Effect of Length of Stay on Smoking among Turkish and Eastern European Immigrants in Germany—Interpretation in the Light of the Smoking Epidemic Model and the Acculturation Theory
Abstract
:1. Introduction
2. Methods
2.1. Data Source
2.2. Study Sample
2.3. Outcome and Exposure Measures
2.4. Statistical Analyses
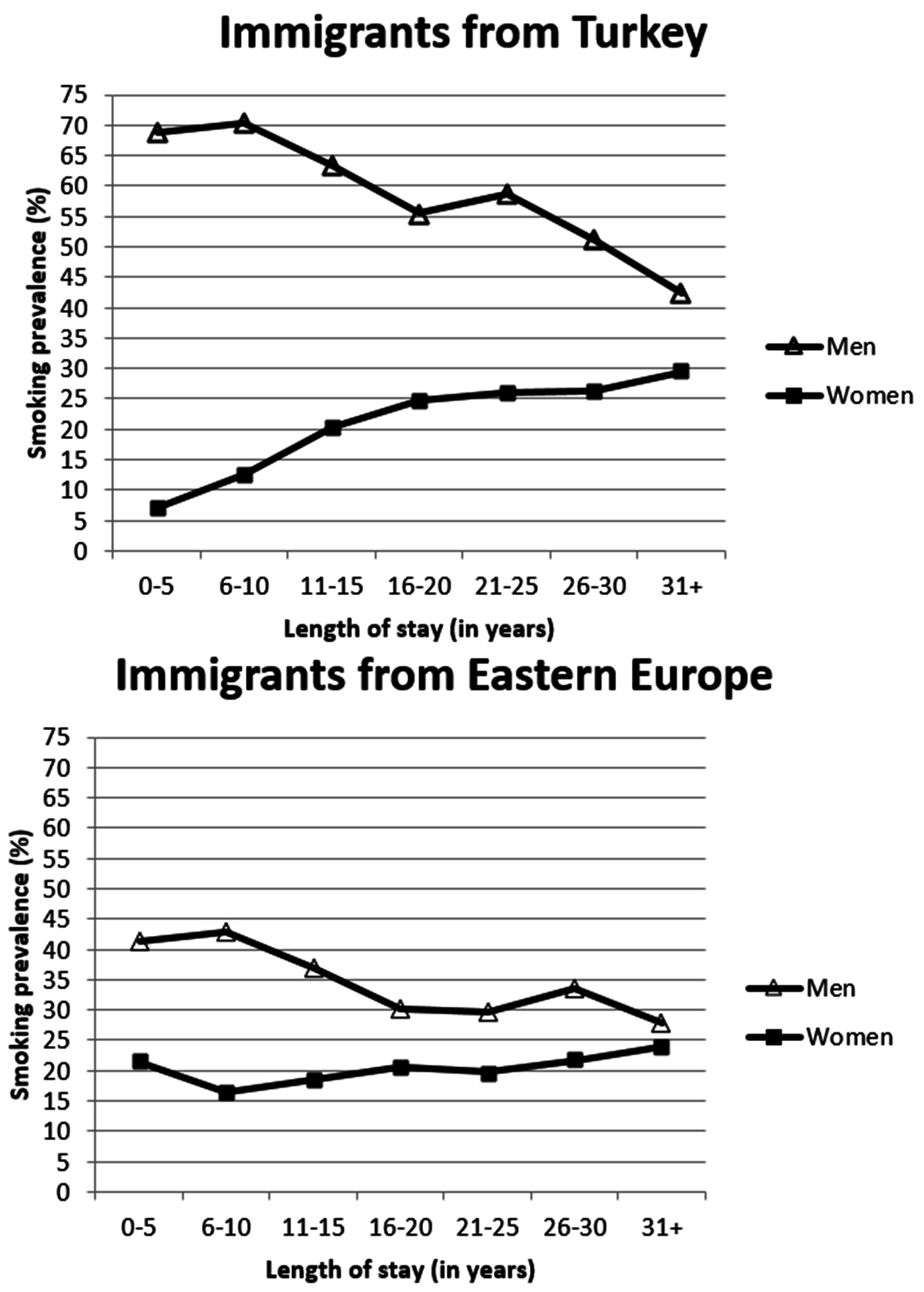
3. Results
| Variable | Immigrants from Turkey (n = 3871 Observations) | Immigrants from Eastern Europe (n = 7202 Observations) | Non-Immigrants (n = 140,701 Observations) | ||||
|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | ||
| Age (in years) | Up to 30 | 614 | 15.9 | 1508 | 20.9 | 21,133 | 15.0 |
| 31–40 | 1415 | 36.5 | 1528 | 21.2 | 25,041 | 17.8 | |
| 41–50 | 721 | 18.6 | 1546 | 21.5 | 29,116 | 20.7 | |
| 51–60 | 565 | 14.6 | 1163 | 16.2 | 24,551 | 17.5 | |
| 61 and older | 556 | 14.4 | 1457 | 20.2 | 40,860 | 29.0 | |
| Mean: 43.1 (SD: 13.2; range: 18–86) | Mean: 45.6 (SD: 16.4; range: 17–99) | Mean: 49.6 (SD: 17.0; range: 17–102) | |||||
| Sex | Male | 2035 | 52.6 | 3185 | 44.2 | 67,096 | 47.7 |
| Female | 1836 | 47.4 | 4017 | 55.8 | 73,605 | 52.3 | |
| Marital Status | Married | 3470 | 89.6 | 5318 | 73.8 | 90,174 | 64.1 |
| Single | 176 | 4.6 | 1117 | 15.5 | 30,261 | 21.5 | |
| Other marital status | 225 | 5.8 | 767 | 10.7 | 20,266 | 14.4 | |
| Annual net household income (in 1000 Euro) | Mean: 28.9 (SD: 16.2; range: 0–177.9) | Mean: 30.0 (SD: 16.8; range: 0–231.4) | Mean: 37.3 (SD: 32.7; range: 0–4282.0) | ||||
| Labour force status | Working | 1908 | 49.3 | 4302 | 59.7 | 82,512 | 58.7 |
| Unemployed | 433 | 11.2 | 565 | 7.9 | 6664 | 4.7 | |
| Non-working | 1530 | 39.5 | 2335 | 32.4 | 51,525 | 36.6 | |
| Education (in years) | Mean: 9.6 (SD: 2.1; range: 7–18) | Mean: 11.4 (SD: 2.3; range: 7–18) | Mean: 12.2 (SD: 2.6; range: 7–18) | ||||
| Length of stay (in years) | 0–5 | 132 | 3.4 | 407 | 5.6 | not applicable | |
| 6–10 | 299 | 7.7 | 1764 | 24.5 | |||
| 11–15 | 356 | 9.2 | 1944 | 27.0 | |||
| 16–20 | 464 | 12.0 | 1325 | 18.4 | |||
| 21–25 | 674 | 17.4 | 705 | 9.8 | |||
| 26–30 | 862 | 22.23 | 297 | 4.1 | |||
