Traditional vs. Contemporary Management Control Practices for Developing Public Health Policies
Abstract
:1. Introduction
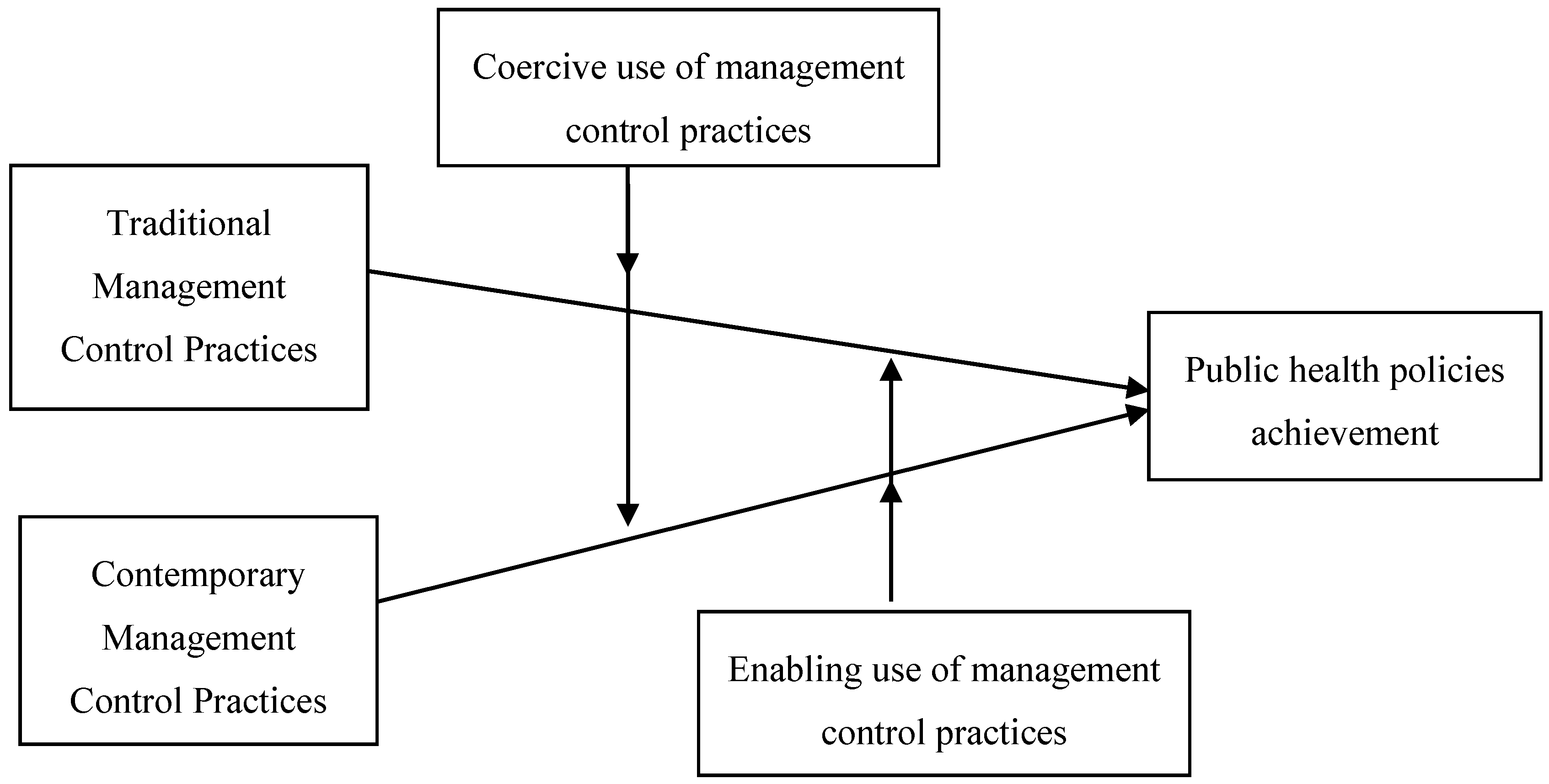
2. Research Hypotheses Development
3. Materials and Methods
Measurement of Variables
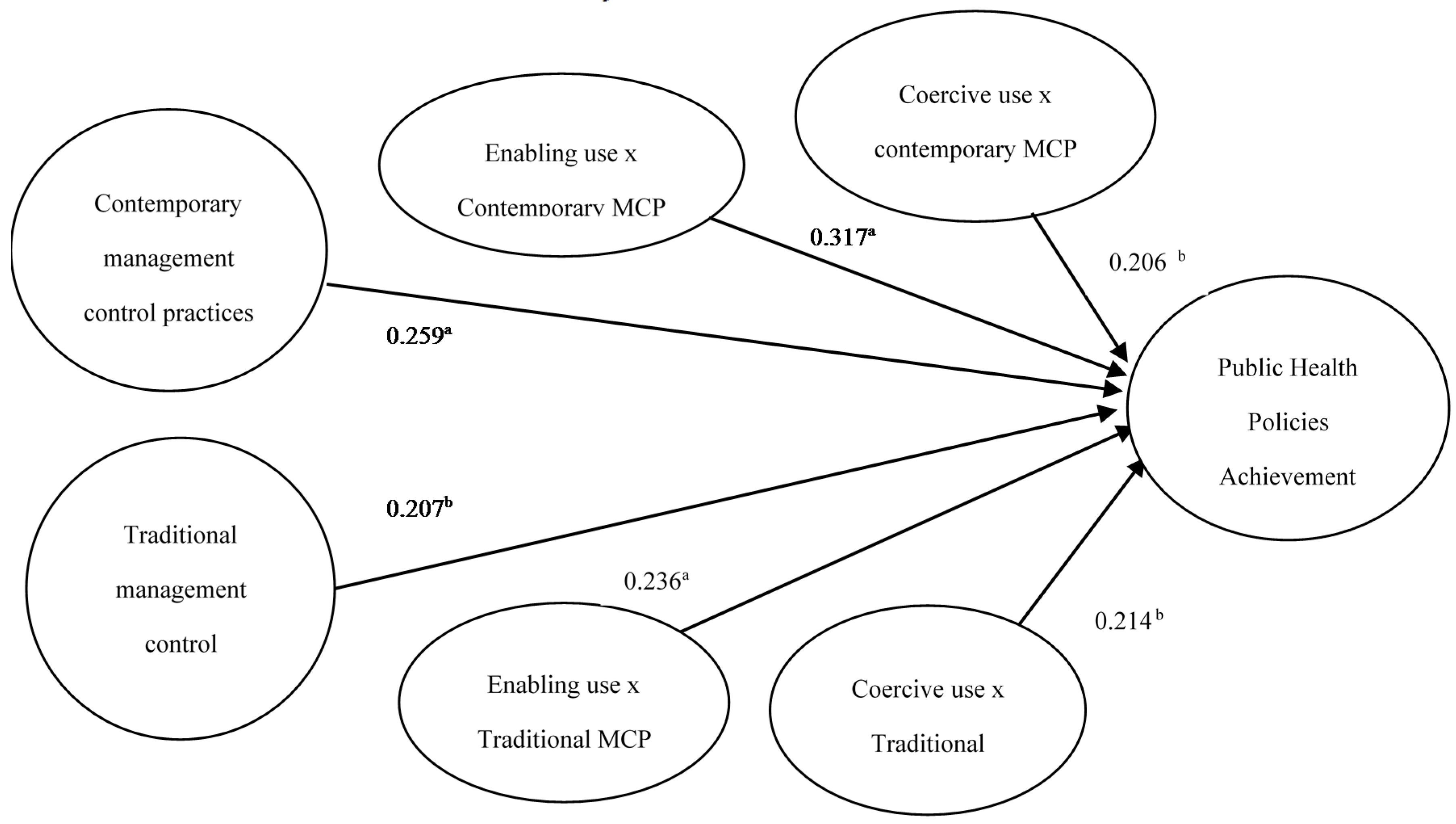
4. Results
5. Discussion
6. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Walker, R. Health information and public health. Health Inf. Manag. J. 2008, 37, 4–5. [Google Scholar] [CrossRef]
- Chen, H.; Hailey, D.; Wang, N.; Yu, P. A review of data quality assessment methods for public health information systems. Int. J. Environ. Res. Public Health 2014, 11, 5170–5207. [Google Scholar] [CrossRef] [PubMed]
- Health Research & Educational Trust. Environmental Sustainability in Hospitals: The Value of Efficiency; Health Research & Educational Trust: Chicago, IL, USA, 2014. [Google Scholar]
- Sandin-Vazquez, M.; Sarria-Santamera, A. Evaluación de impacto en salud: Valorando la efectividad de las políticas en la salud de las poblaciones. Rev. Esp. Salud Pública 2008, 82, 261–272. [Google Scholar] [CrossRef] [PubMed]
- Bialek, R.; Duffy, G.; Moran, J. The Public Health Quality Improvement Handbook; American Society for Quality; Quality Press: Milwaukee, WI, USA, 2009. [Google Scholar]
- Frizzelle, B.G.; Evenson, K.R.; Rodriguez, D.A.; Laraia, B.A. The importance of accurate road data for spatial applications in public health: Customizing a road network. Int. J. Health Geogr. 2009, 8. [Google Scholar] [CrossRef] [PubMed]
- Aqil, A.; Lippeveld, T.; Hozumi, D. PRISM framework: A paradigm shift for designing, strengthening and evaluating routine health information systems. Health Policy Plan. 2009, 24, 217–228. [Google Scholar] [CrossRef] [PubMed]
- Gostin, L.; Lazzarini, Z. The public health information infrastructure: A national review of the law on health information privacy. J. Am. Med. Assoc. 1996, 275, 1921–1927. [Google Scholar] [CrossRef]
