The Association between Maternal Stress and Childhood Eczema: A Systematic Review
Abstract
1. Introduction
2. Methods
2.1. Search Strategy
2.2. Eligibility Criteria
2.3. Data Extraction and Synthesis
2.4. Quality Assessment of Included Studies
3. Results
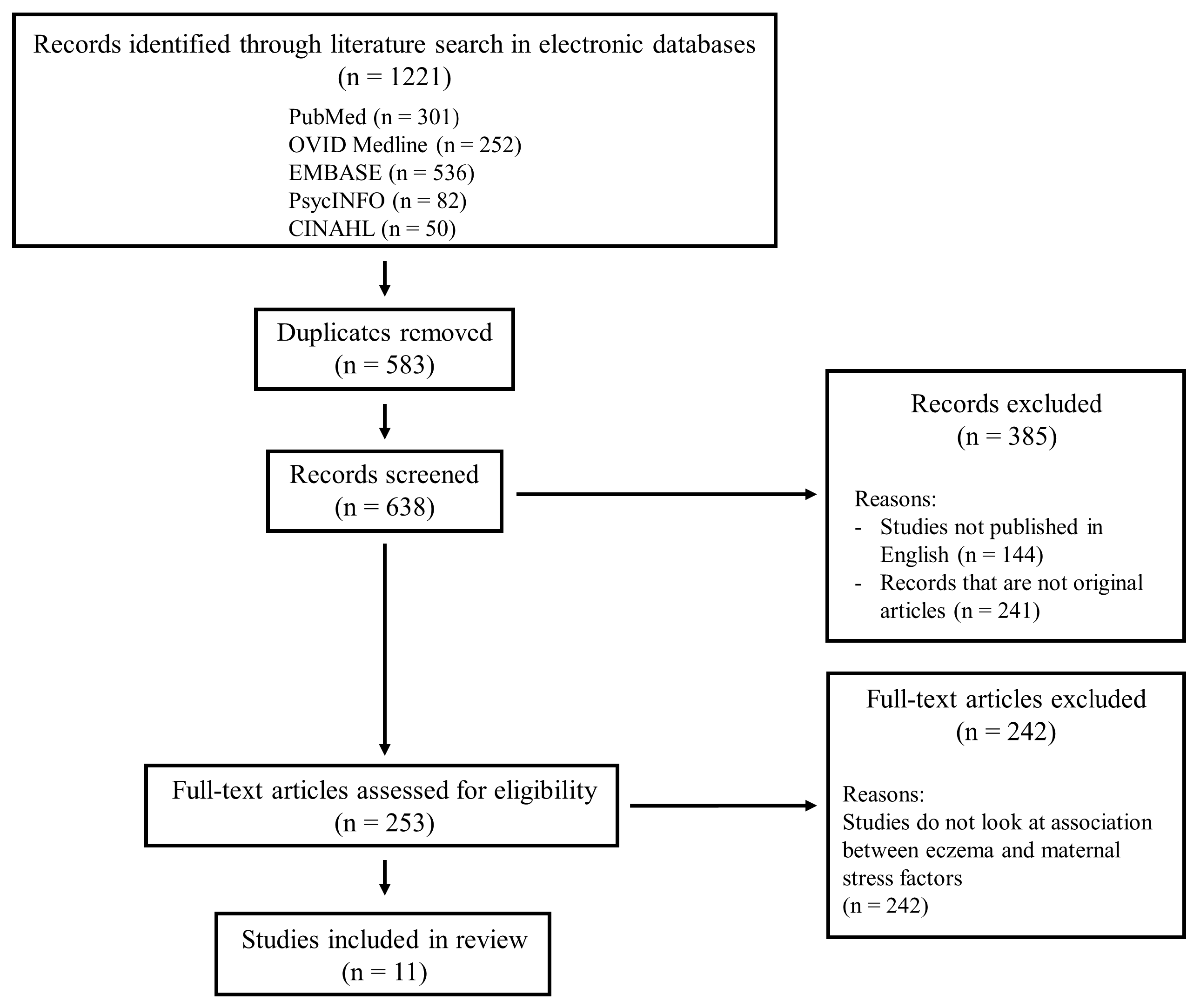
3.1. Search Results
3.2. Quality of the Included Studies
3.3. Characteristics of the Included Studies
3.4. Reported Association between Eczema and Maternal Stress
3.4.1. Depression
3.4.2. Anxiety
3.4.3. Maternal Stress
3.4.4. Adverse Life Events
3.4.5. Others Examined Stress Factors
4. Discussion
4.1. Interpretation of the Review Findings
4.2. Implications of the Review Findings
5. Limitations
6. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Plötz, S.G.; Wiesender, M.; Todorova, A.; Ring, J. What is new in atopic dermatitis/eczema? Expert Opin. Emerg. Drugs 2014, 19, 441–458. [Google Scholar] [CrossRef] [PubMed]
- Herd, R.M.; Tidman, M.J.; Prescott, R.J.; Hunter, J.A. Prevalence of atopic eczema in the community: The Lothian Atopic Dermatitis study. Br. J. Dermatol. 1996, 135, 18–19. [Google Scholar] [CrossRef] [PubMed]
- Thomsen, S.F. Atopic Dermatitis: Natural history, diagnosis, and treatment. ISRN Allergy 2014, 2014. [Google Scholar] [CrossRef] [PubMed]
- Mancini, A.J.; Kaulback, K.; Chamlin, S.L. The socioeconomic impact of atopic dermatitis in the United States: A systematic review. Pediatr. Dermatol. 2008, 25, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Qobadi, M.; Collier, C.; Zhang, L. The effect of stressful life events on postpartum depression: Findings from the 2009–2011 Mississippi pregnancy risk assessment monitoring system. Matern. Child Health J. 2016, 20, 164–172. [Google Scholar] [CrossRef] [PubMed]
