Beyond Disaster Preparedness: Building a Resilience-Oriented Workforce for the Future
Abstract
:1. Introduction
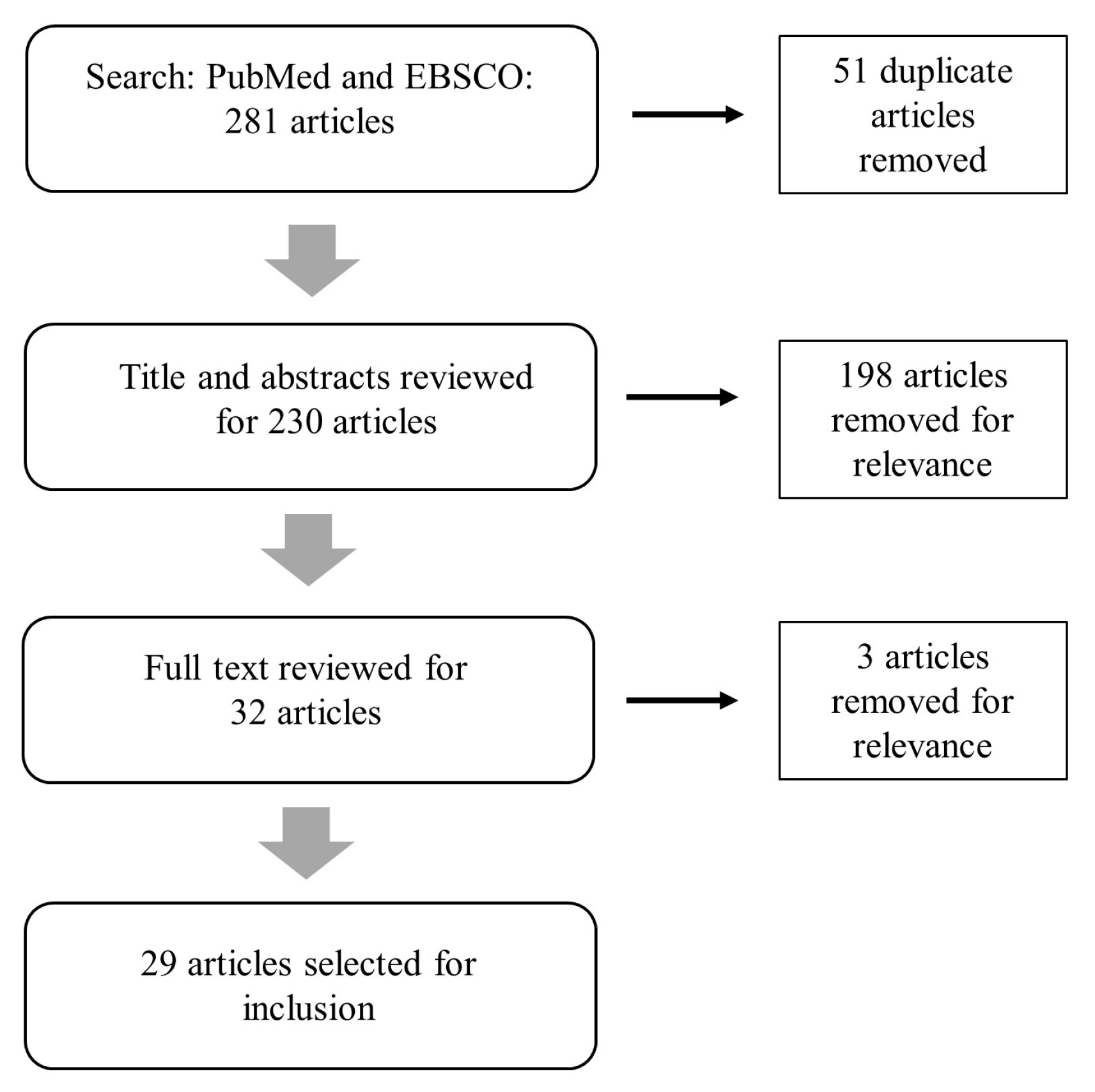
2. Materials and Methods
3. Resilience-Oriented Workforce Studies
3.1. What Organizational Structures Will Support the Connections Needed for a Resilience-Oriented Workforce?
3.2. What Elements of Training Will Support Resilience Education?
3.3. What Are Leadership Models with a Resilience Orientation?
4. Limitations to Existing Evidence
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Department of Homeland Security. Disaster Declarations. Available online: www.fema.gov/disasters (accessed on 2 November 2017).
