Sri Lanka Pilot Study to Examine Respiratory Health Effects and Personal PM2.5 Exposures from Cooking Indoors
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.1.1. Exposure Data
2.1.2. Respiratory Health Conditions
2.2. Statistical Analysis
2.3. Ethics
3. Results
3.1. Participant Characteristics
3.2. Cookstove, Fuels, and Kitchen Characteristics
3.3. Personal and Indoor PM2.5 Concentrations
3.4. Health Outcomes for Cooks
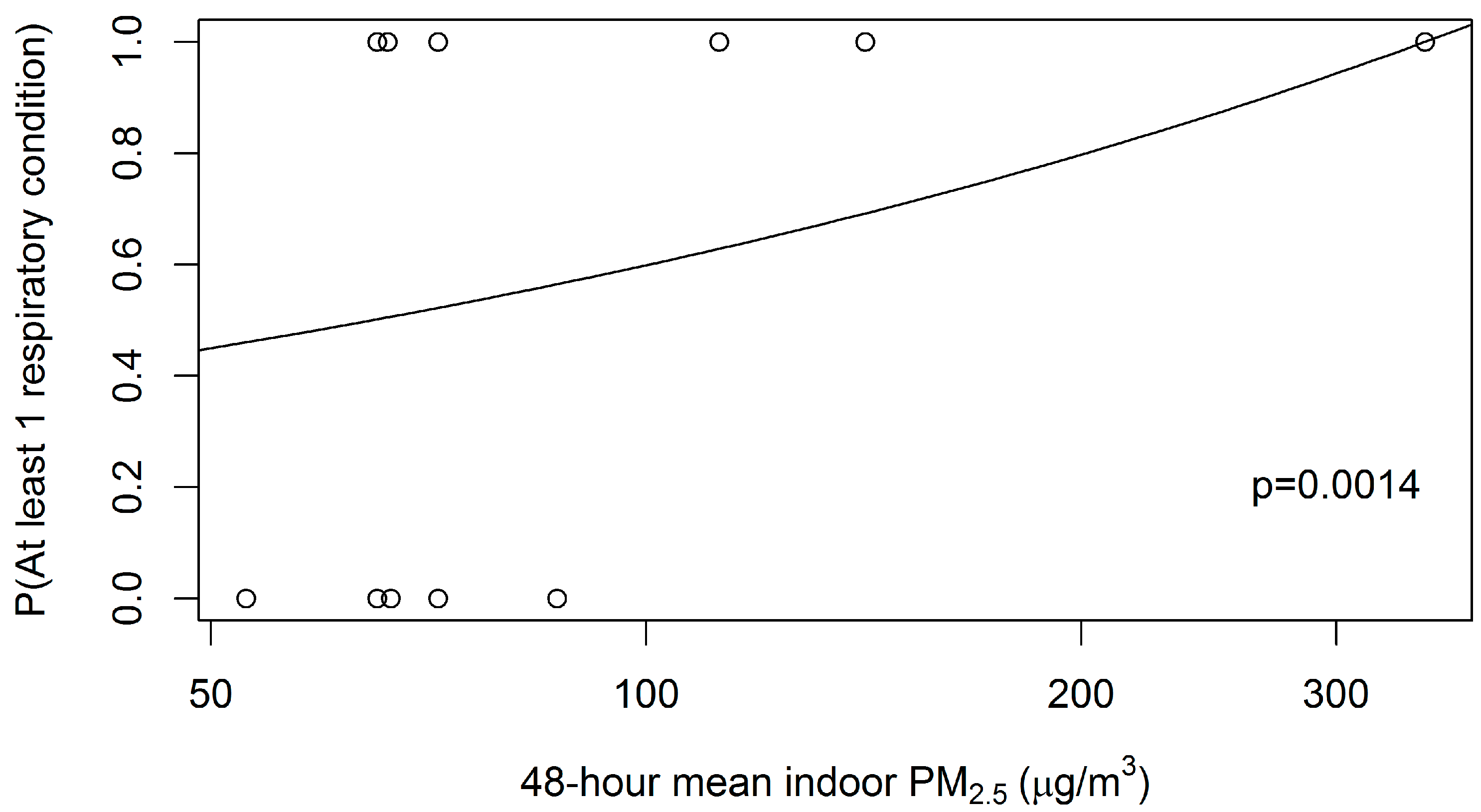
3.5. Health Outcomes for Children
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| CI | Confidence interval |
| CO | Carbon monoxide |
| COPD | Chronic obstructive pulmonary disease |
| HAP | Household air pollution |
| IDEA | Integrated Development Association |
| PM | Particulate matter |
| PM2.5 | Particulate matter less than 2.5 mm in diameter |
| PR | Prevalence ratio |
References
- World Health Organization. Burden of Disease from Household Air Pollution for 2012; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Bruce, N.; Perez-Padilla, R.; Albalak, R. Indoor air pollution in developing countries: A major environmental and public health challenge. Bull. World Health Organ. 2000, 78, 1078–1092. [Google Scholar] [PubMed]
- Dherani, M.; Pope, D.; Mascarenhas, M.; Smith, K.R.; Weber, M.; Bruce, N. Indoor air pollution from unprocessed solid fuel use and pneumonia risk in children aged under five years: A systematic review and meta-analysis. Bull. World Health Organ. 2008, 86, 390–398. [Google Scholar] [PubMed]
- Smith, K.R. National burden of disease in India from indoor air pollution. Proc. Natl. Acad. Sci. USA 2000, 97, 13286–13293. [Google Scholar] [CrossRef] [PubMed]
- Pope, D.P.; Mishra, V.; Thompson, L.; Siddiqui, A.R.; Rehfuess, E.A.; Weber, M.; Bruce, N.G. Risk of low birth weight and stillbirth associated with indoor air pollution from solid fuel use in developing countries. Epidemiol. Rev. 2010, 32, 70–81. [Google Scholar] [CrossRef] [PubMed]
