Pericardial Effusion as a Presenting Symptom of Hashimoto Thyroiditis: A Case Report
Abstract
1. Background
2. Ethics, Approval and Consent to Participate
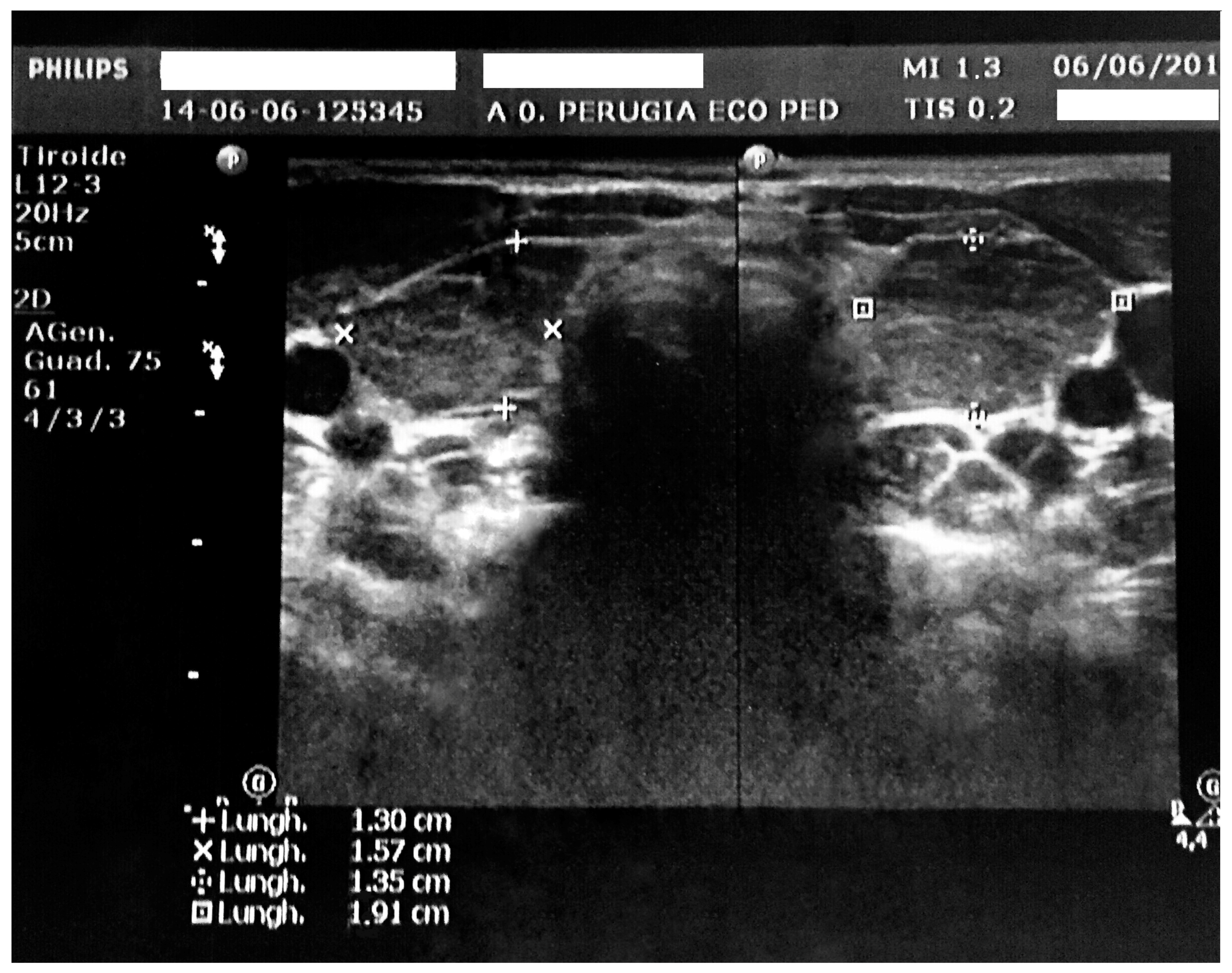
3. Case Report
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Brown, R.S. Autoimmune thyroiditis in childhood. J. Clin. Res. Pediatr. Endocrinol. 2013, 5, 45–49. [Google Scholar] [CrossRef] [PubMed]
- Eisenbarth, G.S. Autoimmune polyendocrine syndromes. Adv. Exp. Med. Biol. 2004, 552, 204–218. [Google Scholar] [CrossRef] [PubMed]
- Inoue, M.; Taketani, N.; Sato, T.; Nakajima, H. High incidence of chronic lymphocytic thyroiditis in apparently healthy school children: Epidemiological and clinical study. Endocrinol. Jpn. 1975, 22, 483–488. [Google Scholar] [CrossRef] [PubMed]
- Zois, C.; Stavrou, I.; Kalogera, C.; Svarna, E. High prevalence of autoimmune thyroiditis in school children after elimination of iodine deficiency in northwestern Greece. Thyroid 2003, 13, 485–489. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Shao, X.; Song, R.; Xu, D.; Zhang, J.A. The emerging role of epigenetics in autoimmune thyroid diseases. Front. Immunol. 2017, 8, 396. [Google Scholar] [CrossRef] [PubMed]
- Kabadi, U.M.; Kumar, S.P. Pericardial effusion in primary hypothyroidism. Am. Heart J. 1990, 120, 1393–1395. [Google Scholar] [CrossRef]
- Dinleyici, E.C.; Ucar, B.; Kilic, Z.; Dogruel, N.; Yarar, C. Pericardial effusion due to hypothyroidism in Down syndrome: Report of four cases. Neuro Endocrinol. Lett. 2007, 28, 141–144. [Google Scholar] [PubMed]
- Martinez-Soto, T.; Deal, C.; Stephure, D.; Trussell, R.; Boutin, C.; Djemli, A.; Ho, J. Pericardial effusion in severe hypothyroidism in children. J. Pediatr. Endocrinol. Metab. 2010, 23, 1165–1168. [Google Scholar] [CrossRef] [PubMed]
- Sanda, S.; Newfield, R.S. A child with pericardial effusion and cardiac tamponade due to previously unrecognized hypothyroidism. J. Natl. Med. Assoc. 2007, 99, 1411–1413. [Google Scholar] [PubMed]
- Lee, M.J.; Kim, B.Y.; Ma, J.S.; Choi, Y.E.; Kim, Y.O.; Cho, H.J.; Kin, C.J. Hashimoto thyroiditis with an unusual presentation of cardiac tamponade in Noonan syndrome. Korean J. Pediatr. 2016, 59 (Suppl. S1), S112–S115. [Google Scholar] [CrossRef] [PubMed]
