Socio-Demographic and Mental Health Profile of Admitted Cases of Self-Inflicted Harm in the US Population
Abstract
:1. Introduction
2. Methods
2.1. Data Source and Participants
2.2. Study Variables
2.3. Data Analysis
3. Results
3.1. Characteristics of the Study Participants
3.2. Results of Multinomial Logistic Regression Analyses
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Appendix A




References
- Fliege, H.; Kocalevent, R.D.; Walter, O.B.; Beck, S.; Gratz, K.L.; Gutierrez, P.M.; Klapp, B.F. Three assessment tools for deliberate self-harm and suicide behavior: Evaluation and psychopathological correlates. J. Psychosom. Res. 2006, 61, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Klonsky, E.D. Non-suicidal self-injury in United States adults: Prevalence, sociodemographics, topography and functions. Psychol. Med. 2011, 41, 1981–1986. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Borges, G.; Walters, E.E. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch. Gen. Psychiatry 1999, 56, 617–626. [Google Scholar] [CrossRef] [PubMed]
- Olfson, M.; Gameroff, M.J.; Marcus, S.C.; Greenberg, T.; Shaffer, D. National trends in hospitalization of youth with intentional self-inflicted injuries. Am. J. Psychiatry 2005, 162, 1328–1335. [Google Scholar] [CrossRef] [PubMed]
- Olfson, M.; Wang, S.; Blanco, C. National trends in hospital-treated self-harm events among middle-aged adults. Gen. Hosp. Psychiatry 2015, 37, 613–619. [Google Scholar] [CrossRef] [PubMed]
- Canner, J.K.; Giuliano, K.; Selvarajah, S.; Hammond, E.R.; Schneider, E.B. Emergency department visits for attempted suicide and self harm in the USA: 2006–2013. Epidemiol. Psychiatr. Sci. 2016. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Web-Based Injury Statistics Query and Reporting System (WISQARS). Available online: https://www.cdc.gov/injury/wisqars/index.html (accessed on 22 September 2017).
- Owens, D.; House, A. General hospital services for deliberate self-harm. Haphazard clinical provision, little research, no central strategy. J. R. Coll. Physicians Lond. 1994, 28, 370–371. [Google Scholar] [PubMed]
- Ahmedani, B.K.; Perron, B.; Ilgen, M.; Abdon, A.; Vaughn, M.; Epperson, M. Suicide thoughts and attempts and psychiatric treatment utilization: Informing prevention strategies. Psychiatr. Serv. 2012, 63, 186–189. [Google Scholar] [CrossRef] [PubMed]
- Doshi, A.; Boudreaux, E.D.; Wang, N.; Pelletier, A.J.; Camargo, C.A., Jr. National study of US emergency department visits for attempted suicide and self-inflicted injury, 1997–2001. Ann. Emerg. Med. 2005, 46, 369–375. [Google Scholar] [CrossRef] [PubMed]
- Bazargan-Hejazi, S.; Ahmadi, A.; Bazargan, M.; Rahmani, E.; Pan, D.; Zahmatkesh, G.; Teruya, S. Profile of Hospital Admissions due to Self-Inflicted Harm in Los Angeles County from 2001 to 2010. J. Forensic Sci. 2017, 62, 1244–1250. [Google Scholar] [CrossRef] [PubMed]
- National Trauma Data Bank. Available online: https://www.facs.org/quality-programs/trauma/ntdb (accessed on 22 September 2017).
- Centers for Disease Control and Prevention (CDC). Nonfatal self-inflicted injuries treated in hospital emergency departments—United States, 2000. MMWR Morb. Mortal. Wkly. Rep. 2002, 51, 436–438. [Google Scholar]
- Salman, S.; Idrees, J.; Hassan, F.; Idrees, F.; Arifullah, M.; Badshah, S. Predictive Factors of Suicide Attempt and Non-Suicidal Self-Harm in Emergency Department. Emerg 2014, 2, 166–169. [Google Scholar]
- Haw, C.; Hawton, K.; Houston, K.; Townsend, E. Correlates of relative lethality and suicidal intent among deliberate self-harm patients. Suicide Life Threat. Behav. 2003, 33, 353–364. [Google Scholar] [CrossRef] [PubMed]
- Vaughn, M.G.; Salas-Wright, C.P.; DeLisi, M.; Larson, M. Deliberate self-harm and the nexus of violence, victimization, and mental health problems in the United States. Psychiatry Res. 2015, 225, 588–595. [Google Scholar] [CrossRef] [PubMed]
- United States QuickFacts. Available online: https://www.census.gov/quickfacts/fact/table/US/PST045216 (accessed on 22 September 2017).