- Kurmi, O.P.; Lam, K.B.; Ayres, J.G. Indoor air pollution and the lung in low- and medium-income countries. Eur. Respir. J. 2012, 40, 239–254. [Google Scholar] [CrossRef] [PubMed]
- Balakrishnan, K.; Sankar, S.; Parikh, J.; Padmavathi, R.; Srividya, K.; Venugopal, V.; Pandey, V.L. Daily average exposures to respirable particulate matter from combustion of biomass fuels in rural households of southern India. Environ. Health Perspect. 2002, 110, 1069–1075. [Google Scholar] [CrossRef] [PubMed]
- Mortimer, K.; Gordon, S.B.; Jindal, S.K.; Accinelli, R.A.; Balmes, J.; Martin, W.J. Household air pollution is a major avoidable risk factor for cardiorespiratory disease. Chest 2012, 142, 1308–1315. [Google Scholar] [CrossRef] [PubMed]
- Department of Census and Statistics (DCS). Sri Lanka Demographic and Health Survey 2006/7 Sri Lanka; Department of Census and Statistics (DCS): Colombo, Sri Lanka, 2008.
- Practical Action Consulting. Scale-up and Commercialisation of Improved Cookstoves in Sri Lanka: Lessons Learnt from the Anagi Experience; Practical Action Consulting: Rugby, UK, 2009. [Google Scholar]
- Elledge, M.F.; Phillips, M.J.; Thornburg, V.E.; Everett, K.H.; Nandasena, S. A profile of biomass stove use in Sri Lanka. Int. J. Environ. Res. Public Health 2009, 9, 1097–1110. [Google Scholar] [CrossRef] [PubMed]
- Nandasena, Y.L.; Wickremasinghe, A.R.; Sathiakumar, N. Air pollution and health in Sri Lanka: A review of epidemiologic studies. BMC Public Health 2010, 10, 300. [Google Scholar] [CrossRef] [PubMed]
- Chartier, R.; Phillips, M.; Mosquin, P.; Elledge, M.; Bronstein, K.; Nandasena, S.; Rodes, C. A comparative study of human exposures to household air pollution from commonly used cookstoves in Sri Lanka. Indoor Air 2016. [Google Scholar] [CrossRef] [PubMed]
- Core, R. Team (2015) R: A Language and Environment for Statistical Computing. Available online: http://www.R-project.org/ (accessed on 3 August 2016).
