The Patient’s Perspective of in-Home Telerehabilitation Physiotherapy Services Following Total Knee Arthroplasty
Abstract
:1. Introduction
2. Methods
2.1. Study Design
2.2. Participant Recruitment
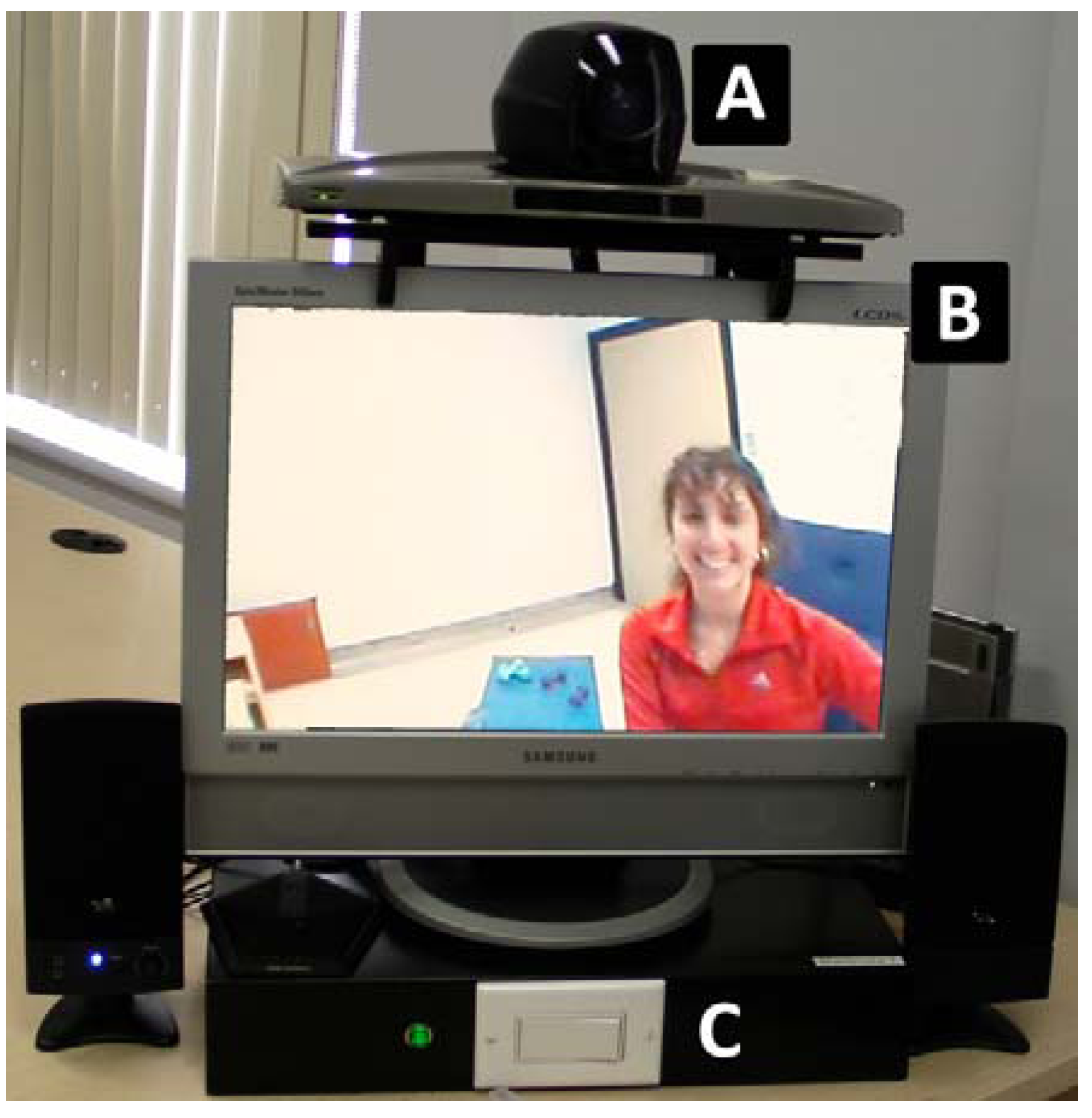
2.3. Description of the in-Home Telerehabilitation Program
2.4. Data Collection and Analysis
3. Results
3.1. Improving Access to Services
| Characteristics | Participant 1 | Participant 2 | Participant 3 | Participant 4 | Participant 5 |
|---|---|---|---|---|---|
| Gender | Woman | Man | Man | Woman | Woman |
| Age (years) | 44 | 72 | 62 | 59 | 70 |
| Years of schooling (years) | 15 | 18.5 | 15 | 16 | 11 |
| Work status | Not working | Retired | On disability | Specialized educator (on leave for recovery from TKA) | Retired |
| Living alone | Yes | No, with wife | Yes | Yes | No, with husband |
| Type of housing | Apartment building | Single family dwelling | Single family dwelling | Apartment building | Duplex |
| Stairs at home | Yes | Yes | No | Yes | Yes |
| Prior internet service | No | Yes | No | Yes | No |
| Years of knee pain (years) | 1–5 | More than 10 | 1–5 | More than 10 | More than 10 |
| Other medical condition | Arthritis, diabetes, anxiety, disc degeneration | Arthritis, diabetes, gastro-intestinal disorder, visual problem, hypertension, prostate cancer in remission | Arthritis, asthma, acute respiratory distress syndrome (ARDS), angina, gastro-intestinal disorder, depression, anxiety | Arthritis, asthma, diabetes, depression, anxiety, sleep apnea, hypertension | Arthritis, gastro-intestinal disorder, hyperthyroidism, double pulmonary embolism |
“I really like it (telerehabilitation). I found it fantastic…you know, just the fact of not having to travel when we are in pain (…) I adored it…” (participant 2)
3.2. Developing a Bond with Their Therapist While Maintaining a Sense of Personal Space
“Well look, she (the physiotherapist), was roughly my nieces’ age. So it was the same as if I was an aunt with her” (participant 1)“…we talked about fishing, we talked about hunting, (…) we talked about skiing, hum, of all sorts of things, while I was doing my exercises, we talked about anything and we always had something to say. I think that she knew my whole life (laughter) (…)” (participant 4)
“I was satisfied. (...) the fact that she (the physiotherapist) was not with me in the house, I was less stressed.” (participant 4)