- Crutcher, C.L., II; Fannin, E.S.; Wilson, J.D. Racial Disparities in Cranial Gunshot Wounds: Intent and Survival. J. Racial Ethn. Health Disparities 2016, 3, 687–691. [Google Scholar] [CrossRef] [PubMed]
- Prosser, J.M.; Perrone, J.; Pines, J.M. The epidemiology of intentional non-fatal self-harm poisoning in the United States: 2001–2004. J. Med. Toxicol. 2007, 3, 20–24. [Google Scholar] [CrossRef] [PubMed]
- Spicer, R.S.; Miller, T.R. Suicide acts in 8 states: Incidence and case fatality rates by demographics and method. Am. J. Public Health 2000, 90, 1885–1891. [Google Scholar] [PubMed]
- Taylor, D.M.; Cameron, P.A. Deliberate self-inflicted trauma: Population demographics, the nature of injury and a comparison with patients who overdose. Aust. N. Z. J. Public Health 1998, 22, 120–125. [Google Scholar] [CrossRef] [PubMed]
- Dennis, M.; Beach, M.; Evans, P.A.; Winston, A.; Friedman, T. An examination of the accident and emergency management of deliberate self harm. J. Accid. Emerg. Med. 1997, 14, 311–315. [Google Scholar] [CrossRef] [PubMed]
- Laskyte, A.; Zemaitiene, N. The types of deliberate self-harm and its prevalence among Lithuanian teenagers. Medicina 2009, 45, 132–139. [Google Scholar] [PubMed]
- Townsend, E.; Hawton, K.; Harriss, L.; Bale, E.; Bond, A. Substances used in deliberate self-poisoning 1985–1997: Trends and associations with age, gender, repetition and suicide intent. Soc. Psychiatry Psychiatr. Epidemiol. 2001, 36, 228–234. [Google Scholar] [CrossRef] [PubMed]
- Townsend, E.; Ness, J.; Waters, K.; Kapur, N.; Turnbull, P.; Cooper, J.; Bergen, H.; Hawton, K. Self-harm and life problems: Findings from the Multicentre Study of Self-harm in England. Soc. Psychiatry Psychiatr. Epidemiol. 2016, 51, 183–192. [Google Scholar] [CrossRef] [PubMed]
| Total in SIH Cases N | SIH Cases % | ||
|---|---|---|---|
| Race/Ethnicity | White | 122,606 | 71.6 |
| Black | 19,076 | 11.1 | |
| Hispanic | 18,525 | 10.8 | |
| Asian/Other | 11,050 | 6.5 | |