- Gitau, R.; Cameron, A.; Fisk, N.M.; Glover, V. Fetal exposure to maternal cortisol. Lancet 1998, 352, 707–708. [Google Scholar] [CrossRef]
- Lou, H.C.; Hansen, D.; Nordentoft, M.; Pryds, O.; Jensen, F.; Nim, J.; Hemmingsen, R. Prenatal stressors of human life affect fetal brain development. Dev. Med. Child Neurol. 1994, 36, 826–832. [Google Scholar] [CrossRef] [PubMed]
- Pincus-Knackstedt, M.K.; Joachim, R.A.; Blois, S.M.; Douglas, A.J.; Orsal, A.S.; Klapp, B.F.; Wahn, U.; Hamelmann, E.; Arck, P.C. Prenatal stress enhances susceptibility of murine adult offspring toward airway inflammation. J. Immunol. 2006, 177, 8484–8492. [Google Scholar] [CrossRef] [PubMed]
- Boguniewicz, M.; Leung, D.Y. Atopic dermatitis: A disease of altered skin barrier and immune dysregulation. Immunol. Rev. 2011, 242, 233–246. [Google Scholar] [CrossRef] [PubMed]
- Veru, F.; Laplante, D.P.; Luheshi, G.; King, S. Prenatal maternal stress exposure and immune function in the offspring. Stress 2014, 17, 133–148. [Google Scholar] [CrossRef] [PubMed]
- Andersson, N.W.; Hansen, M.V.; Larsen, A.D.; Hougaard, K.S.; Kolstad, H.A.; Schlünssen, V. Prenatal maternal stress and atopic diseases in the child: A systematic review of observational human studies. Allergy 2016, 71, 15–26. [Google Scholar] [CrossRef] [PubMed]
- STROBE Checklists. Available online: https://www.strobe-statement.org/index.php?id=available-checklists (accessed on 10 January 2018).