3.3. Complementing Telerehabilitation with in-Person Visits
“… she would have seen if she had touched me that my patella was not in the right place.” (participant 1)“I’m fairly certain that at least twice, on two occasions certainly if he would have come, it would have been a plus. Well, maybe psychologically, I think, thinking that he could have manipulated your knee, to see in a tangible manner and be able to manipulate it, but hum… it’s the suggestion that I would give, to at least meet, I don’t know how often … (…).” (participant 2)
3.4. Providing Standardized yet Tailored and Challenging Exercise Programs Using Telerehabilitation
“I installed the things I needed. Like that, all my bicycle, and hum... my step. I installed that and it went well. Look, it took 2 min.” (participant 3)“I got on the bike (stationary bicycle). I was hooked up (by videoconference), and I got on the bike. Instead of him (the physiotherapist) watching me for 10–15 min, I had already done a few minutes. So that after that, well, we did the rest.” (participant 4)
3.5. Perceived Ease-of-Use of Telerehabilitation Equipment
3.6. Achieving an Ongoing Sense of Support
“They had told me that it would be this way (…). So being advised, you know, you’re ok. (…) This way, being advised of the date, that the beginning of the treatments will be on such and such a date. And having the little handouts that said which exercises to do, well then ultimately, it was positive regardless. We say well we’re heading in, in the right direction… to recuperate.” (participant 2)
4. Discussion
Study Limitations and Future Directions
5. Conclusions
Acknowledgements
Conflicts of Interest
References
- Coyte, P.; Young, W. Variation in Use of and Reinvestment in Home Care Services Following an Acute Hospitalization, 1st ed.; The Institute for Clinical Evaluative Science in Ontario: Toronto, Canada, 1997. [Google Scholar]
- Pérodeau, G.; Côté, D. Le Virage Ambulatoire: Défis et Enjeux, 1st Ed. ed; Les presses de l’Université Laval: Ste-Foy, Canada, 2002. [Google Scholar]
- Ministère de la santé et des services sociaux. Plan de santé et des Services Sociaux, Pour Faire Les Bons Choix. Direction des communications du MSSS-Québec: Québec, Canada, 2002. Available online: http://publications.msss.gouv.qc.ca/acrobat/f/documentation/2002/02-108.pdf (accessed on 28 August 2013).
