Are Changes in Neighbourhood Perceptions Associated with Changes in Self-Rated Mental Health in Adults? A 13-Year Repeat Cross-Sectional Study, UK
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Outcome Variable—Hospital Anxiety and Depression Scale (HADS)
2.3. Independent Variables
2.4. Neighbourhood Perceptions
2.5. Statistical Analysis
- Model 1: Wave only.
- Model 2: Wave and neighbourhood perceptions; crime and disorder, neighbourhood reputation and physical environmental problems.
- Model 3: Identical to model 2 plus individual-level variables sex, age, employment status, health status, LLSI and social class included.
- Model 4: Identical to model 3 plus housing tenure and contextual variables, urban/rural classification included.
- Model 5: Identical to model 4 plus access to car at household included.
- Model 6 (presented in Table 3): Identical structure to model 5 plus interactions by wave and neighbourhood perceptions.
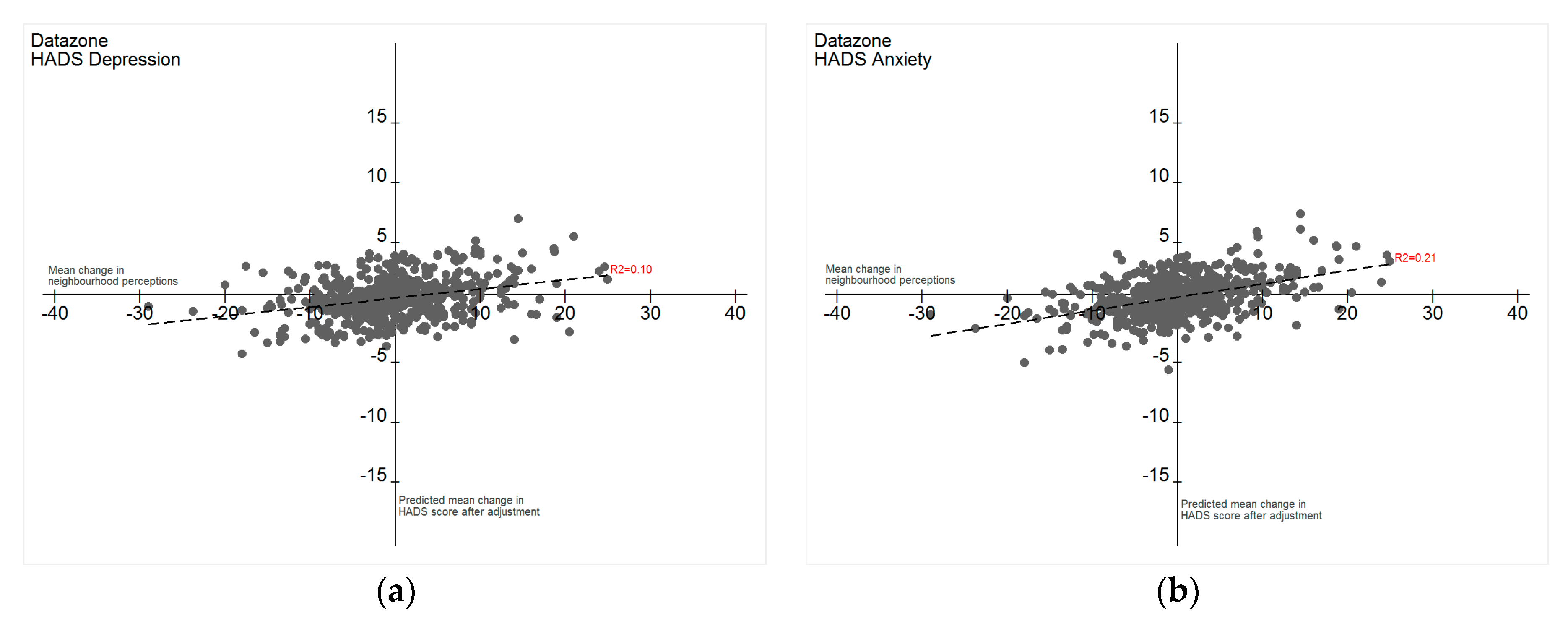
2.6. Change in Neighbourhood Perceptions and HADS over Time
3. Results
3.1. Participant Characteristics
3.2. Depression
3.3. Anxiety
3.4. Overall Change in Neighbourhood Perceptions, and Anxiety and Depression Scores, by Socio-Economic Status
4. Discussion
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
Data Sharing Statement
References
- Kim, D. Blues from the neighborhood? Neighborhood characteristics and depression. Epidemiol. Rev. 2008, 30, 101–117. [Google Scholar] [CrossRef] [PubMed]
- Leslie, E.; Cerin, E. Are perceptions of the local environment related to neighbourhood satisfaction and mental health in adults? Prev. Med. 2008, 47, 273–278. [Google Scholar] [CrossRef] [PubMed]
- Ellaway, A.; Morris, G.; Curtice, J.; Robertson, C.; Allardice, G.; Robertson, R. Associations between health and different types of environmental incivility: A scotland-wide study. Public Health 2009, 123, 708–713. [Google Scholar] [CrossRef] [PubMed]
- Gong, Y.; Palmer, S.; Gallacher, J.; Marsden, T.; Fone, D. A systematic review of the relationship between objective measurements of the urban environment and psychological distress. Environ. Int. 2016, 96, 48–57. [Google Scholar] [CrossRef] [PubMed]
- Chisholm, D.; Sweeny, K.; Sheehan, P.; Rasmussen, B.; Smit, F.; Cuijpers, P.; Saxena, S. Scaling-up treatment of depression and anxiety: A global return on investment analysis. Lancet Psychiatry 2016, 3, 415–424. [Google Scholar] [CrossRef]
- World Health Organisation. Promoting Mental Health: Concepts, Emerging Evidence, Practice: Summary Report; WHO: Geneva, Switzerland, 2004. [Google Scholar]
- Feijten, P.; Van Ham, M. Neighbourhood change. Reason to leave? Urban Stud. 2009, 46, 2103–2122. [Google Scholar] [CrossRef]