| 31+ | 1084 | 28.0 | 760 | 10.6 | |||
| Mean: 24.3 (SD: 9.7; range: 1–53) | Mean: 16.8 (SD: 10.7; range: 0–63) | ||||||
| Smoking | No | 2348 | 60.7 | 5286 | 73.4 | 100,454 | 71.4 |
| Yes | 1523 | 39.3 | 1916 | 26.6 | 40247 | 28.6 | |
| Covariate | Women from Turkey | Men from Turkey | Women from Eastern Europe | Men from Eastern Europe | Non-Immigrant Women | Non-Immigrant Men | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Length of stay (in years) | 1.14 *** | (1.06, 1.21) | 0.96 | (0.90, 1.02) | 1.03 | (0.99, 1.08) | 0.98 | (0.94, 1.02) | - | - | - | - |
| Up to 30 years | ref. | - | ref. | - | ref. | - | ref. | - | ref. | - | ref. | - |
| 31–40 years | 0.45 | (0.20, 1.01) | 1.89 | (0.88, 4.03) | 0.70 | (0.38, 1.30) | 0.86 | (0.43, 1.74) | 0.83 * | (0.69, 1.00) | 0.95 | (0.79, 1.15) |
| 41–50 years | 0.28 * | (0.08, 0.91) | 1.07 | (0.36, 3.23) | 0.50 | (0.23, 1.12) | 0.56 | (0.23, 1.36) | 0.56 *** | (0.45, 0.71) | 0.62 *** | (0.49, 0.79) |
| 51–60 years | 0.05 *** | (0.01, 0.21) | 0.18 * | (0.04, 0.77) | 0.20 *** | (0.08, 0.51) | 0.30 * | (0.10, 0.85) | 0.23 *** | (0.18, 0.30) | 0.24 *** | (0.18, 0.31) |
| 61 years and older | 0.02 *** | (0.00, 0.11) | 0.06 ** | (0.01, 0.34) | 0.03 *** | (0.01, 0.11) | 0.09 *** | (0.03, 0.31) | 0.04 *** | (0.03, 0.05) | 0.05 *** | (0.04, 0.07) |
| Married | ref. | - | ref. | - | ref. | - | ref. | - | ref. | - | ref. | - |
| Single | 0.58 | (0.09, 3.68) | 0.81 | (0.28, 2.35) | 3.27 ** | (1.52, 7.06) | 1.01 | (0.42, 2.41) | 2.68 *** | (2.19, 3.28) | 1.80 *** | (1.47, 2.22) |
| Other marital status | 1.64 | (0.47, 5.69) | 3.16 | (0.67, 14.88) | 3.08 ** | (1.48, 6.41) | 2.69 | (0.83, 8.72) | 1.84 *** | (1.53, 2.22) | 2.56 *** | (2.07, 3.18) |
| Working | ref. | - | ref. | - | ref. | - | ref. | - | ref. | - | ref. | - |
| Unemployed | 1.04 | (0.41, 2.59) | 0.83 | (0.42, 1.62) | 1.36 | (0.67, 2.77) | 0.72 | (0.36, 1.46) | 0.86 | (0.70, 1.07) | 1.48 *** | (1.20, 1.82) |
| Non-working | 0.34 ** | (0.18, 0.65) | 1.24 | (0.54, 2.88) | 0.65 | (0.40, 1.06) | 0.43 * | (0.22, 0.83) | 0.33 *** | (0.29, 0.38) | 0.46 *** | (0.39, 0.53) |