- Keeley, B. Income Inequality: The Gap between Rich and Poor; OECD: France, Paris, 2015. [Google Scholar]
- NOAA National Centers for Environmental Information (NCEI). U.S. Billion-Dollar Weather and Climate Disasters. 2016. Available online: https://www.ncdc.noaa.gov/billions/ (accessed on 2 November 2017).
- Blair, J.P.; Schweit, K.W. A Study of Active Shooter Incidents in the United States between 2000 and 2013; US Department of Justice, Federal Bureau of Investigation: Washington, DC, USA, 2014.
- Abramson, D.M.; Grattan, L.M.; Mayer, B.; Colten, C.E.; Arosemena, F.A.; Bedimo-Rung, A.; Lichtveld, M. The resilience activation framework: A conceptual model of how access to social resources promotes adaptation and rapid recovery in post-disaster settings. J. Behav. Health Serv. Res. 2015, 42, 42–57. [Google Scholar] [CrossRef] [PubMed]
- Chandra, A.; Acosta, J.; Howard, S.; Uscher-Pines, L.; Williams, M.; Yeung, D.; Garnett, J.; Meredith, L.S. Building community resilience to disasters: A way forward to enhance national health security. Rand Health Q. 2011, 1, 6. [Google Scholar] [PubMed]
- Chandra, A.; Williams, M.; Plough, A.; Stayton, A.; Wells, K.B.; Horta, M.; Tang, J. Getting actionable about community resilience: The Los Angeles county community disaster resilience project. Am. J. Public Health 2013, 103, 1181–1189. [Google Scholar] [CrossRef] [PubMed]
- Acosta, J.; Chandra, A.; Madrigano, J. An Agenda to Advance Integrative Resilience Research and Practice; RAND Corporation: Santa Monica, CA, USA, 2017. [Google Scholar]
- U.S. Department of Homeland Security. National Disaster Recovery Framework; U.S. Department of Homeland Security: Washington, DC, USA, 2011.
- US Department of Health and Human Services. National Health Security Strategy of the United States of America; US Department of Health and Human Services: Washington, DC, USA, 2009; Volume 7.
- Centers for Disease Control and Prevention. Public Health Preparedness Capabilities: National Standards for State and Local Planning; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2011.
- United States Department of Housing and Urban Development. National Disaster Resilience Competition. Available online: http://portal.hud.gov/hudportal/documents/huddoc?id=NDRCFactSheetFINAL.pdf (accessed on 3 October 2016).
- Rockefeller Foundation. 100 Resilient Cities. Available online: http://www.100resilientcities.org (accessed on 3 October 2016).
- Ottoson, J.M.; Green, L.W.; Beery, W.L.; Senter, S.K.; Cahill, C.L.; Pearson, D.C.; Greenwald, H.P.; Hamre, R.; Leviton, L. Policy-contribution assessment and field-building analysis of the robert wood johnson foundation’s active living research program. Am. J. Prev. Med. 2009, 36, S34–S43. [Google Scholar] [CrossRef] [PubMed]
- Coaffee, J. Towards next-generation urban resilience in planning practice: From securitization to integrated place making. Plan. Pract. Res. 2013, 28, 323–339. [Google Scholar] [CrossRef]
- Graham, H. Building an inter-disciplinary science of health inequalities: The example of lifecourse research. Soc. Sci. Med. 2002, 55, 2005–2016. [Google Scholar] [CrossRef]
- Harriss, J. The case for cross-disciplinary approaches in international development. World Dev. 2002, 30, 487–496. [Google Scholar] [CrossRef]
- Ernstson, H.; van der Leeuw, S.E.; Redman, C.L.; Meffert, D.J.; Davis, G.; Alfsen, C.; Elmqvist, T. Urban transitions: On urban resilience and human-dominated ecosystems. AMBIO J. Hum. Environ. 2010, 39, 531–545. [Google Scholar] [CrossRef]
- Harvard Transdisciplinary Research in Energetics and Cancer Center. Available online: https://www.hsph.harvard.edu/trec/about-us/definitions/ (accessed on 4 December 2017).