- Hedman, L.; Van Ham, M.; Manley, D. Neighbourhood choice and neighbourhood reproduction. Environ. Plan. A 2011, 43, 1381–1399. [Google Scholar] [CrossRef]
- Gose, M.; Plachta-Danielzik, S.; Willié, B.; Johannsen, M.; Landsberg, B.; Müller, M.J. Longitudinal influences of neighbourhood built and social environment on children’s weight status. Int. J. Environ. Res. Public Health 2013, 10, 5083–5096. [Google Scholar] [CrossRef] [PubMed]
- Pampalon, R.; Hamel, D.; De Koninck, M.; Disant, M.-J. Perception of place and health: Differences between neighbourhoods in the quebec city region. Soc. Sci. Med. 2007, 65, 95–111. [Google Scholar] [CrossRef] [PubMed]
- McAneney, H.; Tully, M.A.; Hunter, R.F.; Kouvonen, A.; Veal, P.; Stevenson, M.; Kee, F. Individual factors and perceived community characteristics in relation to mental health and mental well-being. BMC Public Health 2015, 15, 1237. [Google Scholar] [CrossRef] [PubMed]
- Robinette, J.W.; Charles, S.T.; Gruenewald, T.L. Vigilance at home: Longitudinal analyses of neighborhood safety perceptions and health. SSM Popul. Health 2016, 2, 525–530. [Google Scholar] [CrossRef] [PubMed]
- Haynes, R.; Daras, K.; Reading, R.; Jones, A. Modifiable neighbourhood units, zone design and residents’ perceptions. Health Place 2007, 13, 812–825. [Google Scholar] [CrossRef] [PubMed]
- Macintyre, S.; Ellaway, A.; Hiscock, R.; Kearns, A.; Der, G.; McKay, L. What features of the home and the area might help to explain observed relationships between housing tenure and health? Evidence from the west of scotland. Health Place 2003, 9, 207–218. [Google Scholar] [CrossRef]
- Olsen, J.R.; Macdonald, L.; Ellaway, A. Changes over time in population level transport satisfaction and mode of travel: A 13 year repeat cross-sectional study, UK. J. Transp. Health 2017, 6, 366–378. [Google Scholar] [CrossRef] [PubMed]
- Sedgwick, P. Bias in observational study designs: Cross sectional studies. BMJ 2015, 350, h1286. [Google Scholar] [CrossRef] [PubMed]
- CACI. A Classification of Residential Neighbourhoods. Available online: http://acorn.caci.co.uk (accessed on 9 August 2016).
- Dillman, D. Mail and Telephone Surveys; the Total Design Method; John Wiley: New York, NY, USA, 1978. [Google Scholar]
- Audit Scotland. Health Inequalities in Scotland; Audit Scotland: Edinburgh, UK, 2012.
- National Records of Scotland: Population Estimates for Scotland, Mid-2002 to Mid-2010. Available online: https://www.nrscotland.gov.uk/statistics-and-data/statistics/statistics-by-theme/population/population-estimates/mid-year-population-estimates/mid-2002-to-mid-2010-revision (accessed on 27 January 2017).
- Scottish Goverment. Scottish Household Survey. Available online: http://www.gov.scot/Topics/Statistics/16002 (accessed on 5 January 2016).