| Education (in years) | 1.10 | (0.90, 1.35) | 0.92 | (0.77, 1.09) | 0.99 | (0.86, 1.12) | 0.82 * | (0.70, 0.96) | 0.75 *** | (0.72, 0.78) | 0.73 *** | (0.71, 0.76) |
| Annual net household income (in 1000 Euro) | 1.00 | (0.98, 1.02) | 1.00 | (0.98, 1.01) | 0.98 ** | (0.96, 0.99) | 0.97 *** | (0.95, 0.99) | 0.99 *** | (0.99, 1.00) | 1.00 *** | (0.99, 1.00) |
| Survey year: 1998 | ref. | - | ref. | - | ref. | - | ref. | - | ref. | - | ref. | - |
| Survey year: 1999 | 1.35 | (0.61, 2.95) | 1.03 | (0.56, 1.89) | 1.70 | (0.79, 3.66) | 1.14 | (0.62, 2.11) | 1.31 ** | (1.09, 1.57) | 1.18 | (1.00, 1.40) |
| Survey year: 2001 | 1.72 | (0.77, 3.83) | 0.96 | (0.50, 1.83) | 1.23 | (0.59, 2.56) | 0.84 | (0.46, 1.52) | 1.11 | (0.94, 1.32) | 0.95 | (0.80, 1.12) |
| Survey year: 2002 | 3.15 ** | (1.37, 7.26) | 1.09 | (0.56, 2.15) | 1.53 | (0.73, 3.21) | 0.82 | (0.44, 1.53) | 1.21 * | (1.02, 1.44) | 1.00 | (0.85, 1.18) |
| Survey year: 2004 | 2.00 | (.82, 4.90) | 0.72 | (0.34, 1.52) | 1.37 | (0.64, 2.94) | 0.75 | (0.39, 1.44) | 1.09 | (0.92, 1.30) | 0.81 * | (0.68, 0.95) |
| Survey year: 2006 | 3.46 * | (1.33, 9.03) | 0.66 | (0.28, 1.51) | 1.59 | (0.73, 3.49) | 0.78 | (0.38, 1.56) | 0.97 | (0.81, 1.16) | 0.65 *** | (0.55, 0.77) |
| Survey year: 2008 | 2.08 | (0.72, 6.01) | 0.33 * | (0.13, 0.87) | 1.04 | (0.45, 2.39) | 0.61 | (0.28, 1.32) | 0.71 *** | (0.59, 0.86) | 0.59 *** | (0.50, 0.71) |
| Survey year: 2010 | 1.02 | (0.31, 3.38) | 0.56 | (0.19, 1.67) | 1.48 | (0.62, 3.53) | 0.90 | (0.39, 2.08) | 0.78 * | (0.64, 0.95) | 0.57 *** | (0.47, 0.68) |
| Survey year: 2012 | 0.53 | (0.13, 2.20) | 0.27 * | (0.08, 0.95) | 1.31 | (0.54, 3.16) | 1.00 | (0.41, 2.46) | 0.82 | (0.67, 1.01) | 0.50 *** | (0.42, 0.61) |
| Constant | 0.00 *** | (0.00, 0.03) | 19.24 ** | (2.07, 178.83) | 0.01 *** | (0.00, 0.03) | 13.17 ** | (1.86, 93.04) | 0.71 | (0.42, 1.21) | 6.94 *** | (4.17, 11.55) |
| Rho (intraclass correlation) | 0.88 | 0.87 | 0.91 | 0.89 | 0.94 | 0.93 | ||||||
| Log likelihood | −585.33 | −820.62 | −1101.46 | −1277.19 | −21,083.70 | −22,342.91 | ||||||
