How Sensors Might Help Define the External Exposome
Abstract
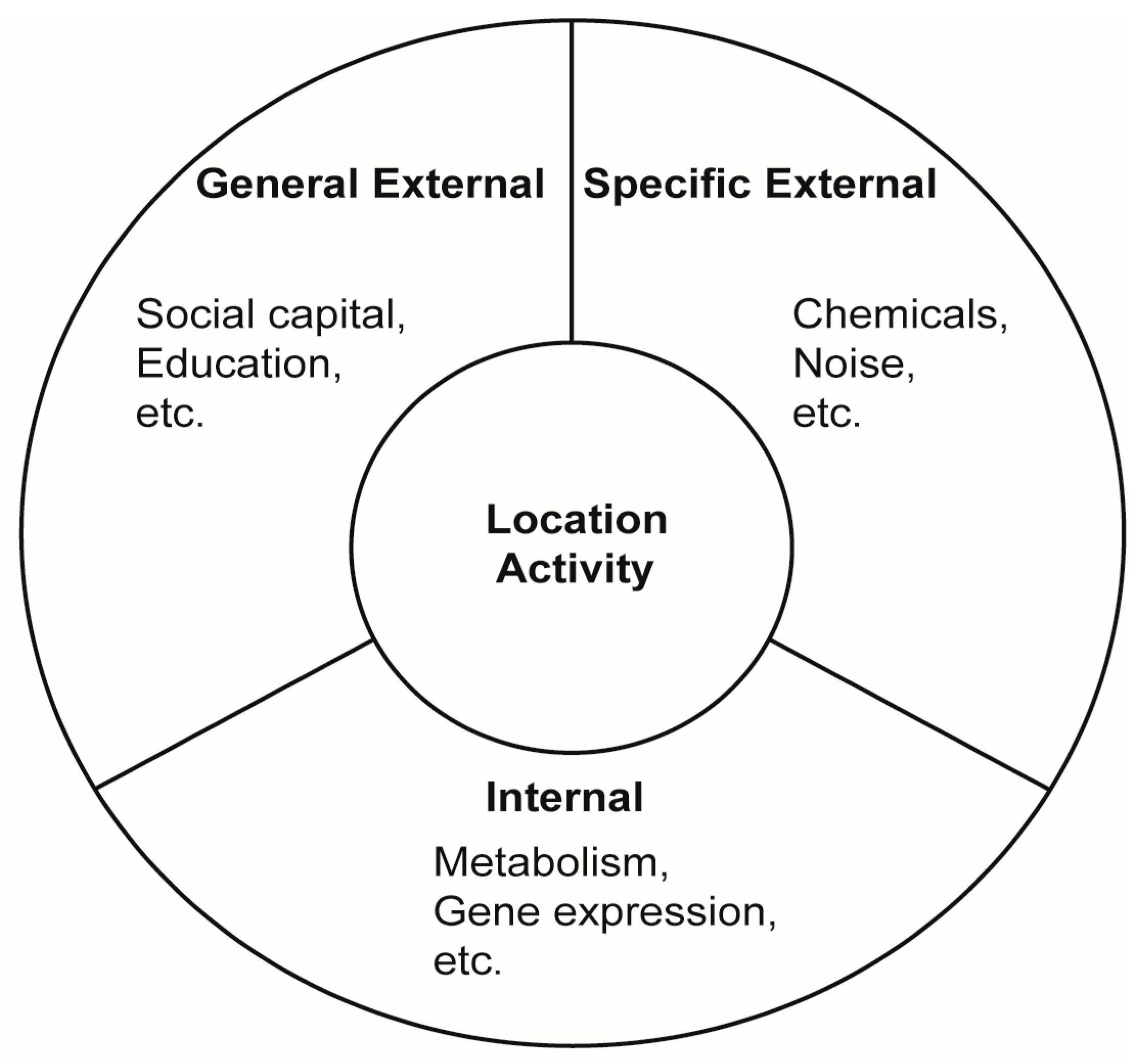
:1. Introduction
2. Sensor Criteria
- Unobtrusive to the user. Unobtrusive means that the item is easily worn/carried/placed.
- “Cost-effective”, i.e., such that widespread deployment of sensors is a practical proposition for the purpose and context of the study. Most research grade instruments are too expensive for large scale personal monitoring, either due to the expense of the equipment, and/or the cost of proprietary software licenses.