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Norton, S.; Cosco, T.; Doyle, F.; Done, J.; Sacker, A. The hospital anxiety and depression scale: A meta confirmatory factor analysis. J. Psychosom. Res. 2013, 74, 74–81. [Google Scholar] [CrossRef] [PubMed]
- Stern, A.F. The hospital anxiety and depression scale. Occup. Med. 2014, 64, 393–394. [Google Scholar] [CrossRef] [PubMed]
- Li, C. Little’s test of missing completely at random. Stata J. 2013, 13, 795–809. [Google Scholar]
- Office of Population Censuses and Surveys. Opcs Standard Occupational Classification; HMSO: London, UK, 1991.
- Scottish Government. Scottish Government Urban Rural Classification. Available online: http://www.gov.scot/Topics/Statistics/About/Methodology/UrbanRuralClassification (accessed on 29 June 2016).
- Scottish Government. Simd: Background and Methodology. Available online: http://www.gov.scot/Topics/Statistics/SIMD/BackgroundMethodology (accessed on 31 March 2016).
- Tabak, R.; Hipp, J.A.; Dodson, E.A.; Yang, L.; Adlakha, D.; Brownson, R.C. Exploring associations between perceived home and work neighborhood environments, diet behaviors, and obesity: Results from a survey of employed adults in missouri. Prev. Med. Rep. 2016, 4, 591–596. [Google Scholar] [CrossRef] [PubMed]
- Foster, S.; Hooper, P.; Knuiman, M.; Christian, H.; Bull, F.; Giles-Corti, B. Safe residential environments? A longitudinal analysis of the influence of crime-related safety on walking. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 22. [Google Scholar] [CrossRef] [PubMed]
- Ellaway, A.; Macintyre, S. Are perceived neighbourhood problems associated with the likelihood of smoking? J. Epidemiol. Community Health 2009, 63, 78–80. [Google Scholar] [CrossRef] [PubMed]
- Low, C.T.; Lai, P.C.; Li, H.D.; Ho, W.K.; Wong, P.; Chen, S.; Wong, W.C. Neighbourhood effects on body constitution–a case study of Hong Kong. Soc. Sci. Med. 2016, 158, 61–74. [Google Scholar] [CrossRef] [PubMed]
- Gobbens, R.J.; van Assen, M.A. Associations of environmental factors with quality of life in older adults. Gerontologist 2017, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Mackenbach, J.D.; Lakerveld, J.; van Oostveen, Y.; Compernolle, S.; De Bourdeaudhuij, I.; Bárdos, H.; Rutter, H.; Glonti, K.; Oppert, J.-M.; Charreire, H. The mediating role of social capital in the association between neighbourhood income inequality and body mass index. Eur. J. Public Health 2017, 27, 218–223. [Google Scholar] [CrossRef] [PubMed]
- National Records of Scotland. Geography—Background Information—Postcodes. Available online: https://www.nrscotland.gov.uk/files/geography/Products/postcode-bkgrd-info.pdf (accessed on 12 May 2017).
- Scottish Goverment. Scottish Neighbourhood Statistics Guide: Scotland’s Statistical Geography. Available online: http://www.gov.scot/Publications/2005/02/20697/52626 (accessed on 12 May 2017).
- Mair, C.F.; Roux, A.V.D.; Galea, S. Are neighborhood characteristics associated with depressive symptoms? A critical review. J. Epidemiol. Community Health 2008, 62, 940–946. [Google Scholar] [CrossRef] [PubMed]
- Lofors, J.; Ramírez-León, V.; Sundquist, K. Neighbourhood income and anxiety: A study based on random samples of the swedish population. Eur. J. Public Health 2006, 16, 633–639. [Google Scholar] [CrossRef] [PubMed]