- Chang, H.Y.; Suh, D.I.; Yang, S.I.; Kang, M.J.; Lee, S.Y.; Lee, E.; Choi, I.A.; Lee, K.S.; Shin, Y.J.; Shin, Y.H.; et al. Prenatal maternal distress affects atopic dermatitis in offspring mediated by oxidative stress. J. Allergy Clin. Immunol. 2016, 138, 468–475. [Google Scholar] [CrossRef] [PubMed]
- Wang, I.J.; Wen, H.J.; Chiang, T.L.; Lin, S.J.; Guo, Y.L. Maternal psychologic problems increased the risk of childhood atopic dermatitis. Pediatr. Allergy Immunol. 2016, 27, 169–176. [Google Scholar] [CrossRef] [PubMed]
- Wen, H.J.; Wang, Y.J.; Lin, Y.C.; Chang, C.C.; Shieh, C.C.; Lung, F.W.; Guo, Y.L. Prediction of atopic dermatitis in 2-yr-old children by cord blood IgE, genetic polymorphisms in cytokine genes, and maternal mentality during pregnancy. Pediatr. Allergy Immunol. 2011, 22, 695–703. [Google Scholar] [CrossRef] [PubMed]
- Letourneau, N.L.; Kozyrskyj, A.L.; Cosic, N.; Ntanda, H.N.; Anis, L.; Hart, M.J.; Campbell, T.S.; Giesbrecht, G.F.; The APrON Team. Maternal sensitivity and social support protect against childhood atopic dermatitis. Allergy Asthma Clin. Immunol. 2017, 13, 26. [Google Scholar] [CrossRef] [PubMed]
- Braig, S.; Weiss, J.M.; Stalder, T.; Kirschbaum, C.; Rothenbacher, D.; Genuneit, J. Maternal prenatal stress and child atopic dermatitis up to age 2 years: The Ulm SPATZ health study. Pediatr. Allergy Immunol. 2017, 28, 144–151. [Google Scholar] [CrossRef] [PubMed]
- Elbert, N.J.; Duijts, L.; den Dekker, H.T.; de Jong, N.W.; Nijsten, T.E.; Jaddoe, V.W.; de Jongste, J.C.; van Wijk, R.G.; Tiemeier, H.; Pasmans, S.G. Maternal psychiatric symptoms during pregnancy and risk of childhood atopic diseases. Clin. Exp. Allergy 2017, 47, 509–519. [Google Scholar] [CrossRef] [PubMed]
- El-Heis, S.; Crozier, S.R.; Healy, E.; Robinson, S.M.; Harvey, N.C.; Cooper, C.; Inskip, H.M.; Baird, J.; Southampton Women’s Survey Study Group; Godfrey, K.M. Maternal stress and psychological distress preconception: Association with offspring atopic eczema at age 12 months. Clin. Exp. Allergy 2017, 47, 760–769. [Google Scholar] [CrossRef] [PubMed]
- Sausenthaler, S.; Rzehak, P.; Chen, C.M.; Arck, P.; Bockelbrink, A.; Schäfer, T.; Schaaf, B.; Borte, M.; Herbarth, O.; Krämer, U.; et al. Stress-related maternal factors during pregnancy in relation to childhood eczema: Results from the LISA Study. J. Investig. Allergol. Clin. Immunol. 2009, 19, 481–487. [Google Scholar] [PubMed]
- Hartwig, I.R.; Sly, P.D.; Schmidt, L.A.; van Lieshout, R.J.; Bienenstock, J.; Holt, P.G.; Arck, P.C. Prenatal adverse life events increase the risk for atopic diseases in children, which is enhanced in the absence of a maternal atopic predisposition. J. Allergy Clin. Immunol. 2014, 134, 160–169. [Google Scholar] [CrossRef] [PubMed]
- Larsen, A.D.; Schlünssen, V.; Christensen, B.H.; Bonde, J.P.; Obel, C.; Thulstrup, A.M.; Hannerz, H.; Hougaard, K.S. Exposure to psychosocial job strain during pregnancy and odds of asthma and atopic dermatitis among 7-year old children—A prospective cohort study. Scand. J. Work Environ. Health 2014, 40, 639–648. [Google Scholar] [CrossRef] [PubMed]
- De Marco, R.; Pesce, G.; Girardi, P.; Marchetti, P.; Rava, M.; Ricci, P.; Marcon, A. Foetal exposure to maternal stressful events increases the risk of having asthma and atopic diseases in childhood. Pediatr. Allergy Immunol. 2012, 23, 724–729. [Google Scholar] [CrossRef] [PubMed]
- Kinsella, M.T.; Monk, C. Impact of maternal stress, depression and anxiety on fetal neurobehavioral development. Clin. Obstet. Gynecol. 2009, 52, 425–440. [Google Scholar] [CrossRef] [PubMed]
- Dipietro, J.A. Maternal stress in pregnancy: Considerations for fetal development. J. Adolesc. Health 2012, 51, S3–S8. [Google Scholar] [CrossRef] [PubMed]
- Wegienka, G.; Johnson, C.C.; Zoratti, E.; Havstad, S. Racial differences in allergic sensitization: Recent findings and future directions. Curr. Allergy Asthma Rep. 2013, 13, 255–261. [Google Scholar] [CrossRef] [PubMed]