- Sahin, Y.G.; Celikkan, U. MEDWISE: An innovative public health information system infrastructure. J. Med. Syst. 2012, 36, 1719–1729. [Google Scholar] [CrossRef] [PubMed]
- Bruce, G.; Tian, G. Lives in the balance: An analysis of the balanced scorecard (BSC) in healthcare organizations. In. J. Product. Perform. Manag. 2008, 57, 6–21. [Google Scholar] [CrossRef]
- Mavlutova, I.; Babauska, S. The Competitiveness and Balanced Scorecard of Health Care Companies. Int. J. Synerg. Res. 2013, 2, 107–128. [Google Scholar]
- Gumbus, A.; Wilson, T. Designing and implementing a balanced scorecard: Lessons learned in nonprofit implementation. Clin. Leadersh. Manag. Rev. 2004, 18, 226–232. [Google Scholar] [PubMed]
- Tessier, S.; Otley, D. From management controls to the management of controls. Account. Audit. Account. J. 2012, 25, 776–805. [Google Scholar] [CrossRef]
- Weir, E.; d’Entremont, N.; Stalker, S.; Kurji, K.; Robinson, V. Applying the balanced scorecard to local public health performance measurement: Deliberations and decisions. BMC Public Health 2009, 9, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Inamdar, N.; Kaplan, R.S.; Bower, M. Applying the balanced scorecard in healthcare provider organizations. J. Healthc. Manag. 2002, 47, 179–195. [Google Scholar] [PubMed]
- Bisbe, J.; Barrubés, J. The balanced scorecard as a management tool for assessing and monitoring strategy implementation in health care organizations. Rev. Esp. Cardiol. 2012, 65, 919–927. [Google Scholar] [CrossRef] [PubMed]
- Kollberg, B.; Elg, M. The practice of the Balanced Scorecard in health care services. Int. J. Product. Perform. Manag. 2011, 60, 427–445. [Google Scholar] [CrossRef]