- Pearce, J.; Shortt, N.; Rind, E.; Mitchell, R. Life course, green space and health: Incorporating place into life course epidemiology. Int. J. Environ. Res. Public Health 2016, 13, 331. [Google Scholar] [CrossRef] [PubMed]
- Polling, C.; Khondoker, M.; Hatch, S.; Hotopf, M.; Team, S.S. Influence of perceived and actual neighbourhood disorder on common mental illness. Soc. Psychiatry Psychiatr. Epidemiol. 2014, 49, 889–901. [Google Scholar] [CrossRef] [PubMed]
- Leventhal, T.; Brooks-Gunn, J. Moving to opportunity: An experimental study of neighborhood effects on mental health. Am. J. Public Health 2003, 93, 1576–1582. [Google Scholar] [CrossRef] [PubMed]
- Robinette, J.W.; Charles, S.T.; Gruenewald, T.L. Neighborhood socioeconomic status and health: A longitudinal analysis. J. Commun. Health 2017, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Fone, D.; White, J.; Farewell, D.; Kelly, M.; John, G.; Lloyd, K.; Williams, G.; Dunstan, F. Effect of neighbourhood deprivation and social cohesion on mental health inequality: A multilevel population-based longitudinal study. Psychol. Med. 2014, 44, 2449–2460. [Google Scholar] [CrossRef] [PubMed]
- D’Haese, S.; Cardon, G.; De Bourdeaudhuij, I.; Deforche, B.; De Meester, F.; Van Dyck, D. Changes in individual and social environmental characteristics in relation to changes in physical activity: A longitudinal study from primary to secondary school. Int. J. Behav. Med. 2016, 23, 539–552. [Google Scholar] [CrossRef] [PubMed]
- Macintyre, S.; Macdonald, L.; Ellaway, A. Do poorer people have poorer access to local resources and facilities? The distribution of local resources by area deprivation in Glasgow, Scotland. Soc. Sci. Med. 2008, 67, 900–914. [Google Scholar] [CrossRef] [PubMed]
- O’Campo, P.; Wheaton, B.; Nisenbaum, R.; Glazier, R.H.; Dunn, J.R.; Chambers, C. The neighbourhood effects on health and well-being (NEHW) study. Health Place 2015, 31, 65–74. [Google Scholar] [CrossRef] [PubMed]
- Sedgwick, P. Cross sectional studies: Advantages and disadvantages. BMJ 2014, 348. [Google Scholar] [CrossRef]
- Cherrie, M.P.; Shortt, N.K.; Mitchell, R.J.; Taylor, A.M.; Redmond, P.; Thompson, C.W.; Starr, J.M.; Deary, I.J.; Pearce, J.R. Green space and cognitive ageing: A retrospective life course analysis in the lothian birth cohort 1936. Soc. Sci. Med. 2017. [Google Scholar] [CrossRef] [PubMed]
- Haynes, R.; Jones, A.P.; Reading, R.; Daras, K.; Emond, A. Neighbourhood variations in child accidents and related child and maternal characteristics: Does area definition make a difference? Health Place 2008, 14, 693–701. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, R. Multilevel modeling might not be the answer. Environ. Plan. A 2001, 33, 1357–1360. [Google Scholar]
- Macintyre, S.; Ellaway, A.; Cummins, S. Place effects on health: How can we conceptualise, operationalise and measure them? Soc. Sci. Med. 2002, 55, 125–139. [Google Scholar] [CrossRef]
| Variable | THAW I (N = 2388) | THAW II (N = 2092) | ||
|---|---|---|---|---|
| N | % | N | % | |
| Sex | ||||
| Male | 985 | 41.39 | 911 | 43.55 |
| Female | 1395 | 58.61 | 1181 | 56.45 |
| Age | ||||
| 17 to 24 | 95 | 3.98 | 112 | 5.35 |
| 25 to 44 | 859 | 35.97 | 504 | 24.09 |
