.16–2.64) | |
| Satisfaction with mouth and teeth | ||
| Yes | Reference | |
| No | 2.51 (1.68–3.77) | <0.001 |
| Difficult to answer | 1.74 (1.04–2.90) | 0.034 |
| Self-assessed oral health | 0.184 | |
| Good | Reference | |
| Poor | 1.34 (0.87–2.05) | |
| DMFT | 1.05 (1.01–1.09) | 0.019 |
| OHI-S | 1.41 (1.00–2.00) | 0.052 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Drachev, S.N.; Brenn, T.; Trovik, T.A. Oral Health-Related Quality of Life in Young Adults: A Survey of Russian Undergraduate Students. Int. J. Environ. Res. Public Health 2018, 15, 719. https://doi.org/10.3390/ijerph15040719
Drachev SN, Brenn T, Trovik TA. Oral Health-Related Quality of Life in Young Adults: A Survey of Russian Undergraduate Students. International Journal of Environmental Research and Public Health. 2018; 15(4):719. https://doi.org/10.3390/ijerph15040719
Chicago/Turabian StyleDrachev, Sergei N., Tormod Brenn, and Tordis A. Trovik. 2018. "Oral Health-Related Quality of Life in Young Adults: A Survey of Russian Undergraduate Students" International Journal of Environmental Research and Public Health 15, no. 4: 719. https://doi.org/10.3390/ijerph15040719
APA StyleDrachev, S. N., Brenn, T., & Trovik, T. A. (2018). Oral Health-Related Quality of Life in Young Adults: A Survey of Russian Undergraduate Students. International Journal of Environmental Research and Public Health, 15(4), 719. https://doi.org/10.3390/ijerph15040719