| Gender | Male | 154,373 | 75.8 |
| Female | 49,283 | 24.2 | |
| Age | 0–14 years | 2902 | 1.4 |
| 15–24 years | 42,826 | 21.0 | |
| 25–34 years | 45,059 | 22.1 | |
| 35–44 years | 38,367 | 18.9 | |
| 45–54 years | 37,783 | 18.6 | |
| 55–64 years | 20,709 | 10.2 | |
| 65–74 years | 8844 | 4.4 | |
| 75–84 years | 5415 | 2.7 | |
| 85+ years | 1508 | 0.7 | |
| Insurance | Private Insurance | 52,583 | 25.7 |
| Government Insurance | 67,519 | 33.0 | |
| Self-pay | 49,141 | 24.0 | |
| Other | 35,390 | 17.3 | |
| Year | Poisoning | Anoxic | Firearms | Cut/Pierce | Jumping | Other |
|---|---|---|---|---|---|---|
| 2007 | 249 (1.06) | 904 (3.83) | 8848 (37.49) | 6346 (26.89) | 4372 (18.53) | 2880 (12.20) |
| 2008 | 299 (1.00) | 831 (2.78) | 10,971 (36.71) | 8933 (29.89) | 5214 (17.45) | 3640 (12.18) |
| 2009 | 321 (0.99) | 1118 (3.43) | 12,242 (37.57) | 9236 (28.34) | 5629 (17.27) | 4039 (12.40) |
| 2010 | 312 (0.88) | 1200 (3.39) | 12,798 (36.19) | 10,038 (28.39) | 6484 (18.34) | 4530 (12.81) |
| 2011 | 260 (0.65) | 1407 (3.53) | 14,576 (36.61) | 11,435 (28.72) | 7256 (18.22) | 4881 (12.26) |
| 2012 | 431 (0.99) | 1621 (3.74) | 15,142 (34.90) | 12,356 (2848) | 8053 (18.56) | 5781 (13.33) |
| Total | 1872 (0.91) | 7081 (3.46) | 74,577 (36.44) | 58,344 (28.51) | 37,008 (18.09) | 25,751 (12.58) |
| Variables | Odds Ratios | Confidence Intervals |
|---|---|---|
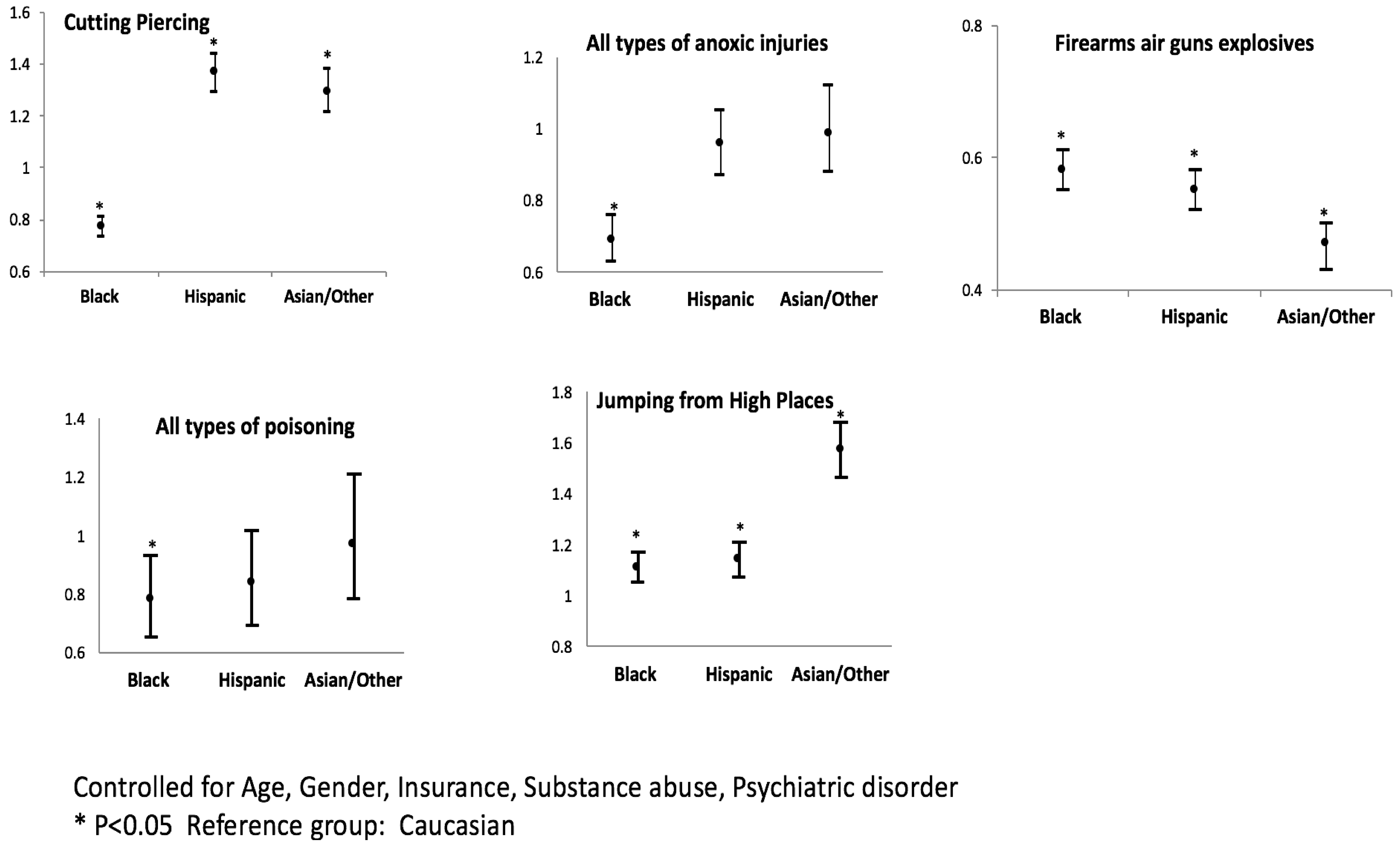
| Cutting/Piercing | ||
| 15–24 years | 1.36 | 1.23–1.51 |
| 25–34 years | 1.66 | 1.50–1.83 |
| 35–44 years | 1.81 | 1.64–1.99 |
| 45–54 years | 1.73 | 1.56–1.91 |
| 55–64 years | 1.63 | 1.47–1.81 |
| 65–74 years | 1.21 | 1.09–1.36 |
| 75–84 years | 0.99 | 0.87–1.11 |
| 85+ years | 1.29 | 1.10–1.51 |
| Female | 1.13 | 1.11–1.16 |
| Black | 0.98 | 0.95–1.02 |
| Hispanic | 1.72 | 1.67–1.78 |
| Asian/Other | 1.51 | 1.45–1.57 |
| Government Insurance | 1.25 | 1.21–1.29 |
| Self-Pay Insurance | 1.12 | 1.09–1.16 |
| Other Insurance | 1.14 | 1.10–1.18 |