- Department of Census and Statistics (DCS) (2013) Household Income and Expenditure Survey–2012/2013. Available online: http://www.statistics.gov.lk/HIES/HIES201213BuletinEng.pdf (accessed on 3 August 2016).
- World Health Organization. Ambient Air Quality and Health. Available online: http://www.who.int/mediacentre/factsheets/fs313/en/ (accessed on 3 August 2016).
- Gurley, E.S.; Salje, H.; Homaira, N.; Ram, P.K.; Haque, R.; Petri, W.A.; Azziz-Baumgartner, E. Indoor exposure to particulate matter and age at first acute lower respiratory infection in a low-income urban community in Bangladesh. Am. J. Epidemiol. 2016, 179, 967–973. [Google Scholar] [CrossRef] [PubMed]
- Smith-Sivertsen, T.; Diaz, E.; Pope, D.; Lie, R.T.; Diaz, A.; McCracken, J.; Bruce, N. Effect of reducing indoor air pollution on women’s respiratory symptoms and lung function: The RESPIRE Randomized Trial, Guatemala. Am. J. Epidemiol. 2009, 170, 211–220. [Google Scholar] [CrossRef] [PubMed]
- Clark, M.L.; Peel, J.L.; Balakrishnan, K.; Breysse, P.N.; Chillrud, S.N.; Naeher, L.P.; Balbus, J.M. Health and household air pollution from solid fuel use: The need for improved exposure assessment. Environ. Health Perspect. 2013, 121, 1120–1128. [Google Scholar] [CrossRef] [PubMed]
- Balakrishnan, K.; Sambandam, S.; Ghosh, S.; Mukhopadhyay, K.; Vaswani, M.; Arora, N.K.; Smith, K.R. Household air pollution exposures of pregnant women receiving advanced combustion cookstoves in India: Implications for intervention. Ann. Glob. Health 2015, 81, 375–385. [Google Scholar] [CrossRef] [PubMed]

| All Households | Households with Children | |||
|---|---|---|---|---|
| Variable | N | (%) | N | (%) |
| Total | 53 | (100.0) | 35 | (100.0) |
| Household Size | ||||
| 2–3 people | 13 | (24.5) | 3 | (8.6) |
| 4–5 people | 27 | (50.9) | 23 | (65.7) |
| 6–7 people | 13 | (24.5) | 9 | (25.7) |
| Number of children (<18 years old) in Household | ||||
| 0 | 18 | (34.0) | – | – |
| 1 | 14 | (26.4) | 14 | (35.9) |
| 2 | 14 | (26.4) | 14 | (35.9) |
| 3 | 7 | (13.2) | 7 | (17.9) |
| Family Monthly Income in Sri Lankan Rupees | ||||
| 15,000 or less | 17 | (32.1) | 11 | (31.4) |
| 15,001–25,000 | 25 | (47.2) | 15 | (42.9) |
| 25,001 or more | 11 | (20.8) | 9 | (25.7) |
| Type of Stove | ||||
| Anagi | 33 | (62.3) | 18 | (51.4) |
| Traditional | 20 | (37.7) | 17 | (48.6) |
| Stove with Chimney | ||||
| Yes | 30 | (56.6) | 18 | (51.4) |
| No | 23 | (43.4) | 17 | (48.6) |
| Stove/Chimney Setup | ||||
| Traditional stove, no chimney | 11 | (20.8) | 9 | (25.7) |
| Traditional stove with chimney | 9 | (17.0) | 8 | (22.9) |
| Anagi stove, no chimney | 12 | (22.6) | 8 | (22.9) |
| Anagi stove with chimney | 21 | (39.6) | 10 | (28.5) |
| Location of Cooking Area | ||||
| Partitioned from rest of home | 24 | (45.3) | 17 | (48.6) |
| Not partitioned from rest of home | 15 | (28.3) | 9 | (25.7) |
| Separate building from living space | 14 | (26.4) | 9 | (25.7) |