| Persons | 393 | 435 | 1118 | 891 | 17,678 | 16,333 | ||||||
| Observations | 1836 | 2035 | 4017 | 3185 | 73,605 | 67,096 | ||||||
| Variable | Women from Turkey 1 | Men from Turkey 2 | |||
|---|---|---|---|---|---|
| SPR | 95% CI | SPR | 95% CI | ||
| Length of stay (in years) | 0–5 | 0.25 | (0.10–0.57) | 1.67 | (1.22–2.26) |
| 6–10 | 0.40 | (0.26–0.61) | 1.67 | (1.38–2.02) | |
| 11–15 | 0.61 | (0.46–0.82) | 1.49 | (1.20–1.84) | |
| 16–20 | 0.84 | (0.65–1.08) | 1.38 | (1.16–1.64) | |
| 21–25 | 0.87 | (0.71–1.08) | 1.48 | (1.29–1.70) | |
| 26–30 | 1.02 | (0.84–1.23) | 1.49 | (1.31–1.69) | |
| 31+ | 1.25 | (1.06–1.48) | 1.38 | (1.23–1.56) | |
| Women from Eastern Europe 1 | Men from Eastern Europe 2 | ||||
| SPR | 95% CI | SPR | 95% CI | ||
| Length of stay (in years) | 0–5 | 0.71 | (0.54–0.94) | 1.16 | (0.92–1.46) |
| 6–10 | 0.59 | (0.51–0.69) | 1.17 | (1.06–1.30) | |
| 11–15 | 0.69 | (0.60–0.79) | 1.06 | (0.96–1.18) | |
| 16–20 | 0.77 | (0.65–0.90) | 0.90 | (0.78–1.04) | |
| 21–25 | 0.75 | (0.60–0.94) | 0.95 | (0.77–1.17) | |
| 26–30 | 0.99 | (0.72–1.35) | 1.24 | (0.91–1.70) | |
| 31+ | 1.14 | (0.94–1.40) | 1.04 | (0.85–1.28) | |
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Teo, K.K.; Ounpuu, S.; Hawken, S.; Pandey, M.R.; Valentin, V.; Hunt, D.; Diaz, R.; Rashed, W.; Freeman, R.; Jiang, L.; et al. Tobacco use and risk of myocardial infarction in 52 countries in the INTERHEART study: A case-control study. Lancet 2006, 368, 647–658. [Google Scholar] [CrossRef]
- Vineis, P.; Alavanja, M.; Buffler, P.; Fontham, E.; Franceschi, S.; Gao, Y.T.; Gupta, P.C.; Hackshaw, A.; Matos, E.; Samet, J.; et al. Tobacco and cancer: Recent epidemiological evidence. J. Natl. Cancer Inst. 2004, 96, 99–106. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Economics of Tobacco Toolkit—Assessment of the Economic Costs of Smoking; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Lopez, A.D.; Collishaw, N.E.; Piha, T. A descriptive model of the cigarette epidemic in developed countries. Tob. Control 1994, 3, 242–247. [Google Scholar] [CrossRef]