- Able to collect, store and transmit real-time and high temporal resolution data.
- Useable by a lay person.
- Ability to connect to the internet so that collected data can be remotely accessed by researchers and users, or, the ability to store collected data for download.
- Meets predefined quality assurance and quality control (QA/QC) specifications as defined for devices of a particular type, including: (i) Sufficient sensitivity and specificity or detection limits that allow environmental concentrations or other factors to be measured; (ii) Low failure rate; (iii) Adequate precision and accuracy to assess the relevant exposure; and (iv) Stability over time.
3. Exposure Parameters and Sensors
3.1. Location
3.2. Physical Activity
3.3. Diet
3.4. Indoor Climate
3.5. Air Quality
3.6. Noise
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- World Health Organization. Health and Environment in Europe: Progress Assessment; WHO Regional Office for Europe: Copenhagen, Denmark, 2010. [Google Scholar]
- Rappaport, S.M.; Smith, M.T. Epidemiology. Environment and disease risks. Science 2010, 330, 460–461. [Google Scholar] [CrossRef] [PubMed]
- Wild, C.P. Complementing the genome with an “exposome”: The outstanding challenge of environmental exposure measurement in molecular epidemiology. Cancer Epidemiol. Biomark. Prev. 2005, 14, 1847–1850. [Google Scholar] [CrossRef] [PubMed]
- Wild, C.P. The exposome: From concept to utility. Int. J. Epidemiol. 2012, 41, 24–32. [Google Scholar] [CrossRef] [PubMed]
- Jacquez, G.M.; Sabel, C.E.; Shi, C. Genetic GIScience: Toward a place-based synthesis of the genome, exposome, and behavome. Ann. Assoc. Am. Geogr. 2015, 105, 454–472. [Google Scholar] [CrossRef] [PubMed]
- Richardson, D.B.; Volkow, N.D.; Kwan, M.P.; Kaplan, R.M.; Goodchild, M.F.; Croyle, R.T. Spatial turn in health research. Science 2013, 339, 1390–1392. [Google Scholar] [CrossRef] [PubMed]
- Yatsunenko, T.; Rey, F.E.; Manary, M.J.; Trehan, I.; Dominguez-Bello, M.G.; Contreras, M.; Magris, M.; Hidalgo, G.; Baldassano, R.N.; Anokhin, A.P.; et al. Human gut microbiome viewed across age and geography. Nature 2012, 486, 222–227. [Google Scholar] [CrossRef] [PubMed]
- Kwan, M.-P. Gender differences in space-time constraints. Area 2000, 32, 145–156. [Google Scholar] [CrossRef]
- Miller, H.J. A measurement theory for time geography. Geogr. Anal. 2005, 37, 17–45. [Google Scholar] [CrossRef]
- Schaerstrom, A. The potential for time geography in medical geography. Geogr. Health Inserm. Paris 2003, 195–207. [Google Scholar]
- Jantunen, M.J.; Hanninen, O.; Katsouyanni, K.; Knoppel, H.; Kuenzli, N.; Lebret, E.; Maroni, M.; Saarela, K.; Sram, R.J.; Zmirou, D. Air pollution exposure in European cities: The “EXPOLIS” study. J. Expo. Anal. Environ. Epidemiol. 1998, 8, 495–518. [Google Scholar]
- Nieuwenhuijsen, M.J.; Donaire-Gonzalez, D.; Foraster, M.; Martinez, D.; Cisneros, A. Using personal sensors to assess the exposome and acute health effects. Int. J. Environ. Res. Public Health 2014, 11, 7805–7819. [Google Scholar] [CrossRef] [PubMed]
- Sax, S.N. Evaluation of Exposures and Cancer Risks from Volatile Organic Compounds among Inner-City Teenagers. Ph.D. Thesis, Harvard School of Public Health, Boston, MA, USA, 2003. [Google Scholar]
- Steinle, S.; Reis, S.; Sabel, C. Quantifying human exposure to air pollution-Moving from static monitoring to spatio-temporally resolved personal exposure assessment. Sci. Total Environ. 2013, 443, 184–193. [Google Scholar] [CrossRef] [PubMed]