- Nebot, M.; López, J.; Ariza, C.; Villalbí, J.R.; García-Altés, A. Evaluación de la efectividad en salud pública: Fundamentos conceptuales y metodológicos. Gac. Sanit. 2011, 25, S3–S8. [Google Scholar] [CrossRef]
- Fottler, M.D.; Erickson, E.; Rivers, P. Bringing human resources to the table: Utilization of an HR balanced scorecard at Mayo Clinic. Health Care Manag. Rev. 2006, 31, 64–72. [Google Scholar] [CrossRef]
- Chang, L. The NHS performance assessment framework as a balanced scorecard approach. Int. J. Public Sector Manag. 2007, 20, 101–117. [Google Scholar] [CrossRef]
- Lorden, A.; Coustasse, A.; Singh, K.P. The balanced scorecard framework-A case study of patient and employee satisfaction: What happens when it does not work as planned? Health Care Manag. Rev. 2008, 33, 145–155. [Google Scholar] [CrossRef] [PubMed]
- Raisch, S.; Birkinshaw, J. Organizational ambidexterity: Antecedents, outcomes and moderators. J. Manag. 2008, 34, 375–409. [Google Scholar] [CrossRef]
- Adler, P.S.; Borys, B. Two Types of Bureaucracy: Enabling and Coercive. Adm. Sci. Q. 1996, 41, 61–89. [Google Scholar] [CrossRef]
- Kivinen, T.; Lammintakanen, J. The success of a management information system in healthcare—A case study from Finland. Int. J. Med. Inform. 2013, 82, 90–97. [Google Scholar] [CrossRef] [PubMed]
- Haux, R. Health information systems—Past, present, future. Int. J. Med. Inform. 2006, 75, 268–281. [Google Scholar] [CrossRef] [PubMed]
- Curry, A.; Moore, C. Assessing information culture—An exploratory model. Int. J. Inf. Manag. 2003, 23, 91–110. [Google Scholar] [CrossRef]
- Berg, M. Implementing information systems in health care organizations: Myths and challenges. Int. J. Med. Inform. 2001, 64, 143–156. [Google Scholar] [CrossRef]