| Psychiatric Disorder | 2.46 | 2.42–2.96 |
| Substance Abuse | 2.22 | 2.05–2.43 |
| Anoxic Injuries | ||
| 15–24 years | 0.28 | 0.25–0.32 |
| 25–34 years | 0.24 | 0.21–0.27 |
| 35–44 years | 0.26 | 0.23–0.29 |
| 45–54 years | 0.19 | 0.17–0.22 |
| 55–64 years | 0.12 | 0.10–0.14 |
| 65–74 years | 0.06 | 0.05–0.08 |
| 75–84 years | 0.06 | 0.04–0.08 |
| 85+ years | 0.08 | 0.05–0.12 |
| Female | 0.78 | 0.74–0.84 |
| Black | 0.87 | 0.80–0.94 |
| Hispanic | 1.01 | 0.93–1.10 |
| Asian/Other | 0.98 | 0.88–1.09 |
| Government Insurance | 1.15 | 1.08–1.23 |
| Self-Pay Insurance | 0.97 | 0.90–1.05 |
| Other Insurance | 1.09 | 1.00–1.19 |
| Psychiatric Disorder | 1.1 | 0.84–1.43 |
| Substance Abuse | 1.16 | 0.94–1.44 |
| Firearms | ||
| 15–24 years | 0.92 | 0.84–1.00 |
| 25–34 years | 0.87 | 0.80–0.96 |
| 35–44 years | 0.9 | 0.82–0.99 |
| 45–54 years | 1.16 | 1.06–1.26 |
| 55–64 years | 1.55 | 1.41–1.70 |
| 65–74 years | 3.45 | 3.12–3.81 |
| 75–84 years | 4.64 | 4.17–5.17 |
| 85+ years | 3.3 | 2.86–3.81 |
| Female | 0.5 | 0.49–0.51 |
| Black | 0.66 | 0.64–0.68 |
| Hispanic | 0.47 | 0.46–0.49 |
| Asian/Other | 0.37 | 0.35–0.39 |
| Government Insurance | 0.7 | 0.68–0.72 |
| Self-Pay Insurance | 1.18 | 1.14–1.21 |
| Other Insurance | 0.85 | 0.82–0.88 |
| Psychiatric Disorder | 0.47 | 0.42–0.54 |
| Substance Abuse | 0.68 | 0.62–0.75 |
| Poisoning | ||
| 15–24 years | 0.43 | 0.33–0.55 |
| 25–34 years | 0.25 | 0.19–0.33 |
| 35–44 years | 0.4 | 0.31–0.52 |
| 45–54 years | 0.4 | 0.31–0.53 |
| 55–64 years | 0.46 | 0.35–0.61 |
| 65–74 years | 0.25 | 0.17–0.36 |
| 75–84 years | 0.26 | 0.17–0.41 |
| 85+ years | 0.53 | 0.30–0.93 |
| Female | 2.57 | 2.33–2.84 |
| Black | 0.98 | 0.83–1.15 |
| Hispanic | 0.83 | 0.69–1.00 |
| Asian/Other | 0.96 | 0.78–1.17 |
| Government Insurance | 1.02 | 0.90–1.15 |
| Self-Pay Insurance | 0.85 | 0.74–0.99 |
| Other Insurance | 0.79 | 0.66–0.94 |
| Psychiatric Disorder | 1.89 | 1.30–2.75 |
| Substance Abuse | 1.46 | 1.00–2.12 |
| Jumping from High Places | ||