- Ministère de la santé et des services sociaux. Plan d’action 2005–2010—un défi de solidarité: Les Services Aux aînés en Perte d’autonomie. Direction des communications du MSSS-Québec: Québec, Canada, 2005. Available online: http://publications.msss.gouv.qc.ca/acrobat/f/documentation/2005/05-830-01.pdf (accessed on 28 August 2013).
- Ministère de la santé et des services sociaux. Chez Soi: Le Premier Choix. Précisions Pour Favoriser l’implantation de la Politique de soutien à Domicile. Direction des communications du MSSS-Québec: Québec, Canada, 2004. Available online: http://publications.msss.gouv.qc.ca/acrobat/f/documentation/2002/02-704-01.pdf (accessed on 28 August 2013).
- Latulipe-Richard, C. Regard approfondi sur sept grandes professions de la santé. Le Bloc Notes. 2008. Available online: http://www.leblocnotes.ca/node/2457 (accessed on 28 August 2013).
- Tran, D.; Hall, L.; Davis, A.; Landry, M.; Burnett, D.; Berg, K.; Jaglal, S. Identification of recruitment and retention strategies for rehabilitation professionals in Ontario, Canada: Results from expert panels. BMC Health Serv. Res. 2008, 8, 249. [Google Scholar] [CrossRef]
- Hailey, D.; Roine, R.; Ohinmaa, A.; Dennett, L. Evidence on the Effectiveness of Telerehabilitation Applications; Institute of Health Economics and Finnish Office for Health Technology Assessment: Edmonton and Helsinki, Canada, 2010. [Google Scholar]
- Russell, T.G. Physical rehabilitation using telemedicine. J. Telemed. Telecare 2007, 13, 217–220. [Google Scholar] [CrossRef]
- Kaur, K.; Foducey, P.; Smith, L.; Scheideman-Miller, C. Organisational design and implementation of a telerehabilitation system in Oklahoma. Int. J. Technol. Manag. 2004, 6, 56–75. [Google Scholar]
- Tousignant, M.; Boissy, P.; Corriveau, H.; Moffet, H. In home telerehabilitation for older adults after discharge from an acute hospital or rehabilitation unit: A proof-of-concept study and costs estimation. Disabil. Rehabil. Assist. Technol. 2006, 1, 209–216. [Google Scholar] [CrossRef]
- Theodoros, D.; Russell, T. Telerehabilitation: Current perspectives. Stud. Health Technol. Inform. 2008, 131, 191–209. [Google Scholar]
- Pineau, G.; Moqadem, K.; St-Hilaire, C.; Levac, E.; Hamel, B. Télésanté: Lignes Directrices Cliniques et Normes Technologiques en Téléréadpatation. In Agences des technologies et des modes d’intervention en santé; Gouvernement du Québec: Québec, Canada, 2006. [Google Scholar]
- Simpson, L.A.; Miller, W.C.; Eng, J.J. Effect of stroke on fall rate, location and predictors: A prospective comparison of older adults with and without stroke. PLoS One 2011, 6, e19431. [Google Scholar] [CrossRef]
- Rogante, M.; Grigioni, M.; Cordella, D.; Giacomozzi, C. Ten years of telerehabilitation: A literature overview of technologies and clinical applications. NeuroRehabilitation 2010, 27, 287–304. [Google Scholar]
- Johansson, T.; Wild, C. Telerehabilitation in stroke care—A systematic review. J. Telemed. Telecare 2011, 17, 1–6. [Google Scholar] [CrossRef]