| 45 to 64 | 788 | 33.00 | 943 | 45.08 |
| 65-plus | 646 | 27.05 | 533 | 25.48 |
| Urban/Rural Classification | ||||
| Large Urban Areas | 1567 | 65.62 | 1204 | 59.49 |
| Other Urban Areas | 594 | 24.87 | 539 | 26.63 |
| Accessible Small Towns | 147 | 6.16 | 175 | 8.65 |
| Accessible Rural | 74 | 3.10 | 92 | 4.55 |
| Remote Rural | 6 | 0.25 | 14 | 0.69 |
| Social Class | ||||
| I/II Professional, managerial and technical | 601 | 32.70 | 820 | 44.10 |
| III Skilled | 531 | 28.90 | 737 | 39.60 |
| IV/V Partly skilled and unskilled | 705 | 38.40 | 302 | 16.30 |
| Employment | ||||
| Employed or student | 1139 | 57.50 | 1186 | 62.13 |
| Unemployed | 129 | 6.50 | 100 | 5.24 |
| Retired | 712 | 36.00 | 623 | 32.63 |
| Housing Tenure | ||||
| Owner occupied | 1478 | 64.32 | 1711 | 83.22 |
| Private Renter | 47 | 2.05 | 60 | 2.92 |
| Social Renter | 773 | 33.64 | 285 | 13.86 |
| Car Access at Household | ||||
| Access | 1452 | 64.10 | 1697 | 81.50 |
| No Access | 813 | 35.90 | 384 | 18.50 |
| Health Status | ||||
| Excellent/Good | 1410 | 59.05 | 1444 | 69.02 |
| Fair/Poor | 978 | 40.95 | 648 | 30.98 |
| LLSI | ||||
| Has LLSI | 1133 | 47.45 | 956 | 45.70 |
| No LLSI | 1255 | 52.55 | 1136 | 54.30 |
| HADS Depression | ||||
| Mean (sd 1) | Median (IQR 2) | Mean (sd 1) | Median (IQR 2) | |
| 4.9 (3.8) | 4 (2–7) | 4.2 (3.8) | 3 (1–6) | |
| HADS Anxiety | ||||
| Mean (sd 1) | Median (IQR 2) | Mean (sd 1) | Median (IQR 2) | |
| 7.1 (4.0) | 7 (4–9) | 6.6 (4.1) | 6 (3–9) | |
| Neighbourhood Perceptions Scale | ||||
| Mean (sd 1) | Median (IQR 2) | Mean (sd 1) | Median (IQR 2) | |
| 9.5 (7.5) | 8 (4–13) | 8.0 (7.0) | 6 (3–11) | |
| (a) | ||||||||||||||||||||
| HADS Depression | Model 1: Wave Only | Model 2: Wave and Neighbourhood Perceptions | Model 3: Model 2 + Individual Variables | Model 4: Model 3 + Contextual Variables | Model 5: Model 4 + Car Access | |||||||||||||||
| Coef | p | LL 95% CI | UL 95% CI | Coef | p | LL 95% CI | UL 95% CI | Coef | p | LL 95% CI | UL 95% CI | Coef | p | LL 95% CI | UL 95% CI | Coef | p | LL 95% CI | UL 95% CI | |
| Sex | ||||||||||||||||||||
| Male | REF | REF | REF | |||||||||||||||||
| Female | 0.11 | 0.31 | −0.10 | 0.32 | 0.13 | 0.23 | −0.08 | 0.34 | 0.12 | 0.28 | −0.09 | 0.33 | ||||||||
| Age | ||||||||||||||||||||
| 17 to 24 | REF | REF | REF | |||||||||||||||||
| 25 to 44 | 0.56 | 0.02 | 0.08 | 1.04 | 0.57 | 0.02 | 0.09 | 1.06 | 0.59 | 0.02 | 0.10 | 1.07 | ||||||||
| 45 to 64 | 0.66 | 0.01 | 0.18 | 1.15 | 0.66 | 0.01 | 0.17 | 1.15 | 0.67 | 0.01 | 0.18 | 1.16 | ||||||||
| 65-plus | 0.64 | 0.04 | 0.02 | 1.27 | 0.68 | 0.04 | 0.05 | 1.31 | 0.64 | 0.05 | 0.00 | 1.27 | ||||||||
| Employment | ||||||||||||||||||||
| Employed or Student | REF | REF | REF | |||||||||||||||||
| Unemployed | 1.32 | <0.001 | 0.85 | 1.79 | 1.22 | 0.00 | 0.74 | 1.70 | 1.22 | <0.001 | 0.73 | 1.71 | ||||||||
| Retired | −0.05 | 0.79 | −0.45 | 0.35 | −0.11 | 0.59 | −0.52 | 0.29 | −0.13 | 0.52 | −0.54 | 0.27 | ||||||||
| Health status | ||||||||||||||||||||
| Excellent/Good | REF | REF | REF | |||||||||||||||||
| Fair/Poor | 2.43 | <0.001 | 2.17 | 2.68 | 2.35 | 0.00 | 2.08 | 2.61 | 2.31 | <0.001 | 2.05 | 2.57 | ||||||||
| LLSI | ||||||||||||||||||||
| Has LLSI | REF | REF | REF | |||||||||||||||||