- Caruso, C.C. Negative impacts of shiftwork and long work hours. Rehabil. Nurs. 2014, 39, 16–25. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.Y.; Kim, E.; Choi, M.H. Technical and clinical aspects of cortisol as a biochemical marker of chronic stress. BMB Rep. 2015, 48, 209–216. [Google Scholar] [CrossRef] [PubMed]
- Yoon, S.; Sim, J.K.; Cho, Y.H. A flexible and wearable human stress monitoring patch. Sci. Rep. 2016, 6. [Google Scholar] [CrossRef] [PubMed]
| Item No. | Item | Braig et al., 2017 | Chang et al., 2016 | De Marco et al., 2012 | Elbert et al., 2017 | El-Heis et al., 2017 | Hartwig et al., 2014 | Larsen et al., 2014 | Letourneau et al., 2017 | Sausanthaler et al., 2009 | Wang et al., 2016 | Wen et al., 2011 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Study design described | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | No |
| 2 | Study setting described | Yes | No | Yes | No | Yes | Yes | No | Yes | Yes | Yes | Yes |
| 3 | Eligibility criteria of participants described | Yes | No | No | Yes | No | No | Yes | Yes | No | No | No |
| 4 | Outcomes and variables defined | Yes | Yes | Yes | Yes | Partial | Yes | Yes | Yes | Yes | Yes | Yes |
| 5 | Sources of measures described | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 6 | Attempts in addressing biases described | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 7 | Rationale of sample size given | No | No | No | No | No | No | No | No | No | No | No |
| 8 | Statistical methods described | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 9 | Number of participants at each study stage reported | Yes | No | Yes | Yes | No | No | No | Yes | Yes | Yes | Yes |
| 10 | Characteristics of participants reported | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| 11 | Outcome data reported | No | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes |
| 12 | Adjusted and/or unadjusted estimates reported | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Score (Max. 12) | 10 | 8 | 10 | 10 | 7 | 9 | 8 | 11 | 10 | 10 | 9 |
| Author/Year/Country | Design | Sample Size | Age of Child When Data Collection Was Performed | Methodology in Assessing Eczema | Stress Factor Studied | Confounding Factors Adjusted for | Major Findings |
|---|---|---|---|---|---|---|---|
| Braig et al., 2017; Germany [17] | Prospective cohort (longitudinal) | 787 mother-child pairs | 6 months 12 months 24 months | Self-report |
|
| Maternal stress and anxiety have positive associations with risk of child having atopic dermatitis (AD) symptoms at 2 years old, but no such associations were observed if we compare maternal stress and anxiety with diagnosis of AD using strict definitions. Adjusted relative risks (RR) when AD diagnosis was by presence of AD-associated symptoms Use of Inventory of Chronic Stress Screening Scale Adjusted RR: 1.5, 95% CI: 1.0–2.3, p = 0.05 Use of Hospital Anxiety and Depression Scale-Anxiety subscale Adjusted RR: 1.4, 95% CI: 1.0–2.0 Use of Hospital Anxiety and Depression Scale-Depression subscale Adjusted RR: 1.1, 95% CI: 0.5–2.1 Use of Pregnancy-related anxiety questionnaire Adjusted RR: 1.5, 95% CI: 0.9–2.4 Use of Hair cortisol concentration (comparison between 90th percentile with lowest quartile) Adjusted RR: 1.2, 95% CI: 0.8–2.0 Adjusted relative risks (RR) when AD diagnosis was strict definition of AD Use of Inventory of Chronic Stress Screening Scale Adjusted RR: 1.1, 95% CI: 0.7–1.9 Use of Hospital Anxiety and Depression Scale-Anxiety subscale Adjusted RR: 1.1, 95% CI: 0.7–1.9 Use of Hospital Anxiety and Depression Scale-Depression subscale Adjusted RR: 0.6, 95% CI: 0.2–2.3 Use of Pregnancy-related anxiety questionnaire Adjusted RR: 1.2, 95% CI: 0.6–2.4 Use of Hair cortisol concentration (comparison between 90th percentile with lowest quartile) Adjusted RR: 1.5, 95% CI: 0.8–2.7 |