- Sadler, R.C.; Gilliland, J.A. Comparing children’s GPS tracks with geospatial proxies for exposure to junk food. Spat. Spatio-Temporal Epidemiol. 2015, 14–15, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Elgethun, K.; Yost, M.G.; Fitzpatrick, C.T.E.; Nyerges, T.L.; Fenske, R.A. Comparison of global positioning system (GPS) tracking and parent-report diaries to characterize children’s time-location patterns. J. Expo. Sci. Environ. Epidemiol. 2006, 17, 196–206. [Google Scholar] [CrossRef] [PubMed]
- Adams, C.; Riggs, P.; Volckens, J. Development of a method for personal, spatiotemporal exposure assessment. J. Environ. Monit. 2009, 11, 1331. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Jiang, C.; Liu, Z.; Houston, D.; Jaimes, G.; McConnell, R. Performances of different global positioning system devices for time-location tracking in air pollution epidemiological studies. Environ. Health Insights 2010, 4, 93–108. [Google Scholar] [PubMed]
- Beekhuizen, J.; Kromhout, H.; Huss, A.; Vermeulen, R. Performance of GPS-devices for environmental exposure assessment. J. Expo. Sci. Environ. Epidemiol. 2013, 23, 498–505. [Google Scholar] [CrossRef] [PubMed]
- De Nazelle, A.; Seto, E.; Donaire-Gonzalez, D.; Mendez, M.; Matamala, J.; Nieuwenhuijsen, M.J.; Jerrett, M. Improving estimates of air pollution exposure through ubiquitous sensing technologies. Environ. Pollut. 2013, 176, 92–99. [Google Scholar] [CrossRef] [PubMed]
- Wiehe, S.E.; Carroll, A.E.; Liu, G.C.; Haberkorn, K.L.; Hoch, S.C.; Wilson, J.S.; Jerrett, M. Using GPS-enabled cell phones to track the travel patterns of adolescents. Int. J. Health Geogr. 2008, 7, 22. [Google Scholar] [CrossRef] [PubMed]
- Zandbergen, P.A.; Barbeau, S.J. Positional accuracy of assisted GPS data from high-sensitivity GPS-enabled mobile phones. J. Navig. 2011, 64, 381–399. [Google Scholar] [CrossRef]
- Donaire-Gonzalez, D.; Valentín, A.; de Nazelle, A.; Ambros, A.; Carrasco-Turigas, G.; Seto, E.; Jerrett, M.; Nieuwenhuijsen, M.J. Benefits of Mobile Phone Technology for Personal Environmental Monitoring. JMIR mHealth uHealth 2016, 4, e126. [Google Scholar] [CrossRef] [PubMed]
- Hurvitz, P.M.; Moudon, A.V.; Kang, B.; Saelens, B.E.; Duncan, G.E. Emerging technologies for assessing physical activity behaviors in space and time. Front. Public Health 2014, 2, 2. [Google Scholar] [CrossRef] [PubMed]
- Su, J.G.; Jerrett, M.; Meng, Y.-Y.; Pickett, M.; Ritz, B. Integrating smart-phone based momentary location tracking with fixed site air quality monitoring for personal exposure assessment. Sci. Total Environ. 2015, 506–507, 518–526. [Google Scholar] [CrossRef] [PubMed]
- Wan, N.; Lin, G. Classifying human activity patterns from smartphone collected GPS data: A fuzzy classification and aggregation approach. Trans. GIS 2016, 20, 869–886. [Google Scholar] [CrossRef]
- Hu, M.; Li, W.; Li, L.; Houston, D.; Wu, J. Refining time-activity classification of human subjects using the global positioning system. PLoS ONE 2016, 11, e0148875. [Google Scholar] [CrossRef] [PubMed]
- Breen, M.S.; Long, T.C.; Schultz, B.D.; Crooks, J.; Breen, M.; Langstaff, J.E.; Isaacs, K.K.; Tan, Y.M.; Williams, R.W. GPS-based microenvironment tracker (MicroTrac) model to estimate time–location of individuals for air pollution exposure assessments: Model evaluation in central North Carolina. J. Expo. Sci. Environ. Epidemiol. 2014, 24, 412–420. [Google Scholar] [CrossRef] [PubMed]