- Kennedy, V.C.; Moore, F.I. A systems approach to public health workforce development. J. Public Health Manag. Pract. 2001, 7, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Handler, A.; Issel, M.; Turnock, B. A conceptual framework to measure performance of the public health system. Am. J. Public Health 2001, 91, 1235–1239. [Google Scholar] [CrossRef] [PubMed]
- Dawes, S.S.; Cresswell, A.M.; Cahan, B.B. Learning from crisis. Soc. Sci. Comput. Rev. 2004, 22, 52–66. [Google Scholar] [CrossRef]
- Sprang, G.; Silman, M. Using professional organizations to prepare the behavioral health workforce to respond to the needs of pediatric populations impacted by health-related disasters: Guiding principles and challenges. Disaster Med. Public Health Prep. 2015, 9, 642–649. [Google Scholar] [CrossRef] [PubMed]
- Katz, A.; Staiti, A.B.; McKenzie, K.B. Preparing for the unknown, responding to the known: Communities and public health preparedness. Health Aff. 2006, 25, 946–957. [Google Scholar] [CrossRef] [PubMed]
- Slack, M.K.; McEwen, M.M. Perceived impact of an interprofessional education program on community resilience: An exploratory study. J. Interprof. Care 2013, 27, 408–412. [Google Scholar] [CrossRef] [PubMed]
- Dunlop, A.L.; Logue, K.M.; Vaidyanathan, L.; Isakov, A.P. Facilitators and barriers for effective academic-community collaboration for disaster preparedness and response. J. Public Health Manag. Pract. 2016, 22, E20–E28. [Google Scholar] [CrossRef] [PubMed]
- Phillips, S.J. The national library of medicine’s disaster information management research center. Front. Public Health 2013, 1, 70. [Google Scholar] [CrossRef] [PubMed]
- DesVignes-Kendrick, M.; Matthews, G.W.; Steeg, S.K.; Zinder, S.F. The private bar: A force for public health. J. Law Med. Ethics 2005, 33, 77–78. [Google Scholar] [PubMed]
- Santos, J.R.; Herrera, L.C.; Yu, K.D.; Pagsuyoin, S.A.; Tan, R.R. State of the art in risk analysis of workforce criticality influencing disaster preparedness for interdependent systems. Risk Anal. Off. Publ. Soc. Risk Anal. 2014, 34, 1056–1068. [Google Scholar] [CrossRef] [PubMed]
- Black, J.; Morris, T.; Harbert, A.; Mathias, C. Educational collaboration in psychiatric disability, rehabilitation, and recovery: Developing transformative solutions. J. Soc. Work Disabil. Rehabil. 2008, 7, 163–186. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Framework for Action on Interprofessional Education & Collaborative Practice; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- Veenema, T.G. Expanding educational opportunities in disaster response and emergency preparedness for nurses. Nurs. Educ. Perspect. 2006, 27, 93–99. [Google Scholar] [PubMed]
- Potter, M.A.; Miner, K.R.; Barnett, D.J.; Cadigan, R.; Lloyd, L.; Olson, D.K.; Parker, C.; Savoia, E.; Shoaf, K. The evidence base for effectiveness of preparedness training: A retrospective analysis. Public Health Rep. 2010, 125, 15–23. [Google Scholar] [CrossRef] [PubMed]
- Morrison, A.M.; Catanzaro, A.M. High-fidelity simulation and emergency preparedness. Public Health Nurs. 2010, 27, 164–173. [Google Scholar] [CrossRef] [PubMed]
- Achora, S.; Kamanyire, J.K. Disaster preparedness: Need for inclusion in undergraduate nursing education. Sultan Qaboos Univ. Med. J. 2016, 16, e15–e19. [Google Scholar] [CrossRef] [PubMed]
- Veenema, T.G.; Griffin, A.; Gable, A.R.; MacIntyre, L.; Simons, R.N.; Couig, M.P.; Walsh, J.J., Jr.; Lavin, R.P.; Dobalian, A.; Larson, E. Nurses as leaders in disaster preparedness and response—A call to action. J. Nurs. Scholarsh. 2016, 48, 187–200. [Google Scholar] [CrossRef] [PubMed]
- Catlett, C.L.; Jenkins, J.L.; Millin, M.G. Role of emergency medical services in disaster response: Resource document for the national association of ems physicians position statement. Prehosp. Emerg. Care 2011, 15, 420–425. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Weibley, E. Disaster management and physician preparedness. South. Med. J. 2013, 106, 17–20. [Google Scholar] [CrossRef] [PubMed]