| 48-Hour Mean Indoor PM2.5 Concentrations, µg/m3 | ||||
| Less than 100 | 21 | (39.6) | 13 | (37.1) |
| 100 to <200 | 19 | (35.9) | 12 | (34.3) |
| 200 or higher | 13 | (24.5) | 10 | (28.6) |
| 48-Hour Mean Personal (cook) PM2.5 Concentrations, µg/m3 | ||||
| Less than 100 | 31 | (58.5) | 20 | (57.1) |
| 100 to <200 | 14 | (26.4) | 9 | (25.7) |
| 200 or higher | 6 | (11.3) | 5 | (14.3) |
| missing | 2 | (3.8) | 1 | (2.9) |
| Location of Cooking Area | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Not Partitioned from the Rest of the Home | Partitioned from the Rest of the Home/Other Room | Separate Building from Living Space | |||||||
| Stove/Chimney Setup | n | Indoor | Personal | n | Indoor | Personal | n | Indoor | Personal |
| Anagi stove with chimney | 5 | 66.3 | 47.2 | 13 | 56.0 | 70.2 | 3 | 66.6 | 62.5 |
| Anagi stove, no chimney | 3 | 141.8 | 83.1 | 3 | 202.2 | 128.9 | 6 | 222.3 | 114.0 |
| Traditional stove with chimney | 5 | 71.8 | 64.5 | 4 | 109.5 | 64.0 | 0 | - | - |
| Traditional stove, no chimney | 2 | 221.5 | 139.2 | 4 | 430.3 | 160.4 | 5 | 417.7 | 215.7 |
| Study Factors | Had 1 or More Respiratory Conditions | PR a (95% CI) | p Value | |
|---|---|---|---|---|
| n/N ^ | n (%) P | |||
| Household Size | ||||
| 2–3 people R | 8/12 | 66.7 | 1.00 | |
| 4–5 people | 17/27 | 63.0 | 0.94 (0.58–1.55) | 0.821 |
| 6–7 people | 8/13 | 61.5 | 0.92 (0.51–1.66) | 0.790 |
| Family Monthly Income in Sri Lankan Rupees | ||||
| 15,000 or less R | 14/17 | 82.4 | 1.00 | |
| 15,001–25,000 | 12/25 | 48.0 | 0.58 (0.37–0.93) | 0.023 |
| 25,001 or more | 7/10 | 70.0 | 0.85 (0.54–1.35) | 0.490 |
| Age | ||||
| 35 years or younger R | 7/11 | 63.6 | 1.00 | |
| 36–45 years | 9/12 | 75.0 | 1.18 (0.68–2.05) | 0.561 |
| 46–55 years | 8/15 | 53.3 | 0.84 (0.44–1.61) | 0.595 |
| 56 years or older | 9/14 | 64.3 | 1.01 (0.56–1.83) | 0.973 |
| Highest Level of Education Achieved | ||||
| None to grade 9 R | 14/20 | 70.0 | 1.00 | |
| Grade 10 | 15/26 | 57.7 | 0.82 (0.53–1.28) | 0.385 |
| Grade 11 or higher | 4/6 | 66.7 | 0.95 (0.51–1.80) | 0.880 |
| Number of Years Cooking | ||||
| Less than 20 years R | 6/10 | 60.0 | 1.00 | |
| 21–30 years | 10/14 | 71.4 | 1.19 (0.65–2.18) | 0.572 |
| 21–40 years | 11/18 | 61.1 | 1.02 (0.54–1.90) | 0.954 |
| 41 years or more years | 6/10 | 60.0 | 1.00 (0.50–2.05) | 1.000 |
| Cooks 100% of the time * | ||||
| No R | 17/24 | 70.8 | 1.00 | |
| Yes | 16/28 | 57.1 | 0.81 (0.57–+∞) | 0.153 |
| Type of Stove * | ||||
| Anagi R | 19/32 | 59.4 | 1.00 | |
| Traditional | 14/20 | 70.0 | 1.18 (0.84–+∞) | 0.213 |
| Stove with Chimney * | ||||
| Yes R | 15/29 | 51.7 | 1.00 | |
| No | 18/23 | 72.3 | 1.51 (1.07–+∞) | 0.025 |
| Location of Cooking Area | ||||
| Partitioned from rest of home R | 12/23 | 52.2 | 1.00 | |
| Not partitioned from rest of home | 10/15 | 66.7 | 1.28 (0.75–2.17) | 0.365 |
| Separate building from living space | 11/14 | 78.6 | 1.51 (0.93–2.43) | 0.093 |