- Zhou, P.; Zheng, Y.; Li, Z.; Li, M.; Shen, G. IODetector: A generic service for indoor outdoor detection. In Proceedings of the 10th ACM Conference on Embedded Network Sensor Systems, Toronto, ON, Canada, 6–9 November 2012. [Google Scholar]
- Radu, V.; Katsikouli, P.; Sarkar, R.; Marina, M.K. A semi-supervised learning approach for robust indoor-outdoor detection with smartphones. In Proceedings of the 12th ACM Conference on Embedded Network Sensor Systems, Memphis, TN, USA, 3–6 November 2014. [Google Scholar]
- Gerharz, L.E.; Kruger, A.; Klemm, O. Applying indoor and outdoor modeling techniques to estimate individual exposure to PM2.5 from personal GPS profiles and diaries: A pilot study. Sci. Total Environ. 2009, 407, 5184–5193. [Google Scholar] [CrossRef] [PubMed]
- Glasgow, M.L.; Rudra, C.B.; Yoo, E-H.; Demirbas, M.; Merriman, J.; Nayak, P.; Crabtree-Ide, C.; Szpiro, A.A.; Rudra, A.; Wactawski-Wende, J.; et al. Using smartphones to collect time–activity data for long-term personal-level air pollution exposure assessment. J. Expo. Sci. Environ. Epidemiol. 2014, 26, 356–364. [Google Scholar] [CrossRef] [PubMed]
- Bassett, D.R. Device-based monitoring in physical activity and public health research. Physiol. Meas. 2012, 33, 1769–1783. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.-C.; Hsu, Y.-L. A Review of Accelerometry-Based Wearable Motion Detectors for Physical Activity Monitoring. Sensors 2010, 10, 7772–7788. [Google Scholar] [CrossRef] [PubMed]
- Loprinzi, P.D.; Lee, H.; Cardinal, B.J.; Crespo, C.J.; Andersen, R.E.; Smit, E. The relationship of actigraph accelerometer cut-points for estimating physical activity with selected health outcomes. Res. Q. Exerc. Sport 2012, 83, 422–430. [Google Scholar] [CrossRef] [PubMed]
- Hailstone, J.; Kilding, A.E. Reliability and Validity of the ZephyrTM BioHarnessTM to Measure Respiratory Responses to Exercise. Meas. Phys. Educ. Exerc. Sci. 2011, 15, 293–300. [Google Scholar] [CrossRef]
- Case, M.A.; Burwick, H.A.; Volpp, K.G.; Patel, M.S. Accuracy of smartphone applications and wearable devices for tracking physical activity data. JAMA 2015, 313, 625–626. [Google Scholar] [CrossRef] [PubMed]
- Adam Noah, J.; Spierer, D.K.; Gu, J.; Bronner, S. Comparison of steps and energy expenditure assessment in adults of Fitbit Tracker and Ultra to the Actical and indirect calorimetry. J. Med. Eng. Technol. 2013, 37, 456–462. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, E.A.; Western, M.J.; Nightingale, T.E.; Peacock, O.J.; Thompson, D. Assessment of laboratory and daily energy expenditure estimates from consumer multi-sensor physical activity monitors. PLoS ONE 2017, 12, e0171720. [Google Scholar] [CrossRef] [PubMed]
- Chu, A.H.Y.; Ng, S.H.X.; Paknezhad, M.; Gauterin, A.; Koh, D.; Brown, M.S.; Riemenschneider, F.M. Comparison of wrist-worn Fitbit Flex and waist-worn ActiGraph for measuring steps in free-living adults. PLoS ONE 2017, 12, e0172535. [Google Scholar] [CrossRef] [PubMed]
- Evenson, K.R.; Goto, M.M.; Furberg, R.D. Systematic review of the validity and reliability of consumer-wearable activity trackers. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 159. [Google Scholar] [CrossRef] [PubMed]
- Takacs, J.; Pollock, C.L.; Guenther, J.R.; Bahar, M.; Napier, C.; Hunt, M.A. Validation of the Fitbit One activity monitor device during treadmill walking. J. Sci. Med. Sport 2014, 17, 496–500. [Google Scholar] [CrossRef] [PubMed]
- Woodman, J.A.; Crouter, S.E.; Bassett, D.R.; Fitzhugh, E.C.; Boyer, W.R. Accuracy of Consumer Monitors for Estimating Energy Expenditure and Activity Type. Med. Sci. Sports Exerc. 2017, 49, 371–377. [Google Scholar] [CrossRef] [PubMed]