- Archer, F.; Seynaeve, G. International guidelines and standards for education and training to reduce the consequences of events that may threaten the health status of a community. A report of an open international wadem meeting, Brussels, Belgium, 29–31 October 2004. Prehosp. Disaster Med. 2007, 22, 120–130. [Google Scholar] [CrossRef] [PubMed]
- Amodeo, A.R. Commentary: Developing and retaining a public health workforce for the 21st century: Readiness for a paradigm shift to community-based public health. J. Public Health Manag. Pract. 2003, 9, 500–503. [Google Scholar] [CrossRef] [PubMed]
- Acosta, J.; Chandra, A. Harnessing a community for sustainable disaster response and recovery: An operational model for integrating nongovernmental organizations. Disaster Med. Public Health Prep. 2013, 7, 361–368. [Google Scholar] [CrossRef] [PubMed]
- Resnick, B.; Zablotsky, J.; Farrow, O.; Glotfelty, R.; Heard, P.; Kelly, S.; Mitchell, C.; Phillips, F.; Burke, T. Enhancing the maryland environmental public health workforce: A collaborative approach. J. Environ. Health 2007, 70, 32–36. [Google Scholar] [PubMed]
- Barnett, D.J.; Everly, G.S.; Parker, C.L.; Links, J.M. Applying educational gaming to public health workforce emergency preparedness. Am. J. Prev. Med. 2005, 28, 390–395. [Google Scholar] [CrossRef] [PubMed]
- Mosca, N.W.; Sweeney, P.M.; Hazy, J.M.; Brenner, P. Assessing bioterrorism and disaster preparedness training needs for school nurses. J. Public Health Manag. Pract. 2005, 11, S38–S44. [Google Scholar] [CrossRef]
- Stanley, J.M. Disaster competency development and integration in nursing education. Nurs. Clin. N. Am. 2005, 40, 453–467. [Google Scholar] [CrossRef] [PubMed]
- Davies, K.; Moran, L. Nurses need advanced skills in disaster health care. Br. J. Nurs. 2005, 14, 190. [Google Scholar] [CrossRef] [PubMed]
- Douglas, V. Developing disaster management modules: A collaborative approach. Br. J. Nurs. 2007, 16, 526–529. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, H.E.; Barnett, D.J.; Hsu, E.B.; Kirsch, T.D.; James, J.J.; Subbarao, I. Perspectives of future physicians on disaster medicine and public health preparedness: Challenges of building a capable and sustainable auxiliary medical workforce. Disaster Med. Public Health Prep. 2009, 3, 210–216. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, A.R.; Studnek, J.R.; Margolis, G.S.; Mac Crawford, J.; Bentley, M.A.; Marcozzi, D. Disaster preparedness of nationally certified emergency medical services professionals. Acad. Emerg. Med. 2011, 18, 403–412. [Google Scholar] [CrossRef] [PubMed]
- Lim, G.H.; Lim, B.L.; Vasu, A. Survey of factors affecting health care workers’ perception towards institutional and individual disaster preparedness. Prehosp. Disaster Med. 2013, 28, 353–358. [Google Scholar] [CrossRef] [PubMed]
- Fulmer, T.; Portelli, I.; Foltin, G.L.; Zimmerman, R.; Chachkes, E.; Goldfrank, L.R. Organization-based incident management: Developing a disaster volunteer role on a university campus. Disaster Manag. Response 2007, 5, 74–81. [Google Scholar] [CrossRef] [PubMed]
- Wyche, K.F.; Pfefferbaum, R.L.; Pfefferbaum, B.; Norris, F.H.; Wisnieski, D.; Younger, H. Exploring community resilience in workforce communities of first responders serving katrina survivors. Am. J. Orthopsychiatry 2011, 81, 18–30. [Google Scholar] [CrossRef] [PubMed]
| Author | Year | Discipline | Workforce Segment 1 | Workforce Segment 2 | Type of Study | Research Question(s) | Summary |
|---|---|---|---|---|---|---|---|
| Dawes et al. | 2004 | Disaster Preparedness/Response | Emergency Response | Responders | Case Study | Organization | Summarizes human and infrastructure issues post disaster: importance of data quality, usability and resource sharing among responders; discusses information policy challenges for workforce response |
| desVignes-Kendrick et al. | 2005 | Disaster Preparedness/Response | Other | Lawyers | Session abstract | Organization | Discusses the role of private lawyers in dealing with public health emergencies. |