| Chang et al., 2016; South Korea [13] | Two prospective cohort studies, including Cohort for Childhood Origin of Asthma and Allergic Diseases (COCOA) and Panel Study on Korean children (PSKC) (longitudinal) | COCOA: 973 mother-child pairs PSKC: 1531 mother-child pairs | 6 months 1 year 2 years 3 years 4 years | COCOA: clinical diagnosis PSKC: self-report |
|
| Both studies showed that prenatal depression/anxiety/distress are positively associated with the risk of child to develop atopic dermatitis. COCOA: Prenatal depression: Adjusted OR: 1.31, 95% CI: 1.02–1.69, p < 0.05 Prenatal anxiety Adjusted OR: 1.41, 95% CI: 1.06–1.89, p < 0.05 PSKC: Prenatal distress: Adjusted OR: 1.85, 95% CI: 1.06–3.25, p < 0.05 |
| de Marco et al., 2012; Italy [23] | Retrospective cohort (cross-sectional) | 3854 mother-child pairs | Not specified | Self-report |
|
| Exposure to stressful life events by mothers during pregnancy will increase the odds of the child having eczema Adjusted OR: 1.53, 95% CI: 1.11–2.10 |
| Elbert et al., 2017; Holland [18] | Prospective cohort (longitudinal) | 5205 mother-child pairs | 10 years | Self-report of physician diagnosis |
|
| 1-unit rise in measures for anxiety and depression is positively associated with eczema risk in children at 10 year, but only anxiety shows statistical significance for this association Anxiety during pregnancy Adjusted OR: 1.21, 95% CI: 1.05–1.39, p < 0.05 Depression during pregnancy Adjusted OR: 1.15, 95% CI: 1.02–1.29, p > 0.05 |
| El-Heis et al., 2017; United Kingdom [19] | Prospective cohort (longitudinal) | 3008 mother-child pairs | 6 months 12 months | self-report |
|
| At 6 months: All stress factors investigated have positive association with infant having eczema, but association is not significant. Perceived stress in life affecting subjects’ health Unadjusted OR: 1.10, 95% CI: 0.98–1.24, p = 0.093 Adjusted OR: 1.08, 95% CI: 0.96–1.23, p = 0.22 Perceived stress in daily living Unadjusted OR: 1.13, 95% CI: 1.01–1.28, p = 0.039 Adjusted OR: 1.12, 95% CI: 0.99–1.28, p = 0.072 Psychological distress Unadjusted OR: 1.21, 95% CI: 0.85–1.73, p = 0.30 Adjusted OR: 1.24, 95% CI: 0.84–1.83, p = 0.28 At 12 months: All stress factors investigated have positive association with infant having eczema, with most having association being significant. Perceived stress in life affecting subjects’ health Unadjusted OR: 1.21, 95% CI: 1.08–1.35, p = 0.001 Adjusted OR: 1.21, 95% CI: 1.01–1.37, p = 0.002 Perceived stress in daily living Unadjusted OR: 1.16, 95% CI: 1.03–1.30, p = 0.014 Adjusted OR: 1.14, 95% CI: 1.00–1.29, p = 0.046 Psychological distress Unadjusted OR: 1.43, 95% CI: 1.00–2.04, p = 0.044 Adjusted OR: 1.37, 95% CI: 0.93–2.01, p = 0.11 |
| Hartwig et al., 2014; Australia [21] | Prospective cohort (longitudinal) | 1587 mother-child pairs | 6 years 14 years | self-report of physician diagnosis coupled with self-report |
|
| Increased number of adverse life events experienced by mothers during gestation would result in increased odds of the child having eczema at both 6 years and 14 years of age. The odds increase even further if the adverse life events happen late during the gestational stage. At 6 years: Adverse life events in the first 18 weeks of gestation (comparing between 3 or more life events and no life events): Adjusted OR: 1.41, 95% CI: 0.61–3.29, p = 0.75 Adverse life events between 18–34 weeks of gestation (comparing between 3 or more life events and no life events): Adjusted OR: 2.38, 95% CI: 0.63–2.19, p = 0.21 At 14 years: Adverse life events in the first 18 weeks of gestation (comparing between 3 or more life events and no life events): Adjusted OR: 1.18, 95% CI: 0.54–2.60, p = 0.61 Adverse life events between 18-34 weeks of gestation (comparing between 3 or more life events and no life events): Adjusted OR: 4.19, 95% CI: 1.97–8.89, p < 0.01 |