- Kooiman, T.J.M.; Dontje, M.L.; Sprenger, S.R.; Krijnen, W.P.; van der Schans, C.P.; de Groot, M. Reliability and validity of ten consumer activity trackers. BMC Sports Sci. Med. Rehabil. 2015, 7, 24. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.-M.; Kim, Y.; Welk, G.J. Validity of consumer-based physical activity monitors. Med. Sci. Sports Exerc. 2014, 46, 1840–1848. [Google Scholar] [CrossRef] [PubMed]
- Mammen, G.; Gardiner, S.; Senthinathan, A.; McClemont, L.; Stone, M.; Faulkner, G. Is this bit fit? Measuring the quality of the fitbit step-counter. Health Fit. J. Can. 2012, 5, 30–39. [Google Scholar]
- Guo, F.; Li, Y.; Kankanhalli, M.S.; Brown, M.S. An Evaluation of Wearable Activity Monitoring Devices. In Proceedings of the 1st ACM International Workshop on Personal Data Meets Distributed Multimedia, New York, NY, USA, 21–25 October 2013. [Google Scholar]
- Bates, A.; Ling, M.J.; Mann, J.; Arvind, D.K. Respiratory Rate and Flow Waveform Estimation from Tri-axial Accelerometer Data. In Proceedings of the 2010 International Conference on Body Sensor Networks (BSN), Los Alamitos, CA, USA, 7–9 June 2010; pp. 144–150. [Google Scholar]
- Mann, J.; Rabinovich, R.; Bates, A.; Giavedoni, S.; MacNee, W.; Arvind, D.K. Simultaneous Activity and Respiratory Monitoring Using an Accelerometer. In Proceedings of the 8th International Conference on Body Sensor Networks, Dallas, TX, USA, 23–25 May 2011. [Google Scholar]
- Rusin, M.; Arsand, E.; Hartvigsen, G. Functionalities and input methods for recording food intake: A systematic review. Int. J. Med. Inf. 2013, 82, 653–664. [Google Scholar] [CrossRef] [PubMed]
- Cade, J. Measuring diet in the 21st century: Use of new technologies. Proc. Nutr. Soc. 2016, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Illner, A.K.; Harttig, U.; Tognon, G.; Palli, D.; Salvini, S.; Bower, E.; Amiano, P.; Kassik, T.; Metspalu, A.; Engeset, D.; et al. Feasibility of innovative dietary assessment in epidemiological studies using the approach of combining different assessment instruments. Public Health Nutr. 2011, 14, 1055–1063. [Google Scholar] [CrossRef] [PubMed]
- Shim, J.S.; Oh, K.; Kim, H.C. Dietary assessment methods in epidemiologic studies. Epidemiol. Health 2014, 36. [Google Scholar] [CrossRef] [PubMed]
- Forster, H.; Fallaize, R.; Gallagher, C.; O’Donovan, C.B.; Woolhead, C.; Walsh, M.C.; Macready, A.L.; Lovegrove, J.A.; Mathers, J.C.; Gibney, M.J.; et al. Online dietary intake estimation: The food4Me Food frequency questionnaire. J. Med. Internet Res. 2014, 16, e150. [Google Scholar] [CrossRef] [PubMed]
- Liu, B.; Young, H.; Crowe, F.L.; Benson, V.S.; Spencer, E.A.; Key, T.J.; Appleby, P.N.; Beral, V. Development and evaluation of the Oxford WebQ, a low-cost, web-based method for assessment of previous 24 h dietary intakes in large-scale prospective studies. Public Health Nutr. 2011, 14, 1998–2005. [Google Scholar] [CrossRef] [PubMed]
- Matthys, C.; Pynaert, I.; De Keyzer, W.; De Henauw, S. Validity and reproducibility of an adolescent web-based food frequency questionnaire. J. Am. Diet. Assoc. 2007, 107, 605–610. [Google Scholar] [CrossRef] [PubMed]
- Ngo, J.; Engelen, A.; Molag, M.; Roesle, J.; García-Segovia, P.; Serra-Majem, L. A review of the use of information and communication technologies for dietary assessment. Br. J. Nutr. 2009, 101 (Suppl. 2), S102–S112. [Google Scholar] [CrossRef] [PubMed]