- Thun, M.; Peto, R.; Boreham, J.; Lopez, A.D. Stages of the cigarette epidemic on entering its second century. Tob. Control 2012, 21, 96–101. [Google Scholar] [CrossRef] [PubMed]
- Lampert, T.; von der Lippe, E.; Müters, S. Prevalence of smoking in the adult population of Germany: Results of the German Health Interview and Examination Survey for Adults (DEGS1). Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 2013, 56, 802–808. [Google Scholar] [CrossRef] [PubMed]
- Eriksen, M.; Mackay, J.; Ross, H. The Tobacco Atlas, 4th ed.; American Cancer Society: Atlanta, GA, USA; World Lung Foundation: New York, NY, USA, 2012. [Google Scholar]
- Narain, J.P.; Sinha, D.N. Tobacco epidemic in South-East Asia region: Challenges and progress in its control. Indian J. Public Health 2011, 55, 151–154. [Google Scholar] [CrossRef] [PubMed]
- Ward, K.D.; Eissenberg, T.; Rastam, S.; Asfar, T.; Mzayek, F.; Fouad, M.F.; Hammal, F.; Mock, J.; Maziak, W. The tobacco epidemic in Syria. Tob. Control 2006, 15. [Google Scholar] [CrossRef] [PubMed]
- Pampel, F.C. Patterns of tobacco use in the early epidemic stages: Malawi and Zambia, 2000–2002. Am. J. Public Health 2005, 95, 1009–1015. [Google Scholar] [CrossRef] [PubMed]
- Rudmin, F.W. Catalogue of acculturation constructs: Descriptions of 126 taxonomies, 1918–2003. In Online Readings in Psychology and Culture (Unit 8, Chapter 8); Lonner, W.J., Dinnel, D.L., Hayes, S.A., Sattler, D.N., Eds.; Center for Cross-Cultural Research (Western Washington University): Bellingham, WA, USA, 2003. [Google Scholar]
- Berry, J.W. Immigration, Acculturation, and Adaptation. Appl. Psychol. Int. Rev. 1997, 46, 5–34. [Google Scholar] [CrossRef]
- Schwartz, S.J.; Unger, J.B.; Zamboanga, B.L.; Szapocznik, J. Rethinking the concept of acculturation: Implications for theory and research. Am. Psychol. 2010, 65, 237–251. [Google Scholar] [CrossRef] [PubMed]
- Gordon, M. Assimilation in America: Theory and reality. In Notable Selections in Race and Ethnicity; Aguirre, A., Baker, E., Eds.; Dushkin: Guilford, CT, USA, 1995. [Google Scholar]