- Kairy, D.; Lehoux, P.; Vincent, C.; Visintin, M. A systematic review of clinical outcomes, clinical process, healthcare utilization and costs associated with telerehabilitation. Disabil. Rehabil. 2009, 31, 427–447. [Google Scholar] [CrossRef]
- Broens, T.H.; Huis in’t Veld, R.M.; Vollenbroek-Hutten, M.M.; Hermens, H.J.; van Halteren, A.T.; Nieuwenhuis, L.J. Determinants of successful telemedicine implementations: A literature study. J. Telemed. Telecare 2007, 13, 303–309. [Google Scholar] [CrossRef]
- Finch, T.; Mort, M.; May, C.; Mair, F. Telecare: Perspectives on the changing role of patients and citizens. J. Telemed. Telecare 2005, 11, 51–53. [Google Scholar] [CrossRef]
- Jackson, D.E.; McClean, S.I. Trends in telemedicine assessment indicate neglect of key criteria for predicting success. JHOM 2012, 26, 508–523. [Google Scholar]
- Mair, F.; Whitten, P. Systematic review of studies of patient satisfaction with telemedicine. BMJ 2000, 320, 1517–1520. [Google Scholar] [CrossRef]
- Mair, F.S.; Goldstein, P.; May, C.; Angus, R.; Shiels, C.; Hibbert, D.; O’Connor, J.; Boland, A.; Roberts, C.; Haycox, A.; et al. Patient and provider perspectives on home telecare: Preliminary results from a randomized controlled trial. J. Telemed. Telecare 2005, 11, 95–97. [Google Scholar] [CrossRef]
- Tousignant, M.; Boissy, P.; Moffet, H.; Corriveau, H.; Cabana, F.; Marquis, F.; Simard, J. Patients’ satisfaction of healthcare services and perception with in-home telerehabilitation and physiotherapists’ satisfaction toward technology for post-knee arthroplasty: An embedded study in a randomized trial. Telemed. J. E Health 2011, 17, 376–382. [Google Scholar] [CrossRef]
- Cranen, K.; Drossaert, C.H.; Brinkman, E.S.; Braakman-Jansen, A.L.; Ijzerman, M.J.; Vollenbroek-Hutten, M.M. An exploration of chronic pain patients’ perceptions of home telerehabilitation services. Health Expect. 2011, 15, 339–350. [Google Scholar]
- Cranen, K.; Veld, R.H.; Ijzerman, M.; Vollenbroek-Hutten, M. Change of patients’ perceptions of telemedicine after brief use. Telemed. J. E Health 2011, 17, 530–535. [Google Scholar] [CrossRef]
- Huis in’t Veld, R.; Kosterink, S.; Barbe, T.; Lindegard, A.; Marecek, T.; Vollenbroek-Hutten, M. Relation between patient satisfaction, compliance and the clinical benefit of a teletreatment application for chronic pain. J. Telemed. Telecare 2010, 16, 322–328. [Google Scholar] [CrossRef]
- Eriksson, L.; Lindstrom, B.; Ekenberg, L. Patients’ experiences of telerehabilitation at home after shoulder joint replacement. J. Telemed. Telecare 2011, 17, 25–30. [Google Scholar] [CrossRef]
- Piron, L; Turolla, A; Tonin, P; Piccione, F; Lain, L; Dam, M. Satisfaction with care in post-stroke patients undergoing a telerehabilitation programme at home. J. Telemed. Telecare 2008, 14, 257–260. [Google Scholar] [CrossRef]
- Yin, R. Case Study Research: Design and Methods, 3rd ed.; Sage Publications: Thousand Oaks, CA, USA, 2003. [Google Scholar]
- Tripp-Reimer, T.; Doebbeling, B. Qualitative perspectives in translational research. Worldviews Evid. Based Nurs. 2004, 1, S65–S72. [Google Scholar] [CrossRef]