| Katz et al. | 2006 | Disaster Preparedness/Response | Health | LHD executives, community partners, hospital executives, community health center executives | Longitudinal evaluation | Organization | Collaborative relationships developed for bioterrorism preparedness have proved useful in addressing other threats. Major ongoing challenges include funding constraints, inadequate surge capacity, public health workforce shortages, competing priorities, and jurisdictional issues. |
| Phillips | 2013 | Disaster Preparedness/Response | Other | Librarians | Review | Organization | Describes the Disaster Information Management Research Center (DIMRC) develops and provides access to health information resources and technology for disaster preparedness, response, and recovery. |
| Santos et al. | 2014 | Interdependent workforce, infrastructure, and economic systems | Other | general workforce | Review | Organization | Highlights importance of workforce sectors in formulating synergistic preparedness and recovery policies for interdependent infrastructure and regional economic systems. |
| Sprang and Silman | 2015 | Disaster Preparedness/Response | Health | Behavioral health professionals | Review/Commentary | Organization; Training | Describes five principles to integrate behavioral health services in the public health disaster response plan which use a strengths-based approach to prioritize resilience; underscore the importance of context, collaboration, and coordination; recognize the unique needs of pediatric populations; and guide ongoing training and content development in the area of biopsychosocial responses to health-related disasters. |
| Dunlop et al. | 2016 | Disaster Preparedness/Response | Health | Public health and emergency management workers, academics | Needs Assessment/Survey/Focus groups | Organization; Leadership | Explored the opinions of leaders of public health and emergency management agencies and academic institutions regarding the facilitators for and barriers to effective collaboration for disaster preparedness and response. Recognized barriers to engagement included unfamiliarity of organizational personnel, concerns about ownership of outputs resulting from the collaboration, and differences in organizational culture and modus operandi. On-going relationships through shared training of students and staff and participation in community-level partner meetings facilitated collaboration in disaster response as does having a recognizable point of contact that can comprehensively represent academic institutional resources. Legal issues were identified as both facilitators and barriers to engagement. |
| Barnett et al. | 2005 | Disaster Preparedness/Response | Health | LHD Workers | Presentation of Workforce Training Program | Training | Describes a competency-based training for public health emergency response. |
| Stanley | 2005 | Disaster Preparedness/Response | Health | Nurses | Review/Commentary | Training | Roles of key entities are essential for education’s successful implementation of disaster preparedness: education and professional organizations, accreditation and regulatory bodies, schools of nursing, and continuing education providers. |
| Davies and Moran | 2005 | Disaster Preparedness/Response | Health | Nurses | Review/Commentary | Training | Describes role of nursing workforce in disaster preparedness |
| Mosca et al. | 2005 | Disaster Preparedness/Response | Health | Nurses (school) | Needs Assessment | Training | Assessed bioterrorism and disaster preparedness needs of school nurses assessed; low confidence in preparedness capabilities across almost all categories was reported; high training need was identified across almost all competencies. |
| Veenema | 2006 | Disaster Preparedness/Response | Health | Nurses | Presentation of Workforce Training Program | Training | Workforce development and nurse preparedness for schools of nursing. |
| Archer and Seynaeve | 2007 | Disaster Preparedness/Response | Health | Health professionals | Issues Paper/Framework | Training | World Association for Disaster and Emergency Medicine (WADEM) meeting convened in support of a framework for “Disaster Health”, which included: (1) primary disciplines; (2) support disciplines; (3) community response, resilience, and communication; and (4) socio-political context. |