| No LLSI | −0.51 | <0.001 | −0.74 | −0.27 | −0.53 | 0.00 | −0.77 | −0.29 | −0.54 | <0.001 | −0.78 | −0.29 | ||||||||
| Social class | ||||||||||||||||||||
| I/II Professional, Managerial and Technical | REF | REF | REF | |||||||||||||||||
| III Skilled | 0.36 | <0.001 | 0.12 | 0.60 | 0.38 | <0.001 | 0.14 | 0.62 | 0.37 | <0.001 | 0.13 | 0.62 | ||||||||
| IV/V Partly Skilled and Unskilled | 0.16 | 0.24 | −0.11 | 0.44 | 0.15 | 0.30 | −0.13 | 0.43 | 0.12 | 0.41 | −0.17 | 0.41 | ||||||||
| Urban/rural classification | ||||||||||||||||||||
| Large Urban Areas | REF | REF | ||||||||||||||||||
| Other Urban Areas | 0.06 | 0.64 | −0.19 | 0.31 | 0.05 | 0.71 | −0.21 | 0.30 | ||||||||||||
| Accessible Small Towns | −0.03 | 0.87 | −0.45 | 0.38 | 0.00 | 1.00 | −0.42 | 0.42 | ||||||||||||
| Accessible Rural | 0.27 | 0.38 | −0.33 | 0.88 | 0.31 | 0.32 | −0.30 | 0.92 | ||||||||||||
| Remote Rural | −0.01 | 0.99 | −1.57 | 1.56 | 0.02 | 0.98 | −1.55 | 1.59 | ||||||||||||
| Housing Tenure | ||||||||||||||||||||
| Owner Occupied | REF | REF | ||||||||||||||||||
| Private Renter | −1.20 | <0.001 | −1.89 | −0.52 | −1.31 | <0.001 | −2.00 | −0.61 | ||||||||||||
| Social Renter | 0.33 | 0.05 | 0.01 | 0.66 | 0.24 | 0.17 | −0.10 | 0.58 | ||||||||||||
| Car access at household | ||||||||||||||||||||
| Access | REF | |||||||||||||||||||
| No Access | −0.28 | 0.07 | −0.58 | 0.02 | ||||||||||||||||
| Neighbourhood perceptions | ||||||||||||||||||||
| Crime and Disorder | 0.03 | 0.32 | −0.03 | 0.08 | −0.03 | 0.29 | −0.08 | 0.02 | −0.03 | 0.33 | −0.08 | 0.03 | −0.03 | 0.34 | −0.08 | 0.03 | ||||
| Social Environment | 0.27 | <0.001 | 0.21 | 0.34 | 0.15 | <0.001 | 0.08 | 0.21 | 0.14 | <0.001 | 0.08 | 0.21 | 0.14 | <0.001 | 0.08 | 0.21 | ||||
| Physical Environmental Problems | 0.13 | <0.001 | 0.08 | 0.19 | 0.11 | <0.001 | 0.06 | 0.16 | 0.10 | <0.001 | 0.05 | 0.15 | 0.10 | <0.001 | 0.04 | 0.15 | ||||
| THAW wave | ||||||||||||||||||||
| Wave 1 | REF | REF | REF | REF | REF | |||||||||||||||
| Wave 2 | −0.62 | <0.001 | −0.84 | −0.39 | −0.50 | <0.001 | −0.72 | −0.28 | −0.27 | 0.02 | −0.48 | −0.05 | −0.25 | 0.03 | −0.47 | −0.03 | −0.24 | 0.04 | −0.46 | −0.02 |
| Cons | 4.87 | <0.001 | 4.70 | 5.03 | 3.80 | <0.001 | 3.58 | 4.02 | 2.37 | 0.00 | 1.80 | 2.94 | 2.37 | <0.001 | 1.79 | 2.95 | 2.65 | <0.001 | 2.00 | 3.30 |
| Variance | ICC | S.Err. | LL 95% CI | UL 95% CI | ICC | S.Err. | LL 95% CI | UL 95% CI | ICC | S.Err. | LL 95% CI | UL 95% CI | ICC | S.Err. | LL 95% CI | UL 95% CI | ICC | S.Err. | LL 95% CI | UL 95% CI |
| Level 3: datazone | 5.1% | 0.29 | 0.16 | 1.29 | 3.0% | 0.25 | −0.10 | 0.89 | 3.5% | 0.19 | −0.08 | 0.68 | 3.6% | 0.19 | −0.08 | 0.68 | 3.8% | 0.19 | −0.06 | 0.70 |
| Level 2: postcode | 5.7% | 0.37 | 0.09 | 1.53 | 3.8% | 0.33 | −0.15 | 1.15 | 0.5% | 0.25 | −0.44 | 0.53 | 0.0% | 0.25 | −0.49 | 0.49 | 0.0% | 0.25 | −0.49 | 0.49 |
| Level 1: ID | 89.3% | 0.36 | 12.04 | 13.44 | 93.3% | 0.34 | 11.73 | 13.08 | 96.0% | 0.26 | 7.65 | 8.68 | 96.4% | 0.27 | 7.60 | 8.66 | 96.2% | 0.27 | 7.58 | 8.63 |
| (b) | ||||||||||||||||||||
| HADS depression | Model 1: Wave only | Model 2: Wave and neighbourhood perceptions | Model 3: Model 2 + Individual variables | Model 4: Model 3 + contextual variables | Model 5: Model 4 + car access | |||||||||||||||