| Larsen et al., 2014; Denmark [22] | Prospective cohort (longitudinal) | 32,271 mother-child pairs | 18 months 7 years | self-report |
|
| The level of job strain experienced by mothers during pregnancy increases the risk of their children having atopic dermatitis at 7 years of age. By comparing subjects in high-strain group and those in low-strain group: Adjusted OR: 1.15, 95% CI: 1.02–1.31, p < 0.001 |
| Letourneau et al., 2017; Canada [16] | Retrospective cohort (secondary data analysis) (cross-sectional) | 242 mother-child pairs | 18 months | self-report of physician diagnosis |
|
| Pregnancy-specific anxiety has a positive impact on the odds of the child having atopic dermatitis at 18 months. Unadjusted OR: 1.57, 95% CI: 0.76–3.27, p > 0.05 Adjusted OR: 2.74, 95% CI: 1.04–7.19, p < 0.05 |
| Sausenthaler et al., 2009; Germany [20] | Retrospective cohort (secondary data analysis) (longitudinal) | 3004 mother-child pairs | 0.5 year 1 year 1.5 years 2 years 4 years 6 years | self-report of physician diagnosis coupled with self-report |
|
| Maternal stress during pregnancy is positively correlated with the odds of the child having eczema up to 2 years old only At 1 year old Adjusted OR: 1.24, 95% CI: 0.72–2.13 At 2 years old Adjusted OR: 1.48, 95% CI: 0.95–2.30 At 3 years old Adjusted OR: 1.06, 95% CI: 0.66–1.70 At 4 years old Adjusted OR: 1.06, 95% CI: 0.67–1.68 At 5 years old Adjusted OR: 1.21, 95% CI: 0.76–1.91 At 6 years old Adjusted OR: 1.13, 95% CI: 0.71–1.79 |
| Wang et al., 2016; Taiwan [14] | Prospective cohort (longitudinal) | 18,024 mother-child pairs | 6 months 3 years | self-report of physician diagnosis coupled with self-report |
|
| Postpartum depression shows positive association on the risk of questionnaire-diagnosed atopic dermatitis and physician-diagnosed atopic dermatitis among children at 3 years old. Questionnaire-diagnosed atopic dermatitis (through observation of symptoms) Adjusted OR: 1.17, 95% CI: 0.97–1.41, p = 0.094 Physician-diagnosed atopic dermatitis Adjusted OR: 1.42, 95% CI: 1.21–1.66, p < 0.001 |
| Wen et al., 2011; Taiwan [15] | Prospective cohort (longitudinal) | 730 mother-child pairs | 6 months 2 years | self-report of physician diagnosis coupled with self-report |
|
| Maternal stress during pregnancy is positively correlated with the odds of the child being diagnosed with atopic dermatitis by a physician at 2 years old. Comparing between high and low reported level of maternal stress during pregnancy: Adjusted OR: 2.3, 95% CI: 1.1–5.3, p = 0.036 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chan, C.W.H.; Law, B.M.H.; Liu, Y.-H.; Ambrocio, A.R.B.; Au, N.; Jiang, M.; Chow, K.M. The Association between Maternal Stress and Childhood Eczema: A Systematic Review. Int. J. Environ. Res. Public Health 2018, 15, 395. https://doi.org/10.3390/ijerph15030395
Chan CWH, Law BMH, Liu Y-H, Ambrocio ARB, Au N, Jiang M, Chow KM. The Association between Maternal Stress and Childhood Eczema: A Systematic Review. International Journal of Environmental Research and Public Health. 2018; 15(3):395. https://doi.org/10.3390/ijerph15030395
Chicago/Turabian StyleChan, Carmen W. H., Bernard M. H. Law, Yun-Hong Liu, Alexandra R. B. Ambrocio, Natasha Au, Melody Jiang, and Ka Ming Chow. 2018. "The Association between Maternal Stress and Childhood Eczema: A Systematic Review" International Journal of Environmental Research and Public Health 15, no. 3: 395. https://doi.org/10.3390/ijerph15030395
APA StyleChan, C. W. H., Law, B. M. H., Liu, Y.-H., Ambrocio, A. R. B., Au, N., Jiang, M., & Chow, K. M. (2018). The Association between Maternal Stress and Childhood Eczema: A Systematic Review. International Journal of Environmental Research and Public Health, 15(3), 395. https://doi.org/10.3390/ijerph15030395