- Touvier, M.; Kesse-Guyot, E.; Méjean, C.; Pollet, C.; Malon, A.; Castetbon, K.; Hercberg, S. Comparison between an interactive web-based self-administered 24 h dietary record and an interview by a dietitian for large-scale epidemiological studies. Br. J. Nutr. 2011, 105, 1055–1064. [Google Scholar] [CrossRef] [PubMed]
- Vereecken, C.A.; Covents, M.; Sichert-Hellert, W.; Alvira, J.M.F.; Le Donne, C.; De Henauw, S.; De Vriendt, T.; Phillipp, M.K.; Béghin, L.; Manios, Y.; et al. Development and evaluation of a self-administered computerized 24-h dietary recall method for adolescents in Europe. Int. J. Obes. 2008, 32 (Suppl. 5), S26–S34. [Google Scholar] [CrossRef] [PubMed]
- Kumar, P.; Morawska, L.; Martani, C.; Biskos, G.; Neophytou, M.; Di Sabatino, S.; Bell, M.; Norford, L.; Britter, R. The rise of low-cost sensing for managing air pollution in cities. Environ. Int. 2015, 75, 199–205. [Google Scholar] [CrossRef] [PubMed]
- Mead, M.I.; Popoola, O.A.M.; Stewart, G.B.; Landshoff, P.; Calleja, M.; Hayes, M.; Baldoví, J.; McLeod, M.W.; Hodgson, T.F.; Dicks, J.; et al. The use of electrochemical sensors for monitoring urban air quality in low-cost, high-density networks. Atmos. Environ. 2013, 70, 186–203. [Google Scholar] [CrossRef]
- Williams, R.; Long, R.; Beaver, M.; Kaufman, A.; Zeiger, F.; Heimbinder, M.; Hang, I.; Yap, R.; Acharya, B.; Ginwald, B.; et al. Sensor Evaluation Report; Report EPA/600/R-14/143; Environmental Protection Agency: Washington, DC, USA, 2014.
- Piedrahita, R.; Xiang, Y.; Masson, N.; Ortega, J.; Collier, A.; Jiang, Y.; Li, K.; Dick, R.P.; Lv, Q.; Hannigan, M.; et al. The next generation of low-cost personal air quality sensors for quantitative exposure monitoring. Atmos. Meas. Tech. 2014, 7, 2425–2457. [Google Scholar] [CrossRef]
- Fine, G.F.; Cavanagh, L.M.; Afonja, A.; Binions, R. Metal oxide semi-conductor gas sensors in environmental monitoring. Sensors 2010, 10, 5469–5502. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Yin, L.; Zhang, L.; Xiang, D.; Gao, R. Metal oxide gas sensors: Sensitivity and influencing factors. Sensors 2010, 10, 2088–2106. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.; Gillespie, J.; Schuder, M.D.; Duberstein, W.; Beverland, I.J.; Heal, M.R. Evaluation and calibration of Aeroqual series 500 portable gas sensors for accurate measurement of ambient ozone and nitrogen dioxide. Atmos. Environ. 2015, 100, 111–116. [Google Scholar] [CrossRef]
- Holstius, D.M.; Pillarisetti, A.; Smith, K.R.; Seto, E. Field calibrations of a low-cost aerosol sensor at a regulatory monitoring site in California. Atmos. Meas. Tech. 2014, 7, 605–632. [Google Scholar] [CrossRef]
- Northcross, A.L.; Edwards, R.J.; Johnson, M.A.; Wang, Z.M.; Zhu, K.; Allen, T.; Smitha, K.R. A low-cost particle counter as a realtime fine-particle mass monitor. Environ. Sci. Process. Impacts 2013, 15, 433. [Google Scholar] [CrossRef] [PubMed]
- Semple, S.; Ibrahim, A.E.; Apsley, A.; Steiner, M.; Turner, S. Using a new, low-cost air quality sensor to quantify second-hand smoke (SHS) levels in homes. Tob. Control 2013, 24, 153–158. [Google Scholar] [CrossRef] [PubMed]
- Manikonda, A.; Zíková, N.; Hopke, P.K.; Ferro, A.R. Laboratory assessment of low-cost PM monitors. J. Aerosol. Sci. 2016, 102, 29–40. [Google Scholar] [CrossRef]
- Volckens, J.; Quinn, C.; Leith, D.; Mehaffy, J.; Henry, C.S.; Miller-Lionberg, D. Development and evaluation of an ultrasonic personal aerosol sampler. Indoor Air 2017, 27, 409–416. [Google Scholar] [CrossRef] [PubMed]