| Coef | p | LL 95% CI | UL 95% CI | Coef | p | LL 95% CI | UL 95% CI | Coef | p | LL 95% CI | UL 95% CI | Coef | p | LL 95% CI | UL 95% CI | Coef | p | LL 95% CI | UL 95% CI | |
| Sex | ||||||||||||||||||||
| Male | REF | REF | REF | |||||||||||||||||
| Female | 1.17 | 0.00 | 0.92 | 1.42 | 1.19 | 0.00 | 0.94 | 1.45 | 1.19 | 0.00 | 0.94 | 1.44 | ||||||||
| Age | ||||||||||||||||||||
| 17 to 24 | REF | REF | REF | |||||||||||||||||
| 25 to 44 | −0.11 | 0.69 | −0.68 | 0.45 | −0.15 | 0.62 | −0.72 | 0.43 | −0.13 | 0.66 | −0.70 | 0.45 | ||||||||
| 45 to 64 | −0.79 | 0.01 | −1.36 | −0.22 | −0.82 | 0.01 | −1.40 | −0.24 | −0.81 | 0.01 | −1.39 | −0.23 | ||||||||
| 65-plus | −1.94 | 0.00 | −2.69 | −1.20 | −1.89 | 0.00 | −2.64 | −1.14 | −1.88 | 0.00 | −2.63 | −1.12 | ||||||||
| Employment | ||||||||||||||||||||
| Employed or Student | REF | REF | REF | |||||||||||||||||
| Unemployed | 0.68 | 0.02 | 0.12 | 1.24 | 0.68 | 0.02 | 0.10 | 1.26 | 0.69 | 0.02 | 0.10 | 1.28 | ||||||||
| Retired | −0.15 | 0.54 | −0.62 | 0.32 | −0.22 | 0.36 | −0.70 | 0.26 | −0.25 | 0.30 | −0.74 | 0.23 | ||||||||
| Health status | ||||||||||||||||||||
| Excellent/Good | REF | REF | REF | |||||||||||||||||
| Fair/Poor | 1.78 | 0.00 | 1.47 | 2.09 | 1.75 | 0.00 | 1.43 | 2.06 | 1.72 | 0.00 | 1.40 | 2.03 | ||||||||
| LLSI | ||||||||||||||||||||
| Has LLSI | REF | REF | REF | |||||||||||||||||
| No LLSI | −0.32 | 0.03 | −0.60 | −0.03 | −0.33 | 0.03 | −0.62 | −0.04 | −0.34 | 0.02 | −0.63 | −0.05 | ||||||||
| Social class | ||||||||||||||||||||
| I/II Professional, Managerial and Technical | REF | REF | REF | |||||||||||||||||
| III Skilled | 0.05 | 0.73 | −0.23 | 0.33 | 0.07 | 0.66 | −0.22 | 0.35 | 0.07 | 0.64 | −0.22 | 0.36 | ||||||||
| IV/V Partly Skilled and Unskilled | 0.18 | 0.29 | −0.15 | 0.50 | 0.15 | 0.37 | −0.18 | 0.49 | 0.14 | 0.43 | −0.20 | 0.48 | ||||||||
| Urban/rural classification | ||||||||||||||||||||
| Large Urban Areas | REF | REF | ||||||||||||||||||
| Other Urban Areas | 0.21 | 0.17 | −0.09 | 0.51 | 0.20 | 0.19 | −0.10 | 0.50 | ||||||||||||
| Accessible Small Towns | −0.10 | 0.68 | −0.59 | 0.39 | −0.09 | 0.72 | −0.58 | 0.40 | ||||||||||||
| Accessible Rural | 0.21 | 0.57 | −0.51 | 0.92 | 0.23 | 0.54 | −0.49 | 0.94 | ||||||||||||
| Remote Rural | −0.76 | 0.40 | −2.54 | 1.01 | −0.74 | 0.41 | −2.52 | 1.03 | ||||||||||||
| Housing Tenure | ||||||||||||||||||||
| Owner Occupied | REF | REF | ||||||||||||||||||
| Private Renter | −0.93 | 0.03 | −1.75 | −0.12 | −1.00 | 0.02 | −1.83 | −0.18 | ||||||||||||
| Social Renter | 0.05 | 0.82 | −0.34 | 0.43 | 0.01 | 0.97 | −0.39 | 0.41 | ||||||||||||
| Car access at household | ||||||||||||||||||||
| Access | REF | |||||||||||||||||||
| No Access | −0.18 | 0.34 | −0.53 | 0.18 | ||||||||||||||||
| Neighbourhood perceptions | ||||||||||||||||||||
| Crime and Disorder | 0.10 | 0.00 | 0.04 | 0.16 | 0.07 | 0.04 | 0.00 | 0.13 | 0.07 | 0.04 | 0.00 | 0.13 | 0.07 | 0.04 | 0.00 | 0.13 | ||||
| Social Environment | 0.26 | 0.00 | 0.19 | 0.33 | 0.11 | 0.01 | 0.03 | 0.18 | 0.10 | 0.01 | 0.02 | 0.18 | 0.11 | 0.01 | 0.03 | 0.19 | ||||
| Physical Environmental Problems | 0.14 | 0.00 | 0.08 | 0.19 | 0.14 | 0.00 | 0.08 | 0.21 | 0.14 | 0.00 | 0.08 | 0.21 | 0.13 | 0.00 | 0.07 | 0.20 | ||||
| THAW wave | ||||||||||||||||||||