- Groenewald, T. A phenomenological research design illustrated. Int. J. Qual. Methods 2004, 3, 4:1–4:26. [Google Scholar]
- Moffet, H.; Collet, J.P.; Shapiro, S.H.; Paradis, G.; marquis, F.; Roy, L. Effectiveness of intensive rehabilitation on functional ability and quality of life after first total knee arthroplasty: A single-blind randomized controlled trial. Arch. Phys. Med. Rehabil. 2004, 85, 546–556. [Google Scholar] [CrossRef]
- Tousignant, M.; Boissy, B.; Corriveau, H.; Moffet, H.; Cabana, F. In-home telerehabilitation for post-knee arthroplasty: A pilot study. Int. J. Telereabil. 2009, 1, 9–16. [Google Scholar]
- Venkatesh, V.; Morris, M.; Davis, G.; Davis, F. User acceptance of information technology: Toward a unified view. MIS Quaterly 2003, 27, 425–478. [Google Scholar]
- Miles, M.B.; Huberman, A.M. Qualitative Data Analysis: An Expanded Sourcebook, 2nd ed.; Sage publications: Thousand Oaks, CA, USA, 1994. [Google Scholar]
- Crepeau, E.B.; Garren, K.R. I looked to her as a guide: The therapeutic relationship in hand therapy. Disabil. Rehabil. 2011, 33, 872–881. [Google Scholar] [CrossRef]
- Bonnin, M.P.; Basiglini, L.; Archbold, H.A. What are the factors of residual pain after uncomplicated tka? Knee Surg. Sports Traumatol. Arthrosc. 2011, 19, 1411–1417. [Google Scholar] [CrossRef]
- Brander, V.A.; Stulberg, S.D.; Adams, A.D.; Harden, R.N.; Bruehl, S.; Stanos, S.P.; Houle, T. Predicting total knee replacement pain: A prospective, observational study. Clin. Orthop. Relat. Res. 2003, 416, 27–36. [Google Scholar] [CrossRef]
- Guba, E.; Lincoln, Y. Fourth Generation Evaluation; Sage Publications: Thousand Oaks, CA, USA, 1989. [Google Scholar]
© 2013 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Kairy, D.; Tousignant, M.; Leclerc, N.; Côté, A.-M.; Levasseur, M.; Researchers, T.T. The Patient’s Perspective of in-Home Telerehabilitation Physiotherapy Services Following Total Knee Arthroplasty. Int. J. Environ. Res. Public Health 2013, 10, 3998-4011. https://doi.org/10.3390/ijerph10093998
Kairy D, Tousignant M, Leclerc N, Côté A-M, Levasseur M, Researchers TT. The Patient’s Perspective of in-Home Telerehabilitation Physiotherapy Services Following Total Knee Arthroplasty. International Journal of Environmental Research and Public Health. 2013; 10(9):3998-4011. https://doi.org/10.3390/ijerph10093998
Chicago/Turabian StyleKairy, Dahlia, Michel Tousignant, Nancy Leclerc, Anne-Marie Côté, Mélanie Levasseur, and The Telage Researchers. 2013. "The Patient’s Perspective of in-Home Telerehabilitation Physiotherapy Services Following Total Knee Arthroplasty" International Journal of Environmental Research and Public Health 10, no. 9: 3998-4011. https://doi.org/10.3390/ijerph10093998
APA StyleKairy, D., Tousignant, M., Leclerc, N., Côté, A.-M., Levasseur, M., & Researchers, T. T. (2013). The Patient’s Perspective of in-Home Telerehabilitation Physiotherapy Services Following Total Knee Arthroplasty. International Journal of Environmental Research and Public Health, 10(9), 3998-4011. https://doi.org/10.3390/ijerph10093998