- Chakraborty, B.M.; Chakraborty, R. Concept, measurement and use of acculturation in health and disease risk studies. Coll. Antropol. 2010, 34, 1179–1191. [Google Scholar] [PubMed]
- Cabassa, L.J. Measuring acculturation: Where we are and where we need to go. Hisp. J. Behav. Sci. 2003, 25, 127–146. [Google Scholar] [CrossRef]
- Abraído-Lanza, A.F.; Armbrister, A.N.; Flórez, K.R.; Aguirre, A.N. Toward a theory-driven model of acculturation in public health research. Am. J. Public Health 2006, 96, 1342–1346. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.S.; Ziedonis, D.; Chen, K.W. Tobacco use and dependence in Asian Americans: A review of the literature. Nicotine Tob. Res. 2007, 9, 169–184. [Google Scholar] [CrossRef] [PubMed]
- Parker, E.D.; Solberg, L.I.; Foldes, S.S.; Walker, P.F. A surveillance source of tobacco use differences among immigrant populations. Nicotine Tob. Res. 2010, 12, 309–314. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Stable, E.J.; Ramirez, A.; Villareal, R.; Talavera, G.A.; Trapido, E.; Suarez, L.; Marti, J.; McAlister, A. Cigarette smoking behavior among U.S. Latino men and women from different countries of origin. Am. J. Public Health 2011, 91, 1424–1430. [Google Scholar] [CrossRef]
- Corral, I.; Landrine, H. Acculturation and ethnic-minority health behavior: A test of the operant model. Health Psychol. 2008, 27, 737–745. [Google Scholar] [CrossRef] [PubMed]
- Federal Statistical Office of Germany. Population and Occupation. People with Migration Background—Results from the Micro Census 2012; Federal Statistical Office of Germany: Wiesbaden, Germany, 2013. [Google Scholar]
- Federal Office for Migration and Refugees. Migration Report 2013; Federal Office for Migration and Refugees: Nürnberg, Germany, 2015. [Google Scholar]
- The Ministry of Health of Turkey. Global Adult Tobacco Survey (GATS)—Turkey Report 2012; The Ministry of Health of Turkey: Ankara, Turkey, 2014. [Google Scholar]
- Ministry of Health and Social Development of the Russian Federation. Global Adult Tobacco Survey (GATS)—Russian Federation Report 2009; Ministry of Health and Social Development of the Russian Federation: Moscow, Russian, 2010.