| Wave 1 | REF | REF | REF | REF | REF | |||||||||||||||
| Wave 2 | −0.48 | 0.00 | −0.73 | −0.24 | −0.30 | 0.01 | −0.53 | −0.06 | −0.01 | 0.93 | −0.27 | 0.24 | −0.02 | 0.86 | −0.29 | 0.24 | −0.02 | 0.87 | −0.28 | 0.24 |
| Cons | 7.08 | 0.00 | 6.91 | 7.25 | 5.75 | 0.00 | 5.51 | 5.98 | 5.41 | 0.00 | 4.73 | 6.08 | 5.42 | 0.00 | 4.73 | 6.11 | 5.59 | 0.00 | 4.81 | 6.37 |
| Variance | ICC | Std. Err. | LL 95% CI | UL 95% CI | ICC | Std. Err. | LL 95% CI | UL 95% CI | ICC | Std. Err. | LL 95% CI | UL 95% CI | ICC | Std. Err. | LL 95% CI | UL 95% CI | ICC | Std. Err. | LL 95% CI | UL 95% CI |
| Level 3: datazone | 2.7% | 0.30 | −0.14 | 1.03 | 1.6% | 0.26 | −0.27 | 0.75 | 2.5% | 0.18 | −0.06 | 0.65 | 2.3% | 0.19 | −0.90 | 0.64 | 2.3% | 0.28 | −0.26 | 0.83 |
| Level 2: postcode | 1.8% | 0.39 | −0.48 | 1.05 | 0.4% | 0.34 | −0.61 | 0.74 | 0.0% | 0.00 | 0.00 | 0.00 | 0.0% | 0.00 | 0.00 | 0.00 | 0.0% | 0.00 | 0.00 | 0.00 |
| Level 1: ID | 95.5% | 0.42 | 14.68 | 16.34 | 98.0% | 0.39 | 13.90 | 15.43 | 97.5% | 0.34 | 11.01 | 12.33 | 97.7% | 0.34 | 11.01 | 12.36 | 97.2% | 0.39 | 10.86 | 12.37 |
| Interactions over Time (1997 to 2010) | HADS Depression | HADS Anxiety | ||||||
|---|---|---|---|---|---|---|---|---|
| Coef | p | LL 95% CI | UL 95% CI | Coef | p | LL 95% CI | UL 95% CI | |
| Individual factor groupings by wave | ||||||||
| Crime and Disorder | 0.07 | 0.06 | -0.00 | 0.14 | 0.08 | 0.06 | -0.01 | 0.17 |
| Social Environment | 0.13 | 0.01 | 0.03 | 0.22 | 0.10 | 0.07 | -0.01 | 0.21 |
| Physical Environmental Problems | 0.08 | 0.05 | -0.00 | 0.16 | 0.09 | 0.07 | -0.01 | 0.19 |
| Overall neighbourhood perception by wave | ||||||||
| 0.04 | 0.01 | 0.01 | 0.07 | 0.04 | 0.04 | 0.00 | 0.08 | |
| Socio-Economic Status (SIMD Quintile) | Depression | Anxiety |
|---|---|---|
| SIMD 1 (most deprived) | 0.132 | 0.292 |
| SIMD 2 | 0.114 | 0.247 |
| SIMD 3 | 0.073 | 0.175 |
| SIMD 4 | 0.183 | 0.348 |
| SIMD 5 (least deprived) | 0.005 | 0.022 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Olsen, J.R.; Dundas, R.; Ellaway, A. Are Changes in Neighbourhood Perceptions Associated with Changes in Self-Rated Mental Health in Adults? A 13-Year Repeat Cross-Sectional Study, UK. Int. J. Environ. Res. Public Health 2017, 14, 1473. https://doi.org/10.3390/ijerph14121473
Olsen JR, Dundas R, Ellaway A. Are Changes in Neighbourhood Perceptions Associated with Changes in Self-Rated Mental Health in Adults? A 13-Year Repeat Cross-Sectional Study, UK. International Journal of Environmental Research and Public Health. 2017; 14(12):1473. https://doi.org/10.3390/ijerph14121473
Chicago/Turabian StyleOlsen, Jonathan R., Ruth Dundas, and Anne Ellaway. 2017. "Are Changes in Neighbourhood Perceptions Associated with Changes in Self-Rated Mental Health in Adults? A 13-Year Repeat Cross-Sectional Study, UK" International Journal of Environmental Research and Public Health 14, no. 12: 1473. https://doi.org/10.3390/ijerph14121473
APA StyleOlsen, J. R., Dundas, R., & Ellaway, A. (2017). Are Changes in Neighbourhood Perceptions Associated with Changes in Self-Rated Mental Health in Adults? A 13-Year Repeat Cross-Sectional Study, UK. International Journal of Environmental Research and Public Health, 14(12), 1473. https://doi.org/10.3390/ijerph14121473