| Douglas | 2007 | Disaster Preparedness/Response | Health | Nurses and Paramedics | Presentation of Workforce Training Program | Training | Describes multi-agency collaborative approach to develop modules on the management of mass casualty events and incidents involving hazardous substances, offered to registered nurses and registered paramedics. |
| Fulmer et al. | 2007 | Disaster Preparedness/Response | Other | University volunteers | Survey on volunteer willingness for disaster response | Training | Survey results suggest that volunteers can and will help and that disaster preparedness drills are a logical next step for university-based volunteers. |
| Resnick et al. | 2007 | Environmental public health | Health | LHD Workers | Review | Training | Obstacles for strengthening the environmental public health workforce include recruitment shortfalls, inability to retain qualified staff, impending retirements, inadequate training opportunities, insufficient compensation, and the absence of a robust career advancement pathway. |
| Black et al. | 2008 | Mental health resiliency | Health | Social work and public mental health students | Presentation of IPE program | Training | Describes an innovative statewide collaboration between schools of social work and public mental health departments to transform social work curriculum and address the workforce crisis in public mental health service system. |
| Kaiser et al. | 2009 | Disaster Preparedness/Response | Health | Medical students | Survey/Needs Assessment | Training | Survey results indicate future physicians’ willingness to respond to disasters, but education and training in disaster medicine and public health preparedness offered in US medical schools is inadequate. |
| Morrison and Catanzaro | 2010 | Disaster Preparedness/Response | Health | Nursing students | Presentation and evaluation of training simulation exercise | Training | Describes a public health emergency simulation exercise with undergraduate senior nursing students enrolled in a public health clinical course. |
| Potter et al. | 2010 | Disaster Preparedness/Response | Health | Public health workers | Review | Training | Reviews of progress in preparedness training for the public health workforce should be repeated in the future. Governmental investment in training for preparedness should continue. Future training programs should be grounded in policy and practice needs, and evaluations should be based on performance improvement. |
| Catlett et al. | 2011 | Disaster Preparedness/Response | Health | EMS Physicians | Resource document | Training | Advocates for a strong emergency medical services (EMS) role in all phases of disaster management—preparedness, response, and recovery. |
| Fernandez et al. | 2011 | Disaster Preparedness/Response | Health | EMTs and Paramedics | Needs Assessment | Training | A majority of nationally certified EMT-Basics and paramedics reported participating in both individual and multiagency disaster-preparedness training. A large majority of respondents reported feeling adequately prepared to respond to man-made and natural disasters and the perception of preparedness correlated with hours of training. Some areas for improvement were identified. |
| Slack et al. | 2013 | Community resilience | Health | Health Science students | Evaluation of IPE program | Training | By acting as a catalyst, a community based interprofessional program can affect components of community resilience/capacity, primarily human, social, and informational capital. |
| Lim et al. | 2013 | Disaster Preparedness/Response | Health | Health care workers (Physicians, Nurses, Allied Health workers) | Survey/Needs Assessment | Training | Survey indicates that health care workers fare poorly in their perception of their individual preparedness. Identifies Important factors that might contribute to improving this perception at the individual and institution level. |