- Razum, O.; Twardella, D. Time travel with Oliver Twist—Towards an explanation for a paradoxically low mortality among recent immigrants. Trop. Med. Int. Health 2002, 7, 4–10. [Google Scholar] [CrossRef] [PubMed]
- Pampel, F.C. Cigarette diffusion and sex differences in smoking. J. Health Soc. Behav. 2001, 42, 388–404. [Google Scholar] [CrossRef] [PubMed]
- Pampel, F.C. Age and education patterns of smoking among women in high-income nations. Soc. Sci. Med. 2003, 57, 1505–1514. [Google Scholar] [CrossRef]
- Wagner, G.G.; Frick, J.R.; Schupp, J. The German Socio-Economic Panel Study (SOEP)—Scope, Evolution and Enhancement. Schmollers Jahrb. 2007, 127, 139–169. [Google Scholar] [CrossRef]
- Schunck, R. Transnational Activities and Immigrant Integration in Germany Concurrent or Competitive Processes; Springer International Publishing: Cham, Switzerland, 2014. [Google Scholar]
- Kroh, M. Documentation of Sample Sizes and Panel Attrition in the German Socio-Economic Panel (SOEP) (1984 until 2012); SOEP Survey Papers 177: Series D; DIW/SOEP: Berlin, Germany, 2014. [Google Scholar]
- Razum, O.; Zeeb, H.; Rohrmann, S. The “healthy migrant effect”—Not merely a fallacy of inaccurate denominator figures. Int. J. Epidemiol. 2000, 29, 191–192. [Google Scholar] [CrossRef] [PubMed]
- Schunck, R.; Rogge, B.G. No causal effect of unemployment on smoking? A German panel study. Int. J. Public Health 2012, 57, 867–874. [Google Scholar] [CrossRef] [PubMed]
- Schunck, R.; Reiss, K.; Razum, O. Pathways between perceived discrimination and health among immigrants: Evidence from a large national panel survey in Germany. Ethn. Health 2015, 20, 493–510. [Google Scholar] [CrossRef] [PubMed]
- Schunck, R.; Sauer, C.; Valet, P. Unfair Pay and Health: The effects of perceived injustice of earnings on physical health. Eur. Sociol. Rev. 2015. [Google Scholar] [CrossRef]
- Rabe-Hesketh, S.; Skrondal, A. Volume II: Categorical responses, counts, and survival. In Multilevel and Longitudinal Modeling Using Stata, 3rd ed.; STATA Press: College Station, TX, USA, 2012. [Google Scholar]
- Bethel, J.W.; Schenker, M.B. Acculturation and smoking patterns among Hispanics: A review. Am. J. Prev. Med. 2005, 29, 143–148. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Wang, Z. Factors associated with smoking in Asian American adults: A systematic review. Nicotine Tob. Res. 2008, 10, 791–801. [Google Scholar] [CrossRef] [PubMed]
- Hu, S.S.; Pallonen, U.E.; Meshack, A.F. The impact of immigration status on tobacco use among Chinese-American adults in Texas. J. Immigr. Minor. Health 2010, 12, 206–214. [Google Scholar] [CrossRef] [PubMed]
- Reiss, K.; Breckenkamp, J.; Borde, T.; Brenne, S.; David, M.; Razum, O. Smoking during pregnancy among Turkish immigrants in Germany—Are there associations with acculturation? Nicotine Tob. Res. 2015, 17, 643–652. [Google Scholar] [CrossRef] [PubMed]
- Reiss, K.; Spallek, J.; Razum, O. ‘Imported risk’ or ‘health transition’? Smoking prevalence among ethnic German immigrants from the Former Soviet Union by duration of stay in Germany—Analysis of microcensus data. Int. J. Equity Health 2010, 9. [Google Scholar] [CrossRef] [PubMed]
- Reiss, K.; Sauzet, O.; Breckenkamp, J.; Spallek, J.; Razum, O. How immigrants adapt their smoking behaviour: Comparative analysis among Turkish immigrants in Germany and The Netherlands. BMC Public Health 2014, 14. [Google Scholar] [CrossRef] [PubMed]
- Joossens, L.; Raw, M. The Tobacco Control Scale 2013 in Europe. Available online: http://www.europeancancerleagues.org/images/TobaccoControl/TCS_2013_in_Europe_13-03-14_final_1.pdf (accessed on 20 November 2015).
- Mackenbach, J.P.; Karanikolos, M.; McKee, M. The unequal health of Europeans: Successes and failures of policies. Lancet 2013, 381, 1125–1134. [Google Scholar] [CrossRef]
- Grüning, T.; Gilmore, A.B.; McKee, M. Tobacco industry influence on science and scientists in Germany. Am. J. Public Health 2006, 96, 20–32. [Google Scholar]
- WHO Report on the Global Tobacco Epidemic. 2013. Available online: http://www.who.int/tobacco/global_report/2013/en/ (accessed on 10 June 2015).