- Cacciari, E.; Milani, S.; Balsamo, A.; Spada, E.; Bona, G.; Cavallo, L.; Cerutti, F.; Gargantini, L.; Greggio, N.; Tonini, G.; et al. Italian cross-sectional growth charts for height, weight and BMI (2 to 20 yr). J. Endocrinol. Investig. 2006, 29, 581–593. [Google Scholar] [CrossRef] [PubMed]
- Adler, Y.; Charron, P.; Imazio, M.; Badano, L.; Baron-Esquivias, G.; Bogaert, J.; Brucato, A.; Gueret, P.; Klingel, K.; Lionis, C.; et al. 2015 ESC Guidelines for the diagnosis and management of pericardial diseases. Eur. Heart J. 2015, 36, 2921–2964. [Google Scholar] [CrossRef] [PubMed]
- Klein, I.; Danzi, S. Thyroid disease and the heart. Curr. Probl. Cardiol. 2016, 41, 65–92. [Google Scholar] [CrossRef] [PubMed]
- Zaletel, K.; Gaberšček, S. Hashimoto’s thyroiditis: From genes to the disease. Curr. Genom. 2011, 12, 576–588. [Google Scholar] [CrossRef] [PubMed]

© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leonardi, A.; Penta, L.; Cofini, M.; Lanciotti, L.; Principi, N.; Esposito, S. Pericardial Effusion as a Presenting Symptom of Hashimoto Thyroiditis: A Case Report. Int. J. Environ. Res. Public Health 2017, 14, 1576. https://doi.org/10.3390/ijerph14121576
Leonardi A, Penta L, Cofini M, Lanciotti L, Principi N, Esposito S. Pericardial Effusion as a Presenting Symptom of Hashimoto Thyroiditis: A Case Report. International Journal of Environmental Research and Public Health. 2017; 14(12):1576. https://doi.org/10.3390/ijerph14121576
Chicago/Turabian StyleLeonardi, Alberto, Laura Penta, Marta Cofini, Lucia Lanciotti, Nicola Principi, and Susanna Esposito. 2017. "Pericardial Effusion as a Presenting Symptom of Hashimoto Thyroiditis: A Case Report" International Journal of Environmental Research and Public Health 14, no. 12: 1576. https://doi.org/10.3390/ijerph14121576
APA StyleLeonardi, A., Penta, L., Cofini, M., Lanciotti, L., Principi, N., & Esposito, S. (2017). Pericardial Effusion as a Presenting Symptom of Hashimoto Thyroiditis: A Case Report. International Journal of Environmental Research and Public Health, 14(12), 1576. https://doi.org/10.3390/ijerph14121576