| Mean 48-h Personal PM2.5 Concentrations, µg/m3 1,* | ||||
| Less than 100 R | 15/30 | 50.0 | 1.00 | |
| 100 to <200 | 10/14 | 71.4 | 1.25 (0.92–+∞) | 0.120 |
| 200 or higher | 6/6 | 100.0 | +∞ | – |
| Had 1 or More Respiratory Conditions | ||||
|---|---|---|---|---|
| Study Factors | n/N ^ | n (%) P | PR a (95% CI) | p Value |
| Mother’s Education Level | ||||
| None to grade 9 R | 8/21 | 38.1 | 1.00 | |
| Grade 10 | 10/32 | 31.3 | 0.82 (0.38–1.75) | 0.609 |
| Grade 11 or higher | 3/10 | 30.0 | 0.79 (0.39–1.60) | 0.509 |
| School-aged (5 years old or older) | ||||
| Yes | 13/41 | 31.7 | 1.00 | |
| No | 8/22 | 36.4 | 1.14 (0.52–2.50) | 0.744 |
| Type of Stove * | ||||
| Anagi R | 8/34 | 23.5 | 1.00 | |
| Traditional | 13/29 | 44.8 | 2.08 (1.21–+∞) | 0.014 |
| Stove with Chimney * | ||||
| Yes R | 9/32 | 28.1 | 1.00 | |
| No | 12/31 | 38.7 | 1.45 (0.80–+∞) | 0.153 |
| Location of Cooking Area | ||||
| Partitioned from rest of home R | 8/32 | 25.0 | 1.00 | |
| Not partitioned from rest of home | 8/13 | 61.5 | 2.46 (1.22–4.95) | 0.012 |
| Separate building from living space | 5/18 | 27.8 | 1.11 (0.49–2.50) | 0.799 |
| Mean 48-h Indoor PM2.5 Concentrations, µg/m3 * | ||||
| Less than 100 R | 6/24 | 25.0 | 1.00 | |
| 100 to <200 | 5/17 | 29.4 | 1.18 (0.49–+∞) | 0.379 |
| 200 or higher | 10/22 | 45.5 | 1.82 (0.92–+∞) | 0.077 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Phillips, M.J.; Smith, E.A.; Mosquin, P.L.; Chartier, R.; Nandasena, S.; Bronstein, K.; Elledge, M.F.; Thornburg, V.; Thornburg, J.; Brown, L.M. Sri Lanka Pilot Study to Examine Respiratory Health Effects and Personal PM2.5 Exposures from Cooking Indoors. Int. J. Environ. Res. Public Health 2016, 13, 791. https://doi.org/10.3390/ijerph13080791
Phillips MJ, Smith EA, Mosquin PL, Chartier R, Nandasena S, Bronstein K, Elledge MF, Thornburg V, Thornburg J, Brown LM. Sri Lanka Pilot Study to Examine Respiratory Health Effects and Personal PM2.5 Exposures from Cooking Indoors. International Journal of Environmental Research and Public Health. 2016; 13(8):791. https://doi.org/10.3390/ijerph13080791
Chicago/Turabian StylePhillips, Michael J., Emily A. Smith, Paul L. Mosquin, Ryan Chartier, Sumal Nandasena, Katherine Bronstein, Myles F. Elledge, Vanessa Thornburg, Jonathan Thornburg, and Linda M. Brown. 2016. "Sri Lanka Pilot Study to Examine Respiratory Health Effects and Personal PM2.5 Exposures from Cooking Indoors" International Journal of Environmental Research and Public Health 13, no. 8: 791. https://doi.org/10.3390/ijerph13080791
APA StylePhillips, M. J., Smith, E. A., Mosquin, P. L., Chartier, R., Nandasena, S., Bronstein, K., Elledge, M. F., Thornburg, V., Thornburg, J., & Brown, L. M. (2016). Sri Lanka Pilot Study to Examine Respiratory Health Effects and Personal PM2.5 Exposures from Cooking Indoors. International Journal of Environmental Research and Public Health, 13(8), 791. https://doi.org/10.3390/ijerph13080791