- Nierkens, V.; van der Ploeg, M.V.; van Eer, M.Y.; Stronks, K. How do psychosocial determinants in migrant women in the Netherlands differ from these among their counterparts in their country of origin? A cross-sectional study. BMC Public Health 2011, 11. [Google Scholar] [CrossRef] [PubMed]
- Stigler, M.; Dhavan, P.; Van Dusen, D.; Arora, M.; Reddy, K.S.; Perry, C.L. Westernization and tobacco use among young people in Delhi, India. Soc. Sci. Med. 2010, 71, 891–897. [Google Scholar] [CrossRef] [PubMed]
- Roberts, B.; Gilmore, A.; Stickley, A.; Rotman, D.; Prohoda, V.; Haerpfer, C.; McKee, M. Changes in smoking prevalence in 8 countries of the former Soviet Union between 2001 and 2010. Am. J. Public Health 2012, 102, 1320–1328. [Google Scholar] [CrossRef] [PubMed]
- Kyobutungi, C.; Ronellenfitsch, U.; Razum, O.; Becher, H. Mortality from cancer among ethnic German immigrants from the Former Soviet Union, in Germany. Eur. J. Cancer 2006, 42, 2577–2584. [Google Scholar] [CrossRef] [PubMed]
- Bharmal, N.; Hays, R.D.; McCarthy, W.J. Validity of temporal measures as proxies for measuring acculturation in Asian Indian survey respondents. J. Immigr. Minor. Health 2014, 16, 889–897. [Google Scholar] [CrossRef] [PubMed]
- Urquia, M.L.; Janevic, T.; Hjern, A. Smoking during pregnancy among immigrants to Sweden, 1992–2008: The effects of secular trends and time since migration. Eur. J. Public Health 2014, 24, 122–127. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; O’Neill, A.H.; Ihara, E.S.; Chae, D.H. Change in self-reported health status among immigrants in the United States: Associations with measures of acculturation. PLoS ONE 2013, 8. [Google Scholar] [CrossRef] [PubMed]
- Poonia, J. Smoking Cessation and Ethnic Minority Communities. Findings of Qualitative Research Project with Turkish, Polish, and Somalian Communities in London; NHS Commissioning Support for London: London, UK, 2009. [Google Scholar]
© 2015 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reiss, K.; Schunck, R.; Razum, O. Effect of Length of Stay on Smoking among Turkish and Eastern European Immigrants in Germany—Interpretation in the Light of the Smoking Epidemic Model and the Acculturation Theory. Int. J. Environ. Res. Public Health 2015, 12, 15925-15936. https://doi.org/10.3390/ijerph121215030
Reiss K, Schunck R, Razum O. Effect of Length of Stay on Smoking among Turkish and Eastern European Immigrants in Germany—Interpretation in the Light of the Smoking Epidemic Model and the Acculturation Theory. International Journal of Environmental Research and Public Health. 2015; 12(12):15925-15936. https://doi.org/10.3390/ijerph121215030
Chicago/Turabian StyleReiss, Katharina, Reinhard Schunck, and Oliver Razum. 2015. "Effect of Length of Stay on Smoking among Turkish and Eastern European Immigrants in Germany—Interpretation in the Light of the Smoking Epidemic Model and the Acculturation Theory" International Journal of Environmental Research and Public Health 12, no. 12: 15925-15936. https://doi.org/10.3390/ijerph121215030
APA StyleReiss, K., Schunck, R., & Razum, O. (2015). Effect of Length of Stay on Smoking among Turkish and Eastern European Immigrants in Germany—Interpretation in the Light of the Smoking Epidemic Model and the Acculturation Theory. International Journal of Environmental Research and Public Health, 12(12), 15925-15936. https://doi.org/10.3390/ijerph121215030