- Moore, E.; Chatzidiakou, L.; Jones, R.L.; Smeeth, L.; Beevers, S.; Kelly, F.J.; Quint, J.K.; Barratt, B. Linking e-health records, patient-reported symptoms and environmental exposure data to characterise and model COPD exacerbations: Protocol for the COPE study. BMJ Open 2016, 6, e011330. [Google Scholar] [CrossRef] [PubMed]
- Kardous, C.A.; Shaw, P.B. Evaluation of smartphone sound measurement applications. J. Acoust. Soc. Am. 2014, 135, EL186–EL192. [Google Scholar] [CrossRef] [PubMed]
- Maisonneuve, N.; Stevens, M.; Niessen, M.E.; Steels, L. NoiseTube: Measuring and mapping noise pollution with mobile phones. In Information Technologies in Environmental Engineering; Athanasiadis, I.N., Rizzoli, A.E., Mitkas, P.A., Gómez, J.M., Eds.; Springer: Berlin/Heidelberg, Germany, 2009; pp. 215–228. [Google Scholar]
- Murphy, E.; King, E.A. Testing the accuracy of smartphones and sound level meter applications for measuring environmental noise. Appl. Acoust. 2016, 106, 16–22. [Google Scholar] [CrossRef]
- Schreckenberg, D.; Griefahn, B.; Meis, M. The associations between noise sensitivity, reported physical and mental health, perceived environmental quality, and noise annoyance. Noise Health 2010, 12, 7. [Google Scholar] [CrossRef] [PubMed]
- Shiffman, S.; Stone, A.A.; Hufford, M.R. Ecological Momentary Assessment. Annu. Rev. Clin. Psychol. 2008, 4, 1–32. [Google Scholar] [CrossRef] [PubMed]
- Stahler, G.J.; Baron, D.A. Geospatial technology and the “exposome”: New perspectives on addiction. Am. J. Public Health 2013, 103, 1354–1356. [Google Scholar] [CrossRef] [PubMed]
- Sarigiannis, D.; Gotti, A.; Cimino Reale, G.; Marafante, E. Reflections on new directions for risk assessment of environmental chemical mixtures. Int. J. Risk Assess Manag. 2009, 13, 216–241. [Google Scholar] [CrossRef]
- Armstrong, S. What happens to data gathered by health and wellness apps? BMJ 2016, 353, i3406. [Google Scholar] [CrossRef] [PubMed]
- Paul, G.; Irvine, J. Privacy Implications of wearable health devices. In Proceedings of the 7th International Conference on Security of Information and Networks, New York, NY, USA, 9–11 September 2014. [Google Scholar]
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Loh, M.; Sarigiannis, D.; Gotti, A.; Karakitsios, S.; Pronk, A.; Kuijpers, E.; Annesi-Maesano, I.; Baiz, N.; Madureira, J.; Oliveira Fernandes, E.; et al. How Sensors Might Help Define the External Exposome. Int. J. Environ. Res. Public Health 2017, 14, 434. https://doi.org/10.3390/ijerph14040434
Loh M, Sarigiannis D, Gotti A, Karakitsios S, Pronk A, Kuijpers E, Annesi-Maesano I, Baiz N, Madureira J, Oliveira Fernandes E, et al. How Sensors Might Help Define the External Exposome. International Journal of Environmental Research and Public Health. 2017; 14(4):434. https://doi.org/10.3390/ijerph14040434
Chicago/Turabian StyleLoh, Miranda, Dimosthenis Sarigiannis, Alberto Gotti, Spyros Karakitsios, Anjoeka Pronk, Eelco Kuijpers, Isabella Annesi-Maesano, Nour Baiz, Joana Madureira, Eduardo Oliveira Fernandes, and et al. 2017. "How Sensors Might Help Define the External Exposome" International Journal of Environmental Research and Public Health 14, no. 4: 434. https://doi.org/10.3390/ijerph14040434
APA StyleLoh, M., Sarigiannis, D., Gotti, A., Karakitsios, S., Pronk, A., Kuijpers, E., Annesi-Maesano, I., Baiz, N., Madureira, J., Oliveira Fernandes, E., Jerrett, M., & Cherrie, J. W. (2017). How Sensors Might Help Define the External Exposome. International Journal of Environmental Research and Public Health, 14(4), 434. https://doi.org/10.3390/ijerph14040434