- Mitton, C.; Dionne, F.; Donaldson, C. Managing healthcare budgets in times of austerity: The role of program budgeting and marginal analysis. Appl. Health. Econ. Health Policy 2014, 12, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Handler, A.; Issel, M.; Turnock, B. A conceptual framework to measure performance of the public health system. Am. J. Public Health 2001, 91, 1235–1239. [Google Scholar] [CrossRef] [PubMed]
- Turnock, B.J.; Handler, A.S. From measuring to improving public health practice. Annu. Rev. Public Health 1997, 18, 261–282. [Google Scholar] [CrossRef] [PubMed]
- Chow, C.W.; Ganulin, D.; Williamson, J. The Balanced Scorecard: A potent tool for energizing and focusing healthcare organization management. J. Healthc. Manag. 1998, 43, 263–280. [Google Scholar] [PubMed]
- Zelman, W.N.; Pink, G.H.; Matthias, C.B. Use of the Balanced Scorecard in Health Care. J. Health Care Finance 2003, 29, 1–16. [Google Scholar] [PubMed]
- Wernerfelt, B. A resource-based view of the firm. Strateg. Manag. J. 1984, 5, 171–180. [Google Scholar] [CrossRef]
- Henri, J. Management control systems and strategy: A resource-based perspective. Account. Organ. Soc. 2006, 31, 529–558. [Google Scholar] [CrossRef]
- Langfield-Smith, K. Strategic Management Accounting: How far Have We Come in 25 Years? Account. Audit. Account. J. 2008, 21, 204–228. [Google Scholar]
- Naranjo-Gil, D. Strategic performance in hospitals: The use of the balanced scorecard by nurse managers. Health Care Manag. Rev. 2009, 34, 161–170. [Google Scholar] [CrossRef] [PubMed]
- Derose, S.F.; Asch, S.M.; Fielding, J.E.; Schuster, M.A. Developing quality indicators for local health departments: Experience in Los Angeles County. Am. J. Prev. Med. 2003, 25, 347–357. [Google Scholar] [CrossRef]
- Woodward, G.; Manuel, D.; Goel, V. Developing a Balanced Scorecard for Public Health. 2004. Available online: http://www.ices.on.ca/~/media/Files/Atlases-Reports/2004/Developing-a-balanced-scorecard-for-public-health/Full%20report.ashx (accessed on 20 April 2016).