| Baack and Alfred | 2013 | Disaster Preparedness/Response | Health | Nurses (rural) | Survey/Needs Assessment | Training | Most rural nurses are not confident in their abilities to respond to major disaster events. The nurses who were confident were more likely to have had actual prior experience in disasters or shelters. |
| Kumar and Weibley | 2013 | Disaster Preparedness/Response | Health | Physicians | Review/Commentary | Training | Describes physicians’ obligations, role, education, preparation, and response for disasters. |
| Veenema et al. | 2016 | Disaster Preparedness/Response | Health | Nurses | Needs Assessment/SME interviews | Training | Describes a vision for the future of disaster nursing, and identifies current barriers and opportunities to advance professional disaster nursing. Includes recommendations for nursing practice, education, policy, and research, as well as implementation challenges. |
| Achora and Kamanyire | 2016 | Disaster Preparedness/Response | Health | Nurses | Review/Commentary | Training | Highlights the current state of nursing education and training in disaster management, both generally and in Oman. |
| Wyche et al. | 2011 | Disaster Preparedness/Response | Emergency Response | First responders | Evaluation of work place teams-survey, focus groups, interviews | Leadership | Community resilience activities were assessed in workplace teams that became first responders for Hurricane Katrina survivors. Resilient behaviors were characterized by: shared organizational identity, purpose, and values; mutual support and trust; role flexibility; active problem solving; self-reflection; shared leadership; and skill building. |
| Category | Recommendation |
|---|---|
| Improve the evidence base | Develop a core set of metrics for workforce evaluation. |
| Conduct research to determine what does and does not work (e.g., training, organizational structures, leadership models) for achieving pre-defined metrics. | |
| Develop Competencies/Training | Identify, validate, and assess a set of competencies that support a resilience-oriented workforce. |
| Develop resilience-oriented interprofessional education programs at the graduate and continuing education levels. | |
| Incorporate community-based partnerships into training programs to develp skills to work with local communities. | |
| Faciltate Organizational Structures | Use common language across fields. |
| Develop integrated organizational frameworks for doing business across human and infrastructure systems. | |
| Cultivate Leadership Models | Determine incentive structures that promote horizontal leaderships and shared identity. |
| Create career advancement opportunities that recognize interdisciplinary and intersectoral experience. | |
| Establish mechanisms of collaboration across sectors and disciplines (e.g., through regional coordination centers). |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Madrigano, J.; Chandra, A.; Costigan, T.; Acosta, J.D. Beyond Disaster Preparedness: Building a Resilience-Oriented Workforce for the Future. Int. J. Environ. Res. Public Health 2017, 14, 1563. https://doi.org/10.3390/ijerph14121563
Madrigano J, Chandra A, Costigan T, Acosta JD. Beyond Disaster Preparedness: Building a Resilience-Oriented Workforce for the Future. International Journal of Environmental Research and Public Health. 2017; 14(12):1563. https://doi.org/10.3390/ijerph14121563
Chicago/Turabian StyleMadrigano, Jaime, Anita Chandra, Tracy Costigan, and Joie D. Acosta. 2017. "Beyond Disaster Preparedness: Building a Resilience-Oriented Workforce for the Future" International Journal of Environmental Research and Public Health 14, no. 12: 1563. https://doi.org/10.3390/ijerph14121563
APA StyleMadrigano, J., Chandra, A., Costigan, T., & Acosta, J. D. (2017). Beyond Disaster Preparedness: Building a Resilience-Oriented Workforce for the Future. International Journal of Environmental Research and Public Health, 14(12), 1563. https://doi.org/10.3390/ijerph14121563