| 15–24 years | 1.5 | 1.35–1.67 |
| 25–34 years | 1.52 | 1.37–1.69 |
| 35–44 years | 1.32 | 1.18–1.47 |
| 45–54 years | 1.17 | 10.5–1.31 |
| 55–64 years | 0.88 | 0.79–0.99 |
| 65–74 years | 0.48 | 0.42–0.55 |
| 75–84 years | 0.42 | 0.36–0.49 |
| 85+ years | 0.31 | 0.24–0.40 |
| Female | 1.53 | 1.49–1.57 |
| Black | 1.54 | 1.49–1.60 |
| Hispanic | 1.23 | 1.18–1.28 |
| Asian/Other | 1.83 | 1.74–1.91 |
| Government Insurance | 1.28 | 1.24–1.32 |
| Self-Pay Insurance | 0.76 | 0.73–0.79 |
| Other Insurance | 1.06 | 1.02–1.10 |
| Psychiatric Disorder | 0.62 | 0.53–0.72 |
| Substance Abuse | 0.52 | 0.46–0.60 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hanuscin, C.; Zahmatkesh, G.; Shirazi, A.; Pan, D.; Teklehaimanot, S.; Bazargan-Hejazi, S. Socio-Demographic and Mental Health Profile of Admitted Cases of Self-Inflicted Harm in the US Population. Int. J. Environ. Res. Public Health 2018, 15, 77. https://doi.org/10.3390/ijerph15010077
Hanuscin C, Zahmatkesh G, Shirazi A, Pan D, Teklehaimanot S, Bazargan-Hejazi S. Socio-Demographic and Mental Health Profile of Admitted Cases of Self-Inflicted Harm in the US Population. International Journal of Environmental Research and Public Health. 2018; 15(1):77. https://doi.org/10.3390/ijerph15010077
Chicago/Turabian StyleHanuscin, Chris, Golara Zahmatkesh, Anaheed Shirazi, Deyu Pan, Senait Teklehaimanot, and Shahrzad Bazargan-Hejazi. 2018. "Socio-Demographic and Mental Health Profile of Admitted Cases of Self-Inflicted Harm in the US Population" International Journal of Environmental Research and Public Health 15, no. 1: 77. https://doi.org/10.3390/ijerph15010077
APA StyleHanuscin, C., Zahmatkesh, G., Shirazi, A., Pan, D., Teklehaimanot, S., & Bazargan-Hejazi, S. (2018). Socio-Demographic and Mental Health Profile of Admitted Cases of Self-Inflicted Harm in the US Population. International Journal of Environmental Research and Public Health, 15(1), 77. https://doi.org/10.3390/ijerph15010077