- Robinson, V.A.; Hunter, D.; Shortt, S.E. Accountability in public health units: Using a modified nominal group technique to develop a balanced scorecard for performance measurement. Can. J. Public Health 2003, 94, 391–96. [Google Scholar] [PubMed]
- Bible, L.; Kerr, S.; Zanini, M. The Balanced Scorecard: Here and Back. Manag. Account. Q. 2006, 7, 18–23. [Google Scholar]
- Schmidt, S.; Bateman, I.; Breinlinger-O’Reilly, J.; Smith, P. A management approach that drives actions strategically: Balanced scorecard in a mental health trust case study. Int. J. Health Care Qual. Assur. 2006, 19, 119–135. [Google Scholar] [CrossRef]
- Moore, M.H. Managing for Value: Organizational Strategy in For-Profit, Nonprofit and Governmental Organizations. Nonprofit Volunt. Sect. Q. 2000, 29, 183–204. [Google Scholar] [CrossRef]
- Porter, M.E.; Olmsted, T. Redefining Health Care: Creating Value Based Competition on Results; Harvard Business School Press: Boston, MA, USA, 2006. [Google Scholar]
- Chapman, C.S.; Kihn, L.A. Information System Integration, Enabling Control and Performance. Account Organ. Soc. 2009, 34, 151–169. [Google Scholar] [CrossRef]
- Kober, R.; Ng, J.; Paul, B. The interrelationship between management control mechanisms and strategy. Manag. Account. Res. 2007, 18, 425–452. [Google Scholar] [CrossRef]
- Pettersen, I.; Nyland, K. Management and control of public hospitals—The use of performance measures in Norwegian hospitals. A case-study. Int. J. Health Plan. Manag. 2006, 21, 133–149. [Google Scholar] [CrossRef]
- Bacigalupe, A.; Esnaola, S.; Calderón, C.; Zuzagoitia, J.; Aldasoro, E. La evaluación del impacto en la salud: Una herramienta para incorporar la salud en las intervenciones no sanitarias. Gac. Sanit. 2009, 23, 62–66. [Google Scholar] [CrossRef] [PubMed]
- Chenhall, R.H. Accounting for the horizontal organization: A review essay. Account. Organ. Soc. 2008, 33, 517–550. [Google Scholar] [CrossRef]
- Cadez, S.; Guilding, C. Strategy, strategic management accounting and performance: A configurational analysis. Ind. Manag. Data Syst. 2012, 112, 484–501. [Google Scholar] [CrossRef]
- Hair, J.; Anderson, R.; Tatham, R.; Black, W. Multivariate Data Analysis; Prentice Hall: Upper Saddle River, NJ, USA, 1999. [Google Scholar]
- García Armesto, S.; Abadía Taira, M.B.; Durán, A.; Hernández Quevedo, C.; Bernal Delgado, E. España: Análisis del sistema sanitario. Sist. Sanit. Transic. 2011, 12, 1–240. [Google Scholar]
- Ramiro Avilés, M.; Lobo, F. La justificación de las políticas de salud pública desde la ética y la eficiencia económica. Gac. Sanit. 2010, 24, 120–127. [Google Scholar] [CrossRef] [PubMed]
- Fischer, K. Decision-making in healthcare: A practical application of partial least square path modelling to coverage of newborn screening programmes. BMC Med. Inform. Decis. Mark. 2012, 12, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Lawson, J.; Rotem, A. From Clinician to Manager: An Introduction to Hospital and Health Service Management; McGraw Hill: Sydney, Australia, 2004. [Google Scholar]
- Peirce, J.C. The paradox of physicians and administrators in health care organizations. Health Care Manag. Rev. 2000, 25, 7–28. [Google Scholar] [CrossRef]
- Abernethy, M.A.; Lillis, A.M. Interdependencies in Organization Design: A Test in Hospitals. J. Manag. Account. Res. 2001, 13, 107–129. [Google Scholar] [CrossRef]
- Hambrick, D.C. Upper Echelons Theory: An Update. Acad. Manag. Rev. 2007, 32, 334–343. [Google Scholar] [CrossRef]
- Helgsen, S. The Female Advantage: Women’s Ways of Leadership; Doubleday Currency: Toronto, ON, Canada, 1995. [Google Scholar]
- Anderson, D. The integration of gender and political behavior into Hambrick and Mason’s upper echelons model of organizations. J. Am. Acad. Bus 2003, 3, 29–36. [Google Scholar]
| Factor 1 Coercive Use | Factor 2 Enabling Use | |
|---|---|---|
| Item 1: following up preset plans and goals tightly | 0.782 | 0.214 |
| Item 2: Managing through the exceptions’ analysis and deviation | 0.849 | 0.186 |
| Item 3: Evaluating and control subordinates tightly | 0.772 | 0.327 |
| Item 4: Encouraging new public health initiatives and policies | 0.226 | 0.834 |
| Item 5: Signaling key strategic priorities | 0.274 | 0.812 |
| Item 6: Encouraging the adoption of new actions and processes | 0.183 | 0.791 |
| Cumulative Variance | 32.540% | 59.815% |
| Cronbach Alpha | 0.789 | 0.812 |
| Factor 1 | |
|---|---|
| Item 1: Monitor health status to identify and solve community health problems | 0.722 |
| Item 2: Timely diagnose and identification of health threats in the community | 0.760 |
| Item 3: Health promotion partnerships within the community | 0.804 |
| Item 4: Develop policies to protect health and guide public health practice | 0.751 |
| Item 5: Assure effective entry into a coordinated system of clinical care | 0.779 |
| Item 6: Assure a competent healthcare workforce by continuing learning | 0.814 |
| Item 7: Monitoring the linkages between public health practice and academic/research (e.g., epidemiological and public health systems studies) | 0.785 |
| Cumulative Variance | 57.148% |
| Cronbach Alpha | 0.836 |
| Variable | Mean | Standard Deviation (SD) | Theoretical Range | Actual Range |
|---|---|---|---|---|
| 1. Adoption of contemporary MCP | 2.98 | 0.32 | 1.00–5.00 | 1.00–5.00 |
| 2. Adoption of traditional MCP | 3.22 | 0.38 | 1.00–5.00 | 1.00–5.00 |
| 3. Coercive use of MCP | 3.29 | 0.45 | 1.00–5.00 | 1.00–5.00 |
| 4. Enabling use of MCP | 3.47 | 0.48 | 1.00–5.00 | 1.00–5.00 |
| 5. Achievement of Public health initiatives | 3.51 | 0.53 | 1.00–5.00 | 1.00–5.00 |
| 6. Age of managers | 44.6 | 4.5 | – | 30–61 |
| 7. Tenure | 6.7 | 4.9 | – | 1–18 |
| 8. Clinical-oriented background | 2.89 | 0.71 | 1.00–5.00 | 1.00–5.00 |
| 9. Business-oriented background | 3.07 | 0.82 | 1.00–5.00 | 1.00–5.00 |
| 10. Male (Female): 82.75% (17.25%) |
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|
| 1. Adoption of contemporary MCP | 1.000 | |||||||
| 2. Adoption of traditional MCP | 0.141 | 1.000 | ||||||
| 3. Coercive use of MCP | 0.183 | 0.211 b | 1.000 | |||||
| 4. Enabling use of MCP | 0.247 a | 0.199 b | 0.104 | 1.000 | ||||
| 5. Achievement of Public health initiatives | 0.257 a | 0.204 b | 0.178 | 0.195 b | 1.000 | |||
| 6. Age of managers | −0.324 a | 0.169 | 0.231 a | −0.182 | 0.065 | 1.000 | ||
| 7. Tenure | 0.219 a | 0.152 | 0.166 | 0.212 b | 0.116 | 0.224 a | 1.000 | |
| 8. Clinical-oriented background | 0.233 a | 0.184 | −0.170 | 0.257 a | 0.153 | 0.126 | 0.147 | 1.000 |
| 9. Business-oriented background | 0.186 | 0.251 a | 0.218 b | 0.188 | 0.161 | 0.139 | 0.120 | 0.074 |
| From: | To: Achievement of Public Health Initiatives |
|---|---|
| 1. Adoption of contemporary MCP | 0.259 a |
| 2. Adoption of traditional MCP | 0.207 b |
| 3. Enabling use of traditional MCP | 0.236 a |
| 4. Enabling use of contemporary MCP | 0.317 a |
| 5. Coercive use of traditional MCP | 0.214 b |
| 6. Coercive use of contemporary MCP | 0.206 b |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Naranjo-Gil, D.; Sánchez-Expósito, M.J.; Gómez-Ruiz, L. Traditional vs. Contemporary Management Control Practices for Developing Public Health Policies. Int. J. Environ. Res. Public Health 2016, 13, 713. https://doi.org/10.3390/ijerph13070713
Naranjo-Gil D, Sánchez-Expósito MJ, Gómez-Ruiz L. Traditional vs. Contemporary Management Control Practices for Developing Public Health Policies. International Journal of Environmental Research and Public Health. 2016; 13(7):713. https://doi.org/10.3390/ijerph13070713
Chicago/Turabian StyleNaranjo-Gil, David, María Jesús Sánchez-Expósito, and Laura Gómez-Ruiz. 2016. "Traditional vs. Contemporary Management Control Practices for Developing Public Health Policies" International Journal of Environmental Research and Public Health 13, no. 7: 713. https://doi.org/10.3390/ijerph13070713
APA StyleNaranjo-Gil, D., Sánchez-Expósito, M. J., & Gómez-Ruiz, L. (2016). Traditional vs. Contemporary Management Control Practices for Developing Public Health Policies. International Journal of Environmental Research and Public Health, 13(7), 713. https://doi.org/10.3390/ijerph13070713





